Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser.
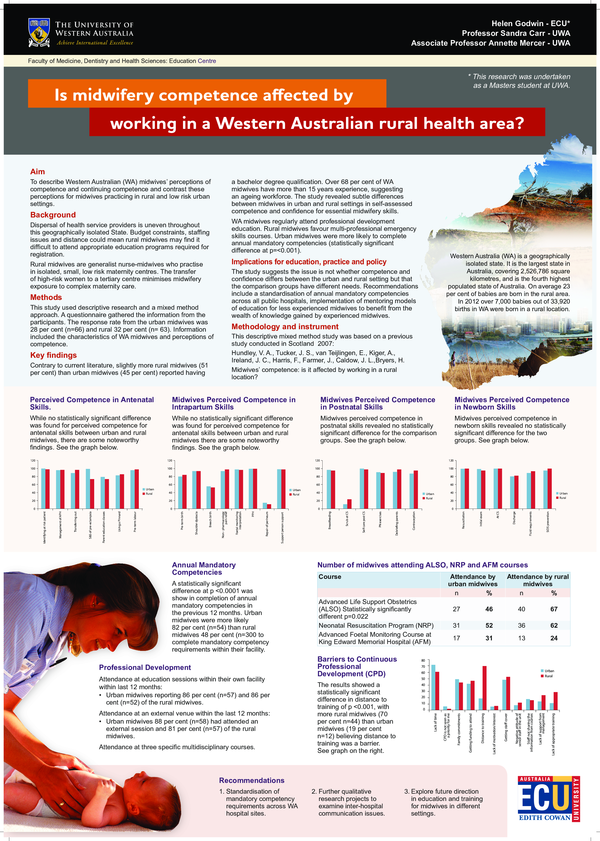
Is midwifery competence affected by working in a Western Australian rural area
Is midwifery competence affected by working in a Western Australian rural area
2013, Women and Birth
Related Papers
2007 •
Australian Health Review
Contemporary issues in the workforce and education of Australian midwives2013 •
2017 •
the complex and challenging nature of rural midwifery is a global issue. New Zealand and Scotland both face similar ongoing challenges in sustaining a rural midwifery workforce, and understanding the best preparation for rural midwifery practice. This study aimed to explore the range of skills, qualities and professional expertise needed for remote and rural midwifery practice. online mixed methods: An initial questionnaire via a confidential SurveyMonkey® was circulated to all midwives working with rural women and families in New Zealand and Scotland. A follow-up online discussion forum offered midwives a secure environment to share their views about the specific skills, qualities and challenges and how rural midwifery can be sustained. Data presented were analysed using qualitative descriptive thematic analysis. 222 midwives participated in this online study with 145 from New Zealand and 77 from Scotland. underpinning rural midwifery practice is the essence of 'fortitude' ...
2011 •
2011 •
2024 •
VIAJE A LOS MUNDOS SUPERIORES Y EL CAMINO HACIA LA CONSCIENCIA CRÍSTICA.
Jacobin Brasil
A desinformação como método: Bolsonaro e o novo regime de verdade na pandemia (Jacobin Brasil, fevereiro 2021)2021 •
https://jacobin.com.br/2021/02/a-desinformacao-como-metodo-bolsonaro-e-o-novo-regime-de-verdade-na-pandemia/
The First Three Hymns of the Ahunauuaitī Gāθā (Ahunauuaiti Gatha)
The First Three Hymns of the Ahunauuaitī Gāθā (Brill 2022, TOC)2022 •
2022 book based on my PhD thesis (SOAS 2021). See https://brill.com/display/title/63273. Full reference: Peschl, Benedikt. 2022. The first three hymns of the Ahunauuaitī Gāθā. The Avestan text of Yasna 28–30 and its tradition (Handbook of Oriental Studies — Corpus Avesticum 32/4). Leiden – New York: Brill.
RELATED PAPERS
2012 •
InterCambios: Dilemas y Transiciones de la Educación Superior
Poner en práctica la educación social: acción, reflexión e incertidumbre2015 •
Taiwanese Journal of Entomological Studies
臺灣研蟲誌第四卷第二期 Taiwanese Journal of Entomological Studies 4(2)2024 •
Revista de Jurisprudencia Laboral (RJL)
Personal laboral indefinido no fijo adscrito a plaza funcionarial cubierta por procedimiento reglamentario y extinción del contrato de trabajo: aplicación del art. 52.c) ET por amortización encubierta de su puesto de trabajo como personal laboral: STS-SOC núm. 528/2019, de 3 de julio2019 •
2019 •
Revista chilena de infectología
Recomendaciones para el diagnóstico y manejo de la infección por citomegalovirus en la mujer embarazada y el recién nacidoRevista Valenciana estudios de filosofía y letras
El decadentismo mexicano y los discursos científicos en diálogo. El caso de Alberto Leduc: del palacio a la vecindad- Find new research papers in:
- Physics
- Chemistry
- Biology
- Health Sciences
- Ecology
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
 Annette Mercer
Annette Mercer