Abstract
Free full text

Erasing stigmas through storytelling: why interactive storytelling environments could reduce health-related stigmas
Abstract
In this article we describe how designers can apply storytelling to reduce health-related stigmas. Stigma is a pervasive problem for people with illnesses, such as obesity, and it can persistently hinder coping, treatment, recovery, and prevention. Reducing health-related stigma is complex because it is multi-layered and self-perpetuating, leading to intertwined vicious circles. Interactive storytelling environments can break these vicious circles by delimiting the narrative freedom of stigma actors. We theoretically explain the potential of interactive storytelling environments to reduce stigma through the following seven functions: 1) expose participants to other perspectives, 2) provide a protective frame, 3) intervene in daily conversations, 4) persuade all stigma actors, 5) exchange alternative understandings, 6) elicit understanding and support for stigma victims, and 7) support stigma victims to cope with stigmatization. We elaborate on these functions through a demonstration of an interactive storytelling environment against weight stigma. In conclusion, this article is a call on designers for health and wellbeing, scientists, and practitioners from various disciplines to be sensitive to the pervasiveness of stigma and to collaboratively create destigmatizing storytelling environments.
Introduction
Stigma is a pervasive problem for people with illnesses (Weiss, Ramakrishna, and Somma 2006), such as HIV/AIDS, skin diseases, depression, and obesity. Victims of health-related stigmatization give testimonies of feeling and being bullied, secluded, and violated. As a result, they continuously feel pressure to act normal, make a good impression, and provide explanations for supposed shortcomings (Goffman 1963). This places a huge burden on people and it can lead to negative physical and psychological health outcomes (Pachankis 2007). At the same time, perpetrators of stigmatization are often not fully aware of their stigmatizing behaviour and its negative effects. They ‘just want the best for someone’, make assumptions about someone’s condition, and are sometimes just ill-informed about a disease.
Health-related stigmatization is a complex phenomenon involving many actors, motivations, and effects that negatively impact the health of stigma victims (Quinn and Chaudoir 2009; Van Beugen et al. 2017). Health-related stigma not only manifests itself in interpersonal interaction. It also manifests itself internally (intrapersonal) and structurally. Stigmatized individuals themselves often internalize parts of the biases and stereotypes leading to self-stigma (Richman and Lattanner 2014). Structural health-related stigma can be found in health insurance policies that exclude certain illnesses, reduced chances on the labour market, and health inequalities among populations (Hatzenbuehler 2016). Hence, health-related stigma can persistently manifest itself in nearly all facets of people’s lives and this negatively influences the health of stigma victims and can lead to health inequalities (Pascoe and Smart Richman 2009; Paradies, Luiz Bastos, and Priest 2016). Some argue that stigma also serves a purpose as a motivator for healthy behaviour change (Bayer 2008), yet health-related stigma does more harm than good and should thus be reduced.
Unfortunately, reducing health-related stigma is a complicated endeavour. Stigmas are generally very persistent because motivations to stigmatize are often deeply ingrained in people’s norms and beliefs, and in societal structures (Scambler 2009). The multifaceted and multi-layered nature of stigmatization (e.g. labelling, distancing, discriminating on an intrapersonal, interpersonal, structural level) makes a centralized top-down approach, such as advertisement campaigns, ineffective in the long term (Link and Phelan 2001). Additionally, stigma is often subject to psychological mechanisms that perpetuate stigmatizing attitudes and behaviours (Brewis 2014).
We propose storytelling to be a driving force against stigmatization because, on a structural level, health-related stigmas can be characterized as a cultural web of narratives (Meretoja 2017) and master narratives have been widely used to uncover societal oppressive structures against marginalized communities (Syed 2015). Moreover, on the intrapersonal level, narratives are strongly related to personal identity formation by which individuals position themselves in conversations (Bamberg 2011).
Rather than intervening on single narratives, as in conventional campaigns against stigma, we suggest targeting the exchange of narratives, i.e. the storytelling. Stigma actors may be invited to create and feel part of destigmatizing stories by safe and unprejudiced social environments with confined degrees of freedom in telling stories and interacting with them. As visualized in Figure 1, ‘interactive storytelling environments’ with a designed conceptual storytelling space, i.e. the set of all possible stories that participants can tell, may provoke stigma perpetrators and stigma victims to 1) appropriate their stories for the other group, 2) reflect on one’s own stories, and 3) adapt one’s stories in collaboration with the other group.
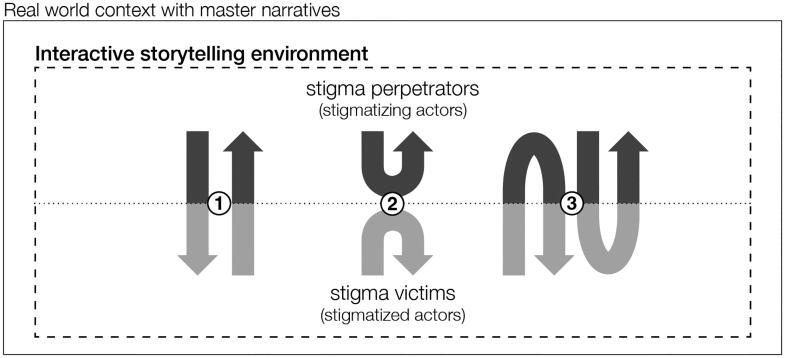
We propose to design interactive storytelling environment that shape the conceptual storytelling space of stigma actors to motivate them to 1) appropriate, 2) reflect on, and 3) co-create their stories.
In this article, we explore the potential of designing interactive storytelling environments to reduce health-related stigmatization by identifying destigmatizing functions of story content and story interactions and applying them to an intervention. In the first half of the article, we review the literature on stigma, with weight stigma as an exemplary case, to better understand its pervasive and self-perpetuating nature. In the second half of the article, we define a research agenda about designing destigmatizing functions of storytelling and describe a serious game against weight stigma to demonstrate the destigmatizing potential of interactive storytelling environments.
Stigma as a psychosocial phenomenon
Stigma is a visible or invisible mark of disapproval, allowing ‘insiders’ to identify and disassociate from ‘outsiders’ (Falk 2001). Goffman (1963) describes the day-to-day experiences of outsiders as ‘managing impressions’ and ‘managing information’. For example, people that are stigmatized by their body size particularly recall managing impressions, such as making sure to dress nicely and not eating in public (Lewis et al. 2011). Link and Phelan (2001) define stigma as a co-occurrence of labelling, stereotyping, separating, status loss, and discrimination in a power situation that allows these processes to unfold. The power difference between a stigmatized group and the group that stigmatizes is important to point out, because stigmas are persistent when they exist within groups that have the power to find new strategies to maintain the disadvantageous status of the stigmatized group. As long as motivations for stigmatization prevail in dominant groups, combatting mediating processes is ineffective (Hatzenbuehler, Phelan, and Link 2013).
Stigmatization should be reviewed on an intrapersonal, interpersonal, and structural level to fully understand it (Cook et al. 2014). Health-related stigma that manifests itself in interpersonal interaction is often easy to identify, such as bullying, negative commenting, or excluding (Hebl and Dovidio 2005). Yet for people with a chronic illness, intrapersonal or self-stigma is particularly salient (Durso and Latner 2008; Kranke et al. 2011). They often go through a process of understanding the causes of their illness and thus regularly fail in their attempts to recover or manage it. This can lead to reduced self-esteem and self-worth and in effect self-stigma in the form of inhibiting or isolating oneself (Corrigan, Larson, and Rüsch 2009).
Structural stigmatization can be found in socioeconomic conditions, cultural norms, and institutional policies (e.g. Hatzenbuehler and Link 2014). For example, people with obesity have on average lower incomes (Giskes et al. 2010) and weight loss services are often not reimbursed by the health insurance (Puhl and Heuer 2009). Stangl et al. (2019) explain that such structural discrimination on health conditions can be found in organizations, communities, and public spaces. Thus, in this article, ‘stigma actor’ refers to people that are the victim or perpetrator of stigmatization as well as non-human actors through which health-related stigmas are expressed, such as health insurance systems, cultural master narratives, and the media. Moreover, our use of ‘victim’ or ‘perpetrator’ in this article refers to the role of a stigma actor in a particular stigmatizing situation, rather than being or feeling a victim or perpetrator in general.
To get a more concrete understanding of the multiple levels and actors of health-related stigma, we dive deeper into the manifestations, causes, and effects of weight stigma. Weight stigma is a valuable case because many recent studies show direct negative health consequences of stigmatization, yet means to reduce weight stigma are scarce (Pearl 2018). Such a comprehensive understanding of health-related stigmas allows us to define mechanisms that could erase it.
Weight stigma
People with obesity are stigmatized in many ways and settings. They are called ‘lazy, unmotivated, lacking in self-discipline, less competent, non-compliant, and sloppy’ (Puhl and Heuer 2009, 941) in employment, healthcare, education, interpersonal relationships, and media settings. As obesity is visible, these stereotypes easily lead to separation and discrimination in the form of gazing, others making decisions for you, negative comments, being ignored or rejected, and bullying or even physical violation (De Brún et al. 2014; Lewis et al. 2011). Next to labelling by others, many people with obesity have the same anti-fat attitudes as slender people (Crandall 1994). This self-stigma is expressed in the form of a negative body image (Harriger and Thompson 2012), feeling guilty or weak (Lillis et al. 2010), distancing from others that have obesity (Durso and Latner 2008), and reduced motivation in weight loss efforts (Corrigan, Larson, and Rüsch 2009; Hunger et al. 2015).
Losing weight is complex due to the wide variety of causes for weight gain. To some extent, it is caused by unhealthy nutrition and too little physical activity, yet a substantial part of the variation in body weight is determined by other determinants, such as genetic composition and reduced access to healthy food (Kolata 2007; Vandenbroeck, Goossens, and Clemens 2010). Moreover, there are many cultural and psychosocial factors that contribute to obesity, such as role models (Lau, Lee, and Ransdell 2007), body image preferences (Becker et al. 1999), preoccupation with dieting (Bacon and Aphramor 2011), stress (Tomiyama 2014), and depression (Milaneschi et al. 2019). Also somatic causes may play a role, e.g. hormonal causes, medication with weight gaining side-effects and many other factors (van der Valk et al. 2019).
On a societal level, people with obesity are generally personally blamed for their weight (Saguy and Gruys 2010). This is often based on the false assumption that personal factors such as a sedentary lifestyle, poor eating behaviours, and psychological problems are the only causes of obesity (Puhl et al. 2015). Moreover, it is often thought that losing weight is easy, whereas compelling evidence exists that mechanisms in the body and brain counteract weight loss when a person developed obesity (Pucci and Batterham 2020). This leads to structural discrimination in practices such as not fitting in seats or clothing (Brewis et al. 2017), negative media portrayals (Heuer, McClure, and Puhl 2011), lower job opportunities (Brewis 2014; Puhl and Heuer 2010), insurances not covering weight loss treatments, and absence of anti-stigma legislation (Pearl 2018).
Thus, living with obesity and dealing with the accompanying stigma can negatively interfere with nearly all facets of people’s lives, in particular, in cultural contexts where a slender body is encouraged in many forms, e.g. social media, fashion, education. This example of weight stigma highlights the pervasive nature of health-related stigma.
Vicious circles of health-related stigma
We dive deeper into the reasons why health-related stigma is so pervasive to arrive at recommendations for sustainable stigma reduction. One explanation are the persistent motivations to stigmatize. Phelan, Link, and Dovidio (2008) describe three generic motivations to stigmatize: 1) exploitation, 2) enforcement of social norms and 3) avoidance of disease. The above-described manifestations of health-related stigma and weight stigma mainly provide evidence for norm enforcement and disease avoidance. Monaghan (2017) suggests that personally blaming people for obesity is rarely challenged due to a predominant ideology of personal responsibility, marketization and rolling back of the welfare state. This fits in a broader practice of stigmatizing people that burden the healthcare system and holding them personally accountable for this burden (Brelet et al. 2021).
Next to attributing chronic illnesses to personal responsibility, other motivations to stigmatize are cultural norms of physical attractiveness and pathogen avoidance. In many cultures there is a preference for thinness (Crandall 1994) and concerns of contagion may arise due to the widespread knowledge of health problems associated with certain chronic illnesses (Pearl 2018). Consequently, self-stigma may arise because the overall norms of being healthy may be stronger than self-interest. Moreover, people with a chronic illness often protect their self-image by distancing themselves from the negative label (De Brún et al. 2014), viewing their illness as a temporary condition (Durso and Latner 2008), and not identifying with others that are ill (Tomiyama et al. 2015). As a result, the stigma prevails because it is not challenged by anyone.
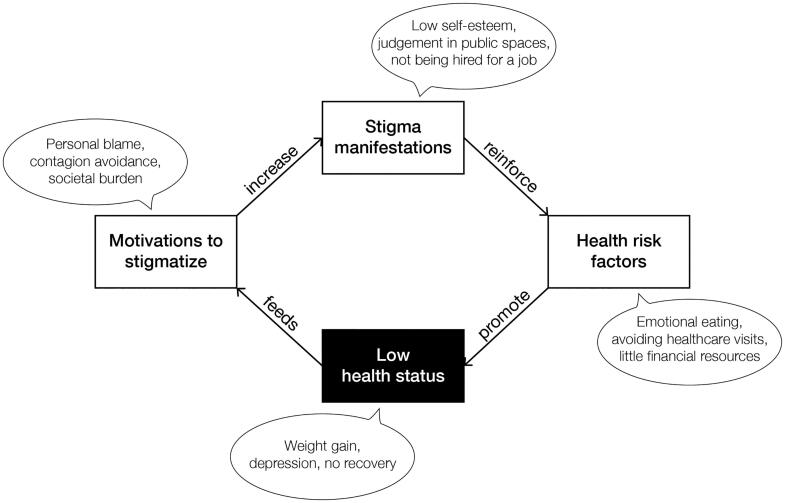
Health-related stigma is also pervasive because it can cause health disparities and vice versa (Hatzenbuehler, Phelan, and Link 2013), leading to a self-perpetuating cycle (see Figure 2). For example, stigmatization seems one of the causes for weight gain and a barrier for weight loss due to its negative social and psychological effects (Papadopoulos and Brennan 2015; Puhl and Suh 2015). If a person with obesity encounters stigma, they may start to feel more alone and isolated. This may cause depression and stress, and depression and stress cause negative health outcomes, such as weight gain (Jackson and Steptoe 2018; Tomiyama 2014). As a result, stigmatization can lead to a negative loop in which causes and effects of weight gain get intertwined.
A vicious circle of health-related stigma starts when the effects of stigmatization negatively influence the victim’s physical or psychological health, and when the worsened health condition feeds motivations to stigmatize. Such vicious circles can be identified in intrapersonal, interpersonal, and structural stigmatization and are interlinked, as visualized in Figure 3. For example, on an intrapersonal level, self-stigma makes people adopt maladaptive coping strategies, such as avoiding stigmatizing situations (Hayward, Vartanian, and Pinkus 2018). This includes avoiding exercising with others (Hunger et al. 2015), which negatively impacts a person’s health. In combination with structural stigmatization, such as negative media portrayals, and interpersonal stigmatization, such as colleagues making remarks, this can lead to lower self-esteem and lower self-efficacy and consequently, people may become less motivated to achieve life goals in general (Corrigan, Larson, and Rüsch 2009). As a result, this reinforces norms and beliefs that stigma victims lack willpower or are lazy, thereby feeding motivations to stigmatize.

People with chronic illnesses can experience interrelated vicious circles of health-related stigma on three levels. Examples of human and non-human actors are visible on the right.
In this way, causes and effects of stigmatization can initiate a vicious circle on one level, triggering new vicious circles on other levels. In the reviewed literature on weight stigma we found vicious circles as a result of failure and success stories of treatment (Bacon and Aphramor 2011), stereotype anxiety and social consensus (Pearl 2018), changes in social network and reduced social support (Brewis 2014), no in-group favouritism (Tomiyama et al. 2015), stress and depression (Tomiyama 2014), low socioeconomic position (Hulshof et al. 2003), and stigmas on other traits (Lewis and van Puymbroeck 2008). This multitude of stigma drivers not only increases the pervasiveness of a health-related stigma but also makes it very persistent and increasingly challenging to deal with for stigma victims.
In conclusion, health-related stigma is a psychosocial phenomenon from which chronically ill individuals can hardly escape, as illustrated in Figure 3. The stigma often manifests itself on so many different levels with different actors that it maintains itself. Inspired by advancements in speculative design (Dunne and Raby 2013) and design fiction (Bleecker 2009), we think that design can play a role in stopping health-related stigmas from perpetuating themselves. In the following section, we argue for an approach in how to achieve this.
Towards designing destigmatizing storytelling environments
Effectively tackling health-related stigma is difficult, as it is often very subtle and difficult to grasp (Cook et al. 2014). For example, Lupton (2018) argues that referring to obesity as an epidemic in itself is not stigmatizing, yet it does render large bodies susceptible for medical labelling. Due to the subtle nature of stigma, public health interventions sometimes even perpetuate it, because they fail to acknowledge that biases are a manifestation of social inequity (Alberga et al. 2016) or because the personal blame argument prevails throughout campaigns and policy (Lewis et al. 2011; de Boer and Lemke 2021).
To bring stigma perpetuation to a halt we suggest to redesign the social environments in which stigmatic interaction takes place, rather than contending against individual stigmatizing narratives or narrators. We can directly or indirectly influence the storytelling in these environments by creating an atmosphere or learning environment that makes participants feel safe, non-judgemental, and open to other perspectives. Within such a safe space, interactive narrative mechanics such as role playing and decision-making can provoke participants to interact with each other in a destigmatizing way. Such mechanics may support them to collaboratively determine the course of unfolding stories, change stories that already exist, or add new stories.
More specifically, designers can influence stigmatic storytelling or stimulate stigma-reducing storytelling by designing 1) the properties of a storytelling environment (e.g. Vaes et al. 2012) and 2) the rules that guide the storytelling interaction in an environment (e.g. Vegt et al. 2016). The first design strategy aims to influence participants’ storytelling through framing, i.e. ‘to select aspects of a perceived reality and make them more salient’ (Entman 1993, 52). For example, stories about obesity in the media were often accompanied by an image of a person with a large body with their head cut off (Heuer, McClure, and Puhl 2011). Image banks now provide images of people with large bodies in active and participating situations to foster recognition in stories about obesity. The second design strategy aims to evoke and steer storytelling by designing constraints and perceived affordances (Norman 1999). For example, predefined story elements and a stage and audience may guide participants towards desired or relevant storytelling.
Narrative freedom as a persuasive dimension in storytelling environments
When creating or shaping the storytelling environment to reduce health-related stigma, ethical questions appear in relation to the narrative agency of participants (Meretoja 2017): which stories should dominate and who should get a voice in discourses where stigmas prevail? The answers to these questions vary over place and time. Hence, the participants in a storytelling environment end up continuously negotiating between values (Korthals Altes 2014).
A storytelling environment influences this value negotiation by setting the narrative freedom that participants have, i.e. to tell their stories in the way they want constraint by all possible stories that the environment allows. For example, a frame narrative that explicitly introduces the role of stigma perpetrator and stigma victim stimulates participants to adopt these two perspectives and interact accordingly. Moreover, narrative freedom arises from resources in the environment to tell stories and to be heard (Zussman 2012). For example, the audience that encourages someone to tell one’s story compromises narrative freedom through their consent, attention, agreement, involvement, and expertise (Pasupathi and Billitteri 2015). In a Black Lives Matter rally, for example, protesters tell other stories than when they sit around the dinner table with their families.
Another strategy of setting narrative freedom is to confine the degrees of freedom participants have in interacting in a storytelling environment. The field of interactive digital narrative has explored various ways to interact within a narrative (e.g. Koenitz 2023), thereby varying the distribution of narrative agency between a narrator and its audience. We can apply such interactive narrative design heuristics on the broader storytelling environment level. Such interventions would than lead to interactive storytelling environments in which participants have a designated freedom to create, present, reflect on, and feel part of stories. Participants may, for example, build on each other’s stories or adapt their own story after hearing someone else’s story.
In relation to stigmatization, balancing this narrative freedom is crucial from an ethical as well as utilitarian point of view. Storytellers need to have a certain degree of narrative freedom to become engaged in telling their story, yet within boundaries that foster stigma reduction. Too low narrative freedom might not trigger enough interaction between stigma actors. Too high narrative freedom might only amplify the status-quo in stigma manifestations, motivations, and health effects.
Reducing health-related stigmas through storytelling
Based on our model of stigma perpetuation (Figure 2), we identify three mechanisms that can break the vicious circle (as depicted in Figure 4). The first two mechanisms are to diminish stigma manifestations (mechanism 1) and deconstruct motivations to stigmatize (mechanism 2). This is supported by the claim of Link and Phelan (2001) that stigma can only be effectively reduced when the power of stigmatizing groups gets limited and when fundamental motivations to stigmatize (i.e. domination, norm enforcement, disease avoidance) are taken away. Richman and Lattanner (2014) add that stigma victims become empowered by promoting personal agency and control over the stigma. This supports the third mechanism of supporting stigma victims in dealing with stigmatizing situations to stop the reinforcement of health risk factors.

Three mechanisms to break the vicious circle in the health-related stigma perpetuation model. 1) Diminish stigma manifestations (press machine). 2) Deconstruct motivations (chisel and hammer). 3) deal with stigmatization (scissors).
These stigma-reducing mechanisms may be well understood from a narrative perspective, as health-related stigma can be characterized as a complicated network of narratives that interact with each other and that perpetuate the stigma, as visualized in Figure 3. Storytelling may provide a way to intervene in this stigmatic narrative network by conveying new experiences, persuading the stigma actors, and exploring alternative perspectives (Meretoja 2017). To come to a more structured understanding of the potential destigmatizing functions of storytelling, we make a distinction between story content and story interaction. In the following sections, we further detail the potential functions of story content and story interactions in relation to the three mechanisms that could stop stigma perpetuation (see Table 1). In this way, we aim to describe a detailed research agenda regarding the destigmatizing potential of interactive storytelling environments.
Table 1.
Seven potential functions of story content and story interactions in three basic stigma-reducing mechanisms.
| Stigma-reducing mechanisms | Potential functions of story content | Potential functions of story interactions |
|---|---|---|
| Diminish manifestations | 1) Expose victims and perpetrators to other perspectives | 2) Provide a protective frame and 3) intervene in daily conversations |
| Deconstruct motivations | 4) Reach stigma actors with persuasive messages | 5) Exchange alternative understandings |
| Deal with stigmatization | 6) Elicit understanding and support for stigma victims | 7) Support stigma coping by stigma victims |
Diminish stigma manifestations
Interventions that aim to directly reduce health-related stigmatization, such as reducing bullying at schools, are often based on inducing empathy (Knaak, Modgill, and Patten 2014). For example, by explaining the difficulty of losing weight through first-person narratives (Teachman et al. 2003) and role-playing exercises (Wiese et al. 1992).
1. Expose to other perspectives – A basic precondition of reducing stigma through empathy is the availability of stories from different perspectives. Carefully distributing and defining these perspectives in a storytelling environment is important. With a clear presentation of scenes through the selection or restriction of narrative information (Gérard 1980), stories can be used to make stigma perpetrators experience the perspective of stigma victims and vice versa. Furthermore, the story medium should be chosen carefully to reach an audience with other perspectives. Davidson et al. (2018), for example, successfully reached the general public by publishing online video testimonies about mental illness among veterans and firefighters. When designing an interactive storytelling environment, it is thus advisable to already collect stories from varying perspectives and use those as prompts for destigmatizing discussions. Role playing and role shifting could be additional interactive narrative mechanisms that support participants in experiencing other perspectives.
2. Provide a protective frame – A protective frame of fiction is assumed to evoke empathic responses (Keen 2006; Kidd and Castano 2013). No conclusive evidence exists regarding the empathy-inducing effect of fictionality (Braddock and Dillard 2016). Yet, Carey et al. (2020) show that using a shared fiction does relieve participants to disclose very personal experiences and establish shared understandings of stigmatizing situations.
This effect is similar to what happens in gaming experiences. As described by Visch et al. (2013), gaming temporarily moves people’s attention away from their daily life. This mental transportation can lead to a psychological protective frame in which participants become more playful (Apter 1993) and feel stronger engagement, immersion, and emotional presence (Roth, Vorderer, and Klimmt 2009). If an interactive storytelling environment affords confidentiality or feels like a game in which exploration is allowed, stigma perpetrators may adopt a more open attitude towards their own stigmatizing behaviours. Additionally, such a protective frame may evoke a safer feeling among stigma victims to disclose personal stigmatic experiences.
3. Intervene in daily conversations – In daily conversations, stigma expressions could reduce by becoming aware of the underlying master narratives. Master narratives are ‘culturally shared stories that guide thoughts, beliefs, values, and behaviours’ (McLean and Syed 2015). This awareness may trigger or teach participants to counter stigmatic master narratives (Bamberg and Andrews 2004). An example of triggering counter narratives is the reframing of texts, such as ‘living with excess weight is not a sin, it is a quest’ (Vyncke and Van Gorp 2020). Participants can be triggered to counter stigmatic stories directly by providing them with ‘narrative ammunition’. For example, the labels imposed upon stigma victims, such as healthy and sick, almost never reflect reality. Being aware of such binary oppositions and normative choice of words and critiquing them (Derrida 1972) may support counter narratives in daily conversations. An interactive storytelling environment could provide triggers to reflect during conversations. Such ‘small story’ interventions not only affect the direct conversation but also enhance people’s reflexivity in general (Georgakopoulou 2015).
Another method that may fuel subversiveness towards stigmas is to recognize what is not being said (cf. Barthes and Duisit 1975). Health-related stigma is often felt the most when implicitly communicated, thus being able to recognize implicit messages in conversations may help in countering stigmatic narratives. Irigaray (1985) provides an example of deploying stories as enacted, as opposed to stories being told. For example, if women are viewed as illogical, they should speak logically about this view, thereby enacting the counter-narrative. Although critiqued for its relatively aggressive approach (Kozel 1996), an interactive storytelling environment could support stigma victims in enacting counter stories through, for example, theatrical props.
Deconstruct motivations to stigmatize
The mechanism of deconstructing stigma motivations entails changes in stigmatic beliefs, attitudes, and intentions, such as the idea that an illness is fully controllable by the individual that is ill. Motivations behind obesity stigma, for example, may be altered through stories about multiple factors, not only lifestyle, that lead to weight gain. Destigmatizing education of healthcare practitioners is mainly aimed at altering motivations (Knaak, Modgill, and Patten 2014), such as stories about the noncontrollable causes of an illness (e.g. Puhl, Schwartz, and Brownell 2005) and the causes and effects of health-related stigma itself (e.g. Hague and White 2005).
4. Persuade stigma actors – The persuasive strength of such stories is key to alter motivations to stigmatize (De Graaf, Sanders, and Hoeken 2016). Van Laer et al. (2013) describe that the persuasiveness of stories depends on narrative transportation, i.e. experiencing story events through feeling the emotions of a story character and vivid images of the story plot. Hence, a persuasive storytelling environment should enable participants to identify with story characters (e.g. Winskell, Sabben, and Obong’o 2019) and easily imaginable events, such as anecdotes and daily life situations (Boeijinga, Hoeken, and Sanders 2017) in familiar cultural contexts (Larkey and Hecht 2010). Another characteristic of narrative persuasion is that it predominantly has story-consistent effects (Braddock and Dillard 2016). Thus embedding destigmatizing messages and showing destigmatizing behaviour in a story is more likely to reduce stigma than showing stigmatic behaviour or literally stating the message of a story (Shen, Sheer, and Li 2015).
5. Exchange alternative understandings – Next to persuasive stories, we suggest feeding storytelling environments with alternative understandings. This proposal builds on social consensus mechanisms that have been studied as a destigmatizing intervention. Puhl, Schwartz, and Brownell (2005) demonstrated that stigmatic attitudes of undergraduate students diminished when being exposed to positive attitudes of peers. Another strategy to evoke alternative views in storytelling environments is to value disagreement and pluralism, i.e. to adopt an agnostic approach (Mouffe 1999). Accordingly, variation in stories should be the denominator for distributing storytelling resources, rather than supporting every storyteller equally. Moreover, the content and message of a story should not be judged but responded to with other stories. As a result, participants in storytelling environments ideally alternate between storyteller and listener roles (cf. Hammond, Pain, and Smith 2007). Still, stigmatic stories may be adopted as easily as destigmatizing stories (Cavazza et al. 2015). Hence, in addition to agnostic resource distribution, storytelling environments should actively promote destigmatizing storytelling or penalize stigmatic stories.
Deal with stigmatization
The mechanism of dealing with stigmatization builds on literature describing how, predominantly female, stigma victims themselves develop their ways of dealing or coping with health-related stigma. First of all, ways to deal with self-stigma come down to maintaining or fostering self-esteem and self-worth, such as depersonalizing the stigma (Bombak and Monaghan 2017), finding social support (Chou, Prestin, and Kunath 2014), focus on body functionality (Alleva et al. 2015), and positive self-talk, self-love, and self-acceptance (Myers and Rosen 1999). Other examples of coping strategies for stigma victims are fighting back, rationalizing the stigmatizing behaviour as a flaw from the perpetrator, feeling competent regarding the illness, refusing to hide the illness and ignoring the stigmatizing situation (Myers and Rosen 1999; Lewis et al. 2011; van Amsterdam and van Eck 2019; Lu et al. 2003). These activities can all be supported with storytelling.
6. Elicit understanding and support - Ziebland and Wyke (2012) suggest that stigma mainly reduces by learning from experiences from others. Moreover, tailoring stories to stigma victims and adopting diversity values are assumed to have an empowering effect (Reid et al. 2014). At the same time stories should address the perspective of stigma perpetrators to exert attitudinal and behavioural change (Larkey and Hecht 2010). Consequently, there is a duality between empowering stigma victims and persuading stigma perpetrators.
Explicating the roles of victim and perpetrator in a storytelling environment may solve this duality. Bruneau and Saxe (2012) show that a positive attitude change happens when members of a low power group tell their perspective to members of a powerful group. Additionally, powerful group members show positive attitude changes towards the low power group after summarizing what they have heard. Hence, explicitly assigning stigma victims as storyteller and perpetrators as listener elicits understanding and support for both sides. Consequently, learning to tell the story helps to deal with stigmatization. Being able to align one’s story with other narratives and thus telling one’s experiences appropriately helps to elicit understanding and support from others.
7. Support stigma coping – The process of constructing a coherent story may support stigma coping as well. Storytelling with others can help in making sense of what has happened, thereby supporting the reflective process of dealing with stigmatizing situations (Lely et al. 2019). On an intrapersonal level, co-created stories may benefit education, counselling, expressive writing, belonging, and values affirmation (Cook et al. 2014). On an interpersonal level, collaborative storytelling could enhance coping in therapy group sessions, patient-physician interactions, parent-child dialogue, and peer support groups (Winskell, Sabben, and Obong’o 2019). Collaborative storytelling could support stigma coping on a structural level by initiating policy and design changes, and by providing role models (Gomillion and Giuliano 2011).
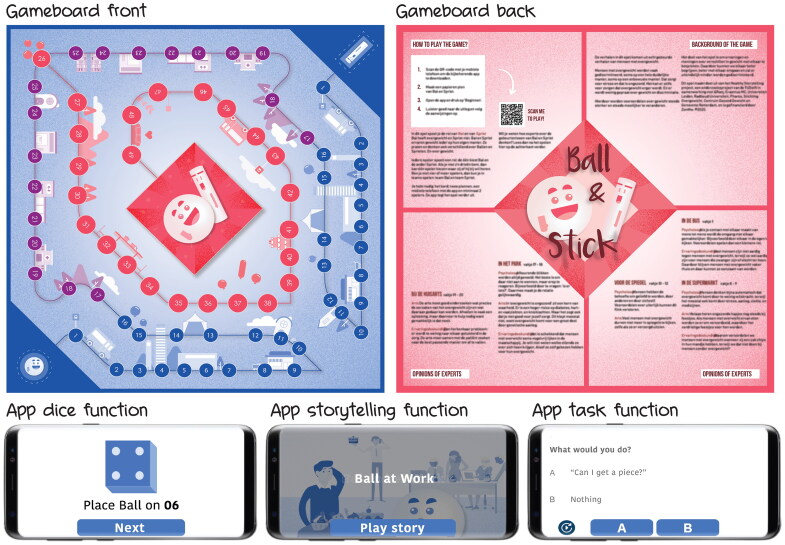
Demonstration of an interactive storytelling environment that reduces weight stigma
To break the vicious circles of health-related stigma, interactive storytelling environments ideally deploy all above-described destigmatizing functions of storytelling. As shown in Figure 5, storytelling environments should 1) expose stigma victims and perpetrators to other perspectives, 2) provide a protective frame, 3) intervene in daily conversations, 4) persuade all stigma actors, 5) exchange alternative understandings, 6) elicit understanding and support for stigma victims, and 7) support stigma victims to cope with stigmatization. In this section we give an example of an interactive storytelling environment against obesity stigma: the game of Ball & Stick. It is not meant as a full case study, but to demonstrate how the above-described theory could be applied (Figure 6).
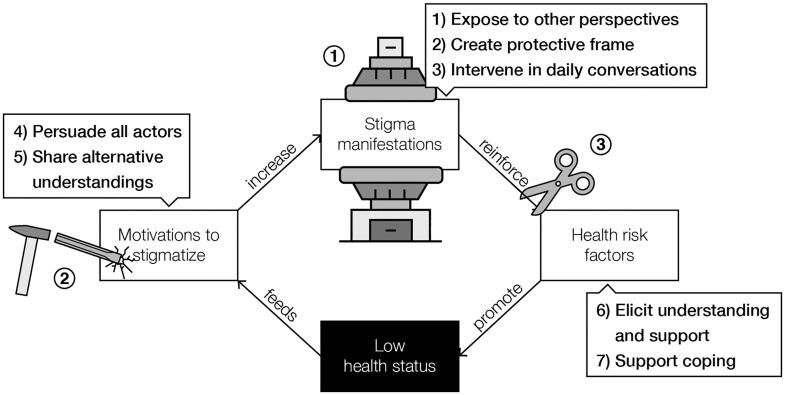
Seven functions of interactive storytelling environments intervening on three mechanisms in the self-perpetuation of stigma.
Ball & Stick
Ball & Stick is a game for community centres with the purpose of reducing the stigmatization of people with obesity. Ideally, it is played with four participants. The game consists of a gameboard, two pawns, and a mobile application that verbally guides players through the game with a virtual dice, narrated stories, and discussion tasks (see Appendix for a detailed content description). The story in the game revolves around two abstractly visualized characters (function 2) represented by two pawns: Ball – a stigma victim, and Stick – a stigma perpetrator. Participants choose which role they want to play. During the game, the players are confronted with stigmatizing situations that people with obesity encounter (function 1). The game facilitates a careful build-up of the discussion between the players through increasing narrative freedom by first choosing between response options, then generating a personal response, and finally jointly agreeing on a response. This varying narrative freedom guides the players in stepwise formulating their thoughts (function 5).
All in-game events are based on conversations with community centre visitors, people with obesity, and obesity specialists. In this way, the events in the game are familiar and easily imaginable (function 4). Additionally, narrative transportation is eased through the common overall narrative of a love story and the game rules were as simple as game of goose. The in-game stigmatic situations were based on regular daily life events, including commonly occurring conversations (function 3). The collected real stories are all from the stigma victim perspective so that the game basically serves as a message from stigma victims to stigma perpetrators (function 6). To allow for coping, next to raising awareness, the back of the gameboard features expert interpretations of several events in the game (function 7). Moreover, the closing narration in the app explicitly states the coping strategy of talking to each other about obesity stigma.
We evaluated the Ball & Stick game with 22 visitors of two community centres (age: 60 (43-83), female: 15) in low-income neighbourhoods of two Dutch cities. We targeted the game to middle aged people with a low income because low socio-economic position is significantly related to obesity prevalence and obesity often develops when people finish their working life (Robroek et al. 2015). Five groups of four players and one group of two played the game in a meeting room at the two community centres. Fourteen of the twenty-two participants lived in neighbourhoods that are within the 10% poorest neighbourhoods in the Netherlands and approximately half of the group had overweight (based on observation).
After a short introduction and giving informed consent the game session started. The two present researchers gave no instructions, as the game was designed to be standalone. Researchers would only intervene in case of a technical malfunction and occasionally encouraged participants to speak more clearly. After playing the game, the players started a discussion, sometimes directly triggered by the game. After their first reactions, the participants were asked to fill in a questionnaire and the researchers initiated a group discussion about the usability, experience, and effect of the game.
Nearly all participants reported a positive engaging experience. Many indicated that the events in the game were familiar to them and that the game raised their awareness. For sixteen participants the game made it easier to talk about obesity and twelve said that it changed their attitude towards people with obesity.
A significant effect of the game was the self-initiated discussion among participants after gameplay. Several groups discussed causes and solutions for discrimination, obesity, and healthy eating. Personal stories about racism, burnout, and depression, suggest that the game created an open atmosphere between the players in which varying beliefs and perspectives in relation to obesity stigma were exchanged. Many participants recognized events from their own experience and explicitly shared their personal beliefs, that were sometimes challenged by others. Moreover, participants explained that the game taught them the basic mechanisms of stigmatization. Yet they also indicated that these positive conversations probably only happen during the game and that they will ‘call each other “fatty” again’ as soon as they leave the room. Nonetheless, we conclude that the Ball & Stick game was successful in creating a storytelling environment for destigmatizing interaction between people with varying experiences, perspectives, and beliefs.
Discussion
In this article we introduce the concept of interactive storytelling environments as a means to reduce health-related stigmatization and suggest applying it to places where health-related stigma is expressed, such as bullying at community centres, judgmental recommendations at supermarkets, or blunt instructions at hospitals. Within interactive storytelling environments, participants are invited to listen and respond to stories from others and at the same time guided in telling their own. As demonstrated by the Ball & Stick game, the advantage of interactive storytelling environments is that they can be deliberately designed to evoke empathy with others, stimulate discussion and critical thinking, and guide towards consensus.
This approach could be a valuable addition to current speculative design approaches in which products and objects are designed to encourage critical reflection (Dunne and Raby 2013). Provocative storytelling environments can stimulate critical reflection and facilitate interactions between different stigma actors. The narrative freedom for each actor is a major parameter in such environments to influence the storytelling possibilities that stigma actors have. By designing interventions that afford or limit this freedom in storytelling, stigma actors can be directed towards 1) diminishing stigma manifestations, 2) deconstructing motivations to stigmatize, and 3) dealing with stigmatizing situations.
The benefit of interactive storytelling environments is not only restricted to health-related stigma. It can also be used to tackle other types of stigmas. Many social issues, such as women’s rights, attitudes towards migrants, and racism could be addressed with design interventions using the storytelling environment approach. More generally, many design processes could benefit from a storytelling environment perspective, in particular where vulnerable or minority groups are involved (Parrott, Carpentier, and Northup 2017). On the one hand storytelling feeds the design process (e.g. Maxwell et al. 2015) and on the other hand a deliberately designed environment can guide the storytelling.
Within the limitations of this paper, we could not give an exhaustive overview of storytelling theories, yet with the seven functions of a storytelling environment we aim to set a research agenda regarding its destigmatizing potential. The Ball & Stick case provides a first idea of designing and applying interactive storytelling environments and demonstrates that such environments contribute to health-related stigma reduction. To apply it more broadly a generic model and design method are required. The basic narratological and interactive digital narrative concepts that we briefly touched upon in this article could serve as a basis for such a model, which could also take further the field of applied narratology (Moenandar 2018). Moreover, knowledge from participatory design and user generated content (cf. Lukyanenko et al. 2016) could support the practical application of such a model.
The seven stigma-reducing functions of storytelling may be applied to a large variation of health-related storytelling environments, for example in the conversation between patients and physicians in consultation rooms. In such contexts, a narrative protective frame could comfort patients and support physicians. Moreover, to welcome storytelling in such a situation could evoke both parties’ openness to the other’s perspective and enable exchange of alternative understandings (Bury 2001). Storytelling tools, such as props or preformatted texts, could help to deliberate on the use of words, as well as deploy the persuasive qualities of narrative transportation. And to make it complete, the consultation room should provide patients with the tools to tell their story appropriately to elicit understanding from the physician and to counter possible unfortunate events of stigmatizing behaviour.
Eventually, the key role of an interactive storytelling environment is to activate a conversation between all stigma actors and guide them towards destigmatizing storytelling. To achieve this, questions about the properties of an interactive storytelling environment pop up. In this article, we covered narrative freedom as a core dimension. Other important properties would include the composition and interests of participants, modes of communication (e.g. verbal, visual, theatrical), and the literacy level of participants. To connect with the participants’ interests and experiences we envision a co-creative process in which all users of a storytelling environment are involved in creating the stories. For example, Whitley et al. (2020) show that documentary-style videos about mental illness, created by people with a mental illness, led to informative, relatable, attention-grabbing, and change-inducing videos that have promising stigma-reducing effects among the viewers.
Finally, we think that interactive storytelling environments contribute to the transition in healthcare from paternalistic top-down approaches to deliberative patient-centred bottom-up approaches (Emanuel and Emanuel 1992). Accordingly, designers of storytelling environments should maintain a neutral position and focus on providing a fitting storytelling environment that stimulates empathy and an awareness and exchange of values and ideas. The environment should mainly facilitate a fair process of meaning-making among all health-related stigma actors, trusting that nearly everyone can tell stories and listen to them.
Conclusion
In this article we propose to use interactive storytelling environments to reduce health-related stigma. We first developed an understanding of the mechanisms behind stigmatization with the health-related stigma perpetuation model (Figure 2) to come to mechanisms on how to break the vicious circle. Due to the multi-layered and multifaceted character of stigmas, we suggest influencing stigmatic storytelling. We theorize seven stigma-reducing functions of storytelling that can be applied to social environments and discuss design considerations within these functions. Some of these considerations have been applied to a design case that demonstrates a destigmatizing interactive storytelling environment: the game of Ball & Stick.
In conclusion, this paper is mainly a call to designers, researchers, and practitioners in health and wellbeing to become aware of health-related stigmatization and create the conditions to reduce stigmas. Our hope is that our propositions in this paper inspire to further erase stigmas by design.
Biographies
Niko Vegt is a Post-Doctoral Researcher at the Faculty of Industrial Design Engineering. His research revolves around social change and the interaction between people through interactive storytelling, serious gaming, and gamification, particularly in healthcare. Niko holds a MSc and BSc degree from Eindhoven University of Technology, faculty Industrial Design. In 2018, he obtained his PhD degree in Industrial Design Engineering at the Delft University of Technology. Niko worked as a human-centered design researcher at the Leiden University Medical Centre. Throughout his career his work is characterized by the research through design approach where the design process is as valuable as analysis and evaluation processes for generating knowledge.
Valentijn Visch is Associate Professor at the Faculty of Industrial Design Engineering at TU Delft. His research is focused on Design for Health Motivation. He coordinates Persuasive Game Design research, chairs the IDE eHealth research lab, and is project leader of several health-related interdisciplinary research projects including subjects like storytelling, digital twins, eHealth & game design, health literacy, obesity prevention, reaching people with low SEP and health journeys.
Wilbert Spooren is professor of Discourse Studies of Dutch at Centre for Language Studies (CLS), Radboud Universiteit Nijmegen. His research concerns the use of language in different genres, and its effect on communication. He has a special interest in the role of language in new media. He obtained his PhD in 1989 at Radboud University. He was one of the initiators of the NWO thematic program Comprehensible Language and Effective Communication (2010-2018). He currently supervises various PhD projects that focus on the role of language in medical communication, specifically with lower literacy target groups.
Elisabeth F. C. van Rossum is internist-endocrinologist and professor in the field of obesity and biological stress research at the Erasmus University Medical Centre, Rotterdam, Netherlands. She is co-founder of the Obesity Centre CGG. She obtained her MD and PhD (both cum laude) in Rotterdam, and performed an obesity research fellowship in Baltimore, USA. Currently, she holds various societal/board positions: European lead of the theme Obesity and Diabetes of the European Society for Endocrinology, Chair of the National Obesity Guideline, and President of the Partnership Overweight Netherlands with an advisory role to the Ministry of Health Welfare. She published with colleague Mariette Boon an international bestseller and award-winning book ‘VET belangrijk’ or -the international edition- ‘FAT, the secret organ’. In 2020 and 2021 she was appointed as Top10 most influencing women in health care in the Netherlands.
Andrea W.M. Evers is professor of Health Psychology and chair of the Institute of Psychology at Leiden University, the Netherlands. She is also affiliated to the Technical University Delft and Erasmus University Rotterdam as Medical Delta Professor Healthy Society. After her PhD (cum laude), Andrea Evers obtained several personal grants and awards) for her innovative, interdisciplinary and translational research on psychoneurobiological mechanisms and treatments for health and disease. She was elected as a lifetime member of the Dutch Royal Academy of Science and Arts (KNAW) as well as the Royal Dutch Society of Science (KHMW). Since 2021, she is also a member of the supervisory board of the VU University Amsterdam.
Annemiek van Boeijen is Assistant Professor Industrial Design at the faculty of Industrial Design Engineering at the Delft University of Technology. Her research isfocused on the role of culture in design processes, with the goal of designing methods and tools, geared to support designers in cultivating a culture-sensitive approach. She is initiator and co-editor of the Delft Design Guide, an overview of perspectives, models, approaches and methods for design, and author of the book Culture Sensitive Design - A guide to culture in practice.
Appendix:
Content of the game of ball & stick
| Introduction story |
|---|
| This is the story of Ball and Stick. It is a fantasy story, but the events come from true stories that people experienced in real life. Ball has overweight and Stick does not. Ball and Stick experience their weight in their own way. They also talk and think differently about balls and sticks. And about weight. People with overweight are regularly discriminated against. This causes stress. And stress is unhealthy. It increases the problem of being overweight. The goal of this game is to increase your knowledge about discrimination on weight. And how you can reduce it. In this game, Ball and Stick experience many different situations. You have to answer a question in each situation. There are no right or wrong answers and there will be no winner. The game finishes when you’ve reached the end together. But how do you do this? You play the game with two players. Both of you have a role; one can choose Ball and the other Stick. If you’re with three, then one player can choose which role to join. If you’re with four players or more, you can play in teams: team Ball and team Stick. Make a paper pawn of Ball and Stick. Place Ball and Stick on position one. Ball begins. Press “Start”. |
| Dilemmas |
Ball steps onto a crowded bus. There is only one narrow seat left. What do you do?
|
Stick steps onto a full bus. There is only one seat left next to someone who takes a lot of space. What do you do?
|
Ball is standing in front of an elevator and hears others thinking: “such balls should take the stairs”. What do you do?
|
Stick is stepping into an elevator. Stick sees someone approaching who is clearly overweight. What do you think?
|
Ball is at work. Someone is serving cake. Ball is being skipped and doesn’t like this. What do you do?
|
Stick is at work. It’s Stick’s birthday, so Stick is serving cake. What do you do?
|
Ball is at the supermarket. Chips and soda are on discount, so Ball buys chips and soda. In the cue at the cash desk someone looks disapprovingly at the groceries. What do you say?
|
Stick walks through the supermarket. Stick sees a person that is overweight buying chips and soda. What do you think?
|
Ball is alone at home and looks in the mirror. What do you think?
|
Stick is alone at home and looks in the mirror. Stick has gained some weight. What do you think?
|
Ball is at a party and sees Stick. What do you think?
|
Stick is at a party and sees Ball standing next to the snacks. What do you think?
|
Ball is at a party talking with some other balls. Ball sees Stick looking at Ball. What do you think?
|
Stick is at a party sitting on the couch. Ball is attracting Stick’s attention. What do you think?
|
| Open response task |
| Ball and Ball’s partner are walking through the park. They see Stick walking. “All those skinny smart asses, yet they look very unhealthy”, says Ball’s partner. How would you react to this? Form your opinion and tell it in 20  seconds to the other. seconds to the other. |
| Stick and Stick’s partner are walking in the park. They see Ball walking. Stick’s partner is pointing at Ball. “Those balls always look very unhealthy.” How would you react to this? Form your opinion and tell it in 20  seconds to the other. seconds to the other. |
| Ball is at the doctor for pain in the knee. The doctor says: “Go first lose some weight.” How would you react to this? Form your opinion and tell it in 20  seconds to the other. seconds to the other. |
| Stick is at the doctor for a sore knee. The doctor says: “There’s nothing you can do about it. Here’s a prescription for painkillers”. How would you react to this? Form your opinion and tell it in 20  seconds to the other. seconds to the other. |
| Ball and the partner of Ball are running on a treadmill at the gym. Ball is exhausted and stops. Ball’s partner says: “Just continue, lazy ass!”. How would you react to this? Form your opinion and tell it in 20  seconds to the other. seconds to the other. |
| Stick and Stick’s partner are at the gym. They see Ball doing exercises. Stick’s partner says: “I bet that ball will drop out any minute now”. How would you react to this? Form your opinion and tell it in 20  seconds to the other. seconds to the other. |
| Ball is standing next to a plus-size rack in a clothing shop. Ball thinks: “Why is the plus-size clothing on a rack separate from the other sizes?” How would you react to this? Form your opinion and tell it in 20  seconds to the other. seconds to the other. |
| Stick is standing in a clothing store. Stick sees a rack of plus-size pants. Stick thinks: “Why can’t those balls just lose some weight?” How would you react to this? Form your opinion and tell it in 20  seconds to the other. seconds to the other. |
| The partner of Ball is coming home from work. Ball’s partner says: “Finding a job is a lot easier for Sticks than for us.” How would you react to this? Form your opinion and tell it in 20  seconds to the other. seconds to the other. |
| Stick and Stick’s partner are at a library. Stick’s partner says: “Balls are stupid, they think that paprika crisps are healthy.” How would you react to this? Form your opinion and tell it in 20  seconds to the other. seconds to the other. |
| Ball is at a party. Ball sees Stick sitting on the couch. Ball joins Stick and thinks: “With Stick I do dare to talk about my weight.” |
| Stick is at a party. Stick sees Ball sitting on the couch. Stick joins Ball and thinks: “With Ball I can have conversations that are not only about how I look.” |
| Making choices together |
Ball and Stick want to do sports together in the park. How do you do this? Choose a way of doing sports without saying it to the other:
Did you both choose for the same option? If not, choose again for a shared answer. |
Ball and Stick prepared dinner together. They want to add a drink that tastes good and is healthy. Which drink will you choose? Choose a drink without saying it to the other:
Did you both choose for the same option? If not, choose again for a shared answer. |
Stick and Ball organize a party. With balls and sticks mingled together. One of the balls greets Ball: “Hi chubby! How are you?” How would you call someone with overweight? Choose for a word without saying it to the other.
Did you both choose for the same option? If not, choose again for a shared answer. |
Ball and Stick are invited for a wedding with a lot of food. They are not sure if they should go. Why do you hesitate? Choose a reason without saying it to the other:
Did you both choose for the same option? If not, choose again for a shared answer. |
Ball and Stick go on a trip by bus to Zeeland. One seat costs 10 euro. What do you do? Choose what you would do without saying it to the other: euro. What do you do? Choose what you would do without saying it to the other:
Did you both choose for the same option? If not, choose again for a shared answer. |
Ball and Stick are sitting on the couch at home. Ball says: “I love you Stick”. “I love you too”, says Stick. How do you think about love? Choose a sentence without saying it to the other:
Did you both choose for the same option? If not, choose again for a shared answer. |
| Ending story |
| Congratulations! You’ve reached the end! The story started with Ball and Stick stepping into a bus. Did you choose to sit? Or rather not? Ball and Stick sometimes did see each other, but they didn’t talk to each other. Then Ball and Stick meet each other at a party. They mainly notice each other’s differences. Among the other Balls and Sticks they encounter many false beliefs. They point at each other and judge each other. But Ball and Stick start to realize that the differences are not so large at all. Being fatter or slimmer is just the way it is. By talking to each other Ball and Stick understand each other better. They also understand other balls and sticks better now. Were you able to better understand Ball and Stick? Did you notice that you also judge people with overweight sometimes? Maybe without being conscious about it? And do people with overweight know that others often have good intentions? We hope that, after playing this game, you can now better deal with differences in weight without making others feel bad about it. Just like Ball and Stick! |
References
- Alberga Angela S., Russell-Mayhew Shelly, von Ranson Kristin M., and McLaren Lindsay.. 2016. “Weight Bias: A Call to Action.” Journal of Eating Disorders 4 (1): 34–34. 10.1186/s40337-016-0112-4 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Alleva Jessica M., Martijn Carolien, Van Breukelen Gerard J. P., Jansen Anita, and Karos Kai.. 2015. “Expand Your Horizon: A Programme That Improves Body Image and Reduces Self-Objectification by Training Women to Focus on Body Functionality.” Body Image 15: 81–89. 10.1016/j.bodyim.2015.07.001 [Abstract] [CrossRef] [Google Scholar]
- Apter, Michael J. 1993. “Phenomenological Frames and the Paradoxes of Experience.” In Advances in Reversal Theory, edited by John H. Kerr, Stephen Murgatroyd, and Michale J. Apter, 27–39. Amsterdam, NL: Swetz & Zeitlinger. [Google Scholar]
- Bacon Linda, and Aphramor Lucy.. 2011. “Weight Science: Evaluating the Evidence for a Paradigm Shift.” Nutrition Journal 10: 9. 10.1186/1475-2891-10-9 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Bamberg, Michael. 2011. “Narrative Practice and Identity Navigation.” In Varieties of Narrative Analysis, edited by James A. Holstein and Jaber F. Gubrium, 99–124. London, UK: SAGE. [Google Scholar]
- Bamberg Michael, and Andrews Molly.. 2004. Considering Counter-Narratives: Narrating, Resisting, Making Sense. Vol. 4. Amsterdam, NL: John Benjamins Publishing. [Google Scholar]
- Barthes Roland, and Duisit Lionel.. 1975. “An Introduction to the Structural Analysis of Narrative.” New Literary History 6 (2): 237–272. 10.2307/468419 [CrossRef] [Google Scholar]
- Bayer, Ronald. 2008. “Stigma and the Ethics of Public Health: not Can we but Should we.” Social Science & Medicine (1982) 67 (3): 463–472. 10.1016/j.socscimed.2008.03.017 [Abstract] [CrossRef] [Google Scholar]
- Becker Diane M., Yanek Lisa R., Koffman Dyann M., and Bronner Yvonne C.. 1999. “Body Image Preferences among Urban African Americans and Whites from Low Income Communities.” Ethnicity & Disease 9 (3): 377–386. [Abstract] [Google Scholar]
- Bleecker, Julian. 2009. Design Fiction: A Short Essay on Design, Science, Fact, and Fiction. Near Future Laboratory. [Google Scholar]
- Boeijinga Anniek, Hoeken Hans, and Sanders José.. 2017. “Storybridging: Four Steps for Constructing Effective Health Narratives.” Health Education Journal 76 (8): 923–935. 10.1177/0017896917725360 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Bombak Andrea E., and Monaghan Lee F.. 2017. “Obesity, Bodily Change and Health Identities: A Qualitative Study of Canadian Women.” Sociology of Health & Illness 39 (6): 923–940. 10.1111/1467-9566.12537 [Abstract] [CrossRef] [Google Scholar]
- Braddock Kurt, and Dillard James Price.. 2016. “Meta-Analytic Evidence for the Persuasive Effect of Narratives on Beliefs, Attitudes, Intentions, and Behaviors.” Communication Monographs 83 (4): 446–467. 10.1080/03637751.2015.1128555 [CrossRef] [Google Scholar]
- Brelet Lisa, Flaudias Valentin, Désert Michel, Guillaume Sébastien, Llorca Pierre-Michel, and Boirie Yves.. 2021. “Stigmatization toward People with Anorexia Nervosa, Bulimia Nervosa, and Binge Eating Disorder: A Scoping Review.” Nutrients 13 (8): 2834. 10.3390/nu13082834 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Brewis, Alexandra. 2014. “Stigma and the Perpetuation of Obesity.” Social Science & Medicine (1982) 118: 152–158. 10.1016/j.socscimed.2014.08.003 [Abstract] [CrossRef] [Google Scholar]
- Brewis Alexandra, Trainer Sarah, Han SeungYong, and Wutich Amber.. 2017. “Publically Misfitting: extreme Weight and the Everyday Production and Reinforcement of Felt Stigma.” Medical Anthropology Quarterly 31 (2): 257–276. 10.1111/maq.12309 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Bruneau Emile G., and Saxe Rebecca.. 2012. “The Power of Being Heard: The Benefits of ‘Perspective-Giving’in the Context of Intergroup Conflict.” Journal of Experimental Social Psychology 48 (4): 855–866. 10.1016/j.jesp.2012.02.017 [CrossRef] [Google Scholar]
- Bury, Mike. 2001. “Illness Narratives: fact or Fiction?” Sociology of Health & Illness 23 (3): 263–285. 10.1111/1467-9566.00252 [CrossRef] [Google Scholar]
- Carey Hillary, To Alexandra, Hammer Jessica, and Kaufman Geoff.. 2020. “Fictional, Interactive Narrative as a Foundation to Talk about Racism.” Paper Presented at the Companion Publication of the 2020 ACM Designing Interactive Systems Conference. 10.1145/3393914.3395885 [CrossRef]
- Cavazza Marc, Charles Fred, Lindsay Alan, Siddle Jonathan, and Georg Gersende.. 2015. “An Interactive Narrative Format for Clinical Guidelines.” KI - Künstliche Intelligenz 29 (2): 185–191. 10.1007/s13218-015-0354-3 [CrossRef] [Google Scholar]
- Chou Wen-ying Sylvia, Prestin Abby, and Kunath Stephen.. 2014. “Obesity in Social Media: A Mixed Methods Analysis.” Translational Behavioral Medicine 4 (3): 314–323. 10.1007/s13142-014-0256-1 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Cook Jonathan E., Purdie-Vaughns Valerie, Meyer Ilan H., and Busch Justin T. A.. 2014. “Intervening within and across Levels: A Multilevel Approach to Stigma and Public Health.” Social Science & Medicine (1982) 103: 101–109. 10.1016/j.socscimed.2013.09.023 [Abstract] [CrossRef] [Google Scholar]
- Corrigan Patrick W., Larson Jonathon E., and Rüsch Nicolas.. 2009. “Self-Stigma and the ‘Why Try’ Effect: impact on Life Goals and Evidence-Based Practices.” World Psychiatry: official Journal of the World Psychiatric Association (WPA) 8 (2): 75–81. 10.1002/j.2051-5545.2009.tb00218.x [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Crandall, Christian S. 1994. “Prejudice against Fat People: Ideology and Self-Interest.” Journal of Personality and Social Psychology 66 (5): 882–894. 10.1037//0022-3514.66.5.882 [Abstract] [CrossRef] [Google Scholar]
- Davidson Tatiana, Moreland Angela, Bunnell Brian E., Winkelmann Jennifer, Hamblen Jessica L., and Ruggiero Kenneth J.. 2018. “Reducing Stigma in Mental Health through Digital Storytelling.” In Deconstructing Stigma in Mental Health, 169–183. London, UK: IGI Global. [Google Scholar]
- de Boer Bas, and Lemke Mailin.. 2021. “Bringing Disgust in through the Backdoor in Healthy Food Promotion: A Phenomenological Perspective.” Medicine, Health Care, and Philosophy 24 (4): 731–743. 10.1007/s11019-021-10037-0 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- De Brún Aoife, McCarthy Mary, McKenzie Kenneth, and McGloin Aileen.. 2014. “Weight Stigma and Narrative Resistance Evident in Online Discussions of Obesity.” Appetite 72: 73–81. 10.1016/j.appet.2013.09.022 [Abstract] [CrossRef] [Google Scholar]
- Derrida, Jacques. 1972. Positions. Paris, FR: Nouvelles Editions Latines. [Google Scholar]
- Dunne Anthony, and Raby Fiona.. 2013. Speculative Everything: design, Fiction, and Social Dreaming. Cambridge, US: MIT Press. [Google Scholar]
- Durso Laura E., and Latner Janet D.. 2008. “Understanding Self-Directed Stigma: Development of the Weight Bias Internalization Scale.” Obesity 16 (S2): 80–86. 10.1038/oby.2008.448 [Abstract] [CrossRef] [Google Scholar]
- Emanuel Ezekiel J., and Emanuel Linda L.. 1992. “Four Models of the Physician-Patient Relationship.” Jama 267 (16): 2221–2226. 10.1001/jama.1992.03480160079038 [Abstract] [CrossRef] [Google Scholar]
- Entman, Robert M. 1993. “Framing: Toward Clarification of a Fractured Paradigm.” Journal of Communication 43 (4): 51–58. 10.1111/j.1460-2466.1993.tb01304.x [CrossRef] [Google Scholar]
- Falk, Gerhard. 2001. Stigma: How we Treat Outsiders. Buffalo, US: Prometheus Books. [Google Scholar]
- Georgakopoulou, Alexandra. 2015. “Small Stories Research.” In The Handbook of Narrative Analysis, edited by De Fina Anna and Georgakopoulou Alexandra., 255–271. Chichester: John Wiley & Sons, Inc. [Google Scholar]
- Gérard, Genette. 1980. Narrative Discourse: An Essay in Method. Translated by Jane E. Lewin, editor. . Ithaca: Cornell UP. [Google Scholar]
- Giskes K., Avendano M., Brug J., and Kunst A. E.. 2010. “A Systematic Review of Studies on Socioeconomic Inequalities in Dietary Intakes Associated with Weight Gain and Overweight/Obesity Conducted among European Adults.” Obesity Reviews: An Official Journal of the International Association for the Study of Obesity 11 (6): 413–429. 10.1111/j.1467-789X.2009.00658.x [Abstract] [CrossRef] [Google Scholar]
- Goffman, E. 1963. Stigma: The Management of Spoiled Identity. Harmondsworth: Penguin. [Google Scholar]
- Gomillion Sarah C., and Giuliano Traci A.. 2011. “The Influence of Media Role Models on Gay, Lesbian, and Bisexual Identity.” Journal of Homosexuality 58 (3): 330–354. 10.1080/00918369.2011.546729 [Abstract] [CrossRef] [Google Scholar]
- De Graaf Anneke, Sanders José, and Hoeken Hans.. 2016. “Characteristics of Narrative Interventions and Health Effects: A Review of the Content, Form, and Context of Narratives in Health-Related Narrative Persuasion Research.” Review of Communication Research 4: 88–131. 10.12840/issn.2255-4165.2016.04.01.011 [CrossRef] [Google Scholar]
- Hague Anne L., and White Adrienne A.. 2005. “Web-Based Intervention for Changing Attitudes of Obesity among Current and Future Teachers.” Journal of Nutrition Education and Behavior 37 (2): 58–66. 10.1016/s1499-4046(06)60017-1 [Abstract] [CrossRef] [Google Scholar]
- Hammond Sean, Pain Helen, and Smith Tim J.. 2007. “Player Agency in Interactive Narrative: audience, Actor & Author.” Proceedings of AISB '07: Artificial and Ambient Intelligence, 2-4 Apr 2007, Newcastle, UK.
- Harriger Jennifer A., and Thompson J. Kevin.. 2012. “Psychological Consequences of Obesity: Weight Bias and Body Image in Overweight and Obese Youth.” International Review of Psychiatry (Abingdon, England) 24 (3): 247–253. 10.3109/09540261.2012.678817 [Abstract] [CrossRef] [Google Scholar]
- Hatzenbuehler, Mark L. 2016. “Structural Stigma and Health Inequalities: Research Evidence and Implications for Psychological Science.” The American Psychologist 71 (8): 742–751. 10.1037/amp0000068 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Hatzenbuehler Mark L., and Link Bruce G.. 2014. “Introduction to the Special Issue on Structural Stigma and Health.” Social Science & Medicine (1982) 103: 1–6. 10.1016/j.socscimed.2013.12.017 [Abstract] [CrossRef] [Google Scholar]
- Hatzenbuehler Mark L., Phelan Jo. C., and Link Bruce G.. 2013. “Stigma as a Fundamental Cause of Population Health Inequalities.” American Journal of Public Health 103 (5): 813–821. 10.2105/AJPH.2012.301069 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Hayward Lydia E., Vartanian Lenny R., and Pinkus Rebecca T.. 2018. “Weight Stigma Predicts Poorer Psychological Well‐Being through Internalized Weight Bias and Maladaptive Coping Responses.” Obesity (Silver Spring, Md.) 26 (4): 755–761. 10.1002/oby.22126 [Abstract] [CrossRef] [Google Scholar]
- Hebl Michelle R., and Dovidio John F.. 2005. “Promoting the “Social” in the Examination of Social Stigmas.” Personality and Social Psychology Review: An Official Journal of the Society for Personality and Social Psychology, Inc 9 (2): 156–182. 10.1207/s15327957pspr0902_4 [Abstract] [CrossRef] [Google Scholar]
- Heuer Chelsea A., McClure Kimberly J., and Puhl Rebecca M.. 2011. “Obesity Stigma in Online News: A Visual Content Analysis.” Journal of Health Communication 16 (9): 976–987. 10.1080/10810730.2011.561915 [Abstract] [CrossRef] [Google Scholar]
- Hulshof K. F. A. M., Brussaard J. H., Kruizinga A. G., Telman J., and Löwik M. R. H.. 2003. “Socio-Economic Status, Dietary Intake and 10 y Trends: The Dutch National Food Consumption Survey.” European Journal of Clinical Nutrition 57 (1): 128–137. 10.1038/sj.ejcn.1601503 [Abstract] [CrossRef] [Google Scholar]
- Hunger Jeffrey M., Major Brenda, Blodorn Alison, and Miller Carol T.. 2015. “Weighed down by Stigma: How Weight-Based Social Identity Threat Contributes to Weight Gain and Poor Health.” Social and Personality Psychology Compass 9 (6): 255–268. 10.1111/spc3.12172 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Irigaray, Luce. 1985. This Sex Which is Not One (1977). New York, US: Cornell University Press. [Google Scholar]
- Jackson Sarah E., and Steptoe Andrew.. 2018. “Obesity, Perceived Weight Discrimination, and Hair Cortisol: A Population-Based Study.” Psychoneuroendocrinology 98: 67–73. 10.1016/j.psyneuen.2018.08.018 [Abstract] [CrossRef] [Google Scholar]
- Keen, Suzanne. 2006. “A Theory of Narrative Empathy.” Narrative 14 (3): 207–236. 10.1353/nar.2006.0015 [CrossRef] [Google Scholar]
- Kidd David Comer, and Castano Emanuele.. 2013. “Reading Literary Fiction Improves Theory of Mind.” Science (New York, N.Y.) 342 (6156): 377–380. 10.1126/science.1239918 [Abstract] [CrossRef] [Google Scholar]
- Knaak Stephanie, Modgill Geeta, and Patten Scott B.. 2014. “Key Ingredients of anti-Stigma Programs for Health Care Providers: A Data Synthesis of Evaluative Studies.” The Canadian Journal of Psychiatry 59 (1_suppl): 19–26. 10.1177/070674371405901S06 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Koenitz, Hartmut. 2023. Understanding Interactive Digital Narrative: Immersive Expressions for a Complex Time. London, UK: Taylor & Francis. [Google Scholar]
- Kolata, Gina Bari. 2007. Rethinking Thin: The New Science of Weight Loss–and the Myths and Realities of Dieting. London, UK: Macmillan. [Google Scholar]
- Korthals Altes, Liesbeth. 2014. Ethos and Narrative Interpretation: The Negotiation of Values in Fiction. Lincoln, US: U of Nebraska Press. [Google Scholar]
- Kozel, Susan. 1996. “The Diabolical Strategy of Mimesis: Luce Irigaray’s Reading of Maurice Merleau‐Ponty.” Hypatia 11 (3): 114–129. 10.1111/j.1527-2001.1996.tb01018.x [CrossRef] [Google Scholar]
- Kranke Derrick A., Floersch Jerry, Kranke Bridget O., and Munson Michelle R.. 2011. “A Qualitative Investigation of Self-Stigma among Adolescents Taking Psychiatric Medication.” Psychiatric Services (Washington, D.C.) 62 (8): 893–899. 10.1176/ps.62.8.pss6208_0893 [Abstract] [CrossRef] [Google Scholar]
- Larkey Linda K., and Hecht Michael.. 2010. “A Model of Effects of Narrative as Culture-Centric Health Promotion.” Journal of Health Communication 15 (2): 114–135. 10.1080/10810730903528017 [Abstract] [CrossRef] [Google Scholar]
- Lau Patrick W. C., Lee Antoinette, and Ransdell Lynda.. 2007. “Parenting Style and Cultural Influences on Overweight Children’s Attraction to Physical Activity.” Obesity (Silver Spring, Md.) 15 (9): 2293–2302. 10.1038/oby.2007.272 [Abstract] [CrossRef] [Google Scholar]
- Lely Jeannette C. G., Smid Geert E., Jongedijk Ruud A., Knipscheer Jeroen W., and Kleber Rolf J.. 2019. “The Effectiveness of Narrative Exposure Therapy: A Review, Meta-Analysis and Meta-Regression Analysis.” European Journal of Psychotraumatology 10 (1): 1550344. 10.1080/20008198.2018.1550344 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Lewis Sophie, Thomas Samantha L., Blood R. Warwick, Castle David J., Hyde Jim, and Komesaroff Paul A.. 2011. “How Do Obese Individuals Perceive and Respond to the Different Types of Obesity Stigma That They Encounter in Their Daily Lives? A Qualitative Study.” Social Science & Medicine (1982) 73 (9): 1349–1356. 10.1016/j.socscimed.2011.08.021 [Abstract] [CrossRef] [Google Scholar]
- Lewis Stephen T., and van Puymbroeck Marieke.. 2008. “Obesity-Stigma as a Multifaceted Constraint to Leisure.” Journal of Leisure Research 40 (4): 574–588. 10.1080/00222216.2008.11950153 [CrossRef] [Google Scholar]
- Lillis Jason, Luoma Jason B., Levin Michael E., and Hayes Steven C.. 2010. “Measuring Weight Self‐Stigma: The Weight Self‐Stigma Questionnaire.” Obesity (Silver Spring, Md.) 18 (5): 971–976. 10.1038/oby.2009.353 [Abstract] [CrossRef] [Google Scholar]
- Link Bruce G., and Phelan Jo. C.. 2001. “Conceptualizing Stigma.” Annual Review of Sociology 27 (1): 363–385. 10.1146/annurev.soc.27.1.363 [CrossRef] [Google Scholar]
- Lu Y., Duller P., Van Der Valk P. G. M., and Evers A. W. M.. 2003. “Helplessness as Predictor of Perceived Stigmatization in Patients with Psoriasis and Atopic Dermatitis.” Dermatology and Psychosomatics / Dermatologie Und Psychosomatik 4 (3): 146–150. 10.1159/000073991 [CrossRef] [Google Scholar]
- Lukyanenko Roman, Parsons Jeffrey, Wiersma Yolanda, Sieber Renee, and Maddah Mahed.. 2016. “Participatory Design for User-Generated Content: Understanding the Challenges and Moving Forward.” Scandinavian Journal of Information Systems 28 (1): 2. [Google Scholar]
- Lupton, Deborah. 2018. Fat. London, UK: Routledge. [Google Scholar]
- Maxwell Deborah, Speed Chris, Monsen Karl, and Zamora Diego.. 2015. “Creating a Collaborative Space for Creativity through a Pervasive User Experience.” Paper Presented at the Proceedings of the 2015 ACM SIGCHI Conference on Creativity and Cognition. 10.1145/2757226.2757234 [CrossRef]
- McLean Kate C., and Syed Moin.. 2015. “Personal, Master, and Alternative Narratives: An Integrative Framework for Understanding Identity Development in Context.” Human Development 58 (6): 318–349. 10.1159/000445817 [CrossRef] [Google Scholar]
- Meretoja, Hanna. 2017. The Ethics of Storytelling: Narrative Hermeneutics, History, and the Possible. Oxford, UK: Oxford University Press. [Google Scholar]
- Milaneschi Yuri, Simmons W. Kyle, van Rossum Elisabeth F. C., and Penninx Brenda W. J. H.. 2019. “Depression and Obesity: evidence of Shared Biological Mechanisms.” Molecular Psychiatry 24 (1): 18–33. 10.1038/s41380-018-0017-5 [Abstract] [CrossRef] [Google Scholar]
- Moenandar, Sjoerd-Jeroen. 2018. “When Not to Tell Stories: Unnatural Narrative in Applied Narratology.” Frontiers of Narrative Studies 4 (1): 6–20. 10.1515/fns-2018-0002 [CrossRef] [Google Scholar]
- Monaghan, Lee F. 2017. “Re-Framing Weight-Related Stigma: From Spoiled Identity to Macro-Social Structures.” Social Theory & Health 15 (2): 182–205. 10.1057/s41285-016-0022-1 [CrossRef] [Google Scholar]
- Mouffe, Chantal. 1999. “Deliberative Democracy or Agonistic Pluralism?.” Social Research 66 (3): 745–758. [Google Scholar]
- Myers Anne, and Rosen James C.. 1999. “Obesity Stigmatization and Coping: relation to Mental Health Symptoms, Body Image, and Self-Esteem.” International Journal of Obesity and Related Metabolic Disorders: journal of the International Association for the Study of Obesity 23 (3): 221–230. 10.1038/sj.ijo.0800765 [Abstract] [CrossRef] [Google Scholar]
- Norman, Donald A. 1999. “Affordance, Conventions, and Design.” Interactions 6 (3): 38–43. 10.1145/301153.301168 [CrossRef] [Google Scholar]
- Pachankis, John. 2007. “The Psychological Implications of Concealing a Stigma: A Cognitive–Affective–Behavioral Model.” Psychological Bulletin 133 (2): 328–345. 10.1037/0033-2909.133.2.328 [Abstract] [CrossRef] [Google Scholar]
- Papadopoulos Stephanie, and Brennan Leah.. 2015. “Correlates of Weight Stigma in Adults with Overweight and Obesity: A Systematic Literature Review.” Obesity (Silver Spring, Md.) 23 (9): 1743–1760. 10.1002/oby.21187 [Abstract] [CrossRef] [Google Scholar]
- Paradies Yin, Luiz Bastos João, and Priest Naomi.. 2016. “Prejudice, Stigma, Bias, Discrimination, and Health.” In The Cambridge Handbook of the Psychology of Prejudice, edited by Sibley Chris G. and Barlow Fiona Kate., 559–581. Cambridge: Cambridge University Press. [Google Scholar]
- Parrott Scott, Carpentier Francesca R. Dillman, and Northup C. Temple.. 2017. “A Test of Interactive Narrative as a Tool against Prejudice.” Howard Journal of Communications 28 (4): 374–389. 10.1080/10646175.2017.1300965 [CrossRef] [Google Scholar]
- Pascoe Elizabeth A., and Smart Richman Laura.. 2009. “Perceived Discrimination and Health: A Meta-Analytic Review.” Psychological Bulletin 135 (4): 531–554. 10.1037/a0016059 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Pasupathi Monisha, and Billitteri Jacob.. 2015. “Being and Becoming through Being Heard: Listener Effects on Stories and Selves.” International Journal of Listening 29 (2): 67–84. 10.1080/10904018.2015.1029363 [CrossRef] [Google Scholar]
- Pearl, Rebecca L. 2018. “Weight Bias and Stigma: Public Health Implications and Structural Solutions.” Social Issues and Policy Review 12 (1): 146–182. 10.1111/sipr.12043 [CrossRef] [Google Scholar]
- Phelan Jo, Link Bruce G., and Dovidio John F.. 2008. “Stigma and Prejudice: One Animal or Two?” Social Science & Medicine (1982) 67 (3): 358–367. 10.1016/j.socscimed.2008.03.022 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Pucci Andrea, and Batterham Rachel L.. 2020. “Endocrinology of the Gut and the Regulation of Body Weight and Metabolism.” Endotext [internet], edited by Feingold K. R., Anawalt, B., Blackman, M. R., et al. South Darmouth: MDText.com Inc. [Abstract] [Google Scholar]
- Puhl Rebecca M., and Heuer Chelsea A.. 2009. “The Stigma of Obesity: A Review and Update.” Obesity (Silver Spring, Md.) 17 (5): 941–964. 10.1038/oby.2008.636 [Abstract] [CrossRef] [Google Scholar]
- Puhl Rebecca M., and Heuer Chelsea A.. 2010. “Obesity Stigma: Important Considerations for Public Health.” Framing Health Matters 100 (6): 1019–2010. [Abstract] [Google Scholar]
- Puhl R. M., Latner J. D., O'Brien K., Luedicke J., Danielsdottir S., and Forhan M.. 2015. “A Multinational Examination of Weight Bias: Predictors of Anti-fat Attitudes across Four Countries.” International Journal of Obesity 39 (7): 1166–1173. 10.1038/ijo.2015.32 [Abstract] [CrossRef] [Google Scholar]
- Puhl Rebecca M., Schwartz Marlene B., and Brownell Kelly D.. 2005. “Impact of Perceived Consensus on Stereotypes about Obese People: A New Approach for Reducing Bias.” Health Psychology: official Journal of the Division of Health Psychology, American Psychological Association 24 (5): 517–525. 10.1037/0278-6133.24.5.517 [Abstract] [CrossRef] [Google Scholar]
- Puhl Rebecca M., and Suh Young.. 2015. “Health Consequences of Weight Stigma: Implications for Obesity Prevention and Treatment.” Current Obesity Reports 4 (2): 182–190. 10.1007/s13679-015-0153-z [Abstract] [CrossRef] [Google Scholar]
- Quinn Diane M., and Chaudoir Stephenie R.. 2009. “Living with a Concealable Stigmatized Identity: The Impact of Anticipated Stigma, Centrality, Salience, and Cultural Stigma on Psychological Distress and Health.” Journal of Personality and Social Psychology 97 (4): 634–651. 10.1037/a0015815 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Reid Allecia E., Dovidio John F., Ballester Estrellita, and Johnson Blair T.. 2014. “HIV Prevention Interventions to Reduce Sexual Risk for African Americans: The Influence of Community-Level Stigma and Psychological Processes.” Social Science & Medicine (1982) 103: 118–125. 10.1016/j.socscimed.2013.06.028 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Richman Laura Smart, and Lattanner Micah R.. 2014. “Self-Regulatory Processes Underlying Structural Stigma and Health.” Social Science & Medicine (1982) 103: 94–100. 10.1016/j.socscimed.2013.12.029 [Abstract] [CrossRef] [Google Scholar]
- Robroek Suzan J. W., Rongen Anne, Arts Coos H., Otten Ferdy W. H., Burdorf Alex, and Schuring Merel.. 2015. “Educational Inequalities in Exit from Paid Employment among Dutch Workers: The Influence of Health, Lifestyle and Work.” PLoS One 10 (8): e0134867. 10.1371/journal.pone.0134867 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Roth Christian, Vorderer Peter, and Klimmt Christoph.. 2009. “The Motivational Appeal of Interactive Storytelling: Towards a Dimensional Model of the User Experience.” In Interactive Storytelling: Second Joint International Conference on Interactive Digital Storytelling, ICIDS 2009, edited by Iurgel Ido A., Zagalo Nelson and Petta Paolo., 38–43. Guimarães, Portugal: Springer. [Google Scholar]
- Saguy Abigail C., and Gruys Kjerstin.. 2010. “Morality and Health: News Media Constructions of Overweight and Eating Disorders.” Social Problems 57 (2): 231–250. 10.1525/sp.2010.57.2.231 [CrossRef] [Google Scholar]
- Scambler, Graham. 2009. “Health‐Related Stigma.” Sociology of Health & Illness 31 (3): 441–455. 10.1111/j.1467-9566.2009.01161.x [Abstract] [CrossRef] [Google Scholar]
- Shen Fuyuan, Sheer Vivian C., and Li Ruobing.. 2015. “Impact of Narratives on Persuasion in Health Communication: A Meta-Analysis.” Journal of Advertising 44 (2): 105–113. 10.1080/00913367.2015.1018467 [CrossRef] [Google Scholar]
- Stangl Anne L., Earnshaw Valerie A., Logie Carmen H., van Brakel Wim, Simbayi Leickness C., Barré Iman, and Dovidio John F.. 2019. “The Health Stigma and Discrimination Framework: A Global, Crosscutting Framework to Inform Research, Intervention Development, and Policy on Health-Related Stigmas.” BMC Medicine 17 (1): 31. 10.1186/s12916-019-1271-3 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Syed, Moin. 2015. “Theoretical and Methodological Contributions of Narrative Psychology to Ethnic Identity Research.” In Studying Ethnic Identity: Methodological and Conceptual Approaches Across Disciplines, edited by C. E. Santos and A. J. Umaña-Taylor, 27–54. New York, US: American Psychological Association. 10.1037/14618-003 [CrossRef]
- Teachman Bethany A., Gapinski Kathrine D., Brownell Kelly D., Rawlins Melissa, and Jeyaram Subathra.. 2003. “Demonstrations of Implicit anti-Fat Bias: The Impact of Providing Causal Information and Evoking Empathy.” Health Psychology: official Journal of the Division of Health Psychology, American Psychological Association 22 (1): 68–78. 10.1037//0278-6133.22.1.68 [Abstract] [CrossRef] [Google Scholar]
- Tomiyama, A. Janet. 2014. “Weight Stigma is Stressful. A Review of Evidence for the Cyclic Obesity/Weight-Based Stigma Model.” Appetite 82: 8–15. 10.1016/j.appet.2014.06.108 [Abstract] [CrossRef] [Google Scholar]
- Tomiyama A. Janet, Finch Laura E., Incollingo Belsky Angela C., Buss Julia, Finley Carrie, Schwartz Marlene B., and Daubenmier Jennifer.. 2015. “Weight Bias in 2001 versus 2013: Contradictory Attitudes among Obesity Researchers and Health Professionals.” Obesity (Silver Spring, Md.) 23 (1): 46–53. 10.1002/oby.20910 [Abstract] [CrossRef] [Google Scholar]
- Vaes Kristof, Stappers Pieter Jan, Standaert Achiel, and Desager Kristine.. 2012. “Contending Stigma in Product Design: using Insights from Social Psychology as a Stepping Stone for Design Strategies.” Paper Presented at the out of Control; Proceedings of the 8th International Conference on Design and Emotion, London, Great Britain, 11-14 Sept. 2012.
- van Amsterdam Noortje, and van Eck Dide.. 2019. “‘I Have to Go the Extra Mile’. How Fat Female Employees Manage Their Stigmatized Identity at Work.” Scandinavian Journal of Management 35 (1): 46–55. 10.1016/j.scaman.2018.10.002 [CrossRef] [Google Scholar]
- Van Beugen S., Van Middendorp H., Ferwerda M., Smit J. V., Zeeuwen‐Franssen M. E. J., Kroft E. B. M., De Jong E. M. G. J., Donders A. R. T., Van de Kerkhof P. C. M., and Evers A. W. M.. 2017. “Predictors of Perceived Stigmatization in Patients with Psoriasis.” The British Journal of Dermatology 176 (3): 687–694. 10.1111/bjd.14875 [Abstract] [CrossRef] [Google Scholar]
- van der Valk Eline S., van den Akker Erica L. T., Savas Mesut, Kleinendorst Lotte, Visser Jenny A., Van Haelst Mieke M., Sharma Arya M., and van Rossum Elisabeth F. C.. 2019. “A Comprehensive Diagnostic Approach to Detect Underlying Causes of Obesity in Adults.” Obesity Reviews: An Official Journal of the International Association for the Study of Obesity 20 (6): 795–804. 10.1111/obr.12836 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Van Laer Tom, De Ruyter Ko, Visconti Luca M., and Wetzels Martin.. 2013. “The Extended Transportation-Imagery Model: A Meta-Analysis of the Antecedents and Consequences of Consumers’ Narrative Transportation.” Journal of Consumer Research 40 (5): 797–817. 10.1086/673383 [CrossRef] [Google Scholar]
- Vandenbroeck Philippe, Goossens Jo, and Clemens Marshall.. 2010. Foresight: Tackling Obesities: Future Choices. Obesity System Atlas: Government Office for Science. [Google Scholar]
- Vegt Niko, Visch Valentijn, Vermeeren Arnold, and de Ridder Huib.. 2016. “Player Experiences and Behaviors in a Multiplayer Game: Designing Game Rules to Change Interdependent Behavior.” International Journal of Serious Games 3 (4), 69-85. 10.17083/ijsg.v3i4.150 [CrossRef] [Google Scholar]
- Visch V. T., Vegt N. J. H., Anderiesen H., and Van der Kooij K.. 2013. “Persuasive Game Design: A Model and Its Definitions.” Proceedings of CHI 2013: Workshop Designing Gamification: Creating Gameful and Playful Experiences, Paris, France, 27 April-2 May 2013
- Vyncke Bart, and Van Gorp Baldwin.. 2020. “Using Counterframing Strategies to Enhance anti-Stigma Campaigns Related to Mental Illness.” Social Science & Medicine (1982) 258: 113090. 10.1016/j.socscimed.2020.113090 [Abstract] [CrossRef] [Google Scholar]
- Weiss Mitchell G., Ramakrishna Jayashree, and Somma Daryl.. 2006. “Health-Related Stigma: rethinking Concepts and Interventions.” Psychology, Health & Medicine 11 (3): 277–287. 10.1080/13548500600595053 [Abstract] [CrossRef] [Google Scholar]
- Whitley Rob., Sitter Kathleen C., Adamson Gavin, and Carmichael Victoria.. 2020. “Can Participatory Video Reduce Mental Illness Stigma? Results from a Canadian Action-Research Study of Feasibility and Impact.” BMC Psychiatry 20 (1): 16. 10.1186/s12888-020-2429-4 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Wiese Helen J., Wilson John F., Jones R. A., and Neises M.. 1992. “Obesity Stigma Reduction in Medical Students.” International Journal of Obesity and Related Metabolic Disorders: journal of the International Association for the Study of Obesity 16 (11): 859–868. [Abstract] [Google Scholar]
- Winskell Kate, Sabben Gaëlle, and Obong’o Christopher.. 2019. “Interactive Narrative in a Mobile Health Behavioral Intervention (Tumaini): Theoretical Grounding and Structure of a Smartphone Game to Prevent HIV among Young Africans.” JMIR Serious Games 7 (2): e13037. 10.2196/13037 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Ziebland Sue, and Wyke Sally.. 2012. “Health and Illness in a Connected World: How Might Sharing Experiences on the Internet Affect People’s Health?” The Milbank Quarterly 90 (2): 219–249. 10.1111/j.1468-0009.2012.00662.x [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Zussman, Robert. 2012. “Narrative Freedom.” Sociological Forum 27 (4): 807–824. 10.1111/j.1573-7861.2012.01357.x [CrossRef] [Google Scholar]
Citations & impact
This article has not been cited yet.
Impact metrics
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/163929553
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
The Effects of Internet-Based Storytelling Programs (Amazing Adventure Against Stigma) in Reducing Mental Illness Stigma With Mediation by Interactivity and Stigma Content: Randomized Controlled Trial.
J Med Internet Res, 24(8):e37973, 12 Aug 2022
Cited by: 5 articles | PMID: 35969460 | PMCID: PMC9419045
Designing and delivering facilitated storytelling interventions for chronic disease self-management: a scoping review.
BMC Health Serv Res, 16:249, 11 Jul 2016
Cited by: 22 articles | PMID: 27401836 | PMCID: PMC4940988
Review Free full text in Europe PMC
Dynamic and game theory of infectious disease stigmas.
J Theor Biol, 476:95-107, 30 May 2019
Cited by: 3 articles | PMID: 31153888
Stigma experienced by people living with HIV who are on methadone maintenance treatment and have symptoms of common mental disorders in Hanoi, Vietnam: a qualitative study.
AIDS Res Ther, 19(1):63, 14 Dec 2022
Cited by: 2 articles | PMID: 36517849 | PMCID: PMC9753276