Thorax Online First, published on April 7, 2011 as 10.1136/thx.2011.161208
PostScript
RESEARCH LETTER
Background Modern gas analysis techniques permit real time and on-line quantification of
multiple volatile trace gases within a single exhalation. However, the influence of various respiratory manoeuvres affecting exhalation flow and the kinetics of metabolite release to the gasphase remain largely unknown.
Methods We examined variation in the concentrations of selected trace gases over a range of
expiratory flows (50; 100; 250 ml/s) and after 30 second periods of breathold and paced hyperventilation. On-line measurement of breath samples from healthy volunteers (n¼10) was
performed by proton transfer mass spectrometry.
Results Exhaled acetone increased with higher expiratory flow rate (805, 838, 898 ppb, p¼0.02).
Levels of methanol (206 vs 179 ppb, p<0.01), acetaldehyde (26 vs 22 ppb, p<0.01), ethanol (410
vs 208 ppb, p¼0.01) and dimethyl sulphide (113 vs 103 ncps, p<0.01) fell significantly following
30s hyperventilation. After 30 second breathold levels of methanol (206 vs 217 ppb, p¼0.02),
acetone (805 vs 869 ppb, p<0.01), isoprene (348 vs 390 ppb, p¼0.02) and dimethyl sulphide (113
vs 136 ncps, p¼0.02) increased significantly. Variation in respiratory parameters did not significantly alters the level of acetonitrile, propanol and butyric acid within the breath of healthy subjects.
Conclusions These findings demonstrate that respiratory manoeuvres significantly influence the
measured concentration of a number of exhaled VOCs that are of potential importance within the
clinical setting. Our results support the adoption of standardised practices for breath gas analysis
by on-line and real time mass spectrometry methods.
Analysis of volatile trace gases within exhaled
breath, for the purpose of non-invasive
disease detection and monitoring, is a rapidly
emerging field of research.1 2 Recent technological developments such as proton transfer
reaction‑mass spectrometry (PTR-MS) have
allowed on-line and real-time detection of
multiple trace gases in breath, leading to
novel discoveries in cancer, infectious disease
and metabolism.2 3
One of the greatest lessons on clinical
applicability of breath analysis has been the
recognition that multiple physiological variables can influence the quantification of
exhaled nitric oxide (NO), necessitating
international consensus guidelines for its
standardised measurement.4 There remains
however limited experimental evidence
defining the impact of confounding factors
which may influence the quantification of
other exhaled volatile trace gases.5 Herein we
present the finding of a study investigating
the influence of respiratory variables on the
on-line detection and quantification of
a judiciously selected and potentially clinically relevant panel of expiratory trace gases.
We examined the variation in the
concentrations of selected trace gases
(methanol, acetaldehyde, ethanol, acetone,
isoprene, acetonitrile, propanol, dimethyl
sulphide and butyric acid) over a range of
expiratory flows (50, 100, 250 ml/s) and after
the 30-s periods of breath hold and paced
hyperventilation. These volatiles were
compared to exhaled NO and carbon dioxide.
On-line measurement of breath samples
from healthy volunteers (n¼10) was
performed by combining PTR-MS (Ionimed
Analytik GmbH, Innsbruck, Austria) with
the LR2500 multiple-gas analyser (Logan
Research Ltd, Rochester, UK). Quantification
of trace gases by PTR-MS was achieved by
calibration experiments using accurately
known gas standards and a purpose built gas
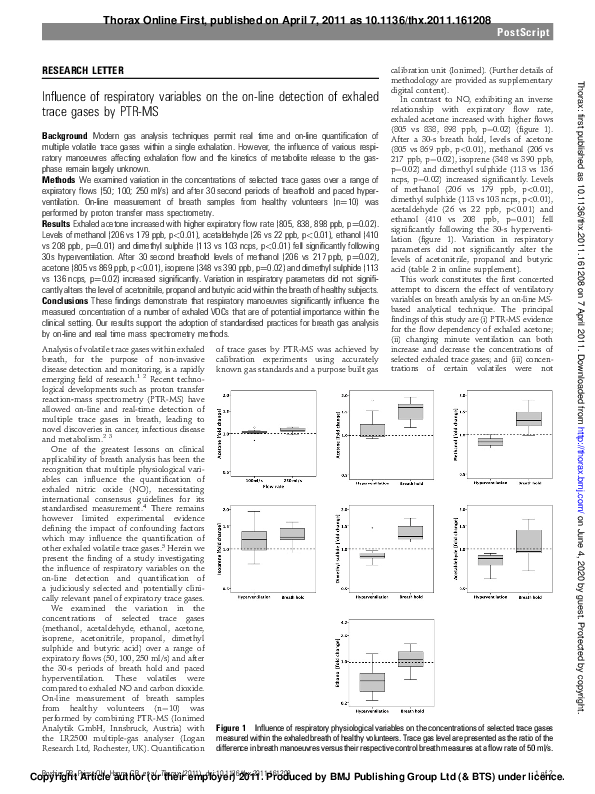
Figure 1 Influence of respiratory physiological variables on the concentrations of selected trace gases
measured within the exhaled breath of healthy volunteers. Trace gas level are presented as the ratio of the
difference in breath manoeuvres versus their respective control breath measures at a flow rate of 50 ml/s.
Boshier PR, Priest
OH, Hanna
GB, et(or
al. Thorax
doi:10.1136/thx.2011.161208
1 of 2
Copyright
Article
author
their(2011).
employer)
2011. Produced by BMJ Publishing Group Ltd (& BTS) under licence.
Thorax: first published as 10.1136/thx.2011.161208 on 7 April 2011. Downloaded from http://thorax.bmj.com/ on June 4, 2020 by guest. Protected by copyright.
Influence of respiratory variables on the on-line detection of exhaled
trace gases by PTR-MS
calibration unit (Ionimed). (Further details of
methodology are provided as supplementary
digital content).
In contrast to NO, exhibiting an inverse
relationship with expiratory flow rate,
exhaled acetone increased with higher flows
(805 vs 838, 898 ppb, p¼0.02) (figure 1).
After a 30-s breath hold, levels of acetone
(805 vs 869 ppb, p<0.01), methanol (206 vs
217 ppb, p¼0.02), isoprene (348 vs 390 ppb,
p¼0.02) and dimethyl sulphide (113 vs 136
ncps, p¼0.02) increased significantly. Levels
of methanol (206 vs 179 ppb, p<0.01),
dimethyl sulphide (113 vs 103 ncps, p<0.01),
acetaldehyde (26 vs 22 ppb, p<0.01) and
ethanol (410 vs 208 ppb, p¼0.01) fell
significantly following the 30-s hyperventilation (figure 1). Variation in respiratory
parameters did not significantly alter the
levels of acetonitrile, propanol and butyric
acid (table 2 in online supplement).
This work constitutes the first concerted
attempt to discern the effect of ventilatory
variables on breath analysis by an on-line MSbased analytical technique. The principal
findings of this study are (i) PTR-MS evidence
for the flow dependency of exhaled acetone;
(ii) changing minute ventilation can both
increase and decrease the concentrations of
selected exhaled trace gases; and (iii) concentrations of certain volatiles were not
�PostScript
Piers R Boshier,1 Oliver H Priest,1
George B Hanna,1 Nandor Marczin2,3
Medicine and Intensive Care, Imperial College London,
Chelsea and Westminster Hospital, London, UK;
3
Department of Anaesthetics, Harefield Hospital, The
Royal Brompton and Harefield NHS Foundation Trust,
Harefield, Middlesex, UK
Correspondence to Dr Nandor Marczin, Department of
Surgery and Cancer, Section of Anaesthetics, Pain
Medicine and Intensive Care, Imperial College London,
Chelsea and Westminster Hospital, London SW10 9NH,
UK; n.marczin@imperial.ac.uk
2 of 2
1.
2.
3.
< An additional table is published online only. To view this
file please visit the journal online (http://thorax.bmj.com).
4.
Competing interests None.
Ethics approval This study was conducted with the
approval of the Riverside Research Ethics Committee
(project reference number: 08/H0706/134).
Provenance and peer review Not commissioned;
externally peer reviewed.
1
Department of Surgery and Cancer, Imperial College
London, St Mary’s Hospital, London, UK; 2Department of
Surgery and Cancer, Section of Anaesthetics, Pain
REFERENCES
Accepted 9 February 2011
5.
Kharitonov SA, Barnes PJ. Exhaled biomarkers. Chest
2006;130:1541e6.
Amann A, Smith D, eds. Breath Analysis for Clinical
Diagnosis and Therapeutic Monitoring. Singapore:
World Scientific, 2005.
Lindinger W, Hansel A, Jordan A. On-line monitoring
of volatile organic compounds at pptv levels by means
of proton-transfer-reaction mass spectrometry
(PTR-MS)-medical applications, food control and
environmental research. Int J Mass Spectrom
1998;173:191e241.
American Thoracic Society; European
Respiratory Society. ATS/ERS recommendations for
standardized procedures for the online and offline
measurement of exhaled lower respiratory nitric oxide
and nasal nitric oxide, 2005. Am J Respir Crit Care
Med 2005;171:912e30.
Larstad MA, Toren K, Bake B, et al. Determination of
ethane, pentane and isoprene in exhaled air: effects of
breath-holding, flow rate and purified air. Acta Physiol
(Oxf) 2007;189:87e98.
Thorax 2011;-:1e2. doi:10.1136/thx.2011.161208
Boshier PR, Priest OH, Hanna GB, et al. Thorax (2011). doi:10.1136/thx.2011.161208
Thorax: first published as 10.1136/thx.2011.161208 on 7 April 2011. Downloaded from http://thorax.bmj.com/ on June 4, 2020 by guest. Protected by copyright.
significantly altered by respiratory manoeuvres in healthy volunteers.
These preliminary observations may have
important implications regarding the standardisation requirement for measuring and
reporting the concentrations of exhaled trace
gases in the future. Further larger studies
both in healthy and diseased subjects are
necessary to expand on these observations
and to provide mechanistic insights into
exchange kinetics of affected volatiles. Such
studies may help to further define the exact
role of on-line MS technologies in non-invasive diagnosis and monitoring pulmonary
and systemic diseases.
�
 Oliver Priest
Oliver Priest