Paper:
Manipulability Analysis of Anterior and Mediolateral Dynamic Gait Stability of Young and Elderly Individuals
Hiroki Watanabe*, Shogo Okamoto*, Tomohito Kuroda*, and Yasuhiro Akiyama**
*Department of Computer Science, Tokyo Metropolitan University
6-6 Asahigaoka, Hino, Tokyo 191-0065, Japan
**Department of Mechanics and Robotics, Shinshu University
3-15-1 Tokida, Ueda, Nagano 386-8567, Japan
Humans maintain postural stability while walking by modulating their spatiotemporal walking features. It is crucial for humans to be able to restore stability in the event of a transient loss. However, the ease of adjusting postural stability has not yet been investigated extensively. This study applied manipulability, a concept widely used in robotics, to analyze the margin of stability (MoS), a measure of dynamic postural stability. The MoS values along each of the anterior and mediolateral directions were modeled as a function of spatiotemporal gait parameters, and the manipulability of the MoS was computed. We observed differences in manipulability between two age groups (60 healthy elderly adults and 60 healthy young individuals in their 20s) from an open database. The manipulability of the elderly was significantly higher than that of the young, suggesting that the elderly employed walking postures that allowed them to adjust their stability with relative ease. Furthermore, for the young group, the manipulability tended to be low when the mediolateral stability was low, with a correlation coefficient of 0.67. In contrast, the elderly group did not exhibit this relationship, showing differences in walking strategies between young and elderly individuals. The manipulability analysis of dynamic gait stability provides insights into revealing human gait strategies.
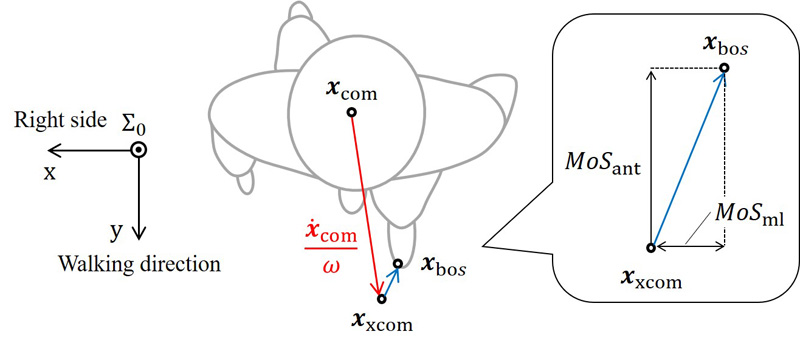
Dynamic gait stability (margin of stability)
- [1] Cabinet Office of Japan, “Annual report on the aging society,” 2022.
- [2] A. M. Sawka, P. Boulos, K. Beattie, L. Thabane, A. Papaioannou, A. Gafni, A. Cranney, N. Zytaruk, D. A. Hanley, and J. D. Adachi, “Do hip protectors decrease the risk of hip fracture in institutional and community-dwelling elderly? A systematic review and meta-analysis of randomized controlled trials,” Osteoporosis Int., Vol.16, pp. 1461-1474, 2005. https://doi.org/10.1007/s00198-005-1932-2
- [3] S. Yahaya, Z. Ripin, and M. Ridzwan, “Test systems for the biomechanical evaluation of hip protectors: A systematic review,” Osteoporosis Int., Vol.31, pp. 43-58, 2020. https://doi.org/10.1007/s00198-019-05128-x
- [4] S. M. Bruijn, O. G. Meijer, P. J. Beek, and J. H. van Dieën, “Assessing the stability of human locomotion: A review of current measures,” J. of the Royal Society Interface, Vol.10, No.83, Article No.20120999, 2013. https://doi.org/10.1098/rsif.2012.0999
- [5] A. L. Hof, M. G. J. Gazendam, and W. W. Sinke, “The condition for dynamic stability,” J. of Biomechanics, Vol.38, No.1, pp. 1-8, 2005. https://doi.org/10.1016/j.jbiomech.2004.03.025
- [6] A. L. Hof, “The ‘extrapolated center of mass’ concept suggests a simple control of balance in walking,” Human Movement Science, Vol.27, No.1, pp. 112-125, 2008. https://doi.org/10.1016/j.humov.2007.08.003
- [7] H. Ohtsu, S. Yoshida, T. Minamisawa, T. Takahashi, S. Yomogida, and H. Kanzaki, “Investigation of balance strategy over gait cycle based on margin of stability,” J. of Biomechanics, Vol.95, Article No.109319, 2019. https://doi.org/10.1016/j.jbiomech.2019.109319
- [8] T. Iwasaki, S. Okamoto, Y. Akiyama, and Y. Yamada, “Gait stability index built by kinematic information consistent with the margin of stability along the mediolateral direction,” IEEE Access, Vol.10, pp. 52832-52839, 2022. https://doi.org/10.1109/ACCESS.2022.3175409
- [9] Y. Akiyama, Y. Fukui, S. Okamoto, and Y. Yamada, “Effects of exoskeletal gait assistance on the recovery motion following tripping,” Plos One, Vol.15, Article No.e0229150, 2020. https://doi.org/10.1371/journal.pone.0229150
- [10] F. Watson, P. C. Fino, M. Thornton, C. Heracleous, R. Loureiro, and J. J. H. Leong, “Use of the margin of stability to quantify stability in pathologic gait – A qualitative systematic review,” BMC Musculoskeletal Disorders, Vol.22, Article No.597, 2021. https://doi.org/10.1186/s12891-021-04466-4
- [11] T. Miyazaki, T. Aoki, J. Aizawa, T. Kawase, M. Sogabe, and K. Kawashima, “Adapting balance training by changing the direction of the tensile load on the lumbar region,” J. Robot. Mechatron., Vol.34, No.6, pp. 1361-1370, 2022. https://doi.org/10.20965/jrm.2022.p1361
- [12] Y. Akiyama, Y. Kuboki, S. Okamoto, and Y. Yamada, “Novel approach to analyze all-round kinematic stability during curving steps,” IEEE Access, Vol.11, pp. 10326-10335, 2023. https://doi.org/10.1109/ACCESS.2023.3240441
- [13] T. Kuroda, S. Okamoto, and Y. Akiyama, “Anterior and mediolateral dynamic gait stabilities attributed to different gait parameters in different age groups,” J. of Biomechanical Science and Engineering, Vol.19, No.1, Article No.23-00183, 2024. https://doi.org/10.1299/jbse.23-00183
- [14] L. Hak, H. Houdijk, P. J. Beek, and J. H. van Dieën, “Steps to take to enhance gait stability: the effect of stride frequency, stride length, and walking speed on local dynamic stability and margins of stability,” Plos One, Vol.8, No.12, Article No.e82842, 2013. https://doi.org/10.1371/journal.pone.0082842
- [15] R. Alamoudi and M. Alamoudi, “Development of linear regression models to estimate the margin of stability based on spatiotemporal gait parameters,” IEEE Access, Vol.8, pp. 19853-19859, 2020. https://doi.org/10.1109/ACCESS.2020.2969294
- [16] S. Sivakumaran, A. Schinkel-Ivy, K. Masani, and A. Mansfield, “Relationship between margin of stability and deviations in spatiotemporal gait features in healthy young adults,” Human Movement Science, Vol.57, pp. 366-373, 2018. https://doi.org/10.1016/j.humov.2017.09.014
- [17] L. Gill, A. H. Huntley, and A. Mansfield, “Does the margin of stability measure predict medio-lateral stability of gait with a constrained-width base of support?,” J. of Biomechanics, Vol.95, Article No.109317, 2019. https://doi.org/10.1016/j.jbiomech.2019.109317
- [18] T. Yamaguchi and K. Masani, “Effects of age on dynamic balance measures and their correlation during walking across the adult lifespan,” Scientific Reports, Vol.12, Article No.14301, 2022. https://doi.org/10.1038/s41598-022-18382-7
- [19] S. Roeles, P. J. Rowe, S. M. Bruijn, C. R. Childs, G. D. Tarfali, F. Steenbrink, and M. Pijnappels, “Gait stability in response to platform, belt, and sensory perturbations in young and older adults,” Medical & Biological Engineering & Computing, Vol.56, pp. 2325-2335, 2018. https://doi.org/10.1007/s11517-018-1855-7
- [20] D. Martelli, F. Aprigliano, P. Tropea, G. Pasquini, S. Micera, and V. Monaco, “Stability against backward balance loss: Age-related modifications following slip-like perturbations of multiple amplitudes,” Gait & Posture, Vol.53, pp. 207-214, 2017. https://doi.org/10.1016/j.gaitpost.2017.02.002
- [21] R. L. Cromwell and R. A. Newton, “Relationship between balance and gait stability in healthy older adults,” J. of Aging and Physical Activity, Vol.12, No.1, pp. 90-100, 2004. https://doi.org/10.1123/japa.12.1.90
- [22] H. L. Rogers, R. L. Cromwell, and J. L. Grady, “Adaptive changes in gait of older and younger adults as responses to challenges to dynamic balance,” J. of Aging and Physical Activity, Vol.16, No.1, pp. 85-96, 2008. https://doi.org/10.1123/japa.16.1.85
- [23] L. Hak, F. J. Hettinga, K. R. Duffy, J. Jackson, G. R. Sandercock, and M. J. Taylor, “The concept of margins of stability can be used to better understand a change in obstacle crossing strategy with an increase in age,” J. of Biomechanics, Vol.84, pp. 147-152, 2019. https://doi.org/10.1016/j.jbiomech.2018.12.037
- [24] S. Park, Y.-M. Ko, and J.-W. Park, “The correlation between dynamic balance measures and stance sub-phase COP displacement time in older adults during obstacle crossing,” J. of Physical Therapy Science, Vol.25, pp. 1193-1196, 2013. https://doi.org/10.1589/jpts.25.1193
- [25] Z. Liu, S. Okamoto, T. Kuroda, and Y. Akiyama, “Estimating the margin of gait stability in healthy elderly using the triaxial kinematic motion of a single body feature,” Applied Sciences, Vol.14, No.7, Article No.3067, 2024. https://doi.org/10.3390/app14073067
- [26] W. S, Erdmann, “Center of mass of the human body helps in analysis of balance and movement,” MOJ Applied Bionics and Biomechanics, Vol.2, pp. 144-148, 2018. https://doi.org/10.15406/mojabb.2018.02.00057
- [27] T. Yoshikawa, “Manipulability of robotic mechanisms,” Int. J. of Robotics Research, Vol.4, No.2, pp. 3-9, 1985. https://doi.org/10.1177/027836498500400201
- [28] J. C. Dean, N. B. Alexander, and A. D. Kuo, “The effect of lateral stabilization on walking in young and old adults,” IEEE Trans. on Biomedical Engineering, Vol.54, No.11, pp. 1919-1926, 2007. https://doi.org/10.1109/tbme.2007.901031
- [29] M. A. Schrager, V. E. Kelly, R. Price, L. Ferrucci, and A. Shumway-Cook, “The effects of age on medio-lateral stability during normal and narrow base walking,” Gait & Posture, Vol.28, No.3, pp. 466-471, 2008. https://doi.org/10.1016/j.gaitpost.2008.02.009
- [30] Y. Hirano, Y. Yamada, Y. Akiyama, H. Nakamura, and Y. Matsui, “Preliminary gait analysis of frail versus older adults,” J. of Physical Therapy Science, Vol.36, No.2, pp. 87-93, 2024. https://doi.org/10.1589/jpts.36.87
- [31] P. Terrier and F. Reynard, “Effect of age on the variability and stability of gait: A cross-sectional treadmill study in healthy individuals between 20 and 69 years of age,” Gait & Posture, Vol.41, No.1, pp. 170-174, 2015. https://doi.org/10.1016/j.gaitpost.2014.09.024
- [32] Balance Project, “Balance augmentation in locomotion through anticipative, natural, and Cooperative control of exoskeletons: Report of BALANCE-Deliverable 3.1-Stability index,” Fundacion Tecnalia Research Innovation, 2014.
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.