Review
1
Anti-endothelin drugs in solid
tumors
5
10
15
20
25
30
1.
Background
2.
Medical need
3.
Existing treatment
4.
Current research goals
5.
Scientific rationale
6.
Competitive environment
7.
Conclusions
8.
Expert opinion
Antonio Russo†, Giuseppe Bronte, Sergio Rizzo, Daniele Fanale, Nicola Gebbia
& Viviana Bazan
†
Universita` di Palermo, Section of Medical Oncology, Department of Surgical and Oncological
Sciences, Via del Vespro 129, 90127 Palermo, Italy
Importance of the field: The endothelin (ET) axis, which includes the biological functions of ETs and their receptors, has played a physiological role in
normal tissue, acting as a modulator of vasomotor tone, tissue differentiation
and development, cell proliferation and hormone production. Interestingly, it
also functions in the growth and progression of various tumors. Several
researchers have identified the blockade of the ET-1 receptor as a promising
therapeutic approach.
Areas covered in this review: The clinical investigation of an orally bioavailable ET antagonist, atrasentan, in prostate cancer, is encouraging. In this
neoplasia, it has shown antitumor activity, bone metastasis control and
amelioration of cancer-related pain but improvement in time to progression
and overall survival has still not been demonstrated. The clinical trials of other
ET antagonists are reported. Literature research was performed by Pubmed
and Pharmaprojects.
What the reader will gain: A comprehensive view about the use of atrasentan
in the treatment of castration-resistant prostate cancer (CRPC) is provided
together with the scientific rationale based on the function of ET and its
receptor in various cancer development mechanisms.
Take home message: Atrasentan seems to be active in CRPC, although
strong scientific evidence is still to be found. Interesting clinical findings
regard zibotentan.
Keywords: atrasentan, endothelins, prostate cancer, zibotentan
35
Expert Opin. Emerging Drugs (2010) 15(1):1-14
1.
40
45
50
55
Background
The endothelins (ETs), discovered by Yanagisawa in 1988, are a family of small
peptides, well conserved from the evolutionary aspect, with multiple roles in a
variety of tissues [1]. Initially, ET was thought to be important in cardiovascular
homeostasis; ET receptor antagonists and endothelin-converting enzyme (ECE)
inhibitors have, therefore, been developed mostly for the treatment of cardiovascular
diseases. Molecular biology has also provided valuable information about ET,
including evidence that the ET system plays an important role in the early
development of the neural crest and, thus, in the formation of organs [2].
At present, the ET system, which comprises ETs, their receptors and the enzymes
of ET biosynthesis and degradation, is thought to have a role in the pathophysiology
of many tumor types, including prostatic, pulmonary, cervical, endometrial, ovarian,
colorectal, breast, bladder, renal and brain tumors, Kaposi’s sarcoma, bone metastases and melanoma [3-5]. In mammals, the ETs comprise a family of three 21 aminoacid peptides, ET-1, ET-2 and ET-3, whose structure consists of a single a-helix and
two intramolecular disulfide bonds. Whereas ET-1 and ET-2 have similar structures,
ET-3 differs in structure at 6 of 21 amino acids. ET-1 is not organ-specific and is
expressed primarily by endothelial cells, whereas ET-2 is mainly present in the
10.1517/14728210903571667 © 2010 Informa UK Ltd ISSN 1472-8214
All rights reserved: reproduction in whole or in part not permitted
1
�Anti-endothelin drugs in solid tumors
56
60
65
70
75
80
85
90
95
100
105
110
intestine and kidney, and ET-3 is mainly localized in the brain
and to a lesser extent in gastrointestinal stromal cells and lung
epithelial cells [4].
The ETs are encoded by distinct genes and are regulated at
the level of mRNA transcription and post-transcription [1].
The primary translation product of the mRNA of ET-1 gene is
the 212-aa prepro-ET-1. Active ET-1 is synthesized from a
biologically inactive 38-aa precursor, Big ET-1, by an unusual
hydrolysis of the Trp21–Val22 bond by a metalloprotease
with intracellular and membrane bound isoforms, known as
the ECE-1 [6,7]. The mature peptide is continuously released
from vascular endothelial cells by the constitutive pathway,
producing intense constriction of the underlying smooth
muscle and contributing to the maintenance of endogenous
vascular tone. Several studies of various malignancies have
revealed that members of the ET family are produced by
several epithelial tumors, in which they act as autocrine and/or
paracrine growth factors. ET-1 is the most common
circulating form of ET [8].
ETs are powerful vasoconstrictive peptides that exert their
effects through two specific heptahelical GPCR subtypes: the
endothelin A receptor (ETAR) specific for ET-1 and ET-2 and
the nonspecific endothelin B receptor (ETBR) [1,9,10]. The ET
receptors share about 59% similarity in the primary structure.
The ETAR selectively binds ET-1 and ET-2, whereas the
ETBR binds all three ET forms with similar affinity. While the
ETAR primarily mediates vaso-/bronchoconstriction, mitogenesis, antiapoptosis, matrix formation, acute and neuropathic pain, the ETBR mediates inflammatory pain and
vasodilatation and has further been proposed to contribute
to clearance of ET as well as to autoinduction of ET-1 [11].
Although the ETBR may also mediate vasoconstriction, this
subtype, which is primarily situated at the plasma membrane
of endothelial cells, is first of all considered causing transient
NO-mediated vasodilatation. The ETBR shares several intracellular signaling pathways with the ETAR; however, unlike
ETA receptor-dependent effects, ETBR-dependent phenomena are shorter lasting and reversible. ET receptor interacts
with heterotrimeric G proteins. After ligand binding, ETARs
become internalized and undergo receptor recycling followed
by relocation to the cell membrane, whereas ETBRs can be
translocated to the lysosomal compartment for degradation [12]
or translocated to nuclear membranes for further signaling
events [13]. ETs and ET receptors are ubiquitously expressed
and regulate a wide range of physiological and pathophysiological functions, such as cardiovascular, mitogenic and neuroregulatory events, hormone production and placental
development [14].
ET-1 production is stimulated by cytokines (IL-1h), growth
factors (TNF-a, TGF-h and platelet-derived growth factor
(PDGF)) and major signals of cardiovascular stress, such as
vocative agents (angiogenesis II, norepinephrine, vasopressin
and bradykinin), thrombin, mechanical stress and hypoxia.
Prostacyclin, NO and atrial natriuretic peptide are the
predominant effectors of negative feedback mechanisms [15].
2
2.
Medical need
Nearly all patients with advanced prostate cancer are sensitive to androgen ablation therapy. However, the effect of
this treatment on disease progression is temporary. These
patients ultimately become resistant to androgen ablation
and are then classified as having castration-resistant prostate
cancer (CRPC). To date, chemotherapy is the main option
for this disease. Docetaxel represents the best tolerated and
effective agent of treating it.
There has been great interest regarding the possibility of
using this drug for the treatment of even elderly patients,
because prostate cancer apparently occurs more frequently in
older men. An intravenously delivered chemotherapeutic
agent with high incidence of hematological toxicity, even
if better tolerated than other drugs with the same clinical
indication, such as docetaxel, may hinder the accessibility of
comorbid patients. For several years, oncologists have been
trying to find new agents with minimal toxicity to be
administered per os.
Another hurdle for these patients is the development of
resistance to docetaxel. When CRPC patients progress after
first-line therapy, there are only a few options available for
their treatment. New types of therapy are required in this
patient setting. The effect of ET receptor antagonists on
angiogenesis might be exploited to overcome taxane resistance.
3.
111
115
120
125
130
135
Existing treatment
Treatment with hormone therapy or chemotherapy is the
standard option for patients with CRPC. After progression on
both a luteinizing-hormone-releasing hormone agonist and
antiandrogen, the withdrawal of antiandrogen therapy results
in an antiandrogen withdrawal response in 25 – 50% of
patients. Secondary hormone medications, including ketoconazole and hydrocortisone, could induce a clinical response in
~ 25% of patients. This benefit lasts for only a short time, with
a mean duration of 4 months. For this reason, chemotherapy
is considered the main choice for such patients. The development of novel therapeutic agents for the treatment of CRPC
is still to be explored in this patient population.
Combination chemotherapy regimens involving agents that
affect microtubule integrity appear to have activity with
tolerable adverse effects. In particular, combination regimens
including taxanes seem the most promising treatment, achieving > 50% response rates. However, the median duration of
response is limited to ~ 6 months. Additional survival benefits
reported in Phase II trials have not yet been confirmed in
Phase III randomized trials.
Because of the increasing proportion of patients included in
earlier application of taxane-based chemotherapy, there is an
ever enlarging subset of patients with disease progression who
remain viable candidates for additional therapy. To date, we
lack enough data from clinical trials to guide decision making,
although clinical investigation is ongoing for this subset of
Expert Opin. Emerging Drugs (2010) 15(1)
140
145
150
155
160
165
�Russo, Bronte, Rizzo, Fanale, Gebbia & Bazan
166
170
175
180
patients. Usually, CRPC patients previously treated with
first-line chemotherapy are classified into two groups:
mitoxantrone-treated patients, for whom the utility of taxanes
as second-line therapy should be considered, and taxanetreated patients, for whom the activity of retreating with
taxanes, mitoxantrone or other microtubular targeted agents
is under investigation.
ET receptor antagonists studied for cancer treatment are
not yet marketed.
A previous US registration submission as Xinlay for the
treatment of metastatic CRPC received a non-approvable
letter (Scrip Daily Online, 17 October 2005, S00899072).
Abbott decided not to pursue further registration of astrasentan for this indication (direct communication, Abbott,
24 August 2007). It had US fast-track status for prostate
cancer (press conference, Abbott, 6 February 2001).
Regarding Zibotentan, European and US filings for the
treatment of CRPC are expected in 2011 (company pipeline,
AstraZeneca, 31 January 2008).
185
Current research goals
4.
The main goals of treatment with ET receptor antagonists for
CRPC patients include:
190
.
.
195
.
200
205
Availability of agents with minimal or manageable toxicity
and orally bioavailable to extend applicability of anticancer
treatment even for elderly and comorbid patients.
Efficacy on cancer-related pain and bone metastases complications, which are the most frequent factors impairing
quality of life.
Applicability also in nonmetastatic CRPC to improve
both progression-free survival and overall survival and
to delay major complications deriving from clinically
evident metastases.
The great hope of the researchers regards the prospect of
using ET receptor antagonists even in other malignancies.
Until now, no clear evidence has been provided for activity of
these agents in different cancers. A better understanding of the
biological mechanisms of their action will make it possible to
investigate them in a more suitable patient setting.
5.
210
215
220
Scientific rationale
Role of ET-1 in cell growth
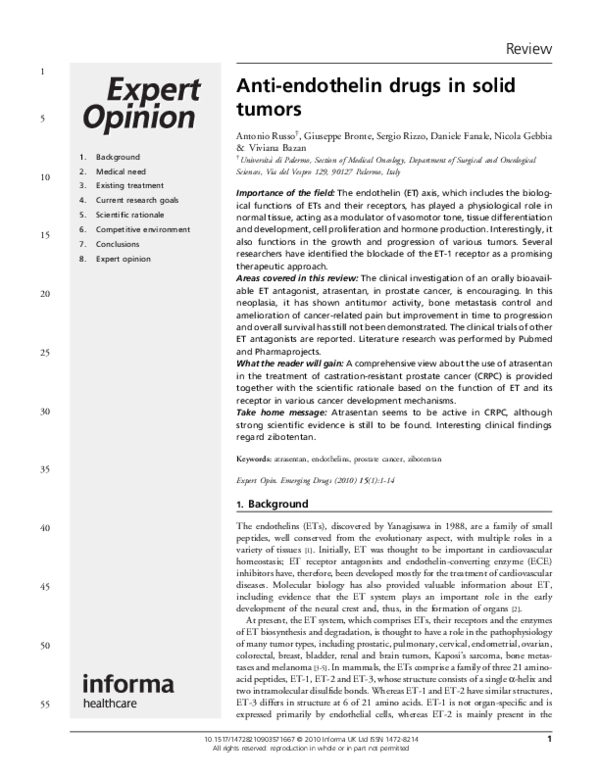
ET-1 is a powerful vasoconstrictor with mitogenic or comitogenic properties, which stimulates proliferation in vitro of
fibroblasts, renal mesangial cells, smooth muscle and
several tumor cell lines, including colorectal cancer [16-20].
Studies involving colorectal, ovarian and prostate cancers
suggest that the receptor responsible for the ET-1 mitogenic
action is ETA, which is probably upregulated. Activation of
the ETAR by ET-1 mediates a signaling cascade, which
promotes tumor cell growth, synergizing with other growth
factors to cause cell proliferation (Figure 1). ETA interacts with
5.1
and activates a G protein that triggers a parallel activation of
several signal transducing pathways. This interaction can in
fact activate multiple signal transduction pathways including
phospholipase C activity with a consequent increase in
intracellular Ca2+ levels, PKC, phosphati-dylinositol 3-kinase
and MAPK [21]. ETBR-mediated coupling in choriocarcinoma
cell lines leads to the activation of the Ras/Raf-MAPK pathway [22]. ET-1 causes EGFR transactivation which is partly
responsible for MAPK activation by a ligand-dependent
mechanism involving a non-receptor tyrosine kinase, such
as Src. Recent work has reported that a specific ETAR
antagonist can reduce the EGFR transactivation [14,23-25].
The phenotypic change of vascular smooth muscle cells in
culture is concommitantly associated with a change in the ET
receptor subtype which potentiates mitogenic activity. This
suggests that the switching of the ET receptor subtype from A
to B during phenotypic change may contribute to a certain
extent to the development of vascular lesions [26].
ET-1 promotes DNA synthesis and cell proliferation in
various epithelial tumor cells, including prostate, cervical and
ovarian cancer cells. Synergistic interactions with other growth
factors, including EGF, basic fibroblast growth factor (bFGF),
insulin, IGF, PDGF, TGFs and IL-6, intensify mitogenic
activity [27].
221
225
230
235
240
245
Role of ET-1 in angiogenesis
Angiogenesis, the formation of new vessels from existing
vasculature, is an important early event in tumor progression
which begins in premalignant lesions. VEGF and bFGF are
the principal regulators of neovascularization. During the
formation of new blood vessels, endothelial cells are stimulated to release proteases, such as MMP-2, in order to migrate,
proliferate and invade surrounding tissue and form capillaries.
Initiation of angiogenesis is controlled by different regulators
including local hypoxia, which activates the expression of
angiogenic factors that can stimulate endothelial cell
growth [28]. Activation of ETAR by ET-1 promotes tumor
growth and progression by stimulating the production of the
key angiogenic factor VEGF in response to hypoxia. ET-1
regulates various stages of neovascularization, including endothelial cell proliferation, migration, invasion, protease
production and tube formation, and also stimulates neovascularization in vivo [29]. ET-1 increases VEGF mRNA expression and VEGF protein levels in a dose- and time-dependent
manner, and does so to a greater extent under hypoxia. ET-1
stimulates VEGF production through the hypoxia-inducible
factor HIF-1a and this mechanism might be responsible for
increasing tumor angiogenesis. Degradation of HIF-1a is in
fact reduced in ET-1-treated ovarian carcinoma cells under
both hypoxic and normoxic conditions, indicating that the
induction of HIF-1a protein production by ET-1 is due to
enhanced HIF-1a stability. After ETAR activation by ET-1,
HIF-1a protein levels are increased, the HIF-1 transcription
complex is formed and binds to the hypoxia-responsive
5.2
Expert Opin. Emerging Drugs (2010) 15(1)
3
250
255
260
265
270
275
�Anti-endothelin drugs in solid tumors
Prepro-ETs
ECE
ET-1
ET-2
ET-3
NEP
G-protein
ETAR
PLC
PKC
ETBR
PI3K
MAPK
Cell
proliferation
Cell
migration
Autoinduction
of ET-1
ET clearance
Evasion
of apoptosis
Angiogenesis
Inflammatory
pain
Angiogenesis
Figure 1. Molecular mechanisms of endothelin axis.
276
280
285
288
element binding site [3]. Furthermore, not only does ET-1
stabilize HIF-1a under hypoxic and normoxic conditions,
inducing the transcription of angiogenic genes, but HIF-1a is
also able to modulate transcription of ET-1 in various cell
types. Moreover, the ETAR blockade exerts an antiangiogenic
effect by completely inhibiting growth and neoangiogenesis in
different tumors [30].
Prostaglandins (PG) and their rate-limiting enzymes
COX-1 and -2 are involved in the progression of a variety
of malignancies in association with elevated levels of
proangiogenic factors [31-33].
Under normoxic condition, ET-1 significantly stimulates
the expression of COX-1 and -2 at mRNA and protein levels,
4
COX-2 promoter activity and prostaglandin PGE2 produc- 289
tion. PGE2 promotes angiogenesis and this effect is mediated 290
by VEGF. The use of EP agonists and antagonists indicates
that ET-1 and PGE2 stimulate VEGF production, principally
via two receptors, EP2 and EP4.
Role of ET-1 in apoptosis
295
Apoptosis is an active cell death process that takes place in a
wide spectrum of physiologic situations such as normal cell
turnover, embryogenesis and endocrine-dependent tissue
atrophy.
Recently, investigations into the role of the ET axis in 300
apoptosis inhibition have provided evidence of the importance 301
5.3
Expert Opin. Emerging Drugs (2010) 15(1)
�Russo, Bronte, Rizzo, Fanale, Gebbia & Bazan
302
305
310
315
320
325
330
of the ET-1 axis in cell survival. Previous studies have
indicated a potential function for ET-1 in cell proliferation
or as a cell survival factor.
Interaction between the Fas receptor (CD95/APO-1), a
member of the TNF-receptor superfamily, and the Fas ligand
(FasL) triggers a pathway to cell death involving caspase-8
activity. However, despite expression of Fas and caspase, death
signals are frequently interrupted by also anti-apoptotic modulators, including caspase inhibitory proteins such as FLIP [34].
In human glioblastoma cell lines, ET-1, acting as survival
factor, probably acts through ERK phosphorylation and the
PKC pathway, determining a stabilization of the short form
of FLIP protein [35]. The binding of ET-1 to high-affinity sites
inhibits FasL-induced apoptosis, while the binding of either
ET-1 or receptor antagonists to low-affinity sites promotes
FasL-induced apoptosis. Thus, ET signaling pathways do not
induce human cancer cell proliferation, but are survival signals
controlling resistance to apoptosis [36].
As these effects are mediated by ETAR, activation of ETB by
ET-1 conversely induces cell death via apoptosis in human
cancer cells [37].
In ovarian carcinoma cells, the addition of ET-1 significantly inhibits paclitaxel-induced apoptosis in a dosedependent fashion as a result of Bcl-2 phosphorylation
suppression. ET-1 also stimulates Akt activation in a
PI3K-dependent manner. Interestingly, the use of specific
ETAR antagonists has demonstrated that ET-1 contributes
to paclitaxel resistance through ETAR binding via activation
of anti-apoptotic signaling pathways [21].
Role of ET-1 in tumor invasiveness
Tumor invasion is characterized by changes in MMPs, connexin, integrin and cadherin expression. The presence of high
levels of ET-1 in ascitic fluids of ovarian cancer patients has
shown that ET-1 may increase the secretion of extracellular
matrix-degrading proteinases and metastatization process. In
fact, ETAR activation induces matrix-degrading enzymes, such
as MMPs and urokinase plasminogen activator, which play
important roles in tissue remodeling and tumor metastasis [38].
The ET-1 system acts by enhancing the invasive potential
of tumor cells. ET-1, in fact, activates MMP-2, MMP-3,
MMP-7, MMP-9 and MMP-13. EP2 and EP4 receptor
antagonists block MMP activity and cell invasion, demonstrating that these receptors are the principal PGE2 receptors
involved in these processes [39]. Furthermore, ET-1 stimulates
focal adhesion kinase (FAK) and paxillin phosphorylation
through the ETAR, which directly correlates with tumor
cell migration and invasion [24]. This indicates that ETAR
antagonists can inhibit cell migration and possibly other
FAK-associated processes.
Defects in regulation of intercellular communication, such
as dysregulated or reduced expression of connexins, allow
cancer cells to escape microenvironmental control from the
normal surrounding tissue. ET-1 is able to disrupt gap
5.4
335
340
345
350
355
356
junctions and this might serve as a basis to further evaluate
the cell–cell metabolic uncoupling and the cell detachment
that occurs during tumor progression [40]. In epithelial cancer,
the loss of the epithelial features and the gain of a mesenchymal phenotype, a process known as epithelial to mesenchymal
transition (EMT), determine the acquisition of tumor invasiveness. A primary event regulating EMT is the disruption of
the E-cadherin-mediated stable interactions between the cells.
In ovarian carcinoma cells, activation of the ETAR pathway by
ET-1 contributes to disruption of normal host–tumor interactions by downregulating the expression of E-cadherin and
associated b-catenin adhesion proteins [41]. ET-1 induces
expression of the transcription factor Snail, which has been
identified as a potent repressor of E-cadherin expression.
Role of ET-1 in osteogenesis
The ET axis seems to have a central role in osteoblastic bone
metastasis. Alkaline phosphatase, a marker of new bone
formation, is elevated in the presence of exogenous ET-1 [42].
ETA and ETB appear to regulate tumor progression by a
mechanism involving bone deposition in skeletal metastases
through the activation of osteoblasts. It is thought that ET-1
production by metastatic cancer cells located in the bone is
stimulated by osteoblast- and endothelial cell-secreted IL-1,
TNF-a and TGF-h. ET-1, in turn, would stimulate mitotic
activity in osteoblasts, decreasing both osteoclastic bone
resorption and osteoclast motility [43,44]. Several experiments
conducted in human prostate cancer cell lines have shown that
osteoclastic bone resorption is significantly blocked by the
presence of ET-1 in a dose-dependent fashion. In prostate and
breast cancer models, selective ETAR inhibition, but not
ETBR modulation, suppressed ET-1-induced osteoblastic
response [45,46]. It seems that a calcineurin/FAT (nuclear factor
of activated T cells) pathway is involved in the molecular
mechanism of ET-1-mediated osteoblast stimulation.
357
360
365
370
5.5
ET receptor antagonists’ preclinical development
ET-1 has shown pleiotropic mechanisms in different pathways
of cancer development and progression. For this reason, many
researchers have hypothesized a role of the ET-1 axis targeting
for cancer treatment. Various approaches have been identified
in order to impair ET biological function in tumors, for
example, inhibition of ET biosynthesis, blockade of ET
production from preproETs, promotion of ET degradation,
selective blockade of ETAR/ETBR activation and enhancement of tumor perfusion by ETBR activation to potentiate
efficacy of antineoplastic drugs.
Red wine polyphenols (i.e., quercetin, resveratrol, cathechins, etc.) can suppress ET-1 release and the transcription of
prepro-ET-1 gene [47]. Similarly, green tea polyphenol epigallocatechin-3-gallate in ovarian carcinoma cells and xenografts have inhibited both ETAR and ET-1 expression and
reduced basal and ET-1-induced cell proliferation and
invasion [48]. ET synthesis might be blocked by inhibition
375
380
385
390
5.6
Expert Opin. Emerging Drugs (2010) 15(1)
5
395
400
405
410
411
�Anti-endothelin drugs in solid tumors
412
415
420
425
430
435
440
445
450
455
460
465
466
of the enzyme which converts preproETs into ETs. ECE
inhibitors have been studied for various cardiovascular,
renal, pulmonary and neurological diseases. They may be
selective or may also inhibit the ACE and neutral endopeptidase [49]. ET degradation has been achieved by means
of neutral endopeptidase transfection in ovarian carcinoma
cells. NEP is a cell surface aminopeptidase with a ubiquitous
expression and is able to degrade various bioactive peptides,
including ET-1 [50].
Among all these options, the ET receptor blockade has
reached the most advanced phases of preclinical and clinical
drug development. Several small molecules functioning as
ETAR antagonists have provided a clearer understanding of
the physiologic role of ET-1 and its effects on ET receptormediated signal transduction in tumor development and
progression. Atrasentan and ZD-4054 are the most potent
and selective ETAR antagonists. They are orally bioavailable.
For this reason, they are well qualified for clinical development
in cancer treatment.
Atrasentan is able to inhibit effectively cell proliferation and
VEGF secretion both in ovarian carcinoma cell lines and
primary cultures. This action of atrasentan can be translated
into biological effects such as reduction of microvessel density,
VEGF and MMP-2 expression and increase in the percentage
of apoptotic tumor cells.
Its combination with paclitaxel seems to be synergistic
because of the enhancement of antitumor, proapoptotic
and antiangiogenic effects. These phenomena may be
explained by the sensitization to paclitaxel-induced apoptosis
by the ETAR blockade [51]. Moreover, the synergistic action of
chemotherapy and ETAR antagonists is supported by the
finding of specific higher expression of ETAR gene in postchemotherapy samples of primary ovarian tumors [52]. In
breast carcinoma, the overexpression of ETAR has induced
resistance to chemotherapy. Some authors have suggested the
use of the evaluation of ETAR expression levels to predict the
responsiveness of cancer patients to chemotherapy [53].
Atrasentan has induced tumor growth inhibition in xenografts of cervical carcinoma cells. This effect has been observed
with just two cycles of treatment [54]. The additive effects of
paclitaxel when combined with atrasentan have been obtained
both in cervical carcinoma models [30] and in ETARoverexpressing prostate cancer cells [43]. They are associated
with a lower cell viability and a higher apoptotic rate.
In prostate cancer, the proliferative action of exogenous
ET-1 is blocked by ETAR antagonists. This observation has
been explained by the finding of bone–tumor interaction
impairment through the direct inhibition of osteoblasts.
The role of ET receptor antagonists in prostate cancer is
also supported by the finding of a high expression of ETAR,
both in primary and metastatic tumors, which is associated
with advanced tumor stage and grade.
ETAR expression is also correlated with survival and might
predict distant metastases in nasopharyngeal carcinoma
(NPC) [55]. The inhibition of NPC cell proliferation by
6
atrasentan depends on ETAR expression. In this type of tumor,
atrasentan has also induced more evident apoptotic effects
when combined with cytotoxic drugs such as cisplatin and
5-fluorouracil in xenograft models. The xenografts of metastatic tumors have demonstrated a role for atrasentan in
reducing metastases to the lung from both nasopharyngeal
and bladder cancers [56,57].
Several other ET receptor antagonists have also been
studied in preclinical cancer models.
Zibotentan (ZD-4054) is an orally active specific ETAR
antagonist. ETAR blockade by zibotentan inhibits ET-1induced mitogenic effects, while the ETBR antagonist, BQ
788, is ineffective. Zibotentan is able to inhibit the proliferative activity of ET-1 in ovarian carcinoma cells [58]. The
combination of zibotentan and paclitaxel produces additive
effects on the reduction of ETAR-driven angiogenesis and
invasive mediators, such as VEGF, COX-1/2 and MMP.
Forty percent of mice bearing human ovarian cancer remained
tumor-free, suggesting a possible clinical role of zibotentan as
monotherapy or in combination with cytotoxic drugs [59]. In
ovarian carcinoma xenografts, zibotentan has enhanced the
efficacy of gefitinib, achieving partial (82%) or complete
tumor regression. A cross-talk between the EGFR and
ETAR pathways has been documented together with the
evidence of decreased vascularization, Ki-67, MMP-2,
VEGF, MAPK and EGFR, and enhanced E-cadherin
expression [60].
Bosentan, a dual ET receptor antagonist targeting ETAR
and ETBR, has therapeutic indications for cardiovascular
diseases. In a breast carcinoma cell metastasis model, bosentan
has shown inhibition of tumor growth, neovascularization and
bone metastasis. In melanoma xenografts, bosentan has
enhanced the effects of alkylating agents, such as dacarbazine,
when a combination treatment was delivered [61].
A-182086 is another dual antagonist. It can inhibit tumor
growth by blocking proliferation not only of tumor cells but
also of endothelial cells expressing ETBR. It has shown a
potential role in Kaposi sarcoma treatment because of simultaneous interference with cell proliferation, invasiveness and
angiogenesis [62,63].
BQ788 is a peptide ETBR antagonist which inhibits growth
and induced death of melanoma cells in vitro and in vivo [64].
A-192621 is a specific ETBR antagonist studied in xenografts of human melanoma cells. It suppresses HIF-1a accumulation, tumor growth, neovascularization and VEGF and
MMP-2 expression [65].
6.
467
470
475
480
485
490
495
500
505
510
Competitive environment
515
The pharmaceutical development of ET receptor antagonists
has derived from the observation of the prominent role of the
ET-1 axis in cardiovascular diseases. ABT-627 is an agent
developed by Abbott Laboratories; it is also known as atrasentan and marketed under the brand name of Xinlay. It is 520
one of the most potent and selective ETAR antagonists. Its 521
Expert Opin. Emerging Drugs (2010) 15(1)
�Russo, Bronte, Rizzo, Fanale, Gebbia & Bazan
522
525
530
535
540
effects on the ET-1 blockade were discovered in in vitro and
in vivo models for cardiovascular diseases and malignancies.
Atrasentan seems qualified for clinical use because it is orally
bioavailable and has a half-life of 25 h, thus, allowing daily
delivery. It has produced mild adverse effects in healthy
volunteers [66], for example, transient headache, rhinitis
and nausea, which appear to be associated with atrasentan
action on the inhibition of the function of ET-1 as a
vasoconstrictor. However, no liver or hematological toxicity
has been reported.
Atrasentan is able to increase plasma levels of ET-1 due
to the blockade of ETB. Zibotentan is the only ET receptor
antagonist in clinical development that targets ETAR
without inhibition of ETBR at doses under clinical
investigation [67]. Table 1 reports a description of the
main features of the agents of this class studied for
anticancer treatment.
Prostate cancer patients have been identified as the best
clinical setting for testing the safety and efficacy of ET
receptor antagonists. Preclinical findings, in fact, have
already shown a clear role of ET-1 in the development
and progression of prostate carcinoma.
545
6.1
550
555
560
565
570
575
576
Atrasentan
Two Phase I clinical trials were designed to treat hormone
refractory prostate cancer patients with escalating doses of
atrasentan ranging between 2.5 and 95 mg orally for 28 days.
In one of the two studies, headache was found to be the doselimiting toxicity obtained at 75 mg, while in the other study
the maximum tolerated dose was not reached. As previously
found in healthy subjects, headache, rhinitis and peripheral
edema were the most common side effects [68,69]. Even though
prostate specific antigen (PSA) response was not the aim of the
study, 68% (15/22) of patients achieved a reduction of PSA
levels ranging between 5 and 95%. Doses of atrasentan
showed no correlation with PSA declines.
Ten patients in the same study were affected by pain which
needed treatment with opioids. In all, 70% of them experienced pain reduction evaluated by VAS. Preclinical findings
indicated the particular effect of ET-1 in inducing hyperalgesia and pain through cutaneous injection [70,71]. This phenomenon is mediated by the excitation of ETAR-mediated
nociceptors. On the other hand, ETBR activation induces
analgesia by the release of b-endorphin and the activation of
the opioid pool [72].
These effects of atrasentan in controlling cancer pain
were studied in one Phase II clinical trial, double-blind and
placebo-controlled; for hormone-refractory metastatic prostate cancer, patients were affected by pain needing opioid
supplementation. The primary end point of this particular
study was to evaluate the rate of pain relief after 12 weeks of
treatment. No statistically significant difference was observed.
A trend toward cancer pain amelioration with control of
analgesic consumption was obtained only in the group of
patients treated with 10 mg atrasentan. In the same group, a
statistical significance was observed in the improvement of
‘pain interference with relations with other people’ (p = 0.031)
and ‘worst pain in the last 24 h’ (p = 0.030). This finding
suggests a possible specific role of atrasentan to increase the
quality of life [73].
A subsequent Phase II trial investigated the antitumor
activity as identified through PSA reductions observed in
previous Phase I studies. This second trial, double-blind
and placebo-controlled, evaluated the effect on time-toprogression prolongation. Asymptomatic hormone-refractory metastatic prostate cancer patients were divided into
three arms, those treated with a placebo, with 2.5 mg and
with 10 mg atrasentan. In the evaluable set, but not in the
intent-to-treat analysis, a statistically significant difference
in the delay of disease progression was seen between placebo
and 10 mg atrasentan groups (p = 0.021).
Overall survival analysis in this study found no significant
advantage in the atrasentan arms versus placebo. This result
seems to be due to the confounding effect of the crossover
toward atrasentan treatment administered to placebo group
patients. Survival advantage proved to be significant when
atrasentan treatment groups were combined into a single arm
achieving HR = 0.69 [68].
Tolerabilty profile included mild toxicity with headache,
rhinitis and edema as the most common side effects.
The markers of bone deposition (alkaline phosphatase,
bone alkaline phosphatase) and bone resorption (N-telopeptides, C-telopeptides and deoxypyridinoline) were evaluated in the same Phase II trial with atrasentan, which
showed a dose-dependent effect on the stabilization of these
markers and a clear trend toward the improvement of the
bone scan index was found in the 10 mg arm [74]. These
findings agree with preclinical data regarding the role of the
ET-1 axis in bone formation. Osteoblasts have shown the
expression of high affinity ETAR receptors and strong
response to ET-1 stimulation leading to the osteoblastic
proliferation associated with metastatic breast and prostate
cancers [44,75]. In vivo models of bone metastasis have
clarified the role of ETAR in osteogenesis by means of
the use of ETAR antagonists [46].
On the basis of the clinical findings of a Phase II trial
involving disease progression delay, a Phase III clinical study
(M00-211) was designed to verify the ability of atrasentan to
duplicate time to progression in asymptomatic hormonerefractory metastatic prostate cancer patients. These were
grouped into two arms, placebo and 10 mg atrasentan.
Secondary end points were PSA response rate, markers of
bone metabolism and quality of life. As in the Phase II
M96-594 trial, time to progression was significantly delayed
in the evaluable set analysis but not in the intent-to-treat
analysis (p = 0.007 vs 0.091). All the secondary end points
showed a significant favor trend for the 10 mg atrasentan arm.
Moreover, in the 10 mg atrasentan group, a stratification of
this trial data made it possible to observe a significant
Expert Opin. Emerging Drugs (2010) 15(1)
7
577
580
585
590
595
600
605
610
615
620
625
630
631
�Anti-endothelin drugs in solid tumors
Table 1. Endothelin receptor antagonists studied in clinical trials for cancer treatment.
Compound
Company
Mechanism of action
Indication
Stage of
development
Side effects
Atrasentan
(ABT-627,
Xinlay)
Abbott, USA
ETAR antagonist
Reduction of microvessel density,
VEGF and
MMP-2 expression and increase
of the percentage of apoptotic
tumor cells
Castration-resistant
prostate cancer
Phase III trial
Headache,
rhinitis and
nausea
Zibotentan
(ZD-4054)
AstraZeneca, UK
ETAR antagonist
Inhibits ET-1-induced mitogenic
effects
The combination with paclitaxel
produces additive effects on
the reduction of ETAR-driven
angiogenesis and invasive
mediators
Castration-resistant
prostate cancer
Phase III trial
Headache,
peripheral
edema, fatigue,
nasal congestion
and nausea
Bosentan
Hoffmann-La
Roche,
Switzerland
Dual ET receptor antagonist
targeting
ETAR and ETBR
Inhibits tumor growth,
neovascularization and bone
metastasis
Melanoma
Phase II trial
Headache,
fatigue, nausea,
back pain and
abnormal
hepatic function
ET: Endothelin; ETAR: Endothelin A receptor; ETBR: Endothelin B receptor.
632
635
640
645
650
655
660
prolongation of time to progression in the subgroup of
patients with bone metastases independently of soft tissue
metastases [76]. This finding suggests interesting implications
regarding the clinical use of atrasentan in CRPC due to the
large number of patients (85%) with bone metastasis.
Subsequently, another Phase III trial was performed in
nonmetastatic hormone-refractory prostate cancer patients
with no radiographic evidence of metastases but rising PSA
levels. These were randomized to receive 10 mg atrasentan or
placebo. The primary end point, time to progression defined
as the time to the onset of metastases, was not achieved.
A favoring trend for atrasentan was highlighted through the
evaluation of the secondary end points: time to PSA progression, change in bone alkaline phosphatase levels, PSA doubling time and overall survival. Large geographic differences in
the median time to progression were observed, which implies
that trial conduct may have influenced the results. A more
adequate study design should, therefore, be considered [77].
Atrasentan has also been studied in clinical trials involving
the combination with other antineoplastic agents. A Phase II
study for the comparison between atrasentan alone and its
combination with zoledronic acid was designed to evaluate
bone turnover markers in men with bone metastases from
prostate cancer. There is no evidence for additive or synergistic
effects of combination treatment on these markers [78].
Preclinical data regarding the combination therapy with
taxanes and atrasentan have already suggested a potential role
in the treatment of refractory malignancies. In metastatic
CRPC patients, a Phase I/II trial investigated the feasibility
8
of docetaxel at doses ranging from 60 to 75 mg/m2 every
21 days, with daily oral atrasentan 10 mg starting on day 3
until evidence of disease progression or unacceptable toxicity.
The maximum tolerated dose of docetaxel in this regimen is
70 – 75 mg/m2. Overall survival and progression-free survival
are similar to that normally obtained with docetaxel and
prednisone. The PSA response rates are slightly lower than
expected. A Phase III trial to compare this combination with
docetaxel and prednisone had already been designed and is still
ongoing [79].
In advanced NSCLC, 10 mg/day atrasentan plus standard
paclitaxel–carboplatin combination have been investigated for
safety and pharmacokinetics. They appear to be well tolerated,
without pharmacokinetic interaction of paclitaxel and atrasentan. Efficacy and survival have proved to be similar to those
already observed in studies involving the use of chemotherapy
alone in advanced NSCLC patients [80]. Phase III trials and
other combination regimen trials should also be designed.
661
665
670
675
680
6.2
Zibotentan
Zibotentan, when studied in asymptomatic or mildly symptomatic hormone-refractory prostate cancer patients with
bone metastases, obtained similar results. Primary end point
(time to progression) was not achieved, but advantage in 685
overall survival was seen in both 10 and 15 mg zibotentan
arms [81].
A subsequent Phase I study evaluated escalating doses of
zibotentan ranging between 10 and 200 mg/day p.o. in 689
Expert Opin. Emerging Drugs (2010) 15(1)
�Russo, Bronte, Rizzo, Fanale, Gebbia & Bazan
Table 2. Clinical studies with ETAR antagonists.
Citation
Phase
Patients
Agents
Schedule
Results
Zonnenberg
2003 [69]
I
Metastatic CRPC
Atrasentan
A 2.5 – 95 mg/day
p.o.
No dose-limiting adverse
events observed up to
95 mg
The most common adverse
events were rhinitis,
headache and peripheral
edema
Armstrong
2008 [79]
I/II
Metastatic CRPC
Atrasentan
+ docetaxel
A 10 mg/day p.o.
+ D every 3 weeks
i.v. 60 – 75 mg/m2
Overall survival and
progression-free survival
are comparable to that
seen with docetaxel and
prednisone, whereas the
rates of PSA decline are
slightly lower than
expected
Drug-related grade 3 – 4
toxicities included
neutropenia (50 – 63%)
and febrile neutropenia
(16 – 25%)
Chiappori
2008 [80]
I/II
Advanced NSCLC
Atrasentan +
carboplatin +
paclitaxel
A 10 mg/day p.o.
+ C every 3 weeks
i.v. AUC6 + P every
3 weeks i.v.
225 mg/m2
Atrasentan plus
paclitaxel–carboplatin was
safe and well tolerated,
with no apparent
paclitaxel–atrasentan
pharmacokinetic
interaction
Efficacy and survival in
advanced NSCLC were
comparable with studies of
chemotherapy alone
Carducci
2003 [68]
II
Metastatic CRPC
Atrasentan
vs placebo
A 2.5 mg/day p.o.
A 10 mg/day p.o.
Placebo
Median TTP prolongation
Headache, peripheral
edema and rhinitis were
primary side effects
Michaelson
2006 [78]
II
Prostate cancer
with bone
metastases
Atrasentan +
zoledronic acid
A 10 mg/day p.o.
A 10 mg/day p.o. +
ZA every 4 weeks
i.v.
No evidence for additive or
synergistic effects of
combination therapy with
atrasentan and zoledronic
acid on bone turnover
markers
Commonly observed
adverse effects were
edema, rhinitis, fatigue
and shortness of breath
Carducci
2007 [76]
III
Metastatic CRPC
Atrasentan vs
placebo
A 10 mg/day p.o.
Placebo
Atrasentan did not delay
disease progression in men
with metastatic CRPC
despite evidence of
biologic effects on markers
of disease burden
Atrasentan
A: Atrasentan; B: Bosentan; b.i.d.: Twice a day; C: Carboplatin; CRPC: Castration-resistant prostate cancer; D: Docetaxel; ETAR: Endothelin A receptor;
i.v.: Intravenous; MWTD: Maximum well-tolerated dose; P: Paclitaxel; p.o.: Per os; PSA: Prostate specific antigen ; TTP: Time to progression; Z: Zibotentan;
ZA: Zoledronic acid.
Expert Opin. Emerging Drugs (2010) 15(1)
9
�Anti-endothelin drugs in solid tumors
Table 2. Clinical studies with ETAR antagonists (continued).
Citation
Phase
Patients
Agents
Schedule
Results
Nelson
2008 [77]
III
Nonmetastatic CRPC
Atrasentan vs
placebo
A 10 mg/day p.o.
Placebo
Although the primary end
point was not achieved,
large regional differences
in TTP were noted,
suggesting that trial
conduct may have
influenced the results
James
2009 [81]
II
Metastatic CRPC
Zibotentan vs
placebo
Z 10 mg/day p.o.
Z 15 mg/day p.o.
Placebo
The primary end point of
TTP was not achieved in
this study, but an
improvement was seen in
overall survival in both
active treatment arms
Adverse events were in line
with the expected
pharmacologic effects of
an ETAR antagonist
Schelman
2009 [82]
I
Metastatic CRPC
Zibotentan
Z 10 – 200 mg/day
p.o.
The MWTD for zibotentan
was 15 mg
Dose-limiting toxicity was
similar to that reported for
other drugs of this class
Some patients experienced
prolonged stable disease
II
Metastatic
melanoma
Bosentan
B 500 mg/day p.o.
b.i.d.
Benefit in disease
stabilization
The most frequent adverse
events were headache,
fatigue, nausea, back pain
and abnormal hepatic
function
Zibotentan
Bosentan
Kefford
2007 [83]
A: Atrasentan; B: Bosentan; b.i.d.: Twice a day; C: Carboplatin; CRPC: Castration-resistant prostate cancer; D: Docetaxel; ETAR: Endothelin A receptor;
i.v.: Intravenous; MWTD: Maximum well-tolerated dose; P: Paclitaxel; p.o.: Per os; PSA: Prostate specific antigen ; TTP: Time to progression; Z: Zibotentan;
ZA: Zoledronic acid.
690
695
metastatic CRPC patients. The maximum well-tolerated dose
for zibotentan was 15 mg/day p.o. Dose-limiting toxicity was
similar to that reported for other drugs of this class. Some
patients experienced prolonged stable disease, suggesting that
new methods are needed to test antitumor activity [82].
Phase III studies with zibotentan in the same setting of
patients are ongoing.
6.3
700
705
706
Bosentan
Bosentan, the dual ETAR/ETBR antagonist, was also studied
in a Phase II trial with metastatic melanoma patients. No
tumor responses were obtained, but disease stabilization was
found in about 20% of patients suggesting the need for further
investigation in combination with other anticancer
drugs [83]. Table 2 summarizes all the clinical trials with ET
receptor antagonists studied for cancer treatment.
10
7.
Conclusions
ETs belong to a family of proteins with regulatory activity in
different cellular pathways, including cell growth, survival,
invasion and angiogenesis. ET-1, which mainly exert their
function on the ETAR, has shown a role in the various phases
of carcinogenesis and cancer progression of different tumor
types. Preclinical studies have demonstrated the capability of
ET antagonists in inhibiting tumor cell proliferation, invasiveness and new vessel formation, as well as their effects on
osteogenesis and cancer-related pain. The clinical investigation
of an orally bioavailable ET antagonist, atrasentan, has suggested its benefit in PSA progression, markers of bone turnover,
and pain in men with prostate cancer, but improvement in time
to progression and overall survival has not yet been demonstrated with sufficient statistical significance, perhaps because of
the small number of patients included in the clinical trials. This
Expert Opin. Emerging Drugs (2010) 15(1)
707
710
715
720
723
�Russo, Bronte, Rizzo, Fanale, Gebbia & Bazan
724
725
class of drugs seems quite promising, above all for CRPC
patients. Nevertheless, we should define their exact role in
different cancer treatments by means of future clinical trials.
8.
730
735
740
745
750
755
760
Expert opinion
The ET axis, which includes the biological functions of the
ETs and their receptors, has played a physiological role in
normal tissue, acting as a modulator of vasomotor tone, tissue
differentiation and development, cell proliferation and hormone production. Interestingly, it also functions in the growth
and progression of various tumors. In vitro and in vivo studies
have suggested that it can trigger signaling pathways implicated in various hallmarks of cancer, including aberrant cell
proliferation, adhesion, migration, invasion, angiogenesis and
antiapoptotic activity.
Several researchers have identified the blockade of the ET-1
receptor as a promising therapeutic approach.
Preclinical findings have highlighted the fact that ET-1
receptor antagonists enhance the efficacy of cytotoxic drugs.
When ETAR is blocked by its antagonists, the cancer cells are
sensitized to the apoptotic potential of chemotherapeutics
drugs. The finding of sensitization to paclitaxel is an
example of this phenomenon obtained by ovarian and cervical
carcinoma preclinical models.
Atrasentan – one of the most potent and selective ETAR
antagonists – has been the most effectively studied, because it
has been included in two Phase III clinical trials as monotherapy and Phase I/II combination trials with chemotherapy.
It has shown a quite amazing tolerability profile and even the
means of administration – oral – would allow a wide applicability if its preliminary efficacy results are subsequently
confirmed. Time to progression, which is the primary end
point of the Phase III trials with atrasentan, has been achieved
only in the evaluable set of metastatic patients. No statistically
significant efficacy has been observed in the intent-to-treat
analysis. Overall survival, one of the secondary end points, has
confirmed a non-positive trend in favor of patients treated
with atrasentan independently of its dose. All these results
suggest that more effective clinical trials are required in order
to evaluate ETAR antagonists.
To date, the treatment of prostate cancer patients is the only
clinical setting to be extensively studied for therapy with
atrasentan. Unsatisfactory results have been obtained from
a Phase II trial with bosentan in metastatic melanoma patients.
The improved characterization of the ET-1 axis will
provide a valid target for more promising molecular treatment strategies to combine with known anticancer drugs.
The synergistic action of ZD-4054 and gefitinib on tumor
burden reduction is the best demonstration of this therapeutic potential.
The choice of the most adequate end point to define the
clinical efficacy of these drugs remains the most controversial
feature. Statistical power, baseline characteristics of patients
and pharmaceutical doses are the parameters to emphasize in
order to reach a definite understanding of the role of these new
agents in cancer treatment.
Combination clinical trials with chemotherapy or other
anticancer agents in various malignancies are needed. These
studies will found a proper rationale in the results of the
combination Phase I/II trials with atrasentan and standard
chemotherapeutic drugs in prostate and lung cancers.
Nevertheless, different end points, not only clinical but also
molecular, should be identified in order to reach a better
understanding of the most appropriate application of these
agents in the treatment of solid tumors.
761
Acknowledgements
790
765
770
775
780
785
A Russo and G Bronte have contributed equally to this work.
Declaration of interest
795
The authors state no conflict of interest and have received no
797
payment in preparation of this manuscript.
Expert Opin. Emerging Drugs (2010) 15(1)
11
�Anti-endothelin drugs in solid tumors
Bibliography
1.
Yanagisawa M, Inoue A, Ishikawa T, et al.
Primary structure, synthesis, and biological
activity of rat endothelin, an
endothelium-derived vasoconstrictor
peptide. Proc Natl Acad Sci USA
1988;85(18):6964-7
2.
Masaki T. Historical review: endothelin.
Trends Pharmacol Sci 2004;25(4):219-24
3.
Bagnato A, Natali PG. Endothelin
receptors as novel targets in tumor therapy.
J Transl Med 2004;2(1):16
4.
Levin ER. Endothelins. N Engl J Med
1995;333(6):356-63
5.
Masaki T. The endothelin family: an
overview. J Cardiovasc Pharmacol
2000;35(4 Suppl 2):S3-5
6.
Schweizer A, Valdenaire O, Nelbock P,
et al. Human endothelin-converting
enzyme (ECE-1): three isoforms with
distinct subcellular localizations.
Biochem J 1997;328 (Pt 3):871-7
7.
Xu D, Emoto N, Giaid A, et al. ECE-1: a
membrane-bound metalloprotease that
catalyzes the proteolytic activation of big
endothelin-1. Cell 1994;78(3):473-85
14.
Nelson J, Bagnato A, Battistini B, Nisen P.
The endothelin axis: emerging role in
cancer. Nat Rev Cancer 2003;3(2):110-6
15.
Remuzzi G, Perico N, Benigni A. New
therapeutics that antagonize endothelin:
promises and frustrations. Nat Rev
Drug Discov 2002;1(12):986-1001
16.
Ali H, Dashwood M, Dawas K, et al.
Endothelin receptor expression in
colorectal cancer. J Cardiovasc Pharmacol
2000 36(5 Suppl 1):S69-71
17.
Hirata Y. Endothelin-1 receptors in
cultured vascular smooth muscle cells and
cardiocytes of rats. J Cardiovasc Pharmacol
1989;13(Suppl 5):S157-8
18.
Kusuhara M, Yamaguchi K, Ohnishi A,
et al. Endothelin potentiates growth
factor-stimulated DNA synthesis in Swiss
3T3 cells. Jpn J Cancer Res
1989;80(4):302-5
19.
Shichiri M, Hirata Y, Marumo F.
Endothelin-1 as an autocrine/paracrine
factor for human tumor cell lines.
J Cardiovasc Pharmacol
1991;17(Suppl 7):S76-8
20.
Simonson MS, Wann S, Mene P,
et al. Endothelin-1 activates the
phosphoinositide cascade in cultured
glomerular mesangial cells.
J Cardiovasc Pharmacol
1989;13(Suppl 5):S80-3, discussion S4
8.
Rubin SA, Levin ER. Clinical review 53:
The endocrinology of vasoactive peptides:
synthesis to function. J Clin
Endocrinol Metab 1994;78(1):6-10
9.
Clozel M, Fischli W, Guilly C. Specific
binding of endothelin on human vascular
smooth muscle cells in culture.
J Clin Invest 1989;83(5):1758-61
21.
Clozel M, Gray GA, Breu V, et al. The
endothelin ETB receptor mediates both
vasodilation and vasoconstriction in vivo.
Biochem Biophys Res Commun
1992;186(2):867-73
Bagnato A, Spinella F, Rosano L.
Emerging role of the endothelin
axis in ovarian tumor progression.
Endocr Relat Cancer 2005;12(4):761-72
22.
Rauh A, Windischhofer W, Kovacevic A,
et al. Endothelin (ET)-1 and ET-3
promote expression of c-fos and c-jun
in human choriocarcinoma via ET(B)
receptor-mediated G(i)- and G
(q)-pathways and MAP kinase activation.
Br J Pharmacol 2008;154(1):13-24
10.
11.
Haynes WG, Webb DJ. The endothelin
family of peptides: local hormones with
diverse roles in health and disease?
Clin Sci (Lond) 1993;84(5):485-500
12.
Foster N, Loi TH, Owe-Young R,
Stanley KK. Lysosomal traffic of liganded
endothelin B receptor.
Biochim Biophys Acta
2003;1642(1-2):45-52
13.
12
Bkaily G, Nader M, Avedanian L, et al.
G-protein-coupled receptors, channels,
and Na+-H+ exchanger in nuclear
membranes of heart, hepatic, vascular
endothelial, and smooth muscle cells.
Can J Physiol Pharmacol
2006;84(3-4):431-41
23.
Bagnato A, Catt KJ. Endothelins as
autocrine regulators of tumor cell
growth. Trends Endocrinol Metab
1998;9(9):378-83
24.
Bagnato A, Tecce R, Di Castro V, Catt KJ.
Activation of mitogenic signaling by
endothelin 1 in ovarian carcinoma cells.
Cancer Res 1997;57(7):1306-11
25.
Vacca F, Bagnato A, Catt KJ, Tecce R.
Transactivation of the epidermal growth
factor receptor in endothelin-1-induced
mitogenic signaling in human ovarian
carcinoma cells. Cancer Res
2000;60(18):5310-7
Expert Opin. Emerging Drugs (2010) 15(1)
26.
Eguchi S, Hirata Y, Imai T, et al.
Phenotypic change of endothelin receptor
subtype in cultured rat vascular smooth
muscle cells. Endocrinology
1994;134(1):222-8
27.
Battistini B, Chailler P, D’Orleans-Juste P,
et al. Growth regulatory properties of
endothelins. Peptides 1993;14(2):385-99
28.
Carmeliet P, Jain RK. Angiogenesis in
cancer and other diseases. Nature
2000;407(6801):249-57
29.
Salani D, Taraboletti G, Rosano L, et al.
Endothelin-1 induces an angiogenic
phenotype in cultured endothelial cells and
stimulates neovascularization in vivo.
Am J Pathol 2000;157(5):1703-11
30.
Bagnato A, Cirilli A, Salani D, et al.
Growth inhibition of cervix carcinoma
cells in vivo by endothelin A receptor
blockade. Cancer Res 2002;62(22):6381-4
31.
Dannenberg AJ, Subbaramaiah K.
Targeting cyclooxygenase-2 in human
neoplasia: rationale and promise.
Cancer Cell 2003;4(6):431-6
32.
Denkert C, Kobel M, Pest S, et al.
Expression of cyclooxygenase 2 is an
independent prognostic factor in human
ovarian carcinoma. Am J Pathol
2002;160(3):893-903
33.
Ferrandina G, Lauriola L, Zannoni GF,
et al. Increased cyclooxygenase-2 (COX-2)
expression is associated with chemotherapy
resistance and outcome in ovarian cancer
patients. Ann Oncol 2002;13(8):1205-11
34.
Irmler M, Thome M, Hahne M, et al.
Inhibition of death receptor signals by
cellular FLIP. Nature
1997;388(6638):190-5
35.
Egidy G, Eberl LP, Valdenaire O, et al.
The endothelin system in human
glioblastoma. Lab Invest
2000;80(11):1681-9
36.
Peduto Eberl L, Bovey R,
Juillerat-Jeanneret L. Endothelin-receptor
antagonists are proapoptotic and
antiproliferative in human colon cancer
cells. Br J Cancer 2003;88(5):788-95
37.
Okazawa M, Shiraki T, Ninomiya H,
et al. Endothelin-induced apoptosis of
A375 human melanoma cells. J Biol Chem
1998;273(20):12584-92
38.
Salani D, Di Castro V, Nicotra MR, et al.
Role of endothelin-1 in neovascularization
of ovarian carcinoma. Am J Pathol
2000;157(5):1537-47
�Russo, Bronte, Rizzo, Fanale, Gebbia & Bazan
39.
Spinella F, Rosano L, Di Castro V, et al.
Endothelin-1-induced prostaglandin
E2-EP2, EP4 signaling regulates vascular
endothelial growth factor production and
ovarian carcinoma cell invasion.
J Biol Chem 2004;279(45):46700-5
40.
Spinella F, Rosano L, Di Castro V, et al.
Endothelin-1 decreases gap junctional
intercellular communication by inducing
phosphorylation of connexin 43 in human
ovarian carcinoma cells. J Biol Chem
2003;278(42):41294-301
41.
42.
43.
44.
45.
46.
47.
48.
49.
Rosano L, Spinella F, Di Castro V,
et al. Endothelin-1 promotes
epithelial-to-mesenchymal transition in
human ovarian cancer cells. Cancer Res
2005;65(24):11649-57
Nelson JB, Hedican SP, George DJ, et al.
Identification of endothelin-1 in the
pathophysiology of metastatic
adenocarcinoma of the prostate. Nat Med
1995;1(9):944-9
50.
Kajiyama H, Shibata K, Terauchi M, et al.
Neutral endopeptidase 24.11/CD10
suppresses progressive potential in ovarian
carcinoma in vitro and in vivo.
Clin Cancer Res 2005;11(5):1798-808
51.
Rosano L, Spinella F, Salani D, et al.
Therapeutic targeting of the endothelin a
receptor in human ovarian carcinoma.
Cancer Res 2003;63(10):2447-53
52.
53.
54.
Carducci MA, Jimeno A. Targeting bone
metastasis in prostate cancer with
endothelin receptor antagonists.
Clin Cancer Res
2006;12(20 Pt 2):6296s-300s
55.
Nelson JB, Nguyen SH, Wu-Wong JR,
et al. New bone formation in an
osteoblastic tumor model is increased by
endothelin-1 overexpression and decreased
by endothelin A receptor blockade.
Urology 1999;53(5):1063-9
56.
Guise TA, Yin JJ, Mohammad KS. Role of
endothelin-1 in osteoblastic bone
metastases. Cancer
2003;97(Suppl 3):779-84
57.
Yin JJ, Mohammad KS, Kakonen SM,
et al. A causal role for endothelin-1 in the
pathogenesis of osteoblastic bone
metastases. Proc Natl Acad Sci USA
2003;100(19):10954-9
Corder R, Douthwaite JA, Lees DM, et al.
Endothelin-1 synthesis reduced by red
wine. Nature 2001;414(6866):863-4
Spinella F, Rosano L, Di Castro V,
et al. Green tea polyphenol
epigallocatechin-3-gallate inhibits the
endothelin axis and downstream signaling
pathways in ovarian carcinoma.
Mol Cancer Ther 2006;5(6):1483-92
Jeng AY, Mulder P, Kwan AL, Battistini B.
Nonpeptidic endothelin-converting
enzyme inhibitors and their potential
therapeutic applications.
Can J Physiol Pharmacol
2002;80(5):440-9
61.
Berger Y, Bernasconi CC,
Juillerat-Jeanneret L. Targeting the
endothelin axis in human melanoma:
combination of endothelin receptor
antagonism and alkylating agents. Exp Biol
Med (Maywood) 2006;231(6):1111-9
62.
Bagnato A, Rosano L, Di Castro V, et al.
Endothelin receptor blockade inhibits
proliferation of Kaposi’s sarcoma cells.
Am J Pathol 2001;158(3):841-7
63.
Rosano L, Spinella F, Di Castro V, et al.
Endothelin receptor blockade inhibits
molecular effectors of Kaposi’s sarcoma cell
invasion and tumor growth in vivo.
Am J Pathol 2003;163(2):753-62
64.
Lahav R, Heffner G, Patterson PH. An
endothelin receptor B antagonist inhibits
growth and induces cell death in human
melanoma cells in vitro and in vivo.
Proc Natl Acad Sci USA
1999;96(20):11496-500
65.
Mai HQ, Zeng ZY, Zhang CQ, et al.
Elevated plasma big ET-1 is associated
with distant failure in patients with
advanced-stage nasopharyngeal carcinoma.
Cancer 2006;106(7):1548-53
Spinella F, Rosano L, Di Castro V, et al.
Endothelin-1 and endothelin-3 promote
invasive behavior via hypoxia-inducible
factor-1alpha in human melanoma cells.
Cancer Res 2007;67(4):1725-34
66.
Mai HQ, Zeng ZY, Feng KT, et al.
Therapeutic targeting of the endothelin a
receptor in human nasopharyngeal
carcinoma. Cancer Sci
2006;97(12):1388-95
Samara E, Dutta S, Cao G, et al.
Single-dose pharmacokinetics of
atrasentan, an endothelin-A receptor
antagonist. J Clin Pharmacol
2001;41(4):397-403
67.
Morris CD, Rose A, Curwen J, et al.
Specific inhibition of the endothelin A
receptor with ZD4054: clinical and
pre-clinical evidence. Br J Cancer
2005;92(12):2148-52
68.
Carducci MA, Padley RJ, Breul J, et al.
Effect of endothelin-A receptor blockade
with atrasentan on tumor progression in
men with hormone-refractory prostate
cancer: a randomized, phase II,
placebo-controlled trial. J Clin Oncol
2003;21(4):679-89
69.
Zonnenberg BA, Groenewegen G,
Janus TJ, et al. Phase I dose-escalation
study of the safety and pharmacokinetics
of atrasentan: an endothelin receptor
antagonist for refractory prostate cancer.
Clin Cancer Res 2003;9(8):2965-72
70.
Ferreira SH, Romitelli M, de Nucci G.
Endothelin-1 participation in overt
and inflammatory pain.
J Cardiovasc Pharmacol
1989;13(Suppl 5):S220-2
71.
Raffa RB, Schupsky JJ, Martinez RP,
Jacoby HI. Endothelin-1-induced
nociception. Life Sci 1991;49(11):PL61-5
Jazaeri AA, Awtrey CS,
Chandramouli GV, et al. Gene expression
profiles associated with response to
chemotherapy in epithelial ovarian cancers.
Clin Cancer Res 2005;11(17):6300-10
Smollich M, Wulfing P. The endothelin
axis: a novel target for pharmacotherapy of
female malignancies. Curr Vasc Pharmacol
2007;5(3):239-48
Venuti A, Salani D, Manni V, et al.
Expression of endothelin 1 and
endothelin A receptor in HPV-associated
cervical carcinoma: new potential targets
for anticancer therapy. FASEB J
2000;14(14):2277-83
Titus B, Frierson HF Jr, Conaway M, et al.
Endothelin axis is a target of the lung
metastasis suppressor gene RhoGDI2.
Cancer Res 2005;65(16):7320-7
58.
Rosano L, Di Castro V, Spinella F, et al.
ZD4054, a potent endothelin receptor A
antagonist, inhibits ovarian carcinoma cell
proliferation. Exp Biol Med (Maywood)
2006;231(6):1132-5
59.
Rosano L, Di Castro V, Spinella F, et al.
ZD4054, a specific antagonist of the
endothelin A receptor, inhibits tumor
growth and enhances paclitaxel activity in
human ovarian carcinoma in vitro and
in vivo. Mol Cancer Ther
2007;6(7):2003-11
60.
Rosano L, Di Castro V, Spinella F, et al.
Combined targeting of endothelin A
receptor and epidermal growth factor
receptor in ovarian cancer shows enhanced
antitumor activity. Cancer Res
2007;67(13):6351-9
Expert Opin. Emerging Drugs (2010) 15(1)
13
�Anti-endothelin drugs in solid tumors
72.
73.
74.
75.
Khodorova A, Navarro B, Jouaville LS,
et al. Endothelin-B receptor activation
triggers an endogenous analgesic cascade
at sites of peripheral injury. Nat Med
2003;9(8):1055-61
Nelson JB. Endothelin receptor
antagonists. World J Urol
2005;23(1):19-27
Nelson JB, Nabulsi AA, Vogelzang NJ,
et al. Suppression of prostate cancer
induced bone remodeling by the
endothelin receptor A antagonist
atrasentan. J Urol 2003;169(3):1143-9
Takuwa Y, Ohue Y, Takuwa N,
Yamashita K. Endothelin-1 activates
phospholipase C and mobilizes Ca2+ from
extra- and intracellular pools in osteoblastic
cells. Am J Physiol
1989;257(6 Pt 1):E797-803
76.
Carducci MA, Saad F, Abrahamsson PA,
et al. A phase 3 randomized controlled trial
of the efficacy and safety of atrasentan in
men with metastatic hormone-refractory
prostate cancer. Cancer
2007;110(9):1959-66
77.
Nelson JB, Love W, Chin JL, et al. Phase 3,
randomized, controlled trial of atrasentan
in patients with nonmetastatic,
hormone-refractory prostate cancer.
Cancer 2008;113(9):2478-87
14
78.
79.
Michaelson MD, Kaufman DS, Kantoff P,
et al. Randomized phase II study of
atrasentan alone or in combination with
zoledronic acid in men with metastatic
prostate cancer. Cancer
2006;107(3):530-5
Armstrong AJ, Creel P, Turnbull J, et al. A
phase I-II study of docetaxel and atrasentan
in men with castration-resistant metastatic
prostate cancer. Clin Cancer Res
2008;14(19):6270-6
80.
Chiappori AA, Haura E, Rodriguez FA,
et al. Phase I/II study of atrasentan, an
endothelin A receptor antagonist, in
combination with paclitaxel and
carboplatin as first-line therapy in
advanced non-small cell lung cancer.
Clin Cancer Res 2008;14(5):1464-9
81.
James ND, Caty A, Borre M, et al. Safety
and efficacy of the specific endothelin-A
receptor antagonist ZD4054 in patients
with hormone-resistant prostate cancer and
bone metastases who were pain free or
mildly symptomatic: a double-blind,
placebo-controlled, randomised, phase 2
trial. Eur Urol 2009;55(5):1112-23
82.
Schelman WR, Liu G, Wilding G, et al. A
phase I study of zibotentan (ZD4054) in
patients with metastatic, castrate-resistant
Expert Opin. Emerging Drugs (2010) 15(1)
prostate cancer. Invest New Drugs 2009,
doi: 10.1007/s10637-009-9318-5
83.
Kefford R, Beith JM, Van Hazel GA, et al.
A phase II study of bosentan, a dual
endothelin receptor antagonist, as
monotherapy in patients with stage IV
metastatic melanoma. Invest New Drugs
2007;25(3):247-52
Affiliation
Antonio Russo†1 MD, Giuseppe Bronte1,
Sergio Rizzo1, Daniele Fanale1, Nicola Gebbia2 &
Viviana Bazan1
†
Author for correspondence
1
Università di Palermo,
Section of Medical Oncology,
Department of Surgical and
Oncological Sciences,
Via del Vespro 129,
90127 Palermo, Italy
Tel: +39 091 6552500; Fax: +39 091 6554529;
E-mail: lab-oncobiologia@usa.net
2
Professor,
Università di Palermo,
Section of Medical Oncology,
Department of Surgical and
Oncological Sciences,
Via del Vespro 129,
90127 Palermo, Italy
�
 Francesca Di Gaudio
Francesca Di Gaudio