FAQs about Betaseron
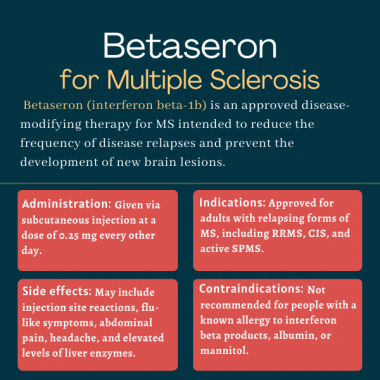
Betaseron was the first disease-modifying therapy to be approved by the U.S. Food and Drug Administration for multiple sclerosis. It was granted that approval in 1993 for relapsing-remitting MS. The approval for Betaseron was later expanded to include clinically isolated syndrome in 2006, and active secondary progressive MS in 2019.
A number of observational studies that tracked the outcomes of more than 2,000 pregnancies exposed to interferon beta therapies, including Betaseron, did not identify an increased risk of adverse pregnancy outcomes or major birth defects. If clinically needed, Betaseron may be considered during pregnancy, but experience with the medication in the second and third trimesters of pregnancy remains limited. Patients who are or plan to become pregnant should discuss the benefits and risks of continuing to receive treatment with their healthcare providers.
There are no studies reporting an interaction between Betaseron and alcohol. However, alcohol and any other compounds with the potential to cause liver damage should be used with caution while taking this medication.
It is difficult to determine a standard timeline for when Betaseron starts to work. In the BENEFIT trial, which tested the medication in people with clinically isolated syndrome, a significant reduction in new brain lesions was evident within the first six months, and a reduction in relapse rates and in progression to needing a wheelchair also were observed after 12 months of treatment. Patients are advised, however, to talk with their healthcare team about how the medication may help in their specific case.
Hair loss has been reported in clinical trials as a potential side effect of interferon-beta medications, including Betaseron. Weight gain also is a possible side effect of this therapy. Patients should talk with their healthcare team about any unexpected symptoms experienced on the medication.
Related Articles

 Fact-checked by
Fact-checked by