Abstract
Objective
A pilot study evaluated whether the addition of online coaching from a peer specialist increased participation in an online program featuring educational and interactive modules to promote self-management of bipolar disorder.Methods
A total of 118 participants with bipolar disorder recruited from online and in-person support groups and clinical settings were enrolled in MyRecoveryPlan. Half the group was randomly assigned to receive online coaching support from a certified peer specialist.Results
Participants offered online peer coaching were more likely to return to the program after registration (71% versus 44%, p=.005) and to continue using the program after three weeks (38% versus 9%, p<.001). This pattern was consistent for all program elements.Conclusions
The addition of online coaching from a peer specialist significantly increased engagement and retention in the program, but further research is needed to evaluate the program's effects on clinical and recovery outcomes.Free full text

An Online Recovery Plan Program: Can Peer Coaching Increase Participation?
Abstract
Objective
A pilot study evaluated whether the addition of online coaching from a peer specialist increased participation in an online program featuring educational and interactive modules to promote self-management of bipolar disorder.
Methods
A total of 118 participants with bipolar disorder recruited from online and in-person support groups and clinical settings were enrolled in MyRecoveryPlan. Half the group was randomly assigned to receive online coaching support from a certified peer specialist.
Results
Participants offered online peer coaching were more likely to return to the program after registration (71% versus 44%, p=.005) and to continue using the program after three weeks (38% versus 9%, p<.001). This pattern was consistent for all program elements.
Conclusions
The addition of online coaching from a peer specialist significantly increased engagement and retention in the program, but further research is needed to evaluate the program’s effects on clinical and recovery outcomes.
Growing evidence supports the effectiveness of psychoeducational and psychotherapy programs to support self-management by people with bipolar disorder (1,2). Key elements of these programs include self-monitoring for warning signs, maintaining healthy routines, and employing behavioral strategies for responding to warning signs or increasing symptoms. Several programs that have proven effective in randomized trials involve the use of support groups to encourage self-management.
Some more recent programs also include a broader emphasis on wellness, strengths, and peer support (3–6). Evidence regarding the effectiveness of these recovery-oriented programs, although limited, suggests that they have positive effects on confidence, wellness, and self-management skills.
Empirically supported psychotherapy or psychoeducational programs that promote self-management have disseminated only minimally beyond research settings and are not available to most people living with bipolar disorder. Formal peer-support services are increasingly available in community mental health settings and in the U.S. Department of Veterans Affairs (7,8) but usually are not present elsewhere. Currently, peer-support groups reach only a small number of the millions of Americans living with bipolar disorder.
Internet-based programs have the potential to significantly increase the reach of psychoeducation and self-management support. They can be provided in any location at any time with minimal cost. Previous research regarding Internet-based programs for depression and anxiety disorders, however, suggests that without peer support, patients tend to drop out at high rates and receive limited benefit (9,10). In contrast, Internet-based programs supported by reminders, coaching, or both have shown higher retention rates and more robust clinical benefits (10–13).
Methods
In this pilot study, individuals with bipolar disorder enrolled in an Internet-based program to help create and use personal recovery plans were randomly assigned to a group that received online peer coaching or a group that did not. We compared the two groups’ use of the program at any time from enrollment (between January and September 2009) until the end of the study period (January 1, 2010). We also examined continued use (any use three weeks after enrollment).
MyRecoveryPlan is an interactive online program to support people living with bipolar disorder in creating and using personal recovery plans. The program was developed by researchers at the Group Health Research Institute and staff of the Depression and Bipolar Support Alliance (DBSA). People living with bipolar disorder contributed to the design of the Web site and the coaching program.
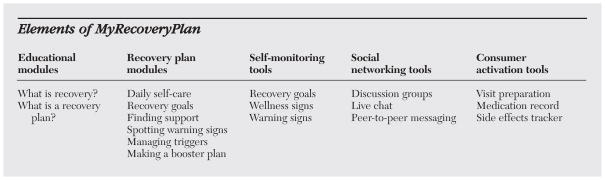
Elements of MyRecoveryPlan are listed in the box on this page. The educational and recovery plan modules include information, slide shows, and brief personal videos about the concept of recovery, the value of creating a personal recovery plan, and each element of the recovery plan, including establishing recovery goals, engaging in daily self-care, building a personal support system, monitoring signs of wellness, noticing symptoms or warning signs, managing stresses or triggers, and creating a booster plan for times of increased symptoms (14). Recovery-plan modules include an interactive section for each user to create and update his or her plan.
Self-monitoring modules included customizable tools for tracking indicators of wellness as well as warning signs or symptoms. Social networking modules, including a discussion board, chat rooms, and peer-to-peer messaging, allow participants to exchange information and support each other. Consumer activation modules encourage participants to become more active partners in health care by tracking medication use and side effects and by maintaining a calendar to organize health care appointments and keeping a list of topics to discuss at each visit.
Study participants were recruited through e-mail announcements to local DBSA chapters, announcements on the DBSA Web site discussion board, announcement cards in mental health clinics in the Seattle area, sponsored advertisements on the Google Web site, and invitations from participants to peers.
Participants were required to electronically sign a consent form available on the Web site describing the purpose of the study, study procedures, and potential risks and to certify that they were currently in treatment for bipolar disorder, were residents of the United States, and were at least 19 years old. Each participant provided an e-mail address in order to receive reminders to use the Web site. To protect participants’ privacy, no identifying information or clinical information was collected that would allow us to assess their diagnosis or severity of symptoms. Each participant gave explicit consent for information collected through the program to be used for research. Participants were enrolled between January and September of 2009, and the program remained available to all participants until January of 2010.
Immediately after initial sign-up, each participant was randomly assigned to one of two groups, a coaching group that received on-line peer coaching and a program-only group that did not. An e-mail was automatically generated to notify participants of their assignment and to invite them to begin creating a personal recovery plan.
The two peer coaches supporting the program were people who had experience in living with bipolar disorder. Both had completed DBSA peer specialist training and certification and had at least four years’ experience working as peer specialists in outpatient mental health settings. Both coaches participated actively in design of the Web site and the coaching program. During the study period, coaches received supervision during weekly teleconferences with GES and EJL.
Each participant assigned to the coaching group received an additional welcome message describing the program, introducing the peer coaches, and encouraging participation in online peer support activities, such as discussion groups and online chats. Participants in the coaching group were encouraged to send messages to coaches seeking additional information or support. To protect participants’ privacy all communications occurred within the secure Web site. An e-mail was sent to the participants alerting them every time they received a new message at MyRecoveryPlan, but it contained no sensitive information.
Peer coaches used several types of messages to communicate with participants. At appropriate times, they sent personal messages encouraging use of a personal recovery plan and responded within two or three days to messages from users requesting information or support. (Participants were advised not to rely on the Web site or the coach in an emergency or crisis.) Coaches sent personalized outreach messages to individuals who had not visited the Web site for at least two weeks. Approximately twice each month, coaches broadcast newsletter messages that discussed specific topics, such as managing stress during holidays, and encouraged participation in discussion groups and chat sessions. The coaches also initiated and participated in discussion threads focused on recovery-oriented topics and scheduled online chat sessions regarding specific topics two or three times each week.
Although the content and frequency of these communications varied from individual to individual, all communications were intended to promote the concept of recovery, foster development and use of a personal recovery plan, and encourage participation in the program’s peer support activities. The program was intended to supplement—not replace —traditional mental health care. Coaches did not provide psychotherapy or give advice regarding medication treatments.
Although members assigned to the program-only group had no contact with peer coaches, they were free to use any features of the program, including social networking tools (discussion groups, live chats, and peer-to-peer messaging). To prevent contamination, discussion groups and chat rooms for the program-only and coaching groups were separated.
Use of specific program components over the course of the study period by the two groups was compared. In addition, we compared the groups’ continued use of the program—that is, after they had been enrolled for three weeks. The three-week threshold was an arbitrarily chosen marker of continued use.
Results
A total of 118 individuals enrolled in MyRecoveryPlan. Most participants were women (N=85, 72%), and 22 (19%) reported being of a minority race or ethnicity. No information was available about the number or characteristics of individuals who visited the program Web site but chose not to enroll. No participants who chose to enroll were excluded.
Table 1 summarizes use by both groups at any time and three weeks after enrollment. Across both groups, rates of engagement were highest for use of the interactive recovery plan, lower for use of social networking features, and lowest for use of self-monitoring tools (Table 1). Rates of engagement for all features of the program were higher in the coaching group, but not every comparison was statistically significant. In the coaching group, proportions using various program features three weeks after enrollment were approximately half the rates of initial use. In the program-only group, the drop-off after initial use was even greater. No participants in the program-only group added to or changed recovery plan components after the initial three weeks.
Table 1
Participation in specific components of MyRecoveryPlan during a one-year pilot study
| Component | At any time
| After 21 days
| ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Coaching group (N=64)
| Program-only group (N=54)
| pa | Coaching group (N=64)
| Program-only group (N=54)
| pa | |||||
| N | % | N | % | N | % | N | % | |||
| Returned after initial sign-up | 45 | 71 | 24 | 44 | .005 | 24 | 38 | 5 | 9 | <.001 |
| Started or updated recovery plan | ||||||||||
 Any section Any section | 38 | 59 | 22 | 41 | .064 | 12 | 19 | 0 | — | <.001 |
 Recovery goals Recovery goals | 33 | 52 | 20 | 37 | .139 | 11 | 17 | 0 | — | <.001 |
 Daily self-care Daily self-care | 22 | 34 | 0 | — | .001 | 11 | 17 | 0 | — | <.001 |
 Finding support Finding support | 18 | 28 | 0 | — | .001 | 10 | 16 | 0 | — | .002 |
 Spotting warning signs Spotting warning signs | 18 | 28 | 10 | 18 | .279 | 10 | 16 | 0 | — | .002 |
| Used self-monitoring tools | ||||||||||
 Progress toward goals Progress toward goals | 7 | 11 | 2 | 4 | .177 | 5 | 8 | 0 | — | .062 |
 Warning signs Warning signs | 6 | 10 | 1 | 2 | .123 | 5 | 8 | 0 | — | .062 |
 Medication and side effects Medication and side effects | 14 | 22 | 0 | — | <.001 | 6 | 10 | 0 | — | .031 |
| Used social networking tools | ||||||||||
 Discussion groups Discussion groups | 19 | 30 | 5 | 9 | .006 | 10 | 16 | 0 | — | .002 |
 Peer-to-peer messages Peer-to-peer messages | 11 | 17 | 3 | 6 | .084 | 7 | 11 | 0 | — | .015 |
Discussion
The findings support our hypothesis that online peer coaching would significantly increase use of an online recovery plan program. The group receiving coaching support had higher rates of engagement in every component of the recovery plan, though some differences were not statistically significant. These differences were greater after three weeks of participation. The program-only group had moderate engagement in sections of the recovery plan recommended as starting points (“recovery goals” and “spotting warning signs”), but they made minimal use of other sections. Nor did they make any changes to their recovery plans after three weeks.
Our findings regarding the positive effect of coaching on participation are similar to those seen with other online interventions for mental health treatment (10,12). We cannot determine whether the effects of online coaching would have been different if our coaches had been clinicians or lay people without the experience of having lived with bipolar disorder.
We are not aware of comparable data regarding other Internet-based programs for people with bipolar disorder, but retention rates in both groups were low compared with those reported in previous studies of Internet-based programs for people with unipolar depression (11,12,15).
This finding may reflect differences between this study sample and those in previous studies. Because our objective was to evaluate acceptability of the MyRecoveryPlan program, the enrollment process included as few barriers to entry as possible. Participants were not asked to provide identifying information, were not asked to submit to clinical assessment, and were not required to participate beyond enrollment. We would expect higher rates of participation if enrollment required a higher level of motivation or commitment.
The participants’ use of self-monitoring tools was lower than we had expected. Their comments and feedback suggested that for most participants customizable self-monitoring tools were too complex and required too much effort. Consequently, our results may reflect more on the design of this program than on the level of interest in self-monitoring.
The social networking features of the MyRecoveryPlan program might have been more engaging if the community of users had been larger. An inherent difficulty of any study of the use or benefits of peer-support networks is their small size; a research intervention may not include enough participants to truly evaluate the potential of a peer network or other social-network intervention.
Conclusions
Online programs to encourage recovery planning and provide peer support have the potential to restore hope, increase self-confidence, and facilitate daily self-care among individuals with bipolar disorders. Our results indicate that online coaching from a peer specialist significantly increased engagement and retention in MyRecoveryPlan. Future research should examine the effect of adding peer coaching to other online programs on quality of life and daily functioning.
Acknowledgments
The study was supported by grant P20-MH068572 from the National Institute of Mental Health.
References
Full text links
Read article at publisher's site: https://doi.org/10.1176/ps.62.6.pss6206_0666
Read article for free, from open access legal sources, via Unpaywall:
https://europepmc.org/articles/pmc4176611?pdf=render
Citations & impact
Impact metrics
Citations of article over time
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1176/ps.62.6.pss6206_0666
Article citations
Best practice guidelines for citizen science in mental health research: systematic review and evidence synthesis.
Front Psychiatry, 14:1175311, 08 Sep 2023
Cited by: 2 articles | PMID: 37743990 | PMCID: PMC10515389
Review Free full text in Europe PMC
Operationalising a Recovery-Oriented Support and Information Programme Online: The EOLAS Programme.
Int J Environ Res Public Health, 20(5):4417, 01 Mar 2023
Cited by: 1 article | PMID: 36901424 | PMCID: PMC10002363
Development and Structures of Trialogue for Bipolar Disorders in Germany and Guidelines of the German Society for Bipolar Disorders.
Medicina (Kaunas), 57(11):1213, 05 Nov 2021
Cited by: 0 articles | PMID: 34833431 | PMCID: PMC8624744
Review Free full text in Europe PMC
Technology-supported strategies for promoting user engagement with digital mental health interventions: A systematic review.
Digit Health, 8:20552076221098268, 01 Jan 2022
Cited by: 16 articles | PMID: 35677785 | PMCID: PMC9168921
Review Free full text in Europe PMC
GamblingLess: A Randomised Trial Comparing Guided and Unguided Internet-Based Gambling Interventions.
J Clin Med, 10(11):2224, 21 May 2021
Cited by: 10 articles | PMID: 34063826 | PMCID: PMC8196610
Go to all (33) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Funding
Funders who supported this work.
NIMH NIH HHS (2)
Grant ID: P20MH068572
Grant ID: P20 MH068572