Abstract
Purpose
To compare the difference and agreement of axial length (AL) and anterior segment parameters obtained from the MYAH device with Pentacam AXL and IOLMaster 700 in myopic children.
Methods
The study included 60 eyes of 60 myopic children. AL, keratometry (K), and horizontal corneal diameter (CD) were measured with Pentacam AXL, IOLMaster 700, and MYAH, respectively. The Friedman test was used to assess the differences. The Intraclass Correlation Coefficient (ICC) and Bland–Altman plots were used to assess the consistency of measurements.
Results
The mean age was 10.2 ± 1.8 years (7–16 years). No statistically significant difference was determined between the Pentacam AXL, IOLMaster 700, and MYAH devices in terms of mean AL values (23.61 ± 1.42, 23.62 ± 1.45, 23.61 ± 1.42, respectively) (p = 0.06). The difference between devices in the mean steep K, flat K, mean K, and CD was statistically significant but clinically insignificant (steep K; 44.45 ± 1.25, 44.59 ± 1.23, 44.51 ± 1.24, flat K; 43.29 ± 1.28, 43.43 ± 1.29, 43.35 ± 1.30, mean K; 43.85 ± 1.21, 44.00 ± 1.19, 43.94 ± 1.20, and CD; 11.90 ± 0.34, 12.11 ± 0.38, 11.96 ± 0.31, respectively; p < 0.05). ICC and Bland–Altman plot analysis revealed a high correlation between the three devices in AL, steep K, flat K, mean K, and CD measurements.
Conclusion
There was a quite good agreement between the MYAH, Pentacam AXL, and IOLMaster 700 devices regarding AL and anterior segment parameters. MYAH provides reliable measurements and will be a good option in the diagnosis of and follow-up with myopic children.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
High myopia, which is a preventable cause of sight loss, is a risk factor for potentially sight-threatening ocular disorders such as retinal detachment, myopic macular degeneration, and glaucoma [1, 2]. Myopic progression is basically linked to an increase in axial length (AL) [3]. In 2017, Tideman et al. defined percentile curves to estimate myopic progression according to patient age and AL. Thus, with these reference curves, children can be compared with other children of the same age, and early treatments can be started in children with AL values higher than expected for their age group [4].
The newly developed MYAH (Topcon EU, Visia Imaging, Japan) device measures AL with the optical low coherence interferometry (OLCI) principle, and progression analysis can be made with the benefit of the Tideman percentile curves integrated into the device. Furthermore, with the integral Placido disk topography, data can be provided about the corneal curvature, aberrations, and ectatic diseases such as keratoconus, which can also cause myopic progression [A].
A number of devices on the market have proven their reliability in measuring the AL and keratometric (K) values. These devices include the IOLMaster 500 (Carl Zeiss Meditec AG, Germany), which works with the partial coherence interferometry (PCI) principle, the IOLMaster 700 (Carl Zeiss Meditec AG, Germany), which works with the swept-source optic coherence tomography (SS-OCT) principle, the Pentacam AXL (Oculus Optikgerate GmbH, Germany), which works with the Scheimpflug camera and the PCI principle, the Lenstar (Haag-Streit AG, Switzerland), which works with optical low coherence reflectometry (OLCR), and the Aladdin (Topcon EU, Visia Imaging, Japan) device, similar to MYAH, which works with optical low coherence interferometry (OLCI) principle [5]. It is critical to compare the MYAH device's measurements to those of other devices to determine whether they can be used interchangeably in clinical practice.
This study aimed to compare the difference and agreement of AL and anterior segment parameters obtained from the MYAH device with Pentacam AXL and IOLMaster 700 in myopic children.
Methods
This retrospective comparative study included 60 eyes of 60 myopic children aged 7–16 years who presented for a routine ophthalmological examination at our clinic between October 2021 and December 2021. Some of the children were newly diagnosed, and some were under follow-up. All had spherical equivalent values in the range of −0.50 and −6.00 diopters (D). To prevent double organ bias, only the right eyes were included. Eyes were excluded from the study if there was any other ocular disease such as strabismus, corneal scarring, retinal disease, degenerative myopia, or a history of ocular trauma or surgery. Approval for the study was granted by the local ethics committee, and all procedures were applied in compliance with the principles of the Declaration of Helsinki. Written informed consent was obtained from the parents or legal guardians of all the children participating in the study.
All cases underwent a detailed ophthalmological examination, including visual acuity, slit-lamp biomicroscopy, fundoscopy, and cycloplegic refraction.
Instruments and measurements
All the measurements were taken by the same doctor in a darkened room before the ophthalmological examination. Each subject was positioned with the chin and forehead placed in the device brackets and was then instructed to fixate on the light. The AL, steep K, flat K, mean K, and CD values were obtained using Pentacam AXL, IOLMaster 700, and MYAH devices. Each measurement was taken three times, and the average value was included in the analyses.
Pentacam AXL
The Pentacam AXL is a device that works with both the Scheimpflug camera and PCI principle. The AL measurement is performed in the range of 14–40 mm using PCI at 780 nm wavelength. Both the anterior and posterior curvatures of the cornea are evaluated with the Scheimpflug camera, and 100 images can be obtained in 2 s.
IOLMaster 700
The IOLMaster 700 is a device that was designed mainly for biometry and works with the principle of SS-OCT at 1050 nm wavelength. With OCT imaging of the fovea centralis, the AL is measured from the actual visual axis. K measurements are taken on 19 reference points, and both the anterior and posterior curvatures of the cornea can be evaluated.
MYAH
The MYAH device is a compact device designed to evaluate the AL measurement with OLCI, the corneal curvature with Placido disk topography, pupillometry, and dry eye assessment. Myopic progression is analyzed with the Tideman curves integrated into the device. The AL measurement is performed in the range of 15–38 mm using a superluminescent 830 nm diode laser. K measurements are performed with the evaluation of 24 Placido rings reflected from the anterior corneal curvature.
Statistical analysis
Data analysis was made by SPSS Statistics (version 28.0, IBM Corporation, Armonk, NY, USA). Descriptive statistics were shown as mean ± standard deviation, median, minimum, and maximum values. While the Friedman test was used to analyze the difference between measurements, the agreement of the measurements was evaluated using the ICC and Bland–Altman plots.
Results
The study included 60 children (32 males and 28 females) with a mean age of 10.2 ± 1.8 years (7–16 years) and a mean spherical equivalent value of −1.55D (−0.75 to −6.00 D).
The mean AL values were measured as 23.61 ± 1.42 mm (21.74–28.22 mm) for the Pentacam AXL, 23.62 ± 1.45 mm (21.77 to 28.23 mm) for the IOLMaster 700, and 23.61 ± 1.42 mm (21.76–28.22) for the MYAH. The mean difference in AL was −0.01 ± 0.03 mm between the Pentacam AXL and IOLMaster 700, −0.01 ± 0.01 mm between the Pentacam AXL and MYAH, and 0.01 ± 0.02 mm between the IOLMaster and MYAH. No statistically significant difference was obtained between the devices regarding the AL measurements (p = 0.06). In addition, a significantly strong agreement was determined between the three devices with the ICC and Bland–Altman plots [r = 0.999 (0.999–1.00)] (Table 1) (Fig. 1).
The mean steep K values were 44.45 ± 1.25 D (42.20–46.50 D) for the Pentacam AXL, 44.59 ± 1.23 D (42.23–46.55 D) for the IOLMaster 700, and 44.51 ± 1.24 D (42.27–46.60 D) for the MYAH. The mean difference in steep K was −0.14 ± 0.02 D between the Pentacam AXL and IOLMaster 700, −0.06 ± 0.01 D between the Pentacam AXL and MYAH, and 0.08 ± 0.01 D between the IOLMaster and MYAH. In terms of steep K readings, a significant difference was noted between the devices (p = 0.00). However, a significantly strong agreement was also determined between the three devices with the ICC and Bland–Altman plots [r = 0.985 (0.973–0.992)] (Table 1) (Fig. 2).
The mean flat K values were measured as 43.29 ± 1.28 D (41.10–46.00 D) for the Pentacam AXL, 43.43 ± 1.29 D (41.22–46.23 D) for the IOLMaster 700, and 43.35 ± 1.30 D (41.09–46.07 D) for the MYAH. The mean difference in flat K was −0.14 ± 0.01 D between the Pentacam AXL and IOLMaster 700, −0.06 ± 0.02 D between the Pentacam AXL and MYAH, and 0.08 ± 0.01 D between the IOLMaster and MYAH. In terms of flat K readings, a significant difference was noted between the devices (p = 0.00). However, a significantly strong agreement was also determined between the three devices with the ICC and Bland–Altman plots [r = 0.983 (0.969–0.991)] (Table 1) (Fig. 3).
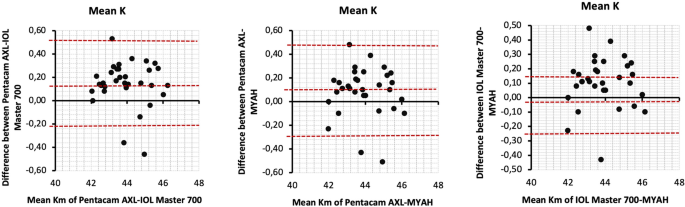
The mean K values were 43.85 ± 1.21 D (42.00–46.20 D) for the Pentacam AXL, 44.00 ± 1.19 D (42.08–46.23 D) for the IOLMaster 700, and 43.94 ± 1.20 D (41.97–46.10 D) for the MYAH. The mean difference in mean K value was −0.15 ± 0.02 D between the Pentacam AXL and IOLMaster 700, −0.09 ± 0.01 D between the Pentacam AXL and MYAH, and 0.06 ± 0.01 D between the IOLMaster and MYAH. A significant difference was noted between the devices regarding mean K readings (p = 0.00). However, a significantly strong agreement was also obtained between the three devices with the ICC and Bland–Altman plots [r = 0.989 (0.981–0.994)] (Table 1) (Fig. 4).
The mean CD values were measured as 11.90 ± 0.34 mm (11.1–12.6 mm) for the Pentacam AXL, 12.11 ± 0.38 mm (11.4 to 12.8 mm) for the IOLMaster 700, and 11.96 ± 0.31 mm (11.2–12.6 mm) for the MYAH. The difference in the mean CD value was −0.21 ± 0.04 mm between the Pentacam AXL and IOLMaster 700, 0.07 ± 0.03 mm between the Pentacam AXL and MYAH, and 0.15 ± 0.07 mm between the IOLMaster and MYAH. In terms of mean CD measurements, a significant difference was noted between the devices (p = 0.00). However, a significantly strong agreement was also determined between the three devices with the ICC and Bland–Altman plots [r = 0.900 (0.830–0.945)] (Table 1) (Fig. 5).
Discussion
In this study, the MYAH device, which has been newly developed mainly for myopic progression, was compared with the Pentacam AXL and IOLMaster 700 devices in terms of the differences and agreements of AL and anterior segment parameters.
Myopia has been a growing public health issue since the onset of the COVID-19 pandemic. High myopia is defined as myopia > −6.0 D and AL ≥ 26 mm [6]. It generally starts in childhood (< 10 years) and progresses rapidly in adolescence [7]. Therefore, identifying the early progression of myopia is of great importance for clinicians to take precautions to halt progression. In 2017, Tideman et al. defined the AL percentile curves used to monitor children with progressive myopia. By comparing the AL of children with that of other children of the same age, clinicians can determine cases that could have abnormal progression even at the time of diagnosis [4].
Several devices on the market have proven themselves for measuring AL. One of the most recent devices is the MYAH. It uses the OLCI principle to measure AL, but the other two devices it was compared to utilize a different principle (Pentacam AXL: PCI, IOLMaster 700: SS-OCT). Knowing whether the measurements made by these devices are comparable and whether they can be used interchangeably in clinical practice is critical for patient follow-up. Although there are studies that have evaluated the differences and consistencies of the measurements of the Pentacam AXL and IOLMaster 700 devices, no previous comparison has been made with the MYAH and other devices. However, as the MYAH employs a similar measurement principle (OLCI) to the Aladdin device manufactured by the same company, studies conducted using the Aladdin device may provide insight on this issue.
In our study, the difference in AL measurements between the three devices was 0.01 mm, which was not statistically significant (p = 0.06). Furthermore, the three devices revealed a high level of agreement. In a previous study by Shajari et al., the difference in AL measurements between the IOLMaster 700 (SS-OCT) and Pentacam AXL (PCI) devices was −0.019 mm, with no statistically significant difference (p = 0.06) [8]. In another study that compared the Aladdin (OLCI) and IOLMaster 500 (PCI) devices, the AL difference was determined as 0.01 mm, which was also not statistically significant (p = 0.07) [9]. In addition, comparable measurements have been determined by the IOLMaster 700 (SS-OCT) and Aladdin (OLCI) devices (AL difference: −0.003, p = 0.648) [10]. In terms of consistency, AL measurements revealed good agreement with the aforementioned devices [8,9,10]. In contrast to these results, several studies have also reported that the AL measurements obtained with these three devices are statistically significantly different. However, the differences still were not clinically significant [11,12,13,14]. Based on these results, it can be said that these devices can be used interchangeably for AL measurement in clinical practice.
In addition to AL, K measurements are required for the diagnosis of and follow-up with myopia. Although a statistically significant but clinically insignificant difference was determined between the K measurements of the three devices (steep K: 0.06–0.14 D, flat K: 0.06–0.14 D, mean K: 0.06–0.15 D), a high level of agreement was obtained between the measurements in our study. In a study, the IOLMaster 700 (SS-OCT) and Pentacam AXL (PCI, Scheimplug camera) devices revealed comparable results for flat K and steep K measurements (a difference in flat K of −0.007 D and steep K of −0.020 D, respectively) [8]. In another study that compared devices working with the OLCI and PCI principles, flat K values were found to be similar (difference: 0.06D), while the steep K (difference: 0.20 D) and mean K (difference: 0.14) values were statistically significantly different [9]. In addition, mean K values (difference: 0.06 and 0.02, respectively) were similar in two other studies conducted with devices operating with the SS-OCT and OLCI principles [10, 15]. However, studies also reported statistically significant K differences [12, 13]. It was known that a 1 D difference in K could result in a 1.40 D difference in IOL power [11, 16]. Additionally, another study stated that devices with a measurement difference of more than 0.14 D of K should not be used interchangeably for IOL power calculation [17]. However, there is no data about the acceptable difference limit of K for using devices interchangeably in myopic progression analysis. The maximum K difference in our study was 0.15 D, and we thought that this measurement difference was not clinically significant enough to affect the follow-up of myopic patients.
Regarding CD measurements, the differences between the devices were statistically significant. However, as for the other measurements, the ICC and Bland–Altman plot analysis showed strong agreement between the measurements. There are few studies in the literature that have compared CD measurements. It was found that the devices using the SS-OCT principle measure the CD larger than the Scheimplug camera does. Therefore, it was advised that they should not be used interchangeably [11, 18, 19]. However, in our study, although the difference in CD between Pentacam AXL and IOLMaster 700 (−0.21 mm) was higher than the others, there was still quite good agreement. In a study that compared PCI and SS-OCT data in myopic young people, the CD measurements were also statistically different [20]. This problem was thought to be caused by the various analysis techniques used to detect the location of the limbus, such as LED sources (IOLMaster 700) or corneal topography (Pentacam AXL, MYAH).
There are several limitations to our study. Firstly, it was conducted retrospectively. Secondly, the sample size was limited, and no follow-up examinations were scheduled. In addition, degenerative myopic patients were not included in the study. Further prospective comparative studies with a larger sample size are required to determine the devices' reliability, particularly in degenerative myopia. Additionally, prospective studies should be conducted to determine the device's efficacy in monitoring myopic progression and functionality of the integrated AL percentile curves.
In conclusion, our study is the first to compare the MYAH device with Pentacam AXL and IOLMaster 700 devices in terms of AL and anterior segment parameters in myopic children. No difference was determined between the MYAH and the other devices regarding AL, which is the most important parameter in the analysis of myopic progression. The high degree of agreement in all parameters demonstrated that MYAH is a reliable instrument. We believe that the MYAH device will be useful for the early diagnosis of children at high risk of developing myopia and monitoring myopic progression during the pandemic era.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Xiang ZY, Zou HD (2020) Recent epidemiology study data of myopia. J Ophthalmol. https://doi.org/10.1155/2020/4395278
Jong M, Sankaridurg P, Naduvilath TJ, Li W, He M (2018) The relationship between progression in axial length/corneal radius of curvature ratio and spherical equivalent refractive error in myopia. Optom Vis Sci 95:921–929. https://doi.org/10.1097/opx.0000000000001281
Kimura S, Hasebe S, Miyata M, Hamasaki I, Ohtsuki H (2007) Axial length measurement using partial coherence interferometry in myopic children: repeatability of the measurement and comparison with refractive components. Jpn J Ophthalmol 51:105–110. https://doi.org/10.1007/s10384-006-0410-5
Tideman JWL, Polling JR, Vingerling JR, Jaddoe VWV, Williams C, Guggenheim JA, Klaver CCW (2018) Axial length growth and the risk of developing myopia in European children. Acta Ophthalmol 96:301–309. https://doi.org/10.1111/aos.13603
Haddad JS, Barnwell E, Rocha KM, Ambrosio R Jr, Waring Iv GO (2020) Comparison of biometry measurements using standard partial coherence interferometry versus new scheimpflug tomography with integrated axial length capability. Clin Ophthalmol 14:353–358. https://doi.org/10.2147/opth.s238112
Tideman JW, Snabel MC, Tedja MS, van Rijn GA, Wong KT, Kuijpers RW, Vingerling JR, Hofman A, Buitendijk GH, Keunen JE, Boon CJ, Geerards AJ, Luyten GP, Verhoeven VJ, Klaver CC (2016) Association of axial length with risk of uncorrectable visual impairment for Europeans With myopia. JAMA Ophthalmol 134:1355–1363. https://doi.org/10.1001/jamaophthalmol.2016.4009
Tideman JWL, Polling JR, Hofman A, Jaddoe VW, Mackenbach JP, Klaver CC (2018) Environmental factors explain socioeconomic prevalence differences in myopia in 6-year-old children. Br J Ophthalmol 102:243–247. https://doi.org/10.1136/bjophthalmol-2017-310292
Shajari M, Cremonese C, Petermann K, Singh P, Müller M, Kohnen T (2017) Comparison of axial length, corneal curvature, and anterior chamber depth measurements of 2 recently introduced devices to a known biometer. Am J Ophthalmol 178:58–64. https://doi.org/10.1016/j.ajo.2017.02.027
Hoffer KJ, Shammas HJ, Savini G, Huang J (2016) Multicenter study of optical low-coherence interferometry and partial-coherence interferometry optical biometers with patients from the United States and China. J Cataract Refract Surg 42:62–67. https://doi.org/10.1016/j.jcrs.2015.07.041
Calvo-Sanz JA, Portero-Benito A, Arias-Puente A (2018) Efficiency and measurements agreement between swept-source OCT and low-coherence interferometry biometry systems. Graefes Arch Clin Exp Ophthalmol 256:559–566. https://doi.org/10.1007/s00417-018-3909-9
Tañá-Rivero P, Aguilar-Córcoles S, Tello-Elordi C, Pastor-Pascual F, Montés-Micó R (2021) Agreement between 2 swept-source OCT biometers and a Scheimpflug partial coherence interferometer. J Cataract Refract Surg 47:488–495. https://doi.org/10.1097/j.jcrs.0000000000000483
Montés-Micó R (2022) Evaluation of 6 biometers based on different optical technologies. J Cataract Refract Surg 48:16–25. https://doi.org/10.1097/j.jcrs.0000000000000690
Sel S, Stange J, Kaiser D, Kiraly L (2017) Repeatability and agreement of Scheimpflug-based and swept-source optical biometry measurements. Cont Lens Anterior Eye 40:318–322. https://doi.org/10.1016/j.clae.2017.03.007
Henriquez MA, Zúñiga R, Camino M, Camargo J, Ruiz-Montenegro K, Izquierdo L Jr (2020) Effectiveness and agreement of 3 optical biometers in measuring axial length in the eyes of patients with mature cataracts. J Cataract Refract Surg 46:1222–1228. https://doi.org/10.1097/j.jcrs.0000000000000237
Hoffer KJ, Hoffmann PC, Savini G (2016) Comparison of a new optical biometer using swept-source optical coherence tomography and a biometer using optical low-coherence reflectometry. J Cataract Refract Surg 42:1165–1172. https://doi.org/10.1016/j.jcrs.2016.07.013
Hua Y, Qiu W, Xiao Q, Wu Q (2018) Precision (repeatability and reproducibility) of ocular parameters obtained by the Tomey OA-2000 biometer compared to the IOLMaster in healthy eyes. PLoS ONE 13:e0193023. https://doi.org/10.1371/journal.pone.0193023
Özyol P, Özyol E (2016) Agreement between swept-source optical biometry and scheimpflug-based topography measurements of anterior segment parameters. Am J Ophthalmol 169:73–78. https://doi.org/10.1016/j.ajo.2016.06.020
Salouti R, Nowroozzadeh MH, Tajbakhsh Z, Bagheri M, Ghoreyshi M, Azizzadeh M, Razeghinejad MR (2017) Agreement of corneal diameter measurements obtained by a swept-source biometer and a scheimpflug-based topographer. Cornea 36:1373–1376. https://doi.org/10.1097/ico.0000000000001300
Tu R, Yu J, Savini G, Ye J, Ning R, Xiong J, Chen S, Huang J (2020) Agreement between two optical biometers based on large coherence length SS-OCT and scheimpflug imaging/partial coherence interferometry. J Refract Surg 36:459–465. https://doi.org/10.3928/1081597x-20200420-02
Shi Q, Wang GY, Cheng YH, Pei C (2021) Comparison of IOL-master 700 and IOL-master 500 biometers in ocular biological parameters of adolescents. Int J Ophthalmol 14:1013–1017. https://doi.org/10.18240/ijo.2021.07.08
Funding
The authors obtained no commercial provider for the investigation, authorship, and broadcasting of the study.
Author information
Authors and Affiliations
Contributions
HS, OT: designed the study; HS, OT: were involved in patient care; OT: collected the data; HS, OT: analysis and interpretation of data; HS, OT: drafting the manuscript; HS, OT: design of the work, revising the work critically for important intellectual content. All authors approved the final version of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no financial conflict of interest related to this article.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of University of Health Sciences, Dıskapı Yıldırım Beyazıt Training and Research Hospital, Ankara, Turkey and with the 1964 Helsinki Declaration and its later amendments or comparable with ethical standards.
Consent for participate and publication
The authors declare that they have participated in this work, and they have reviewed the final version of the work, believe it represents valid work, and approve it for publication.
Informed consent
Written informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sabur, H., Takes, O. Agreement of axial length and anterior segment parameters measured with the MYAH device compared to Pentacam AXL and IOLMaster 700 in myopic children. Int Ophthalmol 43, 475–482 (2023). https://doi.org/10.1007/s10792-022-02444-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02444-w