Topic: Management of Multiple Sclerosis Relapses
Author: Obada Al Jayyousi
Editor: Noor Qasem, Ethar Hazaimeh
Keywords: Neurology, Demyelinating, Relapse, MS
Overview
Despite the increasing number of treatment modalities for Multiple Sclerosis (MS), relapses remain an unpredictable and insufferable aspect of the disease. As such, adequate and efficient treatment of these relapses are of the essence.
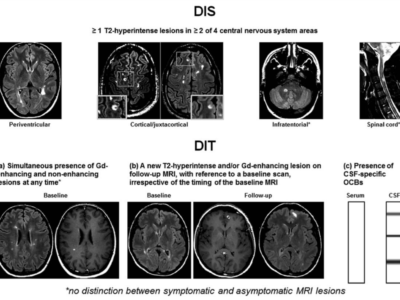
Before we can treat a Multiple Sclerosis (MS) Relapse, however, it is important to correctly distinguish it from a pseudo-relapse. We can distinguish a relapse in multiple sclerosis by clinical and radiological findings implying progression and worsening. (1) The clinical picture should suggest a demyelinating involvement of the CNS, with an event duration of no less than 24 hours, where other possible etiologies are absent, like infection. (2)
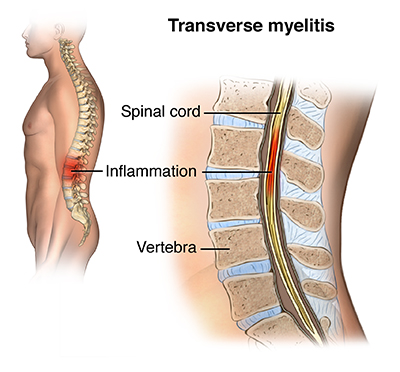
A relapse is treated due to the possible manifestations it could encompass on the optic nerve, brainstem, cerebellum, spinal cord, or cerebral hemispheres.(3)
Treatment of Multiple Sclerosis relapses can be divided into prevention and acute management. The primary management acutely is corticosteroids, while other immunomodulatory therapies are used for prevention. (4) Other treatment options include adrenocorticotropic hormonal therapy, plasmapheresis, and IV immunoglobulins. (3)
Management of Multiple Sclerosis relapses isn’t proven to benefit on the long-term, but evidence shows short-term benefits. (3) However, treatment is still important to relieve any physical or psychological impact acutely.
- Corticosteroids
The earliest published use of corticosteroids in MS was in 1951(5), however IV methylprednisolone is the last approved medication by the FDA for MS relapses so far. (6) 1000 mg daily IV methylprednisolone for 3 to 5 days is one commonly used steroid regimen.
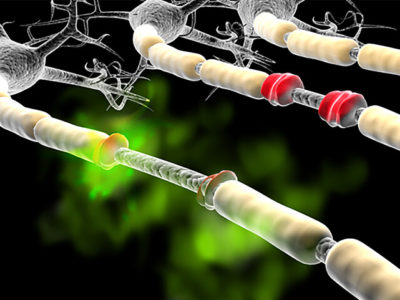
Corticosteroids exhibit anti-inflammatory and immunosuppressive actions which justifies their use in the autoimmune condition. Possible mechanisms include: direct action of high concentrations of corticosteroids on the plasma membrane (8) (9), plasma membrane corticosteroid receptor binding (8), cytosolic corticosteroid receptor binding and consequent downregulation of pro-inflammatory genes. (10)(11)
Steroids are known to have multiple side effects, including: hypertension, hyperglycemia, adrenal crisis, weight gain, moon face, and others. (12) Corticosteroids are indicated acutely for multiple sclerosis as long as there are no contraindications. Contraindications include: being on live “attenuated” vaccines, osteoporosis, diabetes, current systemic infections, and hypersensitivity. (13)
- Adrenocorticotropic hormone therapy (ACTH)
ACTH therapy, Acthar®Gel, was approved by the FDA in1978. (7) ACTH stimulates the adrenal cortex to produce cortisol via melanocortin receptors. There are 5 receptor types in the melanocortin system, where steroidogenesis is the result of melanocortin receptor2 (MCR2) binding (Figure1). Receptor binding involving the other melanocortin receptor types is associated with anti-inflammatory and immunomodulatory effects through decreasing the levels of pro-inflammatory cytokines (IFN-γ, IL-12, TNF, IL-17) and producing anti-inflammatory cytokines (IL-10). (15-18) (Figure 1)

Figure 1, MC2 binding by ACTH. (14)
The Table below (Table 1) summarizes the receptor medicated actions of ACTH on the melanocortin system.


Figure 2, Pro and anti inflammatory cytokines. (19)
ACTH therapy is indicated for MS relapses when patients don’t respond to or can’t tolerate corticosteroids. (21) Routes of administration in the form of “ACTHAR Gel” either subcutaneously or Intramuscularly. Side effects of ACTH are infections, arterial hypertension, osteoporosis, hypokalemic alkalosis (20)
The contraindications are osteoporosis, peptic ulcer disease, chronic heart failure, and allergy to porcine proteins (3)
- Plasmapheresis for MS relapses
Plasmapheresis (Figure 3) is a process of plasma exchange where cells are separated using cell separator technology. Immunoglobulin and Immune complex serum levels can be reduced significantly via repeated plasmapheresis. (23)
Plasmapheresis can be used is severe cases of MS relapses that are not responsive to steroid or ACTH therapy. (21) However, there is some but not a great deal of evidence supporting its effectiveness. (24)

Figure 3, Plasmapheresis. (22)
- IV immunoglobulins (IVIGs) for MS relapses
IV immunoglobulins can potentially help in the prevention of MS relapses, but significant evidence has yet to prove its effectiveness, and so cannot be considered first line therapy. IVIG does however, have the advantage of requiring only monthly perfusions and at doses 0.2 -0.4 g/kg has minimal and infrequent side effects. (25)
Managing MS relapses during pregnancy
Therapy involves IV corticosteroids as first line therapy for acute and severe relapses and immunosuppressive drugs (cyclophosphamide, azathioprine, methotrexate etc) for long term therapy. (26) (27) Furthermore, when steroid therapy isn’t tolerable or is contraindicated for pregnant patients, physicians can use IV immunoglobulins, where some evidence shows a corresponding decrease in the risk of child-birth associated MS exacerbations. (28) (29)
Shepherd MS Institute Protocol for MS relapse: (30)
- To rule out any triggering factors
- To screen for and treat infections when suspected and refrain from steroid use
- In the absence of any obvious triggers, the severity of the symptoms and their implications on daily activities should be assessed
- In case daily life activities aren’t seriously affected, observation is done
- Otherwise, steroid therapy should be tried in the absence of contraindications
- If contraindications are absent, go for 1g/d of IV methylprednisone for 3 days with no oral taper or 300 mg of Oral prednisone twice daily for 3 days with no oral taper.
- Oral lorazepam, 1 mg, can be used for patients with anxiety while on therapy
- 4 g/kg/d of IVIG for 5 days can be used for those who can’t tolerate steroids or those who are pregnant
- For DM patients, steroids should be used carefully while using sliding scale insulin. IVIG could also be used.
In conclusion, patients of MS relapses deserve every effective treatment approach out there to help them have a better quality of life. Up to this date, corticosteroids, ACTH, plasmapheresis, and IVIGs are deemed the most effective, in that order.
Below are a few clinical trials on the management of MS relapses, for further reading:
- Estrogen therapy showing a potential in management of MS relapses. (32)
- Comparing different disease modifying therapies (dimethyl fumarate, fingolimod, teriflunomide) in their effectiveness of reducing the rate of MS relapses (33)
- Combination of Cyclophosphamide and Interferon beta in reducing MS relapse rate (34)
- Use of Copolymer1 (Copaxone) in reducing MS relapse rate (35)