Abstract
We identify the value and usage of a cognitive artifact used by hospital nurses. By analyzing the value and usage of workaround artifacts, unmet needs using intended systems can be uncovered. A descriptive study employed direct observations of registered nurses at two hospitals using a paper workaround (“brains”) and the Electronic Health Record. Field notes and photographs were taken; the format, size, layout, permanence, and content of the artifact were analyzed. Thirty-nine observations, spanning 156 hr, were conducted with 20 nurses across four clinical units. A total of 322 photographs of paper-based artifacts for 161 patients were collected. All participants used and updated “brains” during report, and throughout the shift, most were self-generated. These artifacts contained patient identifiers in a header with room number, last name, age, code status, and physician; clinical data were recorded in the body with historical chronic issues, detailed assessment information, and planned activities for the shift. Updates continuously made during the shift highlighted important information, updated values, and tracked the completion of activities. The primary functional uses of “brains” are to support nurses’ needs for clinical immediacy through personally generated snapshot overviews for clinical summaries and updates to the status of planned activities.
Keywords: cognitive task analysis, domains, ethnography, health care delivery, information systems, methods
INTRODUCTION
Despite the widespread use of Electronic Health Records (EHRs) in hospitals, there remains a heavy reliance upon paper-based cognitive artifacts (Saleem et al., 2009). Cognitive artifacts as defined by Norman (1991) are “those artificial devices that maintain, display, or operate upon information in order to serve a representational function and that affect human cognitive performance” (p. 17). Cognitive artifacts have a persistent presence in health care, both prior to and post recent extensive implementations of EHRs in hospitals and outpatient care settings (Hardey, Payne, & Coleman, 2000; Randell, Wilson, Woodward, & Galliers, 2011). Moreover, cognitive artifacts represent externalized knowledge that is purpose-driven and influences human understanding, reasoning, and decision making (Mclane, Esquivel, & Turley, 2009). Typically, paper-based artifacts are used by a frontline clinician to meet requirements for effective cognitive work, including assessing a change in a patient’s status and implementing treatment plan activities. When the use of the artifact deviates from an intended work process, as documented in policies and procedures, practitioners are using a “workaround” to meet work demands (Alter, 2014).
Investigating the rational reasons for the use of cognitive artifacts as workarounds by expert practitioners has a long history in cognitive engineering (Hollnagel & Woods, 2005; Perry & Wears, 2012); understanding how cognitive artifacts are used as workarounds aids in identifying the difference between Work-as-Imagined (WAI) and Work-as-Done (WAD). Workarounds can be both positive and negative, with some workarounds being innovations that would be useful to incorporate into formal policies and procedures as well as health information technology (HIT). Understanding the context of why cognitive artifacts are used as workarounds highlights gaps in systems to be remedied, to improve system resilience (Clancy, 2010; Hollnagel, Braithwaite, & Wears, 2013). Known reasons for workarounds include avoiding changes to workflow, enabling communication, coordinating activities, and providing access to information summaries (Patterson, 2018) as well as addressing goal conflicts and workload bottlenecks (Woods, 2006). The implementation of new HIT increases system coupling and reliance upon brittle design (Sarter & Woods, 1995), which in turn increases the likelihood of dilemmas with challenging trade-offs. Through the study of cognitive artifacts used as workarounds, we can learn how experts at the sharp end, in this study, nurses, actively adapt and resolve working with the HIT with which they are provided (Woods & Hollnagel, 2006). Examples of studies of cognitive artifacts used as workarounds include identifying data accuracy differences contributing to the preferential use of manual over electronic whiteboards by emergency medicine personnel (Patterson, Rogers, Tomolo, Wears, & Tsevat, 2010) and the team situation awareness benefits of informally using a shared interdisciplinary manual whiteboard in the operating room (Xiao et al., 2007).
Previous research on paper cognitive artifacts by nurses in hospitals identified that registered nurses (RNs) rely on informal, hand-written, personalized paper forms, called “brains,” to perform their cognitive work in a hospital environment (Blaz, Doig, Cloyes, & Staggers, 2016; Staggers & Jennings, 2009). Similarly, nurse coordinators in hospitals utilized personally created paper artifacts, compiling information from the EHR, other electronic artifacts, and clinician handovers, to select, reduce, organize, and annotate key information which could then be accessed in a mobile, rapid fashion and support efficient note-taking (Gurses, Xiao, & Hu, 2009).
Nurses meet their work objectives through self-driven utilization of paper-based artifacts to interpret the environment and create meaning for knowing “where, when, and how” (Mclane & Turley, 2010). The design of EHRs for use in hospitals by nurses has proven to be a complex challenge; nurses taking 30 min every shift to create “brains” provides evidence that current EHRs are not fully meeting the needs of nurses. In particular, the EHR does not perfectly align with their workflow. Information theoretically available in the EHR is easy to miss when nurses prioritize responding to events in a fast-paced, time-constrained environment. This study aims to understand WAD by nurses and the value and usage of self-generated cognitive artifacts. This understanding reveals shortcomings of the current system from the point of view of nurses by understanding where brittleness is occurring and how brittleness is protected against by employing adaptive strategies. Through empirical assessment of the usage and value of the “brains,” we can inform useful evidence-based modifications to the next generation of EHR design, implementation, process workflows, and training.
METHOD
This study is a descriptive, purpose-driven, targeted observational study where data were collected in 2015 and 2016. This research was approved by the Institutional Review Board (IRB) at The Ohio State University. Informed consent was obtained from each study participant. The study site consisted of four inpatient units: three units from a large academic medical center in the Midwest with unionized nursing personnel and one unit from a community hospital with non-unionized nursing personnel. Both hospitals used the same EHR, where local customization, such as regarding default options and order sets, was similar. Each unit had 20 to 35 beds with five to nine RNs staffed during 12-hr shifts with support from patient care associates (PCAs) and a unit clerk. The target units for participation, which were selected to sample a diverse set of patients in acute care, were a (1) cardiovascular step down unit; (2) cardiovascular extended stay unit for surgical patients; (3) general surgery, burn, and ophthalmology unit; and (4) unit with orthopedic, neurological, and trauma patients.
All units included a nursing station with desktop computers. On one unit, additional desktop computers were mounted in the patient rooms. In the remaining three units, Workstations on Wheels (WOWs) with a desktop computer, barcode scanner, and a locking supply drawer were available for each nurse. Computers were used to access multiple types of HIT including the EHR, an electronic medication administration record, a local system to send text pages to hospital personnel, and Internet access to check intravenous (IV) therapy and IV compatibility and general use. The EHR provided access to all patients’ medical records, labs, clinical notes, and so on by navigating through multiple screens and dozens of clicks. At an institutional level, the hospital allowed printing of a patient’s summary report from the EHR, whose content was customized for each hospital unit, titled “NURSING—Notes Only,” intended for nurses and to support handover communication. The summary printouts typically had one summary sheet and four to five supporting printed pages (one side each) in length per patient.
From a human factors perspective, we conducted a contextual design approach with the goal of identifying useful cognitive functions of a cognitive artifact (“brain”) in a complex setting (Beyer & Holtzblatt, 1998). From a traditional ethnographic perspective, we conducted direct observations in a field setting to enable a new understanding of “studied life,” following Charmaz (2008). From both perspectives, understanding the value of a “workaround” artifact requires direct observations to obtain an authentic understanding of how WAD is actually accomplished.
Twenty nurses were recruited. Participants were currently employed nurses working on the four units. Recruitment was a purposeful and convenient sample based on willingness and scheduling. Diversity with respect to years of nursing experience, gender, and shift (night/day) was sought during recruitment.
Data collection was undertaken by a single investigator. This investigator was trained in ethnographic observations, had an educational background in Industrial and Systems Engineering, and had completed an accredited graduate program in Human Factors. The investigator had previously conducted research with direct observations of shift change handovers by nurses and physicians (Rayo et al., 2014), which had included collecting “brains” for analysis.
Field notes were handwritten while shadowing a nurse during 4-hr windows starting at the beginning of the shift, either at 7:00 a.m. or 7:00 p.m. The observer arrived 15 to 30 min prior to the beginning of the shift to observe the strategies used to prepare for the shift before it officially began. Field notes recorded nursing activities, workflow, when and why the EHR was accessed, and how the “brains” were utilized throughout the first 4 hr of the shift. The incorporation of field notes was done following the insight from our previous study (Rayo et al., 2014) collecting “brains,” where it was learned that personally observing their creation and use “in situ” was necessary to fully understand the value and usage of the artifact. During observations, opportunistic interviews were used to clarify the intent of layout, content, and format of printed and handwritten data on the “brain” and reasons for not following intended procedures, which are supported by HIT. Photographs of the “brains” were taken after the patient handover and the end of the 4-hr observation period, such that we could observe the differences or updates made to the “brain” after patient assessment and medication administration.
For analysis, a digital photograph of each patient’s “brain” was used in conjunction with the field notes to analyze the format, layout, and the information content and how these changed over time. “Brain” photos were de-identified before long-term storage, original photos files were destroyed to protect patient privacy. In this way, we determined what information was included on the “brain” along with where, why, and how it evolved as the shift progressed. “Brain” photos were analyzed with an iterative, bottom-up qualitative approach. Information content, style, and layout were coded and counted, by categories which emerged during analysis. Analysis revealed two spatially clustered areas, which we refer to as a “header” and “body” of the “brain.” The purpose of the header was inferred to be patient identity verification, whereas the body contained structured data for predefined body systems and content areas. The detailed data were primarily provided with handwritten annotations in predefined spatial areas with consistent labels, whereas margins tended to contain jotted information to support contacting other personnel or remembering to document information in the EHR documentation at a later time.
A codebook and coding system were developed using a grounded theory approach, allowing codes to emerge through an iterative process. Then, a second investigator analyzed a randomly selected subset of 10% of the “brains” content using the initial codebook. Slight adjustments to the codebook were made based on identified discrepancies; the discrepancies were discussed between coders and a consensus was derived and the codebook was finalized. To assess the reliability of the coding system, we confirmed sufficient interrater reliability using a randomly selected 20% subset of the brains. All data were then again analyzed using the final codebook by a single investigator.
RESULTS
Overall, field notes were collected from 156 hr of observation of 20 nurses from four units at two hospitals. A total of 161 patients were represented by two digital photographs of “brains,” which were taken directly after the completion of the shift change handover and at the end of the thirty-nine 4-hr observation periods, for a total of 322 photographs. “Brains” were defined as informal personally generated artifacts which were solely used by the creator and discarded at the conclusion of care for the related patient. Analysis, focusing on the use of the “brain” workaround artifact, revealed (1) the typical use during nominal workflow; (2) the extent of use; (3) the format, size, layout, and permanence; (4) the information content; and (5) the meaning of handwritten updates and annotations.
Demographics of Observed Nurse Participants
On each of the four units, five nurses were observed on two separate occasions. On the second observation for one of the nurses, there were no patients under her care because she had charge nurse duties, and so that observation is not included in the analysis. One other nurse had charge nurse duties during one observation with a reduced assignment of four patients, so those data are included in the analysis. Therefore, there was a total of 39 total observations of 20 nurses. Twenty-nine observations were conducted during the first 4 hr of the day shift (7:00 a.m.–11:00 a.m.), with the remaining 10 during night shift (7:00 p.m.–11:00 p.m.). The majority of nurse participants were female (85%) and White (85%). Fourteen participants were under 40 years old, five were between 40 and 60 years old, and one was above 60 years old. According to Data USA (2017), the study participant population was generally representative of the nursing population in the United States, although somewhat younger, with more males, and less racially diverse. The observations totaled 156 hr. Across the 39 observation sessions, there were 161 patients seen by the nurses, with an average of four patients per RN (range = 3–5) and an average of 40 patients per hospital unit (range = 30–49).
Typical Use of “Brain” During Nominal Workflow
The typical use of “brains” occurred during shift change handover and during direct patient care provision. When nurses arrived on the unit before their shift, patient assignments were available on unit paperwork and on the unit whiteboard. Based on the assignment, patient identifier information could be used to confirm identifiers used on a “brain” from the previous day, be added to a new “brain,” or, when applicable, to print EHR forms with auto-pulled information that served as the foundation for both the header and body of the “brain.” One nurse who was observed to come before the shift started to complete both the header and body content of the brain for all of her patients based on accessing information in the EHR, using a solely handwritten format.
The nominal workflow sequence of activities for all units began with a nursing huddle. The charge nurse ran nursing huddles with all of the incoming nurses at once, who provided high-level verbal summaries of a subset of the patients on the unit, who were of particularly high concern. For example, patients who had Do Not Resuscitate (DNR) status, were a high fall risk, or had bed exit alarms were discussed. Administrative updates were also provided during nursing huddles. Typically, unless the nurse had previously cared for the patient the day before, the nurses filled in the “brain” for the first time during the nursing huddle based on the verbal updates, as well as based on accessing the EHR on shared computers at the nursing station during the huddle. The nurses first added patient identification information to the header, followed by adding the categories of information in dedicated locations on the page with empty spaces where information would be added later. Following the nursing huddle, the shift change report was conducted verbally with the outgoing and incoming nurse directly responsible for the care of assigned patients. During the handover, the outgoing nurse used their “brain” as the primary resource to provide the verbal update, and the incoming nurse added to their “brain” by handwriting information while facing the other nurse. Following handovers, there were care provision activities for individual patients. These care activities included assessments, medication administration, dressing changes, and clinical procedures. Each nurse continued to refer to and update “brains” while providing care during the first 4 hr of their shift, including jotting notes for documentation in the EHR at a later time.
Extent of Usage of “Brain” Artifact
Most (19/20; 95%) of the nurses employed the “brain” workaround artifact to support the shift change handover and nursing work during the subsequent shift. In contrast, one (5%) of the nurse participants used the first summary page of the intended artifact to support the nursing handover at the shift change. Even in this situation, the intended report to support the shift change was 6 to 8 printed pages per patient, and the study participant only printed and used the first printed page for each patient. For all 161 patients, all nurses personally created and used an individualized paper-based artifact as their primary cognitive artifact. Most (15/20) of the nurses referred unprompted to the artifact as a “brain,” and some (5/20) referred to the artifact as a “report sheet.” Nearly all (19/20) nurses added or updated content on the artifact during the verbal shift report. One nurse, who was above 60 years old, arrived before the shift started to create a “brain” for all assigned patients. On only two occasions, the EHR was accessed by nurses during the 4-hr observation period to update the “brain” other than during the nursing huddle, in both cases for one patient each. In both cases, the nurse was adding information to the “brain” from EHR data following the handover. It was observed that nurses repeatedly wrote information in predefined spaces on their “brain,” as well as making jots on the empty space in the margin to enter the information later in the EHR. Although not directly observed, it is assumed that all nurses pursued this strategy for EHR documentation on the basis of the content included on the “brain.” For example, food administered to patients came with paperwork that had the number of calories for the meal; nurses would typically handwrite the estimated number of calories eaten on the “brain.” This went into either a section titled I&O (intake and output) or in a margin, and then later documented in the EHR.
Format, Size, Layout, and Permanence of “Brain” Artifact
The findings regarding the format and layout of the “brain” artifacts are displayed in Table 1. There was little variability across the four units, no detected variation across the two observations in how each nurse constructed and used their “brain” except when they were assigned administrative charge nurse duties in addition to patient care, and little variation across patient types. Therefore, the data are reported in the aggregate for all patients across all observations for all 20 nurses. The results are reported solely by nurse because their findings are mostly consistent across observations and patients. Three formats were identified for all of the participants: (1) exclusively handwritten on blank white paper; (2) handwritten content and annotations on either a personal printed form created in a word processing package, with category headers but no detailed data for the individual patient, or one of several forms previously developed and available on the unit, and generated collaboratively by the unit staff; and (3) handwritten annotations on a printed EHR report, which in one case was the intended report to support the nursing shift change and in another case was a report intended to support the treatment team handover (where the report was titled “a sign-out report” because it was designed primarily for physician use). Typically, there was one patient per page on the front side, but some had four patients on a single page on both the front and back sides of the page. In addition, another type of “brain” was a blank form which was printed from a word document saved on the computer or a photocopy of blank form and filled in by hand. These forms were observed to be used informally and were informally available to all the nurses on the unit. The only organizationally approved form used was an EHR printout which was multiple pages in length per patient, with the only observed use was by a charge nurse performing shift nursing duties.
TABLE 1:
Format, Size, Layout, and Permanence of “Brain” Artifact Reported by Nurse Participant
| Category | Type | Nurse Participant Total (%) |
|---|---|---|
| Format of empty “brain” | Blank paper | 12/20 (60) |
| Printed form | 7/20 (35) | |
| Printed report from EHR | 1/20 (5) | |
| Format of filled-in “brain” | Handwritten data in structured spaces and empty space during the shift change verbal report on new “brain” or “brain” used during prior shift caring for patient | 20/20 (100) |
| Handwritten annotations in structured spaces and empty space throughout the shift | 20/20 (100) for 34/161 (21) patients | |
| Size: Number of patients per page | 1 | 9/20 (45) |
| 2 | 6/20 (30) | |
| 3 | 4/20 (20) | |
| 4 | 1/20 (5) | |
| Layout: Number of sides (front or front and back) | 1 | 7/20 (35) |
| 2 | 13/20 (65) | |
| Layout: Header with patient identifiers | Upper left corner | 19/20 (95) |
| Upper right corner | 1/20 (5) | |
| Layout: Body with patient data | Below patient identifiers | 20/20 (100) |
| Permanence | Destroyed after patient discharge | 20/20 (100) |
Note. EHR = Electronic Health Records.
Information Content in Header of the “Brain” Artifact
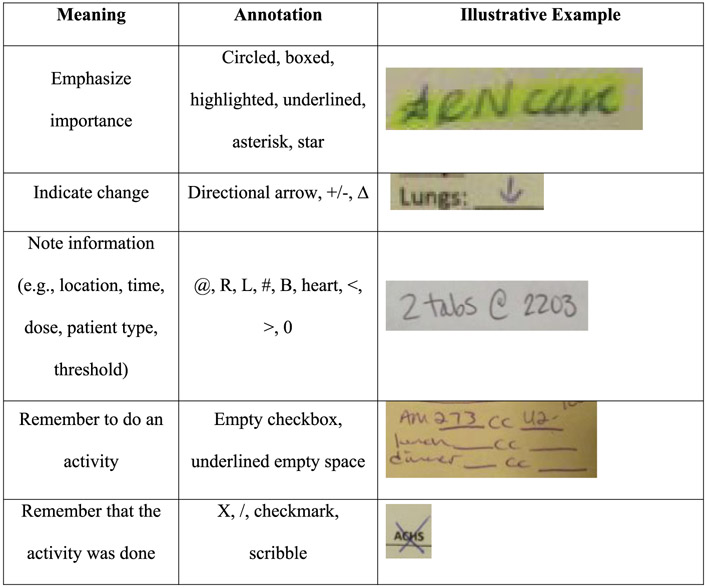
The interrater agreement was confirmed to be acceptable (Cohen’s kappa = 0.94) using the codebook for content categories on the “brain.” We divided the analysis into content included in the “header” and “body” of the “brain.” All of the “brains” included a header which was unique to the patient (see Sarkhel et al., 2018, for the characteristics of a good and bad header design based on multiple raters analyzing the “brain” headers). The header is defined as the information displayed in an area at the top of the page, visually separated with white space or a line from the remaining body content, which included patient identifier information and other patient information deemed of high importance by the nurse. The header was usually located at the top in the upper left for all but one participant; the one nurse who had the header on the upper left used an EHR printout intended to support physicians titled “Sign Out Report for Treatment Team,” which had the header on the upper right. In Figure 1, the frequency of the information contained in the headers is displayed. All nurse participants used the room number to identify patients, most (95%) of whom had this information first in the upper left-hand corner. A majority of participants (>50%) had patient name, patient age, code status, and consult physician name in the header. The least frequently included information would only apply to patients: the name of the sitter assigned to a patient that is confused, agitated, or suicidal, and patients under contact isolation precautions who have different care procedures to prevent the spread of infections through contact. Gender was infrequently included as an identifier, and the Medical Record Number (MRN) and Social Security Number (SSN) were not included on any “brain.”
Figure 1.
Information content categories in “brain” header ordered by the proportion of participants.
Information Content in Body of the “Brain” Artifact
The body of the “brain” is defined as the patient information which was not in the header of the “brain” and was physically separated from the header. Table 2 shows the proportion of the content categories placed in the body of the “brain” by nurses, as well as the frequency in which those categories were updated during the observation period. Although there was some variation by patient in content, the body information was usually structured in the same way for every patient, and in some cases, categories not relevant to a particular patient had the standing titles and locations for information included, and then crossed out (e.g., with an X).
TABLE 2:
Information Content Categories and Descriptions for “Brain” Body Reported by Percentage of Nurses and Patient With Updated Information During Observed Time Periods
| Category of Body Content |
Description | Total Out of 20 Nurse Participants (%) |
Total Updated Out of 161 Patients (%) |
|---|---|---|---|
| “As needed” medications | PRN medications and schedule | 17 (85) | 2 (1) |
| Past medical history | Diagnoses or problems, past events | 16 (80) | 11 (7) |
| Intake and output | Fluid intake and output, drains | 14 (70) | 8 (5) |
| Lab results | Results from ordered tests | 11 (55) | 23 (14) |
| Scheduled medications | Names, dose, and/or frequency of ordered medications | 10 (50) | 21 (13) |
| Body system status | Respiratory, cardiac, skin (integumentary), GI, GU, neurological | 7 (35) | 34 (21) |
| Allergies | Allergies | 6 (30) | 0 (0) |
| Anticipated care activities | Anticipated or ordered new procedures (e.g., MRI, surgery) | 6 (30) | 13 (8) |
| Assessment findings and vital signs | Findings from nursing assessments and vital sign data |
4 (20) | 28 (17) |
| To-do list | Planned tasks | 3 (15) | 34 (21) |
| Contact information | Phone numbers for hospital staff | 0 (0) | 8 (5) |
| Family | Notes about family or patients | 0 (0) | 4 (3) |
| Miscellaneous | Uncategorized jotted information in margins or empty space | 8 (40) | 19 (12) |
Note. PRN = pro re nata; GI = gastrointestinal; GU = genitourinary; MRI = magnetic resonance imaging.
The most frequent content category in the body was PRN (“as needed”) medications and schedule, medical history, and intake and output data. During the observations, on several occasions, nurse participants were asked by several patients when a pain medication could next be taken. In addition to having the PRN medication on the “brain,” several nurses were observed to write when pain medication, which was nearly always ordered “as needed” (PRN), could next be taken by the patient on the whiteboard in the patient’s hospital room.
The most frequently updated content was system status organized by body system (respiratory, cardiac, skin, neurological, etc.), planned activities, assessment findings, vital sign data, and laboratory results. The vital sign data were usually provided verbally by the PCA working under the direction of the observed nurse even though theoretically it was available in the EHR.
Fewer nurses included scheduled medications than “as needed” PRN medication on the body of the “brain,” and updates were written on the “brain” during the observations regarding new scheduled medication information for only 14% of the patients. During observations, several nurse participants described that writing down information about scheduled medications by hand would take a long time and also that scheduled medications frequently change after physicians have completed patient rounds. Nurses were sensitive to patient safety risks for medication errors associated with including dynamically changing medication order information; several nurses mentioned they trusted the scheduled medication computer interface and barcoding system.
For the to-do list, the format, layout, and content were highly variable across nurses, but not variable at all across shifts and patients for the same nurse. Four categories for activities from the to-do list and planned activities on the “brain” were identified. Distinctions were made between scheduled and unscheduled activities, testing/procedural and other care activities, and medical orders made by other providers, such as physicians, and activities for nursing care which are under the authority of nursing personnel.
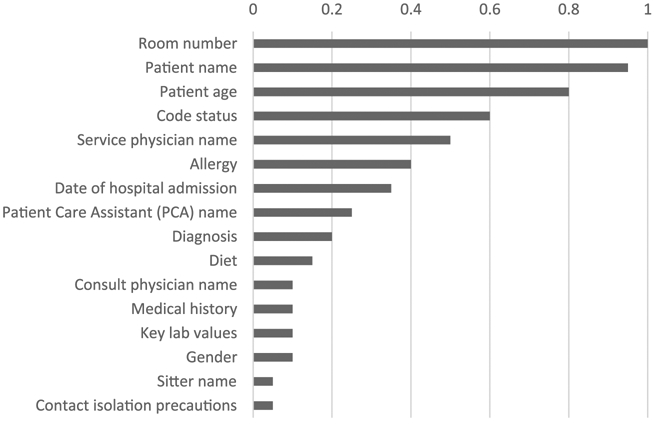
Meaning of Handwritten Annotations on “Brains”
All participants updated and annotated at least one of their patients “brains” during each observation. Many of these updates took the form of handwritten annotations. All of the annotations were exclusively grouped into categories with similar meanings. In Figure 2, the meaning of the categories of annotations used by at least 50% of the participants are reported and illustrative examples from the “brains” are provided. The inferred meaning of the categories of annotations are (1) emphasize importance such as by circling, (2) indicate change using change symbols such as a directional arrow, (3) note information using a compact shorthand such as using R to indicate the right arm for an IV site or a heart symbol for cardiac, (4) remember to do an activity such as using structured empty space with an underline mark underneath it after a field label, and (5) remember activity was done, such as by crossing out ACHS, which stands for doing a care activity AC (before meals) and HS (at bedtime).
Figure 2.
The meaning and illustrative examples of types of annotations handwritten on “brains.”
DISCUSSION
Our findings reveal that the “workaround cognitive artifact” of the “brain” continues to be extensively used by all observed nurses in all of the different observed care units in a hospital, even after a mature EHR has been implemented and in use for years. The typical practice appears to be reusing the “brain” for a patient across multiple days of care and having the verbal handover at the shift change (so-called “report”) be the primary source of information for the “body” content. These findings highlight the extreme importance of these artifacts for nurses to get their cognitive work efficiently and safely conducted. Based on both observed usage and discussions about “brains,” we posit that this externalized information about a patient has high value by aiding in “clinical immediacy.” Subsequently, we define “clinical immediacy” as a clinician being able to provide a clinical response to an expected or unexpected request for information about a particular patient without taking the valuable time logging into HIT to provide an informed response.
Similarly, the extensive use of handwritten annotations enables nurses to track and do formally and personally scheduled, clinical and non-clinical care activities. We infer that support is needed for the dynamic changes of care planning/activity management. The findings point to two primary functions for which the “brain” seems to provide superior value over the EHR and other intended systems: (1) supporting clinical immediacy with a “snapshot” overview of a patient’s status and recent changes, and (2) supporting personalized activity management with handwritten annotations on dynamic and flexible to-do lists for the shift organized by patient for both scheduled and unscheduled care/activities. These two functions were discovered to be sufficiently useful to explain the widespread usage of an informal workaround via the paper-based cognitive artifact dubbed the “brain.” The “brain” supports real-time constructing of a succinct verbal summary based on information that can be efficiently provided during a verbal update. This is accomplished not by a written narrative for the past medical history, but by nurses utilizing a set of “one line bullets” with shorthand such as “COPD, CHF” to indicate chronic obstructive pulmonary disease and congestive heart failure, respectively. Because the shorthand information annotations were found to be unique to the particular user, the person who is providing the update needs to provide an interpretation of their personal bulleted notes in the form of a verbal narrative summary typically occurring during shift change handover. In addition, handwritten annotations can serve as updates of a patient’s status at the beginning of a shift, which is expected to help tailor an update to a nurse who has cared for this patient previously and is familiar with the patient.
Second, the “brain” is used to aid in activity management. Planned activities were typically checked off or scribbled through as soon as they were completed. Outcomes of activities that needed to be documented at a later time in the EHR were placed in predefined sections or jotted in the margins of the body of the “brain.” Particularly important activities were highlighted, with stars, underlines, and asterisks. With the annotations, the scribbles and crossouts typically did not cover up the original information, thus enabling viewing it even after it was done; this approach supported easily incorporating information about what activities were completed during the shift. Although there was functionality in the EHR that supported tracking the completion of formally ordered and scheduled activities, nurses were not allowed to add their own activities to the list, and particularly non-clinical activities. In addition, it was not possible to view easily which activities were completed already in a spatially dedicated layout with similar activities which have not yet been completed.
“Brains” are most likely used as a workaround because what the nurses are provided in the EHR and associated HIT currently is not adequate for them to meet their work requirements in a timely, effective, and efficient manner, and thus not adequately designed for WAD. This study confirms prior findings that nurses prevalently access paper-based “brain” artifacts (which are not formally sanctioned by hospitals) secondary to their need for both immediate physical access while in a patient’s room to summarize information and to track the completion of planned tasks (Blaz et al., 2016; Staggers & Jennings, 2009).
Based on these findings, it is expected that having a paper-based report printed from the EHR tailored to a type of patient (cardiac, burn, etc.) would be useful. As with any similar intervention, the choice of hardware, training, installation, implementation, policy, software design, and report design would impact the usefulness of this approach. In this study, the EHR provided a printed summary which could be dozens of pages long; this length contributed to it being perceived as a burden as opposed to a cognitive artifact that supports clinical immediacy. Therefore, we recommend nothing longer than a onesided page per patient, including a bar code or QR code that can be easily scanned to automatically open the appropriate patient’s chart in the EHR. Presumably, there would be flexibility to tailor the specific information layout and label to the unit’s and/or nurse’s needs. The printout could have auto-populated information that would be used as the basis for handwritten annotations with a pen during the shift change report, such that it supports activity management and clinical immediacy. In the future, print-outs can align the format with how nurses organize their “brains” with standardized location for patient identification and enough blank space to allow handwritten additions.
The results of this study provide detailed insights for EHR and future HIT, such as smartphone-based consumer application designers to innovate more easily accessible overviews of clinical data in tailored formats for specific objectives. Every nurse working on the units where the observations took place used paper-based cognitive artifacts. Understanding the value and usage of these artifacts can inform HIT design and implementation so that it can be more closely connected to a user’s workflow and more directly provide benefit to end users (Lowry et al., 2012). If nurses find HIT sufficiently useful to transition from paper-based to electronic artifacts, secondary users, such as researchers and attending physicians, can benefit from increased information in an electronic format and from the potential analytics capabilities it provides. For example, the following three suggestions are ways designers could leverage what was learned from this study and implement it: (1) auto-populating patient information into a “snap-shot” view that presents as the landing page for the selected patient and matches format, layout, and content found on the “brains” that is printable to at most a single page per patient; (2) allowing space for informal, shortterm, personal notes or adding annotation features, and (3) providing a program or application that allow nurses to easily design an electronic “brain” that auto-populates the selected data. Similarly, the vast majority of attending physician supervisors have been found to remotely monitor and act upon information to improve care which would not otherwise have been detected with the opportunities provided by remote real-time access via the EHR (Martin, Tulla, Meltzer, Arora, & Farnan, 2017). A remotely monitored supervisory function could similarly be performed with nursing administrators in that nurse managers could review the data from “brains” of junior nursing personnel to identify training.
Although the “brain” was highly useful, some potential risks were observed with its use which could be proactively mitigated. Nurses infrequently updated the “brain” information with data from the EHR except for at the beginning of the shift, and supplemented based upon the verbal report information from the outgoing nurse while using their own “brain.” Vital signs were often recorded on the “brain” during generation prior to receiving verbal reports from PCAs mid-shift; in this study, PCAs were responsible for collecting vital signs, updating the vital signs in the EHR, and verbally reporting the vital signs to the supervising nurse. Even though this was not observed in this study, one potential implication of relying upon outdated lab information could be a delay in a time-critical diagnosis, such as sepsis, due to a reduction in situation awareness (Patterson, Militello, Su, & Sarkar, 2016). In prior research, achieving situation awareness was identified to be the most important factor in detecting that a patient is deteriorating (Massey, Chaboyer, & Anderson, 2017). Although nurses do not diagnose directly, their assessment information is critical to physicians making a timely diagnosis because they are at the bedside frequently, and in general, many clinical staff rely upon verbal interactions with nurses to obtain patient updates (Brown, Borowitz, & Novicoff, 2004).
Other potential unintended consequences of heavy reliance on “brains” could be the inadvertent disclosure of protected patient information on sheets that are used across shifts, although no evidence was found that this was an issue in this study. When the patient was no longer expected to be cared for by the same nurse on the next day, typically due to the nurses upcoming work schedule or the patient being discharged, many nurses seemed to already be mitigating this risk by keeping “brains” in locked lockers overnight on the unit and shredding the “brains” papers by placing them in secure bins with patient-protected information that was later shredded. Another consequence could be that documentation in the EHR is delayed and thus information used by other clinical and non-clinical personnel is delayed or incorrect. Although not observed directly, it seems likely that not all of the relevant information on the “brain” was entered into the formal EHR documentation for the patient prior to disposing of the “brain.” Finally, and arguably most importantly, there is an opportunity cost of having each nurse spend 10 to 40 min at the beginning of each shift to generate the “brain” for each patient. On the contrary, it is hypothesized that it would actually take longer to access the information real-time when needed via the EHR unless auto-population of the data from the EHR was utilized. Layout design and operational improvements in EHR usability could potentially make it easier to review clinical summaries or auto-populated information. It is noteworthy that at least one nurse routinely arrived 40 min prior to the start of her shift to generate a handwritten “brain” per patient based on data pulled from the EHR before the handover. Time lost to the construction of “brain” artifacts at the beginning of each shift may also reduce time available to provide “hands-on” care to patients. Less time during a shift for a nurse is negatively correlated with patient outcomes (Kane, Shamliyan, Mueller, Duval, & Wilt, 2007).
There are limitations to this study. Only four clinical units from two hospitals with 20 nurses using one EHR system with highly similar hardware choices, facility implementation approaches, policies and procedures, and training paradigms participated in this study. Nevertheless, the observed EHR is widely used by other hospitals and prior research, which adds to the ability to generalize our and others’ findings beyond a single unit or hospital. Although we observed how long it took to construct and update a brain on a patient, we could not compare that with the time it would take to view or document all the data in the EHR because this did not occur during the observation periods. In addition, the methodology employed did not definitively determine the best explanation for the finding that scheduled medications were not included on most of the “brains.” These results have informed the grounded theory approach that was generated, but evaluation of scheduled medications needs to be replicated to move from the local documented experience to the general work environment of nurses. In addition, although other health care professionals, such as physicians, are known to use handwritten notes during care provision and documentation in the EHR, we did not study the value and usage of other care provider’s handwritten cognitive artifacts. Similarly, additional research would be needed to determine if health care professionals in complex domains with extensive navigation behind the “keyhole” of a computer screen might similarly benefit from the use of paper, whiteboards, and large-screen displays to provide overviews of summary information and reminders for planned tasks.
CONCLUSION
Previous research has shown the persistence of personally generated paper-based “brain” cognitive artifacts. In health care, these artifacts have become essential in supporting the WAD for nurses in hospitals with current HIT. Our analysis of these artifacts can inform future design of HIT by providing supporting patient information such that it aligns with the nurses’ WAD and incorporating preferences by providing a patient “snapshot” view, and minimizes navigation.
Support Clinical Immediacy and Activity Management
HIT in the dynamic, time-pressured hospital environment, with roles distributed across specialized expertise, needs to support nurses with the following:
Immediate access to a “snapshot” overview of a patient’s history, current status regarding diagnostic certainty and treatment plan, and deviations from typical patients
The ability to respond to a request for information from another care provider or for receiving pain medication by a patient without turning a nurse’s back to the requester to access the EHR
The ability to succinctly provide a routinized verbal summary during a shift change handover, which emphasizes important information, significant changes that occurred during the shift, and planned activities that still need to be completed by the oncoming practitioner
The ability to quickly take handwritten notes in coded shorthand during a handover to support sense-making about the patient’s status and the relationship of the patient’s status to the other patients under the care of the nurse
The ability to plan formally ordered activities by a physician, self-identified activities, clinical activities, and non-clinical activities for a single patient in an integrated to-do list that is structured by a systematic approach to prioritizing, completing, documenting, and communicating the state of completion of the activities
ACKNOWLEDGMENTS
This research was supported by an Agency for Healthcare Research and Quality (AHRQ) grant (P30HS024379), the Institute for the Design of Environments Aligned for Patient Safety (IDEA4PS) Center. The views are those of the authors and not necessarily those of AHRQ.
Biography
Austin F. Mount-Campbell is a senior clinical researcher and human factors engineer at the Value Institute of the Christiana Care Health System. He received his BS and MS in industrial engineering and PhD at the School of Health and Rehabilitation Sciences at The Ohio State University. His research interests are human factors and informatics.
Kevin D. Evans is a professor at The Ohio State University’s College of Medicine and the School of Health and Rehabilitation Sciences. He received his undergraduate and graduate degrees at The Ohio State University. His doctoral degree was focused on geriatrics and gerontology. He has extensive clinical practice experience having managed and worked clinically for 25 years. His research interests are in the use of image analysis and sonographic contrast agents to enhance the detection of musculoskeletal disorders.
David D. Woods is a professor in the Department of Integrated Systems Engineering at The Ohio State University. He obtained a PhD in cognitive psychology in 1979 from Purdue University. His research interests are how to design new systems to help people find meaning in large data fields when they are under pressure to diagnose anomalies and re-plan activities, and more recently how to model and measure the adaptive capacities of organizations and distributed systems.
Esther M. Chipps is a clinical nurse scientist and an associate professor of clinical nursing at The Ohio State University. She received her BSN from Columbia University, and MS and PhD in nursing from The Ohio State University. Her research interests are in the nursing practice and work environment.
Susan D. Moffatt-Bruce is a professor in the Department of Surgery and Department of Biomedical Informatics in the College of Medicine at the Ohio State University. She obtained her MD in 1994 from Dalhousie University, her PhD in 1999 from the University of Cambridge, and her MBA in 2016 from The Ohio State University. She is trained in both general surgery (Dalhousie 2001) and cardiothoracic surgery (Stanford University 2004). Her research focuses on how feedback of information can be used to inform the development of robust practices that lead to improved patient safety.
Emily S. Patterson is an associate professor in the Division of Health Information, Management and Systems at the School of Health and Rehabilitation Sciences at The Ohio State University. She received a BS in industrial engineering from University of Illinois Urbana–Champaign and a PhD in integrated and systems engineering from The Ohio State University. Her research interests are human factors, patient safety, and informatics.
Contributor Information
Austin F. Mount-Campbell, Christiana Care Health System, USA
Kevin D. Evans, The Ohio State University, USA
David D. Woods, The Ohio State University, USA
Esther M. Chipps, The Ohio State University, USA
Susan D. Moffatt-Bruce, The Ohio State University, USA
Emily S. Patterson, The Ohio State University, USA
REFERENCES
- Alter S (2014). Theory of workarounds. Communications of the Association for Information Systems, 34, 1041–1066. [Google Scholar]
- Beyer H, & Holtzblatt K (1998). Contextual design: Defining customer-centered design. San Francisco, CA: Elsevier. [Google Scholar]
- Blaz JW, Doig AK, Cloyes KG, & Staggers N (2016). The hidden lives of nurses’ cognitive artifacts. Applied Clinical Informatics, 7, 832–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown PJ, Borowitz SM, & Novicoff W (2004). Information exchange in the NICU: What sources of patient data do physicians prefer to use? International Journal of Medical Informatics, 73, 349–355. [DOI] [PubMed] [Google Scholar]
- Charmaz K (2008). Constructionism and the grounded theory method In Gubrium JF & Holstein J (Eds.), Handbook of constructionist research (Vol. 1, pp. 397–412). New York, NY: Guilford Publications. [Google Scholar]
- Clancy TR (2010). Diamonds in the rough: Positive deviance and complexity. Journal of Nursing Administration, 40, 53–56. [DOI] [PubMed] [Google Scholar]
- Data USA. (2017, December 22). Registered nurses. Retrieved from https://datausa.io/profile/soc/291141/#demographics
- Gurses AP, Xiao Y, & Hu P (2009). User-designed information tools to support communication and care coordination in a trauma hospital. Journal of Biomedical Informatics, 42(4), 667–677. [DOI] [PubMed] [Google Scholar]
- Hardey M, Payne S, & Coleman P (2000). “Scraps”: Hidden nursing information and its influence on the delivery of care. Journal of Advanced Nursing, 32, 208–214. [DOI] [PubMed] [Google Scholar]
- Hollnagel E, Braithwaite J, & Wears RL (Eds.). (2013). Resilient health care. Aldershot, UK: Ashgate Publishing. [Google Scholar]
- Hollnagel E, & Woods DD (2005). Joint cognitive systems: Foundations of cognitive systems engineering. Boca Raton, FL: CRC Press. [Google Scholar]
- Kane RL, Shamliyan TA, Mueller C, Duval S, & Wilt TJ (2007). The association of registered nurse staffing levels and patient outcomes: Systematic review and meta-analysis. Medical Care, 45, 1195–1204. [DOI] [PubMed] [Google Scholar]
- Lowry SZ, Quinn MT, Ramaiah M, Schumacher RM, Patterson ES, North R, … Abbott P (2012). Technical evaluation, testing and validation of the usability of electronic health records (NIST Technical Report NISTIR 7804). Washington, DC: Information Services Office. [Google Scholar]
- Martin SK, Tulla K, Meltzer DO, Arora VM, & Farnan JM (2017). Attending physician remote access of the electronic health record and implications for resident supervision: A mixed methods study. Journal of Graduate Medical Education, 9, 706–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massey D, Chaboyer W, & Anderson V (2017). What factors influence ward nurses’ recognition of and response to patient deterioration? An integrative review of the literature. Nursing Open, 4(1), 6–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLane S, Esquivel A, & Turley J (2009). Developing a taxonomy and an ontology of nurses’ patient clinical summaries. Studies in Health Technology and Informatics, 146, 352–357. [PubMed] [Google Scholar]
- Norman DA (1991). Cognitive artifacts In Carroll JM (Ed.), Cambridge Series on Human-Computer Interaction, No. 4. Designing interaction: Psychology at the human-computer interface (pp. 17–38). New York, NY: Cambridge University Press. [Google Scholar]
- Patterson ES (2018). Workarounds to intended use of health information technology: A narrative review of the human factors engineering literature. Human Factors, 60(3), 281–292. [DOI] [PubMed] [Google Scholar]
- Patterson ES, Militello LG, Su G, & Sarkar U (2016). Characterizing a naturalistic decision-making phenomenon: Loss of system resilience associated with implementation of new technology. Journal of Cognitive Engineering and Decision Making, 10, 229–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson ES, Rogers ML, Tomolo AM, Wears RL, & Tsevat J (2010). Comparison of extent of use, information accuracy, and functions for manual and electronic patient status boards. International Journal of Medical Informatics, 79, 817–823. [DOI] [PubMed] [Google Scholar]
- Perry SJ, & Wears RL (2012). Underground adaptations: Case studies from health care. Cognition, Technology & Work, 14, 253–260. [Google Scholar]
- Randell R, Wilson S, Woodward P, & Galliers J (2011). The ConStratO model of handover: A tool to support technology design and evaluation. Behaviour & Information Technology, 30, 489–498. [Google Scholar]
- Rayo MF, Mount-Campbell AF, O’Brien JM, White SE, Butz A, Evans K, & Patterson ES (2014). Interactive questioning in critical care during handovers: A transcript analysis of communication behaviours by physicians, nurses and nurse practitioners. BMJ Quality & Safety, 23, 483–489. [DOI] [PubMed] [Google Scholar]
- Saleem JJ, Russ AL, Justice CF, Hagg H, Ebright PR, Woodbridge PA, & Doebbeling BN (2009). Exploring the persistence of paper with the electronic health record. International Journal of Medical Informatics, 78, 618–628. [DOI] [PubMed] [Google Scholar]
- Sarkhel R, Socha JJ, Mount-Campbell A, Moffatt-Bruce S, Fernandez S, Patel K, … Patterson ES (2018, June). How nurses identify hospitalized patients on their personal notes: Findings from analyzing “brains” headers with multiple raters In Proceedings of the International Symposium on Human Factors and Ergonomics in Health Care (Vol. 7, No. 1, pp. 205–209). New Delhi, India: SAGE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarter NB, & Woods DD (1995). How in the world did we ever get into that mode? Mode error and awareness in supervisory control. Human Factors, 37, 5–19. [Google Scholar]
- Staggers N, & Jennings BM (2009). The content and context of change of shift report on medical and surgical units. Journal of Nursing Administration, 39, 393–398. [DOI] [PubMed] [Google Scholar]
- Woods DD (2006). Essential characteristics of resilience In Hollnagel E, Woods DD, & Levson N (Eds.), Resilience engineering: Concepts and precepts (pp. 21–34). Aldershot, UK: Ashgate Press. [Google Scholar]
- Woods DD, & Hollnagel E (2006). Joint cognitive systems: Patterns in cognitive systems engineering. Boca Raton, FL: CRC Press. [Google Scholar]
- Xiao Y, Kiesler S, Mackenzie CF, Kobayashi M, Plasters C, Seagull FJ, & Fussell S (2007). Negotiation and conflict in large scale collaboration: A preliminary field study. Cognition, Technology & Work, 9, 171–176. [Google Scholar]