Obesity
Surgery,
5, 61-64
Gastric Banding for Treatment
Preliminary
Results
G. Bajardi;
M. Florena
G. Ricevuto;
G. Mastrandrea;
of Morbid
G. Pischedda;
Obesity:
D. Valenti;
G. Rubino;
Departmenf of Surgical and Anatomical Sciences,Division of General and Vascular Surgery, University of
Palermo, Palermo, Italy
Background:
gastric
banding
(GB)
has been
used
for
treatment
of morbid
obesity.
Methods:
a banding
device,
introduced
by Broadbent
and consisting
of a self-blocking
nylon
strip covered
with a silicone
tube, was used in 13
patients
who
have
completed
l-year
follow-up.
This
device
was used for its mechanical
properties,
biocompatibility,
ease of insertion
and low cost. Results:
at 1 year,
mean
excess
weight
loss was 51.6%,
with all but one
patient
losing
more than 25% of excess
weight.
Associated illnesses
resolved.
There
were
two complications
(15%):
one
patient
required
band
removal
for selfinduced
vomiting
and
one patient
required
repair
of
an incisional
hernia.
Conclusions:
GB has had good
results
thus far. Reported
differences
depend
on materials,
stoma
diameter,
pouch
size,
and
developing
techniques.
Key
words:
surgery
Morbid
obesity,
gastric
banding,
bariatric
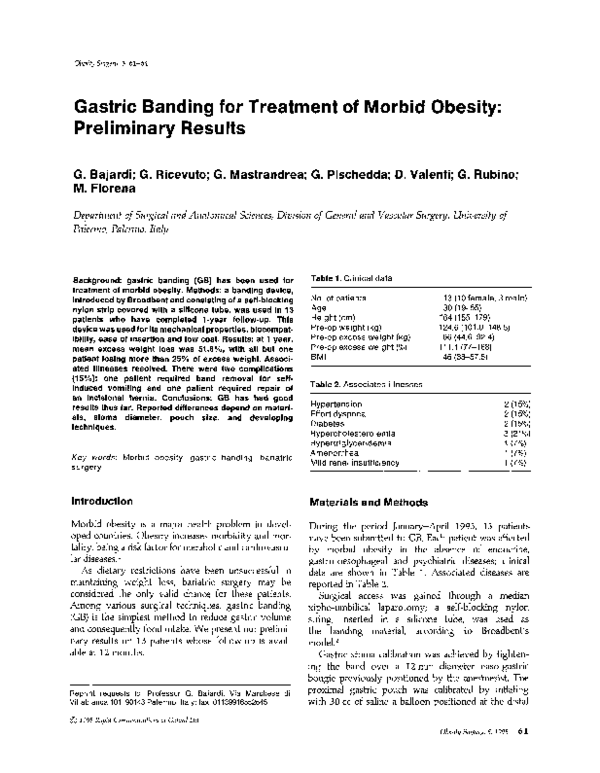
Table
1. Clinical
No. of patients
Age
Height
(cm)
Pre-op
weight
Pre-op
excess
Pre-op
excess
BMI
Table
data
(kg)
weight
weight
2. Associated
(kg)
(%)
13 (10 female,
30 (19-55)
164 (155-179)
124.6 (lOl.rS148.5)
66 (44.8-92.4)
111.1 (77-168)
46 (38-57.5)
3 male)
illnesses
Hypertension
Effort dyspnea
Diabetes
Hypercholesterolemia
Hypertriglyceridemia
Amenorrhea
Mild renal insufficiency
2
2
2
3
1
1
1
(15%)
(15%)
(15%)
(21%)
(7%)
(7%)
(7%)
Introduction
Materials
Morbid obesity is a major health problem in developed countries. Obesity increasesmorbidity and mortality, being a risk factor for metabolic and cardiovascular diseases.l
As dietary restrictions have been unsuccessful in
maintaining weight loss, bariatric surgery may be
considered the only valid chance for these patients.
Among various surgical techniques, gastric banding
(GB) is the simplest method to reduce gastric volume
and consequently food intake. We present our preliminary results on 13 patients whose follow-up is available at 12 months.
During the period January-April 1993, 13 patients
have been submitted to GB. Each patient was affected
by morbid obesity in the absence of endocrine,
gastro-oesophageal and psychiatric diseases;clinical
data are shown in Table 1. Associated diseasesare
reported in Table 2.
Surgical access was gained through a median
xipho-umbilical laparotomy; a self-blocking nylon
string, inserted in a silicone. tube, was used as
the banding material, according to Broadbent’s
model.2
Gastric stoma calibration was achieved by tightening the band over a 12 mm diameter naso-gastric
bougie previously positioned by the anesthesist.The
proximal gastric pouch was calibrated by inflating
with 30 cc of saline a balloon positioned at the distal
Reprint
requests
to: Professor
Villabianca
101, 90143 Palermo,
0
1995 Rapid
Communications
G. Bajardi,
Via Marchese
Italy; fax: 01139916552645
of Oxford
di
and Methods
Ltd
Obesity Surgery, 5, 1995
61
�B~jmdi
et al.
Table
3. Weight
loss
after
GB
EW (kg)
At surgery
1st p.o. month
6th p.o. month
12th p.o. month
63.3
53.3
40.6
31.1
EWL
(%)
17.0
36.8
51.6
WL (kg)
BMI
11.0
23.7
33.2
46.0
42.5
37.4
34.3
EW = excess
weight;
EWL = excess
weight
loss:
loss; BMI = body mass index;
p.o. = post-operative.
Table
4. Weight
loss - literature
EWL
= excess
weight
= weight
results
EWL
Favretti
et ZI/.‘~
Kuzmak”
Forsell
et a/.’
Lovig et a/.’
Lovig et al.7
Kirby et a1.9
WL
56
80
5.5
74
38
54
(%)
Follow-up
12
10
12
12
60
12
months
months
months
months
months
months
follow-up. A functional gastric stoma stenosis at the
seventh post-operative
month caused band removal
(7%); this patient used self-induced vomiting during
the early post-operative
period. After band removal,
no other bariatric surgery attempt was made on this
patient as weight loss achieved was judged satisfactory by herself, and she is being followed. We observed an incisional hernia (7%) at the fourth postoperative month, which was successfully repaired.
No vitamin or other nutrient deficiency has been
registered during the follow-up period. Hemoglobin,
iron, electrolites and proteins were in normal range at
the scheduled samples. The pre-operative
elevated
levels of cholesterol, triglycerides
and blood sugar
always corrected after surgery. In a patient who had
longstanding
amenorrhea pre-operatively,
a normal
ovulatory cycle restarted after the second post-operative month.
loss
Discussion
end of the bougie, immediately below the cardia and
proximal to the band.
Antithrombotic
prophylaxis
was accomplished in
each patient using intra and post-operative
lower
limbs elastic bandage, and early post-operative mobilization. On the third post-operative
day a barium
swallow was given to view gastric pouch emptying
and gastric stoma patency. On the fourth post-operative day a low calory liquid diet was started (50 cc
per day). From the seventh post-operative
day until
the sixth week, a semi-solid diet was advised, and
patients were invited to self-regulate the amount of
food intake according to the sensation of satiety.
After the sixth post-operative
week, a free diet was
allowed.
Results
No early morbidity or mortality occurred. Each patient
was seen at the first, third, sixth and 12th post-operative month.
As shown on Table 3, the highest weight loss was
achieved during the first 6 months; in this period
mean weight loss was 23.7 kg, corresponding
to
36.8% of pre-operative
excess weight. During the
second 6-month period, weight loss has been slower
with tendency to stabilization. At the end of 1 year,
mean weight loss was 32.2 kg, equal to 51.6% of
mean pre-operative excess weight. In only one patient,
weight loss (25% of pre-operative excess weight) was
judged unsatisfactory.
No major late complications were found during
62
Obesity
surgery,
5, 199s
Since its early proposal by Molina3 and K011,~ GB
appeared to be a simple and safe technique, able to
induce a sensible weight loss in morbidly obese patients. Minimal surgical trauma, as well as maintenance
of gastro-enteric
integrity, made this technique fully
reversible. These characteristics led us to use GB as
an alternative to biliopancreatic
diversion
(BPD),
which we had performed since 1990.~
Our preliminary results show at 12 months an
excess weight loss of 51.6%,
with a residual obesity
expressed by a mean BMI of 34.3; these findings are
similar to those reported by others (Table 4). Unfortunately, these data are difficult to compare because of
lack of standardization
of some key steps in this
technique such as gastric pouch and stoma calibration.
Some authors have stressed the high percentage of
complications and revisions.g,ll This may be due to
variability in this technique regarding some markpoints like banding material, stoma diameter, gastric
pouch volume, and whether the whole system will
keep the configuration imposed by the surgeon during
the implant.
We had a late complication rate of 15%; for both of
these patients surgery was necessary, to remove a
band in one and repair an incisional hernia in the
other. More serious complications,
however,
have
been experienced by other workers.
Among nonspecific reported complications, wound
infections (5.7%) and incisional hernias (8.6-10%)
are
the commonest, followed by deep vein thrombosis
(DVT) (1.7%) and p u 1monary complications (Table 5).
Among specific complications, the most frequently
�Gastric
Table
5. Non-specific
Favretti
Kuzmak
Sjoberg
Lovig et
Table
et a/.13
et a/.“’
et a1.6
al.7
6. Specific
Favretti
Kuzmak
Sjoberg
Lovig et
Granstrom
complications
eta/.13
et aI.”
et a/.6
a/.’
et al.”
4.6%
5.3%
17.0%
18.3%
complications
Early
Late
3.4%
2.7%
5.4%
3.6%
4.1%
12.7%
10.6%
13.6%
25.9%
29.1%
Re-operations
22.6%
9.2%
20.0%
14.9%
31.9%
reported are stoma1 stenosis (with or without pouch
dilatation), pouch perforation and band erosion into
the gastric wall (Table 6); these complications determine a reintervention rate of lo-ZO%, with mortality
almost absent.6,7Insufficient weight loss (7% in our
experience) represents another reason for therapeutic
failure.
The optimal stoma diameter is considered to be
12 min;2,7,9KuzmaklO suggestsa wider stoma (13 mm)
for patients below 146 kg. Smaller diameters (11 mm)
have been reported as a cause of persistent vomiting
in 2% of patients submitted to GB.”
Granstrom,” using a Marlex mesh band, observed
16 stenoses(22%), occurring in patients whose stomas
were calibrated with 11 or 12 mm bougies. The diameter of gastric stoma is not the only determinant of
stenosis: stomas patent to a pediatric gastroscope
have been observed in patients clinically showing
persistent vomiting and excessive weight 10~s.~’Excessive food intake may lead to gastric pouch dilatation
far beyond the intraoperatively determined measure,
resulting in a stoma size insufficient for proper pouch
emptying, and responsible for a ‘functional’ stenosis.
Other complications, such as band kinking or erosion
into the stomach wall, have been correlated with the
materials employed. Marlex mesh, Dacron or PTFE
have all been considered responsible for a fibrotic
reaction by the surrounding tissuesor erosions of the
gastric wall. ‘,I1 Pouch perforation with tissue materials, although rare (1.3%), is associated with a high
morta1ity.r’
The major advantage of Broadbent’s system,’
beyond its very low cost, derives from the coupling
of the nylon string stiffness and the silicone coveringtube biocompatibility. These characteristics seem to
prove effective in preventing band dilatation, slippage
or erosion into the gastric wall.
Gastric pouch volume is the other important deter-
Banding
minant of success.Optimal volumes have variously
been reported between 30 rnll’ and 50 m1;gin another
seriesthe banding device has been passedbehind the
stomach using anatomical landmarks for band position,
like the short gastric vessels7’1’or the standard distance of 3 cm below the cardia.s Keeping correct
pouch dimensions is very important, because pouch
dilatation has been correlated with minimal weight
loss and with weight gain observed after prolonged
follow-up; 7,gfurthermore, a large gastric pouch can be
considered responsible of a functional stenosis. We
believe that pouch dimensioning is more precise using
the inflated balloon technique.
Full co-operation is required by the patient to
achieve clinically satisfying results. The patient must
be advised not to provoke vomiting, to take just
enough food to reach satiety, and not to drink highcalorie beverages. Inability to cope with these simple
recommendations must be considered a contraindication to this surgery, as results may be impaired and
severe complications may ensue.
Recently BroadbenP proposed laparoscopic positioning of his banding device. This appears to be a
very important step in preventing morbidity related
to the abdominal wall opening like incisional hernias,
a complication constantly present in every bariatric
surgery experience.
Usually, GB does not result in syndromes related
to vitamins, electrolytes and basic nutrients, but rare
reports of these complications can be found in the
literature.7 From this point of view, GB is much more
reliable than other bariatric surgery techniques, like
the BPD which we used in the past.5 However, we
await longterm weight loss results. Beneficial effects
in lowering cardiovascular risk factors have been
observed.
Conclusions
GB is effective in weight loss in morbidly obese
patients. Among the bariatric operations, it is the least
invasive, is reversible and lacks GI tract opening.
Laparoscopic positioning of the banding device will
be a further strong reason to select this technique for
surgical treatment of obesity. It is imperative that
standardization of measuresand materials is achieved
to compare different series in order to improve the
results. Patient selection is a critical step, as most
unsatisfactory results may be related to incapacity to
follow dietary recommendations.
Obesity Sqery,
5,
19%
63
�et al.
Bajardi
References
1. Drenick EJ, Bale GS, Seltzer F, et al. Excessive mortality
and causes of death in morbidly obese men. ]A&&4
1980;
243:
2. Broadbent
Surg
443-S.
R. A simple band for gastric banding. Obesity
1993;3:307-8.
Molina M,. Oria HE. Gastric banding. Program 6th
Bariatric Surgery Colloquium. Iowa City 1983, p. 15.
4. Kolle K. Gastric Banding, O.M.G.I. 7th Congress, Stockholm 1982, abstract 185, p. 37.
5. Bajardi G, Latteri AM, Ricevuto G, et al. Biliopancreatic
diversion: early complications.
Obesity Surg 1992; 2:
3.
177-80.
6. Sjoberg EJ, Andersen E, Hoe1 R, et al. Gastric banding
in the treatment of morbid obesity. Acta Chir Stand
1989;155:31-4.
7.
Lovig T, Hafner JFW, Kaaresen R, et al. Gastric banding
for morbid obesity: 5 years follow-up. Int J Obes 1993;
17: 453-7.
64
Obesity
8. Forsell P, Hallberg D, Hellers G. Gastric banding for
morbid obesity: initial experience with a new adjustable
band. Obesity Surg 1993; 3: 369-74.
9. Kirby RM, Ismail T, Crowson M, et al. Gastric banding
in the treatment of morbid obesity. Br ] Surg 1989; 76:
surgery,s, 1995
490-L
Kuzmak LI. Gastric banding. In: Deitel M, ed. Surgey
for the Morbidly Obese Patient. Philadelphia:
Lea and
Febiger, 1989,225-60.
11. Granstrom L, Backman L. Technical complication and
related reoperation
after gastric banding. Acta Ckir
Stand 1987;153:215-20.
12. Broadbent R, Tracey M, Harrington
P. Laparoscopic
gastric banding. A preliminary
report. Obesity Surg
10.
1993;
3: 63-7.
13. Favretti F, Enzi G, Pizzirani E, et al. Adjustable silicone
gastric banding (ASGB): the Italian experience. Obesity
Surg 1993;3:
53-6.
(Received 4 August
1994; accepted 15 November 19%).
�
 giuseppe pischedda
giuseppe pischedda