Update
TRENDS in Microbiology
Vol.12 No.2 February 2004
| Research Focus
Variant Creutzfeldt – Jakob disease: between lymphoid
organs and brain
Markus Glatzel, Olivier Giger, Harald Seeger and Adriano Aguzzi
Institute of Neuropathology, Schmelzbergstr. 12, CH – 8091 Zürich, Switzerland
Prion diseases are often caused by peripheral uptake of
the infectious agent. To reach their ultimate target, the
central nervous system (CNS), prions enter their host,
replicate in lymphoid organs and spread via peripheral
nerves. Once the agent has reached the CNS disease
progression is rapid, resulting in neurodegeneration
and death. Many of these mechanisms have been
uncovered using genetically modified mice. A recently
published study has demonstrated the presence of
pathological prion protein in sympathetic ganglia of
patients suffering from variant Creutzfeldt–Jakob
disease, suggesting that these mechanisms might
apply to humans.
A substantial subset of human prion diseases is caused
by peripheral uptake of infectious prions [1]. Examples
include certain instances of iatrogenic Creutzfeldt – Jakob
disease (iCJD), attributed to exposure with material
derived from deceased individuals who had suffered from
an unrecognized human prion disease, such as recipients
of prion-contaminated growth hormone or dura mater
grafts. Variant Creutzfeldt – Jakob disease (vCJD) is a
further example of a human prion disease that is believed
to be initiated by peripheral uptake of prions. vCJD differs
from iCJD because it is thought to be caused by transmission of bovine spongiform encephalopathy (BSE)
prions to humans via the oral route [2]. The list of nonhuman prion diseases ascribed to peripheral prion uptake
includes transmissible spongiform encephalopathies, such
as scrapie, chronic wasting disease and BSE [3].
Neuroinvasion is not exclusive to prions. Many viruses
are capable of invading the central nervous system (CNS),
including rabies and several herpes viruses [4]. More
recent additions to this list are emerging viral diseases,
such as West Nile and Japanese encephalitis virus [5].
Although they do not appear to share any structural
features with conventional viruses, prions possess several
phenotypic attributes that are similar to those of the
aforementioned agents when it comes to neuroinvasion.
In all instances mentioned above, the infectious agent
reaches the CNS from peripheral sites of entry. However,
the methods used to accomplish this are diverse. Rhabdoviruses replicate in muscles and reach the CNS through
motor end plates, whereas herpes viruses enter the body
through mucosal surfaces and exploit retrograde axonal
transport to reach ganglia cells [6]. By contrast, West Nile
Corresponding authors: Markus Glatzel (markus.glatzel@usz.ch),
Adriano Aguzzi (adriano@pathol.unizh.ch).
www.sciencedirect.com
virus travels in the blood stream and ultimately reaches
the CNS by crossing the blood –brain barrier [5].
Prions, which are known to cause transmissible spongiform encephalopathies, are thought to be devoid of informational nucleic acids [7]. The idea that prions are entirely
made up of proteins originates from the fact that the only
molecule that consistently co-purifies with prion infectivity is a partially protease-resistant, abnormally folded
protein. Subsequently it was shown that this protein,
termed PrPSc, represents an isoform of the host-encoded
prion protein, PrPC [8]. Furthermore, prion infectivity
cannot be destroyed by methods that have been shown to
inactivate infectious agents containing informational
nucleic acids [9]. With this information in mind, one
might predict that neuroinvasion of an infectious agent
solely composed of a protein drastically differs from the
mechanisms exploited by infectious agents containing
nucleic acid. Surprisingly, this is not the case. Prion neuroinvasion has remarkable similarities to neuroinvasion by
viral agents. A primary phase of prion accumulation and
possibly also replication in organs of the lymphoreticular
system (LRS) is followed by a secondary phase that is
initiated once the agent has gained access to peripheral
nerves [8]. Although this model might oversimplify the
complex mechanisms of prion neuroinvasion, and studies
have shown that both mechanisms can occur independently,
the vast majority of experimental data can be explained on
the basis of these two stages of neuroinvasion (Table 1).
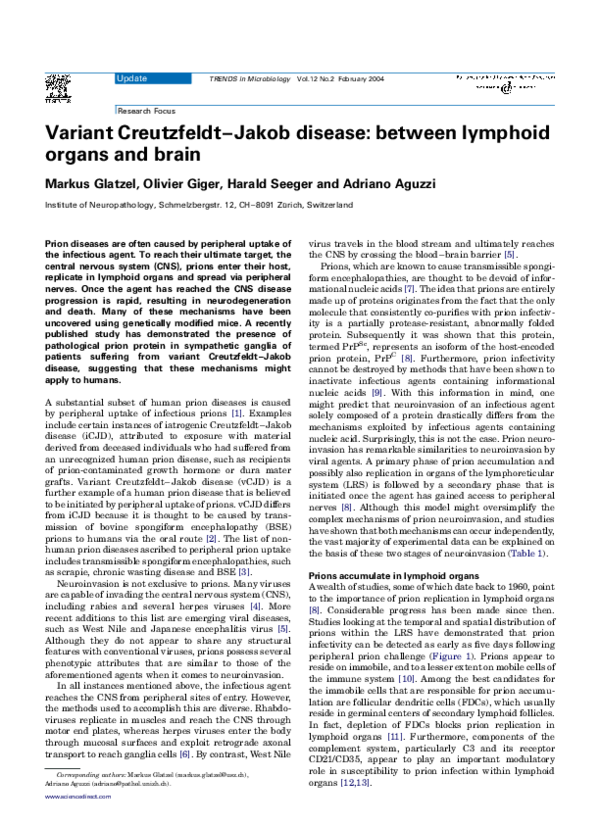
Prions accumulate in lymphoid organs
A wealth of studies, some of which date back to 1960, point
to the importance of prion replication in lymphoid organs
[8]. Considerable progress has been made since then.
Studies looking at the temporal and spatial distribution of
prions within the LRS have demonstrated that prion
infectivity can be detected as early as five days following
peripheral prion challenge (Figure 1). Prions appear to
reside on immobile, and to a lesser extent on mobile cells of
the immune system [10]. Among the best candidates for
the immobile cells that are responsible for prion accumulation are follicular dendritic cells (FDCs), which usually
reside in germinal centers of secondary lymphoid follicles.
In fact, depletion of FDCs blocks prion replication in
lymphoid organs [11]. Furthermore, components of the
complement system, particularly C3 and its receptor
CD21/CD35, appear to play an important modulatory
role in susceptibility to prion infection within lymphoid
organs [12,13].
�Update
52
TRENDS in Microbiology
Vol.12 No.2 February 2004
Table 1. Distribution of PrPSc and prion infectivitiy in sporadic Creutzfeldt –Jakob disease (CJD), variant CJD and mouse or hamster
scrapie
Organ system
Demonstration of PrPSc and prion infectivitya
Compartment
sCJD
vCJD
mouse or hamster
scrapie
PrPS
Infectivity
PrPSc
Infectivity
PrPSc
Infectivity
Gut-associated lymphoid tissue
Tonsil
Spleen
Appendix
Lymph node
n.d.
2
þ
n.d.
2
2
n.d.
þ
n.d.
þ
þ
þ
þ
þ
þ
n.d.
þ
þ
n.d.
n.d.
þ
n.d.
þ
þ
þ
þ
n.d.
þ
þ
þ
Sympathetic nervous system
Parasympathetic nervous system
þ
2
n.d.
2
n.d.
n.d.
n.d.
þ
n.d.
n.d.
n.d.
n.d.
þ
þ
n.d.
þ
n.d.
n.d.
Cortex
Retina
Optic nerve
Olfactory bulb
þ
þ
þ
þ
þ
þ
n.d.
n.d.
þ
þ
þ
n.d.
þ
n.d.
n.d.
n.d.
þ
n.d.
n.d.
n.d.
þ
þ
þ
n.d.
Lymphoreticular organs
Peripheral nervous system
Sensory-somatic nervous system
Autonomous nervous system
Central nervous system
Eye
a
Abbreviations: þ , detected; 2, not detected; n.d., not done.
Prions invade the CNS via peripheral nerves belonging to
the autonomous nervous system
Successful invasion of lymphoid organs does not automatically mean that prions will reach the CNS [14].
Moreover, prions can invade the CNS circumventing
accumulation within the LRS [15]. This might indicate
that a cell compartment distinct from the LRS is required,
and might even be sufficient, for prion neuroinvasion. A
prime candidate for this compartment is the peripheral
nervous system (Figure 1). Studies suggesting an involvement of peripheral nerves date back to the early eighties
[16]. From this time, essential insights have been obtained.
We know that PrPC, produced in neurons, is transported
via fast axonal transport and is organized in clusters on
the outer cell membrane where it cycles between the cell
surface and an endocytic compartment [17]. Peripheral
nerves have to express PrPC to propagate the infectious
Direct invasion
via nerves
Au
to
nom
ous
ner
vou
s
sys
tem
Oral or
i.p. infection
with prions
CNS
Secondary invasion
via nerves
Replication of prions
In lymphatic organs
Secondary invasion
via blood
TRENDS in Microbiology
Figure 1. Possible routes for prion neuroinvasion. Prions accumulate in lymphoreticular organs and invade the central nervous system (CNS) via peripheral
nerves belonging to the autonomous nervous system. In some instances, direct
neuroinvasion via the autonomous nervous system might occur. Neuroinvasion
by the hematogenous route might play a role in some prion diseases.
www.sciencedirect.com
agent [14,18]. Furthermore, there are studies indicating
that fast axonal transport does not appear to be involved in
prion neuroinvasion [19].
The peripheral nervous system (PNS) is composed of
several anatomically and functionally distinct subcompartments. Parts of the PNS, the autonomous nervous
system, especially the sympathetic and parasympathetic
portions, have been the focus of various studies on prion
neuroinvasion [20,21]. Apart from enabling prion neuroinvasion, the autonomous nervous system is capable of
transmitting and processing a variety of information and
contains as many neurons as the entire spinal cord.
Investigations of the temporal and spatial dynamics of
neuroinvasion have shown that spread of orally administered prions occurs via nerves belonging to the autonomous nervous system [20]. Additional refinement of
methods confirmed the physiological relevance of the
autonomous nervous system in prion neuroinvasion [22].
In fact, both the vagal nerve and sympathetic nerve fibers
contribute to this process. Surprisingly, sympathetic
nerves, besides being involved in the transport of prions,
might also accumulate and replicate prions in lymphatic
organs [22]. Recently, these findings were validated by a
study that investigated the involvement of the sympathetic nervous system in vCJD cases [23]. The authors
found PrPSc in stellate and celiac ganglia of three
individuals with confirmed vCJD, whereas stellate and
celiac ganglia of patients succumbing to sporadic CJD
were free of PrPSc. This supports the view that vCJD is
caused by oral uptake of prions, presumably originating
from BSE-contaminated material, and illustrates that
neuroinvasion of prions in humans suffering from vCJD
might occur via sympathetic nerves. However, the recent
discovery of PrPSc in the spleen of sCJD patients [24]
raises the question as to whether the pathogenesis of sCJD
and vCJD might be more closely related than previously
appreciated.
�Update
TRENDS in Microbiology
Open questions
Although it is obvious that an intact LRS and intact
PrPC-expressing autonomous nerves are essential components of prion neuroinvasion, many details of this
process remain enigmatic. It is not known whether prions
can be transferred directly from FDCs to sympathetic
nerve-endings [8]. Although a recently published study
demonstrates that the relative positioning of FDCs and
sympathetic nerves controls the efficiency of prion neuroinvasion [25], it is still not clear if additional cell types are
involved in this process. Moreover, it is unclear how prions
are actually transported within peripheral nerves. Axonal
and non-axonal transport mechanisms might be involved,
and even non-neuronal cells (such as Schwann cells) might
play a role. Some studies appear to indicate a non-axonal
transport mechanism, resulting in periaxonal deposition
of PrPSc. However, experiments that would provide us with
an unambiguous answer to this problem, such as direct
visualization of PrPSc transport in nerves, are non-existent
[18,26]. Until this matter is resolved, models of PrPSc
transport, such as a ‘domino’ mechanism by which incoming PrPSc converts resident PrPC on the axolemmal surface, remain hypothetical.
References
1 Aguzzi, A. et al. (2001) Prions: health scare and biological challenge.
Nat. Rev. Mol. Cell Biol. 2, 118 – 126
2 Bruce, M.E. et al. (1997) Transmissions to mice indicate that ‘new
variant’ CJD is caused by the BSE agent. Nature 389, 498– 501
3 Taylor, D.M. (2002) Current perspectives on bovine spongiform
encephalopathy and variant Creutzfeldt– Jakob disease. Clin. Microbiol. Infect. 8, 332 – 339
4 Marsh, R.F. (1974) Slow virus diseases of the central nervous system.
Adv. Vet. Sci. Comp. Med. 18, 155 – 178
5 Cooper, J.E. (2002) Diagnostic pathology of selected diseases in
wildlife. Rev. Sci. Tech. 21, 77 – 89
6 Tyler, K.L. and McPhee, D.A. (1987) Molecular and genetic aspects of
the pathogenesis of viral infections of the central nervous system. Crit.
Rev. Neurobiol. 3, 221 – 243
7 Prusiner, S.B. (1982) Novel proteinaceous infectious particles cause
scrapie. Science 216, 136 – 144
8 Aguzzi, A. Prions and the immune system: a journey through gut,
spleen, and nerves. Adv. Immunol. (in press)
9 Riesner, D. et al. (1993) Prions and nucleic acids: search for ‘residual’
Vol.12 No.2 February 2004
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
53
nucleic acids and screening for mutations in the PrP-gene. Dev. Biol.
Stand. 80, 173 – 181
Clarke, M.C. and Kimberlin, R.H. (1984) Pathogenesis of mouse
scrapie: distribution of agent in the pulp and stroma of infected
spleens. Vet. Microbiol. 9, 215– 225
Montrasio, F. et al. (2000) Impaired prion replication in spleens of mice
lacking functional follicular dendritic cells. Science 288, 1257 – 1259
Klein, M.A. et al. (2001) Complement facilitates early prion pathogenesis. Nat. Med. 7, 488 – 492
Mabbott, N.A. et al. (2001) Temporary depletion of complement
component C3 or genetic deficiency of C1q significantly delays onset
of scrapie. Nat. Med. 7, 485– 487
Blättler, T. et al. (1997) PrP-expressing tissue required for transfer of
scrapie infectivity from spleen to brain. Nature 389, 69 – 73
Race, R. et al. (2000) Entry versus blockade of brain infection following
oral or intraperitoneal scrapie administration: role of prion protein
expression in peripheral nerves and spleen. J. Virol. 74, 828 – 833
Kimberlin, R.H. and Walker, C.A. (1980) Pathogenesis of mouse
scrapie: evidence for neural spread of infection to the CNS. J. Gen.
Virol. 51, 183 – 187
Borchelt, D.R. et al. (1994) Rapid anterograde axonal transport of the
cellular prion glycoprotein in the peripheral and central nervous
systems. J. Biol. Chem. 269, 14711 – 14714
Glatzel, M. and Aguzzi, A. (2000) PrP(C) expression in the peripheral
nervous system is a determinant of prion neuroinvasion. J. Gen. Virol.
81, 2813 – 2821
Kunzi, V. et al. (2002) Unhampered prion neuroinvasion despite
impaired fast axonal transport in transgenic mice overexpressing fourrepeat tau. J. Neurosci. 22, 7471 – 7477
Beekes, M. et al. (1998) Cerebral targeting indicates vagal spread of
infection in hamsters fed with scrapie. J. Gen. Virol. 79, 601– 607
McBride, P.A. and Beekes, M. (1999) Pathological PrP is abundant
in sympathetic and sensory ganglia of hamsters fed with scrapie.
Neurosci. Lett. 265, 135 – 138
Glatzel, M. et al. (2001) Sympathetic innervation of lymphoreticular
organs is rate limiting for prion neuroinvasion. Neuron 31, 25 – 34
Haik, S. et al. (2003) The sympathetic nervous system is involved in
variant Creutzfeldt – Jakob disease. Nat. Med. 9, 1121 – 1122
Glatzel, M. et al. (2003) Extraneural pathologic prion protein in
sporadic Creutzfeldt–Jakob disease. New Engl. J. Med. 349, 1812–1820
Prinz, M. et al. (2003) Positioning of follicular dendritic cells within the
spleen controls prion neuroinvasion. Nature 425, 957 – 962
Hainfellner, J.A. and Budka, H. (1999) Disease associated prion
protein may deposit in the peripheral nervous system in human
transmissible spongiform encephalopathies. Acta Neuropathol. (Berl.)
98, 458 – 460
0966-842X/$ - see front matter q 2003 Elsevier Ltd. All rights reserved.
doi:10.1016/j.tim.2003.12.001
Horizontal gene transfer and microbial adaptation to
xenobiotics: new types of mobile genetic elements
and lessons from ecological studies
Dirk Springael1 and Eva M. Top2
1
Laboratory of Soil and Water Management, Department of Land Management, Faculty of Agricultural and Applied Biological
Sciences, Catholic University of Leuven, B-3001 Heverlee, Belgium
2
Department of Biological Sciences, 347 Life Sciences Building South, University of Idaho, Moscow ID 83844-3051, USA
The characterization of bacteria that degrade organic
xenobiotics has revealed that they can adapt to these
compounds by expressing ‘novel’ catabolic pathways.
Corresponding author: Dirk Springael (dirk.springael@agr.kuleuven.ac.be).
www.sciencedirect.com
At least some of them appear to have evolved by patchwork assembly of horizontally transmitted genes and
subsequent mutations and gene rearrangements.
Recent studies have revealed the existence of new
types of xenobiotic catabolic mobile genetic elements,
�
 Adriano Aguzzi
Adriano Aguzzi