Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser.
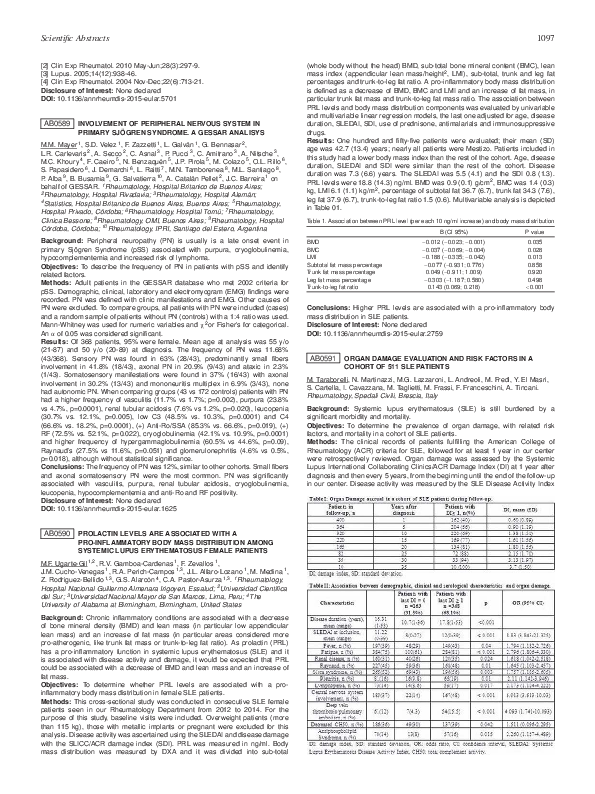
AB0591 Organ Damage Evaluation and Risk Factors in a Cohort of 511 Sle Patients
AB0591 Organ Damage Evaluation and Risk Factors in a Cohort of 511 Sle Patients
AB0591 Organ Damage Evaluation and Risk Factors in a Cohort of 511 Sle Patients
AB0591 Organ Damage Evaluation and Risk Factors in a Cohort of 511 Sle Patients
AB0591 Organ Damage Evaluation and Risk Factors in a Cohort of 511 Sle Patients
2015, Annals of the Rheumatic Diseases
Related Papers
Osteoarthritis and Cartilage
Hyaluronan derivative Hymovis® increases cartilage volume and type II collagen turnover in osteoarhritic knee: data from Mokha study2019 •
2019 update of the EULAR recommendations for the management of systemic lupus erythematosus Antonis Fanouriakis, 1 Myrto Kostopoulou, Alessia Alunno, 3 Martin Aringer, Ingeborg Bajema, John N Boletis, Ricard Cervera, Andrea Doria, 8 Caroline Gordon, Marcello Govoni, Frédéric Houssiau, David Jayne, Marios Kouloumas, Annegret Kuhn, Janni L Larsen, Kirsten Lerstrøm, Gabriella Moroni, Marta Mosca, Matthias Schneider, Josef S Smolen, Elisabet Svenungsson, Vladimir Tesar, Angela Tincani, Anne Troldborg, Ronald van Vollenhoven, Jörg Wenzel, George Bertsias, Dimitrios T Boumpas
Annals of the Rheumatic Diseases
2019 update of the EULAR recommendations for the management of systemic lupus erythematosus2019 •
Our objective was to update the EULAR recommendations for the management of systemic lupus erythematosus (SLE), based on emerging new evidence. We performed a systematic literature review (01/2007–12/2017), followed by modified Delphi method, to form questions, elicit expert opinions and reach consensus. Treatment in SLE aims at remission or low disease activity and prevention of flares. Hydroxychloroquine is recommended in all patients with lupus, at a dose not exceeding 5 mg/kg real body weight. During chronic maintenance treatment, glucocorticoids (GC) should be minimised to less than 7.5 mg/day (prednisone equivalent) and, when possible, withdrawn. Appropriate initiation of immunomodulatory agents (methotrexate, azathioprine, mycophenolate) can expedite the tapering/discontinuation of GC. In persistently active or flaring extrarenal disease, add-on belimumab should be considered; rituximab (RTX) may be considered in organ-threatening, refractory disease. Updated specific recomme...
Aim: To measure disease activity and damage in patients with TA using ITAS (Indian Takayasu Activity Score), ITASESR, ITASCRP and TADS (Takayasu Arter- itis Damage Index). Introduction/Background: The IRAVAS have developed instruments ITAS, ITASESR and ITASCRP to measure disease activity and TADS to capture damage in TA. Methods/Materials/Analytical Procedures: Information was retrieved from hospital records of patients who fulfilled ACR criteria for TA at initial/follow up visit if available with TADS at followup visit only. ITASESR/CRP was calculated by add- ing scores to ITAS if Westergren’s ESR/quantitative CRP were 1 ( 18/6), 2 (19- 29/6- 10), 3 (30- 45/11- 20), 4 (!46/>21) (mm/hr/mg/L). Results: 48 patients (39 females) with mean age 28.19 (`10.12) years and mean duration of illness prior to presentation 2.33 (`2.69) (n 1⁄4 30) years. Predominant symptoms at presentation were hypertension (19; 39.5%), upper limb claudication (12; 25%), dyspnea on exertion (10; 20.8%) and fe...
Annals of the rheumatic diseases
Long-term follow-up of the MAINTAIN Nephritis Trial, comparing azathioprine and mycophenolate mofetil as maintenance therapy of lupus nephritis2015 •
To report the 10-year follow-up of the MAINTAIN Nephritis Trial comparing azathioprine (AZA) and mycophenolate mofetil (MMF) as maintenance therapy of proliferative lupus nephritis, and to test different definitions of early response as predictors of long-term renal outcome. In 2014, data on survival, kidney function, 24 h proteinuria, renal flares and other outcomes were collected for the 105 patients randomised between 2002 and 2006, except in 13 lost to follow-up. Death (2 and 3 in the AZA and MMF groups, respectively) and end-stage renal disease (1 and 3, respectively) were rare events. Time to renal flare (22 and 19 flares in AZA and MMF groups, respectively) did not differ between AZA and MMF patients. Patients with good long-term renal outcome had a much more stringent early decrease of 24 h proteinuria compared with patients with poor outcome. The positive predictive value of a 24 h proteinuria <0.5 g/day at 3 months, 6 months and 12 months for a good long-term renal outc...
2020 •
Objectives It is unknown if hydroxychloroquine blood level dynamics impact flare rates in lupus nephritis patients. We prospectively evaluated hydroxychloroquine levels to determine which blood-based patterns are more associated with disease activity. Methods In total, 82 lupus nephritis patients under a prescribed hydroxychloroquine dose of 4–5.5 mg/kg actual body weight (maximum 400 mg/day) for ≥3 months were evaluated at baseline and 7 months. Hydroxychloroquine blood levels were determined by liquid chromatography-tandem mass spectrometry. Flare was defined as increase ≥3 in the Systemic Lupus Erythematosus Disease Activity Index 2000 score and/or a change or increase in therapy. Results Overall, 9/82(11%) patients had flares during follow-up and had lower baseline hydroxychloroquine blood levels than those without flares (220.4 (53.5–1471.1) vs. 1006.3 (53.5–2137.8) ng/ml, p = 0.013). The hydroxychloroquine blood level cut-off that best predicted flares was 613.5 ng/ml (odds ra...
Annals of the Rheumatic Diseases
Identification of Affimers that bind to the IL-7Ra and inhibits the IL-7 signalling cascade2019 •
Introduction. IL-7R is a heterodimer constituted by the IL-7R alpha (a) chain (CD127) and the common gamma (g) chain (CD132). IL-7 binding to IL-7R expressed on CD4+ T cells induces a survival signal. The IL-7/IL-7R signalling axis has been validated as a therapeutic target for treatment of both T-cell driven autoimmune diseases (AIDs)1 and T Acute Lymphoblastic Leukaemia (T-ALL).2 Affimers are small and stable artificial proteins which bind with nanomolar affinities to human proteins and can block protein-protein interactions.3 They are becoming widespread owing to their stability, ease of production and versatility. Objectives. Identify Affimers that recognise the IL-7Ra and inhibits the IL-7 signalling cascade. This may result in an attractive approach for the treatment of both T-cell driven autoimmune diseases and T-ALL. Methods. The type-II Affimer library (1010) was interrogated by Phage display using fully glycosylated human IL-7Ra ectodomain (ECD). PhageELISA and DNA sequencing were used to either obtain or elucidate the unique binders (Affimers), respectively. Affimers were produced as His-Tagged proteins (~13 kDa) in E. coli and purified using IMAC. Affimer binding to IL-7Ra was confirmed by pull-down assays (soluble) and Flow cytometry (membrane). An IL-7 reporter assay using HEK-IL7R (HEK293 cells stably transfected with the IL-7R) was developed and the biological effect of the Affimers was elucidated. Results. We have screened an Affimer library using human ECD-IL7Ra and after three consecutive panning rounds, 20 Affimers were raised as shown by PhageELISA and DNA sequencing. From these, 17 were able to pull-down the soluble ECD-IL7Ra and 7 stained specifically HEK-IL7R cells (by flow cytometry using anti-His Tag Abs). Finally, we have identified 3 Affimers (1, 42 and 96) that showed inhibition of the IL-7 signalling cascade on HEK-IL7R cells. Conclusions. Our work demonstrates the possibility of screening an Affimer library for a cytokine-receptor target, and selecting specific binders, some of which showed the desired antagonist activity of the cytokine signalling cascade. IL-7 itself is a validated target, so this work offers an alternative to antibody-mediated protein interference. With further biological validation including animal models, it may even offer a novel therapeutic tool for AIDs and T-ALL.
Annals of the Rheumatic Diseases
Phase II randomised trial of type I interferon inhibitor anifrolumab in patients with active lupus nephritis2022 •
ObjectiveTo assess the efficacy and safety of the type I interferon receptor antibody, anifrolumab, in patients with active, biopsy-proven, Class III/IV lupus nephritis.MethodsThis phase II double-blinded study randomised 147 patients (1:1:1) to receive monthly intravenous anifrolumab basic regimen (BR, 300 mg), intensified regimen (IR, 900 mg ×3, 300 mg thereafter) or placebo, alongside standard therapy (oral glucocorticoids, mycophenolate mofetil). The primary endpoint was change in baseline 24-hour urine protein–creatinine ratio (UPCR) at week (W) 52 for combined anifrolumab versus placebo groups. The secondary endpoint was complete renal response (CRR) at W52. Exploratory endpoints included more stringent CRR definitions and sustained glucocorticoid reductions (≤7.5 mg/day, W24–52). Safety was analysed descriptively.ResultsPatients received anifrolumab BR (n=45), IR (n=51), or placebo (n=49). At W52, 24-hour UPCR improved by 69% and 70% for combined anifrolumab and placebo group...
Frontiers in Medicine
Trabecular Bone Score and Bone Quality in Systemic Lupus Erythematosus Patients2020 •
RELATED PAPERS
Saturday, 16 JUNE 2018
SAT0451 Disease course patterns in systemic lupus erythematosusPaediatric rheumatology
AB1121 Evaluation of cases diagnosed with crmo; single centre experience2018 •
Integrative Medicine Insights
Vitamin D Deficiency in Egyptian Systemic Lupus Erythematosus Patients: How Prevalent and Does It Impact Disease Activity?2016 •
2009 •
 Franco Franceschini
Franco Franceschini