Clinical Chemistry 47:5
809 – 814 (2001)
Minireview
Molecular Diagnosis of Mycobacteria
Hanna Soini1,2 and James M. Musser3*
agent of tuberculosis (TB).4 TB is one of the leading
infectious diseases in the world and is responsible for
more than 2 million deaths and 8 million new cases
annually (1 ). M. avium is the most common nontuberculous mycobacterium found in clinical specimens. Infections caused by this species can be clinically significant,
especially when associated with AIDS (2 ). The major
difference between TB and other mycobacterial infections
is that M. tuberculosis is transmitted from person to
person. Thus it is particularly important to diagnose TB as
rapidly as possible. In addition, antibiotic treatment varies according to the species of mycobacterium.
Although the initial diagnosis of mycobacterial disease
often is based on clinical data, definitive diagnosis usually
involves the isolation and identification of the infecting
organism in the laboratory. The usual laboratory procedure for clinical specimens involves decontamination and
digestion of the specimen, microscopic examination for
the presence of acid-fast bacilli (AFB), isolation of the
organism by culture, and identification and drug susceptibility testing of the recovered organism. Because of the
slow growth rate of mycobacteria, isolation, identification, and drug susceptibility testing can take several
weeks or longer.
During the past 10 years, several molecular methods
have been developed for direct detection, identification,
and susceptibility testing of mycobacteria. These methods
can potentially reduce the diagnostic time from weeks to
days. The aim of this review is to briefly describe the
currently available methods and their impact on diagnosis and management of TB.
Tuberculosis is one of the leading infectious diseases in
the world and is responsible for more than 2 million
deaths and 8 million new cases annually. Because of the
slow growth rate of the causative agent Mycobacterium
tuberculosis, isolation, identification, and drug susceptibility testing of this organism and other clinically
important mycobacteria can take several weeks or
longer. During the past several years, many molecular
methods have been developed for direct detection, species identification, and drug susceptibility testing of
mycobacteria. These methods can potentially reduce the
diagnostic time from weeks to days. Currently, two
nucleic acid amplification methods, the Enhanced Mycobacterium tuberculosis Direct Test (Gen-Probe) and
the Amplicor Mycobacterium tuberculosis Test (Roche
Diagnostic Systems), have been approved by the Food
and Drug Administration for direct detection of M.
tuberculosis from clinical specimens. PCR-based sequencing has become commonly used to identify many
mycobacterial species. DNA probes have been widely
used for species determination of the most commonly
encountered mycobacteria. High-density oligonucleotide arrays (DNA microarrays) also have been applied
to simultaneous species identification and detection of
mutations that confer rifampin resistance in mycobacteria.
© 2001 American Association for Clinical Chemistry
The genus Mycobacterium consists of the members of the
Mycobacterium tuberculosis complex and .80 species of
nontuberculous mycobacteria, including pathogenic, opportunistic, and nonpathogenic species. The most important species of this genus is M. tuberculosis, the causative
Direct Detection of Mycobacteria from Specimens
Many mycobacterial species, including M. tuberculosis,
grow extremely slowly in the laboratory and require 3– 8
weeks of incubation on solid medium or at least 2 weeks
in a radiometric liquid culture system (BACTEC). This
1
Department of Pathology, Baylor College of Medicine, Houston, TX
77030.
2
Mycobacterial Reference Laboratory, National Public Health Institute,
Kiinamyllynkatu 13, 20520 Turku, Finland.
3
Laboratory of Human Bacterial Pathogenesis, Rocky Mountain Laboratories, National Institute of Allergy and Infectious Diseases, National Institutes
of Health, 903 South 4th St., Hamilton, MT 59840.
*Author for correspondence. Fax 406-363-9427; e-mail jmusser@niaid.
nih.gov.
Received December 29, 2000; accepted February 15, 2001.
4
Nonstandard abbreviations: TB, tuberculosis; AFB, acid-fast bacilli; NAA,
nucleic acid amplification; FDA, Food and Drug Administration; E-MTD,
Enhanced Mycobacterium tuberculosis Direct Test; Amplicor, Amplicor Mycobacterium tuberculosis Test; RIF, rifampin; INH, isoniazid; and LiPA, Line Probe
assay.
809
�810
Soini and Musser: Molecular Diagnosis of Mycobacteria
slow growth often leads to a delay in TB diagnosis.
Nucleic acid amplification (NAA) methods allow for
detection of mycobacterial DNA or RNA directly from the
specimens before the culture results are available.
The Food and Drug Administration (FDA) has approved two NAA tests for direct detection of M. tuberculosis from clinical specimens. These are the Enhanced
Mycobacterium tuberculosis Direct Test (E-MTD; GenProbe, San Diego, CA) and the Amplicor Mycobacterium
tuberculosis Test (Amplicor; Roche Diagnostic Systems,
Inc., Branchburg, NJ).
amplicor
The Amplicor test is based on the PCR. In this assay,
mycobacterial DNA is amplified with genus-specific
primers formulated on the basis of the 16S rRNA gene.
After amplification, the amplicons are denatured to form
single strands and added to a microtiter plate containing
a bound, M. tuberculosis complex-specific oligonucleotide
probe. An avidin-horseradish peroxidase conjugate then
binds to the bound, biotin-labeled amplicons. The conjugate then reacts with peroxide and 3,39,5,59-tetramethylbenzidine in dimethylformamide to form a color complex.
The results are measured with a photometer. False-positive results produced by carryover contamination are
prevented by the incorporation of dUTP coupled with
uracil-N-glycosylase restriction. After the clinical specimen has been processed with the standard N-acetyl-lcysteine–NaOH decontamination method, the Amplicor
results are available in ;6.5 h. An automated version of
this test is available in Europe (Cobas Amplicor).
The overall sensitivity of the Amplicor test (compared
with culture) for respiratory specimens is 79.4 –91.9%, the
specificity is 99.6 –99.8%, the positive predictive value is
92.6 –96.6%, and the negative predictive value is 98.6 –
98.7% (Table 1). However, the sensitivity for smearnegative specimens is somewhat lower, 40.0 –73.1% (3–5 ).
Therefore, the Amplicor test has been approved by the
FDA only for direct detection of M. tuberculosis in AFB
smear-positive respiratory specimens. Chin et al. (6 ) reported that the sensitivity of the Amplicor test was similar
to that of culture (58% vs 56%) for detecting M. tuberculosis from respiratory specimens when the clinical case
definition of TB was used as the reference standard.
However, Al Zahrani et al. (7 ) reported that although the
Amplicor test had excellent specificity (100%), it was less
sensitive than culture (42% vs 73%) for diagnosis of
minimal active pulmonary TB (patients suspected of
having TB but without spontaneous sputum or with
AFB-negative smears).
e-mtd
The E-MTD test is based on the transcription-mediated
amplification system developed by Kwoh et al. (8 ). In this
assay, rRNA is released from the target cells by sonication, and a promoter-primer binds to the rRNA target.
Reverse transcriptase is then used to copy rRNA to a
cDNA-RNA hybrid. The initial RNA strand is degraded,
and a second primer binds to the cDNA and is extended,
leading to the formation of double-stranded cDNA, which
is then transcribed by DNA-directed RNA polymerase to
produce more rRNA molecules. The new transcripts serve
as templates for reverse transcription and further amplification. The RNA amplicons are detected with an acridinium ester-labeled DNA probe in a solution hybridization assay. Importantly, the amplification procedure is
isothermal and the reaction is performed in a single tube,
which helps to reduce carryover contamination. After
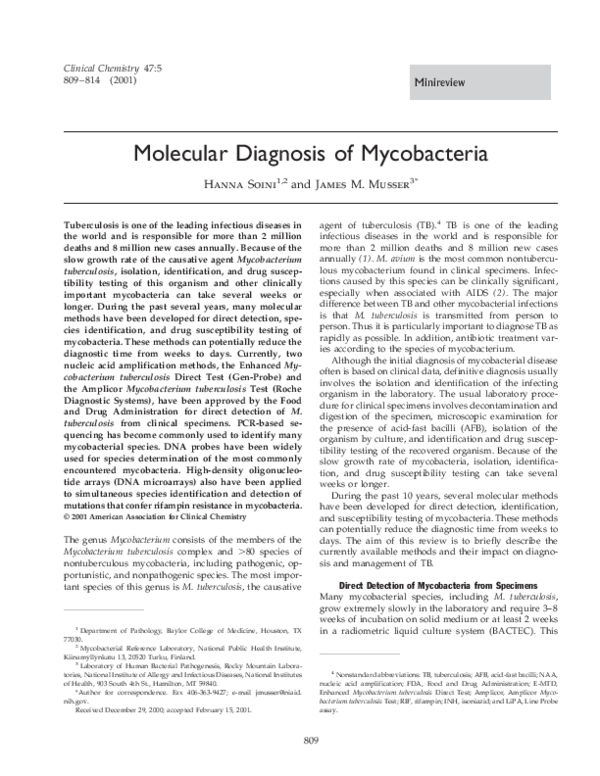
Table 1. Comparison of commercially available, FDA-approved NAA tests for detection of M. tuberculosis
complex organisms.
Test
Amplicor
E-MTD
Manufacturer
Amplification technique
Target
Analytical sensitivity
Clinical sensitivity
Clinical specificity
Sensitivity for AFB smear-negative specimens
Positive predictive value
Negative predictive value
Control for amplification inhibitors
Prevention of carryover contamination
Turnaround time after specimen decontamination
Instrumentation needed
FDA-approved use
Roche
PCR
16S rDNA
$20 organisms/reactionb
79.4–91.9%c
99.6–99.8%c
40.0–73.1%c
92.6–96.6%c
98.6–98.7%c
Yes
Yes
6.5 h
Thermocycler, photometer
AFB smear-positive respiratory
specimens
Gen-Probe
TMAa
rRNA
NA
90.9–95.2d
98.8–100%d
83–100d
83.3–100%d
98.4–99.6%d
No
No
3.5 h
Heat block, luminometer
AFB smear-positive and smear-negative
respiratory specimens
a
TMA, transcription-mediated amplification; NA, not available.
Based on manufacturer’s claim.
c
Based on Refs. (3–5 ).
d
Based on Refs. (9 –11 ).
b
�Clinical Chemistry 47, No. 5, 2001
standard decontamination of the clinical specimen, the
E-MTD test can be completed in 3.5 h.
The E-MTD test has been reported to perform well
with both AFB smear-positive and smear-negative specimens. The overall sensitivity (compared with culture) for
respiratory specimens is 90.9 –95.2%, the specificity is
98.8 –100%, the positive predictive value is 83.3–100%, and
the negative predictive value is 98.4 –99.6% (9 –11 ). In a
study where the performance of the E-MTD test was
assessed based on the degree of clinical suspicion of TB,
the greatest utility was documented for patients with an
intermediate clinical suspicion of having TB (12 ). The
E-MTD test is FDA-approved for detection of M. tuberculosis in both AFB smear-positive and smear-negative specimens.
Scarparo et al. (13 ) compared the performance of the
E-MTD and the Cobas Amplicor tests with 486 respiratory
and nonrespiratory specimens obtained from 323 patients.
No significant differences were observed between the
results of the assays. However, it was noted that although
the turnaround time is shorter for the E-MTD test, the
Amplicor test can be fully automated and has an internal
control for monitoring amplification inhibitors.
clinical utility
The clinical utility of the commercial NAA tests has been
discussed in a recent review (14 ) and in guidelines
published by the FDA (15 ). In brief, it is recommended
that sputum specimens be collected on 3 different days for
AFB smear and culture. The NAA test should be performed on the first specimen collected, the first smearpositive specimen, and additional specimens if needed. If
the first specimen is both AFB smear-positive and NAApositive, the patient can be presumed to have TB. However, if the specimen is smear-positive but NAA-negative,
a test for inhibitors should be performed. This option is
available in the Amplicor test, but if the E-MTD test is
used, a specimen to which M. tuberculosis DNA has been
added must be analyzed. If inhibitors are not detected and
additional specimens remain NAA-negative, the patient
can be presumed to have nontuberculous mycobacteria.
However, if inhibitors are detected, the NAA test does not
offer any diagnostic help. If a specimen is smear-negative
and NAA-positive and the same result is obtained with an
additional specimen, the patient can be presumed to have
TB. In the case that all sputum specimens remain smearnegative and NAA-negative, the patient can be presumed
to be not infectious; however, this does not exclude the
possibility of active TB, and clinical judgment must be
used in decisions regarding TB therapy (14, 15 ).
With respect to extrapulmonary TB, clinical diagnosis
often is uncertain, and NAA tests could provide important information to the clinician. Although the currently
available NAA tests have been approved for respiratory
specimens only, they have also been used to test several
different types of nonrespiratory specimens. In general,
the performance of both tests with nonrespiratory speci-
811
mens has been similar to their performance with respiratory specimens (13, 16, 17 ). NAA tests also appear to be
useful for early identification of M. tuberculosis complex
for all specimen types (except for blood) grown in liquid
cultures (18, 19 ). However, the NAA tests must be validated in house if they are used for other than respiratory
specimens.
In conclusion, the currently available NAA tests can
enhance diagnostic speed, but they do not replace AFB
smear or culture. Because the tests can only detect M.
tuberculosis, cultures are still needed for identification of
nontuberculous mycobacteria and for drug susceptibility
testing. Because the tests cannot distinguish between live
and dead organisms, they cannot be used to monitor TB
therapy. Clinicians should interpret the NAA test results
based on the clinical situation, and the tests should
usually be performed at the request of the clinician.
Identification of Mycobacterial Species from Culture
Mycobacterial isolates have traditionally been identified
to the species level based on their reactions in a series of
phenotypic and biochemical tests. However, the biochemical reactions of isolates of the same species may vary
from each other and from time to time, and in many cases
no definitive identification is obtained. Because biochemical testing is slow, cumbersome, and may yield ambiguous results, laboratories are increasingly using molecular
methods for species identification.
dna probes
Commercial DNA probes (AccuProbe; Gen-Probe Inc.)
have been available for some time for identification of
clinically important mycobacterial species, including M.
tuberculosis complex, M. avium, M. intracellulare, M. avium
complex, M. kansasii, and M. gordonae. The tests are based
on species-specific DNA probes that hybridize with rRNA
released from bacteria. The probes are labeled with acridinium ester, and results are measured with a luminometer. For culture-positive specimens, the turnaround time
for the method is ;2 h. The method is very easy to
perform, and no special instrumentation is needed. The
probes have been evaluated extensively in clinical practice
and are rapid, sensitive, and specific (20, 21 ). The probes
can also be combined with the BACTEC or other liquidbased culture systems to further decrease the time needed
for species identification (22, 23 ). However, probes are
not available for all pathogenic mycobacterial species, and
those isolates must be identified by other methods. In
addition, the M. tuberculosis complex probe cannot differentiate between the members of this complex (M. tuberculosis, M. bovis, M. bovis BCG, M. africanum, and M. microti).
pcr-based sequencing
PCR-based sequencing has become the gold standard for
identification of mycobacterial species. The method consists of PCR amplification of mycobacterial DNA with
genus-specific primers and sequencing of the amplicons.
�812
Soini and Musser: Molecular Diagnosis of Mycobacteria
The organism is identified by comparison of the nucleotide sequence with reference sequences. As commonly
practiced, only one sequencing reaction is needed for a
definitive identification. This method also allows for
direct detection of mycobacterial species that cannot be
grown on conventional laboratory culture media, and
several previously unrecognized species have been identified (24, 25 ).
The target most commonly used is the gene coding for
the 16S rRNA. This gene is present in all bacterial species
and contains both conserved and variable regions, making it an ideal target for taxonomic purposes. The 16S
rRNA gene has been sequenced from a large number of
mycobacterial species, and the identification method
based on this gene has been evaluated extensively in
diagnostic laboratories. Sequencing of two hypervariable
regions of the 16S rRNA gene allows for identification of
the majority of mycobacterial species. However, members
of the M. tuberculosis complex cannot be distinguished.
Similarly, an important pathogen, M. kansasii, has a sequence identical to that of a nonpathogenic species, M.
gastri, and additional 16S rRNA gene regions need to be
sequenced to differentiate M. marinum from M. ulcerans
(26, 27 ).
Several other target genes have been characterized for
this purpose. The genes coding for the 32-kDa protein
(28 ), the 65-kDa heat shock protein (29 ), and the 16S-23S
rRNA internal transcribed spacer (30 ) contain enough
sequence diversity to distinguish all clinically important
mycobacteria except for the members of the M. tuberculosis complex. These target genes also allow for differentiation of M. kansasii and M. gastri. In addition, because of
the intraspecies variation observed in the 65-kDa protein
gene, this target can also be used for distinguishing clones
of certain mycobacterial species (31 ).
dna microarrays
High-density oligonucleotide arrays (DNA microarrays)
offer the possibility of rapid examination of large amounts
of DNA sequences with a single hybridization step. This
approach has recently been applied to simultaneous species identification and detection of mutations that confer
rifampin resistance in mycobacteria. This technique is
based on hybridization of fluorescently labeled PCR amplicons generated from bacterial colonies to a DNA array
containing nucleotide probes. The bound amplicons emit
a fluorescent signal that is detected with a scanner. The
probes used in this array are based on 82 unique 16S
rRNA sequences that allow for discrimination of 54 mycobacterial species and 51 sequences that contain unique
rpoB gene mutations. The method correctly identified 67
of the 70 isolates representing 27 mycobacterial species.
All three M. szulgai isolates were identified as M. malmoense because of an error in the probe sequence. The
turnaround time for this method when performed on
culture positive specimens was only 4 h (32, 33 ).
Molecular methods offer many advantages over con-
ventional methods in the identification of mycobacterial
species. The results are obtained rapidly, are reliable and
reproducible, and even mixed or contaminated cultures
can be analyzed. The probes are already widely used in
clinical laboratories for the identification of the most
common mycobacterial species. Because automatic DNA
sequencers and the programs used for analyzing sequence
data have become technically simpler, the PCR-based
sequencing method is now being used in many mycobacterial reference laboratories as the routine method for
species assignment. The DNA microarray method holds
great promise for the future because it is easy to perform,
it can be readily automated, and it allows for identification of a large number of mycobacterial species in one
reaction.
Identification of Antibiotic Resistance-associated Mutations
Drug-resistant M. tuberculosis isolates are a serious threat
to TB control because only a few effective drugs are
available for treatment of this disease. M. tuberculosis
acquires drug resistance by antibiotic selection of mutations that occur randomly at chromosomal loci. No plasmids or transposable elements (horizontal gene transfer)
are involved in this process. Individual nucleotide changes
(point mutations) confer resistance to single drugs, and
the stepwise accumulation of these mutations leads to
multidrug-resistant TB. Drug-resistant strains emerge when
chemotherapy is intermittent or otherwise inadequate.
After the primary culture results are available, conventional drug susceptibility testing performed on solid medium takes ;2– 4 weeks. When the radiometric BACTEC
drug susceptibility testing system is used, several weeks
are needed to obtain results. Advances in molecular
biology have made it possible to investigate the genetic
mechanisms of drug resistance in M. tuberculosis and to
develop methods for rapid detection of mutations associated with resistance. The currently available methods
have mostly been developed for detection of rifampin
(RIF) resistance because the genetic basis of RIF resistance
in M. tuberculosis is fairly simple and well characterized,
whereas the molecular basis of resistance to other firstline TB drugs is much more complex. Moreover, resistance to RIF can often be used as a marker of multidrugresistant TB.
genetic basis of resistance
The genetic basis of resistance to the five first-line TB
drugs is described here in brief. A detailed review of this
topic has recently been published (34 ). RIF is a semisynthetic derivative of rifamycin that is used as a first-line TB
drug. RIF binds to the b subunit of RNA polymerase,
encoded by the rpoB gene, and inhibits transcription
initiation. Virtually all (96%) RIF-resistant isolates have
point mutations in an 81-bp region of this gene, and these
mutations are absent in susceptible isolates, making it an
ideal target for development of molecular drug susceptibility testing methods (34 ).
�813
Clinical Chemistry 47, No. 5, 2001
In contrast to RIF, the genetic basis of resistance to
other TB drugs is more complex. Isoniazid (INH) is a
synthetic, bactericidal agent that is used only for treatment of TB because basically all other bacteria are inherently resistant to INH. Alterations in a relatively large
number of genes have been associated with INH resistance, but mutations in two genes, katG and inhA, are
found in 75– 85% of INH-resistant M. tuberculosis isolates.
Streptomycin is an aminoglycoside antibiotic that inhibits
protein synthesis. Approximately 65–75% of streptomycin-resistant M. tuberculosis isolates have mutations in the
16S rRNA gene or the rpsL gene, which codes for the
ribosomal protein S12. More than 70% of the pyrazinamide-resistant M. tuberculosis isolates have mutations in
the pncA gene, which encodes for pyrazinamidase, an
enzyme that converts pyrazinamide to its active form.
Ethambutol inhibits the incorporation of essential mycolic
acids into the mycobacterial cell wall. Mutations in the
embB gene are associated with ethambutol resistance in
;70% of resistant isolates (34 ).
pcr-based sequencing
PCR-based sequencing is the main technique used to
elucidate the genetic mechanisms of drug resistance in M.
tuberculosis. It is the most direct and reliable method for
studying mutations and allows for detection of both
previously recognized and unrecognized mutations. Unfortunately, the method is not as readily applicable for
routine identification of drug resistance mutations as it is
for identification of mycobacterial species because many
different genes may be involved, as is the case in INH
resistance, or the mutations may be scattered in a large
segment of the gene. This means that several sequencing
reactions need to be performed for each isolate. However,
for targets such as rpoB, where mutations associated with
RIF resistance are concentrated in a very short segment of
the gene, PCR-based sequencing is a useful technique (31 ).
line-probe assay
The Line Probe assay (LiPA; Inno-Genetics N.V., Zwijndrecht, Belgium) has been developed for rapid detection
of RIF resistance. The test is based on the reverse hybridization method, and it consists of PCR amplification of a
segment of the rpoB gene and denaturation and hybridization of the biotinylated PCR amplicons to capture
probes bound to a nitrocellulose strip. The bound amplicons are then detected with alkaline phosphatase-conjugated streptavidin and BCIP/NBT chromogen, producing
a color reaction. The LiPA test strip contains five probes
for wild-type rpoB sequences and four probes for specific
rpoB mutations, in addition to a conjugate control and M.
tuberculosis control probes. The interpretation of the banding pattern on the strip allows for identification of M.
tuberculosis complex and detection of rpoB mutations. The
test can be performed on M. tuberculosis cultures or
directly from clinical specimens. The turnaround time for
the test is ,48 h. Overall concordance of the LiPA test
with phenotypic susceptibility testing and direct sequencing, when performed from cultures, has been reported to
be good, varying from 92.2% to 99.0% (35–37 ). Although
the LiPA test only detects 4 of the 35 distinct rpoB
mutations, ;75% of the RIF-resistant clinical isolates carry
1 of the 4 mutations (34 ), making the LiPA test a useful
method for rapid detection of RIF resistance. However,
the test cannot be used for detection of rare mutations.
dna microarrays
DNA microarray technology described for mycobacterial
species identification can also be used for rapid detection
of mutations that are associated with resistance to TB
drugs. Gingeras et al. (32 ) studied 44 RIF-resistant M.
tuberculosis isolates with a DNA array containing sequences from the rpoB gene. A total of 40 isolates had a
previously recognized mutation, one new mutation was
detected, and no rpoB mutations were found in the
remaining 3 isolates by either the DNA array or sequencing. These results are in accordance with the data showing
that ;4% of the RIF-resistant isolates have an unknown
resistance mechanism (34 ). In a study performed by
Troesch et al. (33 ), 15 RIF-resistant and 1 sensitive M.
tuberculosis isolate were analyzed with a similar DNA
array. All 15 resistant isolates had mutations in the rpoB
gene, and the mutations were correctly detected with the
DNA array. Mutation types included single- and doublebase substitutions and three- and six-base deletions; in
addition, one previously unrecognized mutation was
found. The results were completely concordant with
sequencing results (33 ). A DNA microarray for simultaneous detection of various drug resistance determinants is
currently being developed. It contains sequences from the
katG, inhA, rpoB, rpsL, and gyrA (associated with fluoroquinolone resistance) genes (32 ). This approach has the
potential of becoming the most effective and rapid
method for detection of drug resistance mutations in M.
tuberculosis.
Despite the clear advantages that molecular methods
offer for drug susceptibility testing, they all suffer from
the problem that the genetic basis of resistance is not fully
understood for any TB drug for all M. tuberculosis isolates.
This means that detection of a mutation associated with
resistance is clinically relevant, but a lack of mutations in
the target gene does not necessarily mean that the organism is susceptible to the drug in question. The currently
available molecular methods may aid in rapid detection of
mutations associated with drug resistance, but the test
results must always be confirmed by phenotypic methods.
References
1. Dye C, Scheele S, Dolin P, Pathania V, Raviglione MC. Global
burden of tuberculosis: estimated incidence, prevalence, and
mortality by country. JAMA 1999;282:677– 86.
2. Horsburgh CR. Mycobacterium avium complex infection in the
acquired immunodeficiency syndrome. N Engl J Med 1991;324:
1332– 8.
3. Bergman JS, Woods GL. Clinical evaluation of the Roche Amplicor
�814
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
Soini and Musser: Molecular Diagnosis of Mycobacteria
PCR Mycobacterium tuberculosis test for detection of M. tuberculosis in respiratory specimens J Clin Microbiol 1996;34:1083–5.
Stauffer F, Mutschlechner R, Hasenberger P, Stadlbauer S,
Schinko H. Detection of Mycobacterium tuberculosis complex in
clinical specimens by a commercial polymerase chain reaction kit.
Eur J Clin Microbiol Infect Dis 1995;14:1046 –51.
Tevere VJ, Hewitt PL, Dare A, Hocknell P, Keen A, Spadoro JP,
Young KKY. Detection of Mycobacterium tuberculosis by PCR
amplification with pan-Mycobacterium primers and hybridization to
an M. tuberculosis-specific probe. J Clin Microbiol 1996;34:918 –
23.
Chin DP, Yajko DM, Hadley WK, Sanders CA, Nassos PS, Mandej
JJ, Hopewell PC. Clinical utility of a commercial test based on the
polymerase chain reaction for detecting Mycobacterium tuberculosis in respiratory specimens. Am J Respir Crit Care Med 1995;
151:1872–7.
Al Zahrani K, Al Jahdali H, Poirier L, René P, Gennaro ML, Menzies
D. Accuracy and utility of commercially available amplification and
serologic tests for the diagnosis of minimal pulmonary tuberculosis. Am J Respir Crit Care Med 2000;162:1323–9.
Kwoh DY, Davis GR, Whitefield KM, Chapelle HL, DiMichele LJ,
Gingeras TR. Transcription-based amplification system and detection of amplified human immunodeficiency virus type 1 with a
bead-based sandwich hybridization format. Proc Natl Acad Sci
U S A 1989;86:1173–7.
Bergmann JS, Yuoh G, Fish G, Woods GL. Clinical evaluation of the
enhanced Gen-Probe amplified Mycobacterium tuberculosis direct
test for rapid diagnosis of tuberculosis in prison inmates. J Clin
Microbiol 1999;37:1419 –25.
Gamboa F, Fernandez G, Padilla E, Manterola JM, Lonca J,
Cardona PJ, et al. Comparative evaluation of initial and new
versions of the Gen-Probe amplified Mycobacterium tuberculosis
direct test for direct detection of Mycobacterium tuberculosis in
respiratory and nonrespiratory specimens. J Clin Microbiol 1998;
36:684 –9.
Smith MB, Bergmann JS, Onoroto M, Mathews G, Woods GL.
Evaluation of the enhanced amplified Mycobacterium tuberculosis
direct test for direct detection of Mycobacterium tuberculosis
complex in respiratory specimens. Arch Pathol Lab Med 1999;
123:1101–3.
Catanzaro A, Perry S, Clarridge JE, Dunbar S, Goodnight-White S,
LoBue PA, et al. The role of clinical suspicion in evaluating a new
diagnostic test for active tuberculosis. Results of a multicenter
prospective trial. JAMA 2000;283:639 – 45.
Scarparo C, Piccoli P, Rigon A, Ruggiero G, Scagnelli M, Piersimoni
C. Comparison of enhanced Mycobacterium tuberculosis amplified direct test with Cobas Amplicor Mycobacterium tuberculosis
assay for direct detection of Mycobacterium tuberculosis complex
in respiratory and extrapulmonary specimens. J Clin Microbiol
2000;38:1559 – 62.
Woods GL. Molecular techniques in mycobacterial detection. Arch
Pathol Lab Med 2001;125:122– 6.
Centers for Disease Control and Prevention. Update: nucleic acid
amplification tests for tuberculosis. MMWR Morb Mortal Wkly Rep
2000;49:593– 4.
Pfyffer GE, Kissling P, Jahn EMI, Welscher H-M, Salfinger M,
Weber R. Diagnostic performance of amplified Mycobacterium
tuberculosis direct test with cerebrospinal fluid, other nonrespiratory and respiratory specimens. J Clin Microbiol 1996;34:834 –
41.
Shah S, Miller A, Mastellone A, Kim K, Colaninno P, Hochstein L,
D’Amato R. Rapid diagnosis of tuberculosis in various biopsy and
body fluid specimens by the Amplicor Mycobacterium tuberculosis
polymerase chain reaction test. Chest 1998;113:1190 – 4.
Smith MB, Bergmann JS, Woods GL. Detection of Mycobacterium
tuberculosis in BACTEC 12B broth cultures by the Roche Amplicor
PCR assay. J Clin Microbiol 1997;35:900 –2.
Katila M-L, Katila P, Erkinjuntti-Pekkanen R. Accelerated detection
and identification of mycobacteria with MGIT 960 and Cobas
Amplicor systems. J Clin Microbiol 2000;38:960 – 4.
Goto M, Oka S, Okuzumi K, Kimura S, Shimada K. Evaluation of
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
acridinium-ester-labeled DNA probes for identification of Mycobacterium tuberculosis and Mycobacterium avium-Mycobacterium intracellulare complex in culture. J Clin Microbiol 1991;29:2473– 6.
Lebrun L, Espinasse F, Poveda JD, Vincent-Levy-Frebault V. Evaluation of nonradioactive DNA probes for identification of mycobacteria. J Clin Microbiol 1992;30:2476 – 8.
Evans KD, Nakasone AS, Sutherland PA, De La Maza LM, Peterson EM. Identification of Mycobacterium tuberculosis and Mycobacterium avium-intracellulare directly from primary BACTEC cultures by using acridinium-ester-labeled DNA probes. J Clin
Microbiol 1992;30:2427–31.
Reisner BS, Gatson AM, Woods GL. Use of Gen-Probe AccuProbes
to identify Mycobacterium avium complex, Mycobacterium tuberculosis complex, Mycobacterium kansasii, and Mycobacterium
gordonae directly from BACTEC TB broth cultures. J Clin Microbiol
1994;32:2995– 8.
Springer B, Kirschner P, Rost-Mayer G, Schröder K-H, Kroppenstedt RM, Böttger EC. Mycobacterium interjectum, a new species
isolated from a patient with chronic lymphadenitis. J Clin Microbiol
1993;31:3083–9.
Springer B, Tortoli E, Richter I, Grunewald R, Rusch-Gerdes S,
Uschmann K, et al. Mycobacterium conspicuum sp. nov, a new
species isolated from patients with disseminated infections.
J Clin Microbiol 1995;33:2805–11.
Rogall T, Flohr T, Böttger EC. Differentiation of Mycobacterium
species by direct sequencing of amplified DNA. J Gen Microbiol
1990;136:1915–20.
Kirschner P, Springer B, Vogel U, Meier A, Wrede A, Kiekenbeck M,
et al. Genotypic identification of mycobacteria by nucleic acid
sequence determination: report of a 2-year experience in a clinical
laboratory. J Clin Microbiol 1993;31:2882–9.
Soini H, Böttger EC, Viljanen MK. Identification of mycobacteria by
PCR-based sequence determination of the 32-kilodalton protein
gene. J Clin Microbiol 1994;32:2944 –7.
Kapur V, Li L-L, Hamrick MR, Plikaytis BB, Shinnick TM, Telenti A,
et al. Rapid Mycobacterium species assignment and unambiguous identification of mutations associated with antimicrobial
resistance in Mycobacterium tuberculosis by automated DNA
sequencing. Arch Pathol Lab Med 1995;119:131– 8.
Roth A, Fischer M, Hamid ME, Michalke S, Ludwig W, Mauch H.
Differentiation of phylogenetically related slowly growing mycobacteria based on 16S–23S rRNA gene internal transcribed spacer
sequences. J Clin Microbiol 1998;36:139 – 47.
Pai S, Esen N, Pan X, Musser JM. Routine rapid Mycobacterium
species assignment based on species-specific allelic variation in
the 65-kilodalton heat shock protein gene (hsp65). Arch Pathol
Lab Med 1997;121:859 – 64.
Gingeras TR, Ghandour G, Wang E, Berno A, Small PM, Drobniewski F, et al. Simultaneous genotyping and species identification using hybridization pattern recognition analysis of generic
Mycobacterium DNA arrays. Genome Res 1998;8:435– 48.
Troesch A, Nguyen H, Miyada CG, Desvarenne S, Gingeras TR,
Kaplan PM, et al. Mycobacterium species identification and
rifampin resistance testing with high-density DNA probe arrays.
J Clin Microbiol 1999;37:49 –55.
Ramaswamy S, Musser JM. Molecular genetic basis of antimicrobial agent resistance in Mycobacterium tuberculosis: 1998 update. Tuber Lung Dis 1998;79:3–29.
De Beenhouwer H, Lhiang Z, Jannes G, Mijs W, Machtelinckx L,
Rossau R, et al. Rapid detection of rifampin resistance in sputum
and biopsy specimens from tuberculosis patients by PCR and line
probe assay. Tuber Lung Dis 1995;76:425–30.
Hirano K, Abe C, Takahashi M. Mutations in the rpoB gene of
rifampin-resistant Mycobacterium tuberculosis strains isolated
mostly in Asian countries and their rapid detection by line probe
assay. J Clin Microbiol 1999;37:2663– 6.
Traore H, Fissette K, Bastian I, Devleeschouwer M, Portaels F.
Detection of rifampin resistance in Mycobacterium tuberculosis
isolates from diverse countries by commercial line probe assay as
an initial indicator of multidrug resistance. Int J Tuberc Lung Dis
2000;4:481– 4.
�
 DE Clothe
DE Clothe