Prostate Cancer
Medically reviewed by Drugs.com. Last updated on Oct 6, 2024.
What do I need to know about prostate cancer?
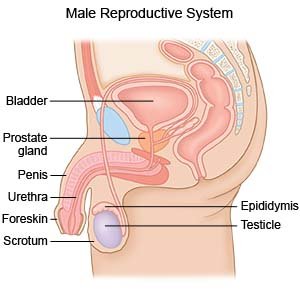
The prostate is the male sex gland that helps make semen. It wraps around the urethra. The urethra is the tube that carries urine from the bladder to the end of the penis. In most cases, prostate cancer is slow growing. Prostate cancer increases your risk for deep vein thrombosis and pulmonary embolism.
 |
What increases my risk for prostate cancer?
- Age older than 50 years
- Father, son, or brother with prostate cancer
- Changes in genes
What are the signs and symptoms of prostate cancer?
You may have no symptoms during the early stages. In the later stages, you may have any of the following:
- Trouble starting or stopping the flow of urine
- Feeling the need to urinate often, especially at night
- Pain or a burning feeling when you urinate or ejaculate semen
- Trouble having an erection
- Blood in your urine or semen
- Not being able to urinate at all
- Pain or stiffness in your lower back, hips, or upper thighs
How is prostate cancer diagnosed?
Your healthcare provider will examine you and ask about your symptoms. Tell your provider if you have a family history of prostate cancer. You may also need any of the following:
- Digital rectal examination (DRE) is a test to check the size and shape of your prostate. Your healthcare provider will insert a gloved finger into your rectum to feel if your prostate is large, firm, or has lumps.
- Prostate-specific antigen (PSA) is a blood test to check PSA levels. These levels may be increased if you have prostate cancer.
- A biopsy is used to take a sample of your prostate gland to be tested for cancer. The sample may also help healthcare providers determine the stage of your cancer.
- A bone scan is used to take x-ray pictures to see if the cancer has spread to your bones.
- A CT scan or MRI may be used to take pictures of your prostate, abdomen, and pelvis. The pictures may show if your cancer has spread. You may be given contrast liquid to help healthcare providers see the pictures better. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if you have any metal in or on your body.
What do I need to know about prostate cancer staging?
- After cancer is found, your healthcare provider will assign a number called a Gleason score. The number can help you understand how quickly the cancer is likely to grow, and if it may spread:
- A number of 6 or lower means the cancer is likely to grow more slowly.
- A score of 7 means it is likely to grow faster, but it may not spread to other areas.
- A score of 8 to 10 means it is likely to grow more quickly and also spread.
- Your healthcare provider will also assign a T stage to the tumor. This number shows the growth of the tumor and if it is likely to spread to other areas.
How is prostate cancer treated?
If you have early stage cancer, your healthcare provider may recommend that you have frequent tests and regular follow-up visits to watch for changes. The following treatments may be used alone or together depending on the type and stage of prostate cancer you have:
- Hormone therapy is medicine used to decrease testosterone (male hormone) levels.
- Chemotherapy is medicine used to shrink or kill cancer cells. It is usually given IV.
- Radiation therapy is used to kill cancer cells with high-energy x-ray beams. You may receive radiation therapy from outside your body or from small beads or rods placed inside your prostate.
- Surgery may be needed, depending on the stage of the cancer. Part or all of your prostate may be removed. You may also need to have some lymph nodes taken out. This may help keep the cancer from spreading to other parts of your body. Your healthcare provider may recommend a combination of radiation therapy and surgery.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
What can I do to manage prostate cancer?
- Do not smoke. Nicotine can damage blood vessels and make it more difficult to manage prostate cancer. Smoking also increases your risk for new or returning cancer and delays healing after treatment. Do not use e-cigarettes or smokeless tobacco in place of cigarettes or to help you quit. They still contain nicotine. Ask your healthcare provider for information if you currently smoke and need help quitting.
- Limit or do not drink alcohol as directed. A drink is 12 ounces of beer, 1½ ounces of liquor, or 5 ounces of wine.
- Eat a variety of healthy foods. Healthy foods include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Your healthcare provider may also recommend changes to the amounts of calcium and vitamin D you have each day.

- Manage your weight. Obesity may increase your risk for problems from prostate cancer. Limit or do not have high-calorie foods or drinks.
- Exercise as directed. Exercise may help you recover after treatment and may help prevent prostate cancer from returning. Exercise can also help you manage your weight. Try to get at least 30 minutes of exercise 5 days a week, such as walking.

- Ask about sexual activity. Ask your healthcare provider when it is safe for you to start having sex after your treatment. Medicines may be given if you have trouble getting or maintaining an erection.
- Manage incontinence. You may have incontinence (trouble controlling when you urinate) after treatment. Ask your healthcare provider for information on managing urinary incontinence. You may be able to gain control over your urination with techniques or medicines.
- Drink liquids as directed. Ask how much liquid to drink each day and which liquids are best for you. Drink extra liquids to prevent dehydration. You will also need to replace fluid if you are vomiting or have diarrhea from cancer treatments.
Call your local emergency number (911 in the US) if:
- You suddenly feel lightheaded and short of breath.
- You have chest pain when you take a deep breath or cough.
- You cough up blood.
When should I seek immediate care?
- Your leg feels warm, tender, and painful. It may look swollen and red.
- You are not able to urinate or urinate very little and you have had enough liquids.
- You have bladder pain.
- You have lower back pain, pain down your legs, or burning or tingling in your feet.
- You have weakness in your legs or trouble walking.
When should I call my doctor?
- You have a fever.
- You feel you cannot cope with your illness.
- You have pain that does not decrease or go away after you take your medicine.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Prostate Cancer
Treatment options
Symptoms and treatments
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
