Nursing Care Plan
Nursing Care Plan
Uploaded by
aln005Copyright:
Available Formats
Nursing Care Plan
Nursing Care Plan
Uploaded by
aln005Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Nursing Care Plan
Nursing Care Plan
Uploaded by
aln005Copyright:
Available Formats
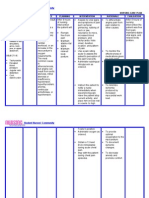
Concept Care Map
Student Name: Tony Neal #2
FHP: Activity-Exercise
Date: 12 FEB 13
FHP: Health-Perception
# #3
#1
FHP: Activity-Exercise
Key Problems/Nursing Diagnosis: Ineffective Breathing Pattern r/t physiological process of fluid infiltration of the pleural space AEB Supporting Data: Alterations in depth of breathing, dyspnea, diminished lung sounds in the left lung fields, faint crackles on left side, body position, and chronic emphysema, chronic pneumothorax, cough, and decreased oxygen saturation
Key Problems/Nursing Diagnosis: Risk for injury r/t physiological process (change in field of vision) d/t ischemic event Supporting Data: Loss of peripheral vision in right eye, unsteady gait, age, fatigue and partial paralysis in LRE
Key Problems/Nursing Diagnosis: Impaired gas exchange r/t physiological process of reduction in lung elasticity and infection AEB Supporting Data: Change in breathing rate, rhythm and depth; headache upon waking, fatigue, malaise, abnormal arterial pH. chronic pneumothorax, iron deficient anemia, and COPD
#4
FHP: NutritionalMetabolic
Reason for needing health care: Loss of peripheral vision in right eye Medical Diagnosis/Surgical Procedure: Ischemic event, R/O TIA, Hypothyroidism, GERD, HLD, Anemia, Chronic right pleural effusion with trap lung, CHF, COPD Key Assessments: Lung sounds, V/S, ABGs, LOC, Pain, I&O, Tele, EKG, Labs (Hct, Hgb, Plt, electrolytes), O2 sat, edema, productive cough, glucose, BP, respirations, CTA of carotid arteries #6
FHP: Self-Perception
Key Problems/Nursing Diagnosis: Fluid volume excess r/t ineffective compensatory mechanism (physiological process) AEB Supporting Data: Adventitious breath sounds, blood pressure changes, pulmonary artery pressure changes; pulmonary congestion; restlessness; specific gravity changes; BUN/creatinine
Key Problems/Nursing Diagnosis: Anxiety (moderate) r/t hospitalization AEB Supporting Data: Inability to sleep, restlessness, disease process, knowledge deficit, changes in field of vision, acute pain
#5
FHP: Activity-Exercise
FHP: NutritionalMetabolic
#7
Key Problems/Nursing Diagnosis: Decreased Cardiac output r/t altered electrical conduction secondary to dysrhythmia AEB Supporting Data: Arrhythmia (chronic A-FIB); bradycardia; electrocardiographic changes; palpitations; tachycardia; edema, fatigue on exertion.
Key Problems/Nursing Diagnosis: Disturbed sensory perception (visual) r/t a stroke (physiological process) and loss of peripheral vision in the right eye AEB Supporting Data: Partial loss of peripheral vision in right eye as assessed for neurological function, verbalization of only being able to see in a straight line.
Explanation of Relationships between Nursing Diagnoses
While anxiety is not the number one diagnosis it is related to almost everything. As the clients condition improves, his anxiety should also improve. However, until CBs breathing is stabilized and he is educated on his potential TIA/loss of peripheral vision his anxiety will remain at a moderate level. However, the clients moderate anxiety level is related to his readiness for enhanced learning and demonstrates an appropriate form of coping. The pathophysiological implications of stress/anxiety indicate a response that involves the nervous system, the endocrine system and the immune system. While all of these work to maintain homeostasis of the body; an influx in physical stress related to hospitalization secondary to a physical illness may upset this delicate balance. Thus the inevitable impact that stress/anxiety will have on all of the other diagnoses. An ineffective breathing pattern can be directly associated with a client who has impaired gas exchange. As the arterial pH in the client changes so will the clients breathing pattern. Respiration rate, rhythm and depth are mechanisms to compensate for the change; increased respirations to blow-off more CO2 or possibly decreased breathing (bradypnea) in an effort to increase CO2. The kidneys will also play a role in regulating an imbalance in arterial pH through filtering the blood and excreting unneeded acids. Decreased cardiac output can alter the amount of oxygenated blood that travels throughout the systemic circulatory system. One of the organs this blood flow may be reduced to is the kidneys. If there is a reduction in the blood flow to the kidneys, then there may be a reduction in urinary output thus causing additional fluid and waste that is not being excreted properly. Furthermore, the clients chronic atrial fibrillation affects preloading of the ventricle prior to ventricular contraction thus causing the decreased cardiac output and ultimately improper cardiac perfusion.
Problem # _1_ & Nursing Diagnosis: Impaired gas exchange r/t physiological process of reduction in lung elasticity AEB change in breathing rate, rhythm and depth; headache upon waking, fatigue, malaise, abnormal arterial pH. chronic pneumothorax, and iron deficient anemia. General Goal: Maintain adequate oxygen saturation Behavioral Outcome Objective(s): The Client will: Demonstrate improved ventilation and adequate oxygenation with the use of pulse oxemetry and arterial blood gas levels with in normal limits that are appropriate for age prior to discharge Maintain a clear lung field on the unaffected side within 48 hours of admission Verbalize understanding of a need for oxygen supplementation and other therapeutic interventions (turning, coughing, deep breathing, positioning, and the use if incentive spirometer) within 24 hours of admission Nursing interventions with rationales & references 1. Monitor respiratory rate, depth, ease of respiration and breath sounds q2h. Watch for use of accessory muscles and nasal flaring. Place client on continuous pulse oxemetry. When the respiratory rate exceeds 30 breaths/min, along with other physiological measures, a significant cardiovascular or respiratory alteration exists (Considine, 2005). 2. Monitor the client's behavior and mental status for the onset of restlessness, agitation, confusion, and (in the late stages) extreme lethargy q2h. Changes in behavior and mental status can be early Patient response to interventions
1. Client maintained an oxygen saturation of > 93% as indicated through pulse oxemetry. There were no indications of negative changes in respiratory rate, rhythm or depth.
2. Client did not exhibit any changes in level of consciousness, restlessness or agitation.
signs of impaired gas exchange (Simmons & Simmons, 2004).
3. If the client is acutely dyspneic, consider having the client lean forward over a bedside table, resting elbows on the table if tolerated. Educate client on the importance of eating smaller meals to conserve energy. Leaning forward can help decrease dyspnea, possibly because gastric pressure allows better contraction of the diaphragm (Langer et al, 2009). 4. Teach the client energy conservation techniques and the importance of alternating rest periods with activity. Conserving energy helps to promote accomplishing activities of daily living(Ackley, B., 2012). 5. Instruct the client/family regarding home oxygen therapy if ordered (e.g., delivery system, liter flow, safety precautions). Long-term oxygen therapy can improve survival, exercise ability, sleep and ability to think in hypoxemic clients. Client education improves compliance with prescribed use of oxygen (Celli & MacNee, 2004).
3. The client sat in this manner while eating. The intent was for him to increase his lung capacity and prevent fatigue. Client maintained enough energy to shower independently following his meal.
4. Client verbalized an understanding of the importance of breaking tasks down into smaller more manageable tasks and knowing when to ask for assistance.
5. The client maintained eye contact during the instruction of the operation of supplemental oxygen in the home. He was able to return instruction in his own words to demonstrate a working knowledge of the equipment. However, his wife was not present during the instruction. Included in the referral for home health was education regarding the use of supplemental oxygen.
Evaluation: (Summarize impressions of patients progress towards outcomes) Client presented receptive to all teaching and interventions. He did not demonstrate any signs or symptoms of respiratory problems/distress. There were no signs or symptoms of cyanosis and his lung field on the unaffected side was clear upon auscultation during all assessments. Client education was conducted in relation to oxygen use in the home; how and where to store the oxygen, when to replace the nasal cannula, how to read the pressure gauge, and how to set the amount of oxygen to be delivered. Based on the clients referral to home health, the home health nurse will conduct additional instruction related to this topic.
Care Plan Problem # _2_ & Nursing Diagnosis: Ineffective Breathing Pattern r/t physiological process of fluid infiltration of the pleural space AEB alterations in depth of breathing, dyspnea, diminished lung sounds in the left lung fields, faint crackles on left side, body position, and chronic emphysema, chronic pneumothorax, cough, and decreased oxygen saturation. General Goal: Establish a normal and effective breathing pattern Behavioral Outcome Objective(s): The Client will: Verbalize no episodes of dyspnea upon q2h assessment within 24 hours following admission Demonstrate a breathing pattern that supports blood gas results within the client's normal parameters (pH 7.35-7.45, CO2 22-26, HCO3 35-45, and O2 > 92%) prior to discharge Demonstrate ability to perform pursed-lip breathing and controlled breathing following initial teaching and during each shift. Nursing interventions with rationales & references 1. Attempt to determine if client's dyspnea is physiological or psychological in cause by evaluating respiratory function, noting increased and shallow respirations, reports of air hunger, cyanosis, or changes in breath sounds and vital signs q2h. A study found that when the cause was psychological (medically unexplained dyspnea), there was affective dyspnea, anxiety, and tingling in the extremities. Whereas when the dyspnea was physiological, there was associated wheezing, cough, Patient response to interventions
1. Unable to assess as the client did not exhibit any signs of dyspnea.
sputum, and palpitations (Han et al, 2008). 2. Note use of accessory muscles, nasal flaring, retractions, irritability, confusion, or lethargy upon q2h assessment. These symptoms signal increasing respiratory difficulty and increasing hypoxia (Ackley, B., 2012) 3. Support the client in using pursedlip and controlled breathing techniques. Pursed-lip breathing results in increased use of intercostal muscles, decreased respiratory rate, increased tidal volume, and improved oxygen saturation levels (Ackley, B., 2012) 4. Encourage ambulation as tolerated. Immobility is harmful to the elderly because it decreases ventilation and increases stasis of secretions (Doenges and Moorhouse, 2011). 5. Encourage elderly clients to sit upright or stand and to avoid lying down for prolonged periods during the day and when lying down, elevate the HOB to at least 30 degrees. Thoracic aging results in decreased lung expansion; an erect position fosters maximal lung expansion (Ackley, B., 2012). 2. Client did not present any signs or symptoms of the onset of respiratory distress; ie., nasal flaring, use of accessory muscles or changes in affect.
3. The client was instructed by the staff nurse of how to utilize pursed lip breathing in the event that breathing becomes difficult. Following the educational session, the client was able to both verbalize as well as return demonstration of pursed-lip breathing. 4. Client ambulated but did so with an unsteady gait. Recommended increasing ambulation distance by 5-10 meters per session per day.
5. Client was sitting in an upright position upon entering the room. Client used this position to visit with family.
Evaluation: (Summarize impressions of patients progress towards outcomes) Evaluation of this client was less than successful as he did not have any exacerbations of his respiratory system. However, this is a good client outcome as no complications are always a successful outcome for any client. Client was receptive to all teaching and demonstrated an understanding.
Problem # _3_ & Nursing Diagnosis: Risk for injury r/t physiological process (change in field of vision) d/t ischemic event General Goal: Prevent injury Behavioral Outcome Objective(s): The Client will: Begin to adapt to physical limitation (change in field of vision) by increasing steadiness while ambulating prior to discharge Remain without injury during current hospitalization Verbalize an understanding of individual factors that may lead to physical injury Nursing interventions with rationales & references 1. Note clients age, gender, developmental stage, decisionmaking ability, level of cognition/competence upon initial assessment. Affects clients ability to protect self and/or others, and influences choice of interventions and teaching (Doenges and Moorhouse, 2011). 2. Assess mood, coping abilities, personality styles (e.g., temperament, aggression, impulsive behavior, level of self-esteem) upon initial assessment and subsequent assessments. May result in carelessness or increased risktaking without consideration of consequence) (Doenges and Moorhouse, 2011). Patient response to interventions
1. No response needed from the client in regards to this demographic information.
2. Clients affect, mood and coping abilities were appropriate for the situation. The client maintains a very strong support system that includes his wife and a daughter who lives locally.
3. Educate the client on his current debility (right hemianopia of the right eye), potential cause and effects on ADLs. Awareness of disability will help to relieve anxiety (Ackley, B., 2012).
3. Client explained this was his reason for seeking medical care. He verbalized I was not sure of what was happening, but I thought it was a good idea to see a doctor. The clients PCM educated him on his condition as well as an optometrist. Unable to assess the full extent of the educational process.
4. The client is unsteady on feet, have two nursing staff members alongside when walking the client. Consider referral to physical therapy for gait training and strengthening. The client can walk independently, but the nurse can rapidly ensure safety if the knees buckle (Ackley, B., 2012). 5. Educate the client of potential hazards within the home. Home hazards present an increased risk of falls and injuries. A thorough home assessment should be conducted to identify physical hazards (Ackley, B., 2012).
4. Client was able to ambulate to the shower independently but guided by a family member and a CNA. Client tolerated this well and without injury.
5. Client states that he has his wife to take care of him at home. Client appeared disinterested in identifying any potential hazards within his home and verbalized a codependency on his wife.
Evaluation: (Summarize impressions of patients progress towards outcomes) Not fully able to evaluate the clients progress. However, the client seemed to have a happy affect throughout the period of care. This lends itself to the deduction that the client was accepting of his new disability.
Problem # _4_ & Nursing Diagnosis: Fluid volume excess r/t ineffective compensatory mechanism (physiological process) AEB adventitious breath sounds, blood pressure changes, pulmonary artery pressure changes; pulmonary congestion; restlessness; and specific gravity changes General Goal: Achieves fluid homestasis Behavioral Outcome Objective(s): The Client will: Remain free of edema throughout hospitalization Maintain body weight appropriate for the client without excessive weight gain (> 2lbs in 2 days or 5 lbs in 1 week) or excessive weight loss (> 2lbs in 2 days or 5 lbs in 1 week) during hospitalization Maintain urine output in relation to intake while hospitalized Maintain clear lung sounds, no evidence of dyspnea or orthopnea upon admission and while hospitalized. Nursing interventions with rationales & references 1. Monitor daily weight for sudden increases use same scale and type of clothing at same time each day, preferably before breakfast. Body weight changes reflect changes in body fluid volume (Ackley, B., 2012) 2. Monitor intake and output q shift; note trends reflecting decreasing urine output in relation to fluid intake. Accurately measuring intake and output is important for the client with fluid volume overload. A study found that visual estimation of intake of fluid was inaccurate; instead, volumes should be Patient response to interventions
1. Client was weighed prior to conducting his CTA at 0800 and weighed 0.8 pounds less than the day prior.
2. A very well experienced nursing aid was responsible for the monitoring of the clients I&O and the staff nurse conducted spot checks. The client was with in normal limits for the amount of fluids he was taking in. Is output was approximately 100mL more than his intake with a weight loss of
measured (McConnell et al, 2007).
0.3lbs.
3. Listen to lung sounds for crackles, monitor respirations for effort, and determine the presence and severity of orthopnea q2h. Pulmonary edema results from excessive shifting of fluid from the vascular space into the pulmonary interstitial space and alveoli, resulting in dyspnea and orthopnea (McConnell et al, 2007). 4. Monitor the client's behavior for restlessness, anxiety, or confusion q2h; use safety precautions if symptoms are present. When excess fluid volume compromises cardiac output, the client may experience cerebral tissue hypoxia, and the client may demonstrate restlessness and anxiety. When the excess fluid volume results in hyponatremia, symptoms such as agitation, irritability, inappropriate behavior, confusion, and seizures may occur (McConnell et al, 2007). 5. Monitor electrolyte levels carefully, including sodium levels and potassium levels, with both increased and decreased levels possible. Elderly are prone to electrolyte abnormalities because of failure of regulatory mechanisms associated with heart and kidney disease, plus the large number of medications that are taken that can
3. The client only has one usable lung (the right lung) but it remained free of any additional sounds such as wheezing or crackles.
4. Clients behavior was upbeat and appropriate during all situations.
5. The clients CBC and CMP all came back from a 0600 lab draw and did not provide any evidence of skewed electrolyte levels
affect electrolyte levels (Zarowitz & Lefkovitz, 2008). Evaluation: (Summarize impressions of patients progress towards outcomes) The client is progressing very well toward maintaining his current fluid status. It is safe to say that the client has adequately maintained fluid homeostasis; however, his loss in weight needs to be monitored as well to prevent him from becoming fluid volume deficient.
Problem # _5_ & Nursing Diagnosis: Decreased Cardiac output r/t altered electrical conduction secondary to dysrhythmia AEB arrhythmia (chronic A-FIB); bradycardia; electrocardiographic changes; palpitations; tachycardia; edema, fatigue on exertion. General Goal: Increase cardiac output Behavioral Outcome Objective(s): The client will: Demonstrate adequate cardiac output as measured by blood pressure and pulse rate and rhythm to be within normal parameters for client (120-129/80-89 and 60100bpm); strong peripheral pulses; and an ability to tolerate activity without symptoms of dyspnea, syncope, or chest pain prior to discharge. Verbalize an increased understanding for proper nutrition related to a heart healthy diet following a consultation with the nutritionist.
Nursing interventions with rationales & references 1. Place client in semi-Fowler's or high Fowler's position with legs down or in a position of comfort. Elevating the head of the bed and legs in down position may decrease the work of breathing and may also decrease venous return and preload Ackley, B., 2012)
Patient response to interventions
1. Client had already been placed in a semi-Fowlers position prior to receiving the client for the shift. Client did not exhibit any signs of dyspnea (rapid or shallow breathing, cyanosis, or air hunger) during the period of care. Client converted between NSR and A-Fib throughout period of care. 2. The morning was kept quiet with few interruptions with the exceptions of q2h assessments and medication administration. However, the clients family arrived in the afternoon and presented some disruption.
2. Provide a restful environment by minimizing controllable stressors and unnecessary disturbances such as combining nursing actions like blood draws and medication administration. Schedule rest periods after meals and activities.
Rest helps lower arterial pressure and reduce the workload of the myocardium by diminishing the requirements for cardiac output (Fauci et al, 2008). 3. Check blood pressure, pulse, and condition before administering cardiac medications such as angiotensin-converting enzyme (ACE) inhibitors, digoxin, calcium channel blockers, and beta-blockers such as metoprolol. Notify physician if heart rate or blood pressure is low before holding medications. It is important that the nurse evaluate how well the client is tolerating current medications before administering cardiac medication (Ackley, B., 2012). 4. Monitor intake and output. If client is acutely ill, measure hourly urine output and note decreases in output Clinical practice guidelines cite that monitoring I&Os are useful for monitoring effects of diuretic therapy. Decreased cardiac output results in decreased perfusion of the kidneys, with a resulting decrease in urine output (Ackley, B., 2012). 3. The clients BP was 136/82 prior to administration of his antihypertensive. This is an allowable BP for the administration of Metoprolol. Upon the next assessment (q2h) the clients BP was 118/78.
4. The client was NPO for the 24 hours prior to period of care and as such all intake was through IV infusion; so the staff nurse and CNA was responsible for recording the clients intake and a urinary catheter was used to monitor output. The client did not have any vomiting to increase the amount of output. There was a 100mL difference in the output versus the input (in favor of output). 5. The client was NPO for 24 hours prior to period of care; however, the clients NPO status was discontinued in enough time for the client to eat lunch with his family. The clients family brought him fast
5. Serve small, frequent, sodiumrestricted, low-cholesterol meals. Sodium-restricted diets help decrease fluid volume excess. Lowcholesterol diets help decrease atherosclerosis, which causes
coronary artery disease. Clients with cardiac disease tolerate smaller meals better because they require less cardiac output to digest (Fauci et al, 2008).
food and as such the family was educated on the necessity to restrict these types of foods for the client. The family was not receptive and provided the excuse of needing something fast.
Evaluation: (Summarize impressions of patients progress towards outcomes) The client was able to understand the nursing interventions and their importance. However, he seemed to disregard any instructions related to nutrition as his family enabled him to eat fast food. The client responded well to all other interventions and his cardiac output was not decreased.
Problem # _6_ & Nursing Diagnosis: Anxiety (moderate) r/t hospitalization AEB inability to sleep, restlessness, disease process, knowledge deficit, changes in field of vision, acute pain. General Goal: Reduce anxiety Behavioral Outcome Objective(s): The client will: Identify and verbalize symptoms of anxiety such as restlessness, tearfulness, increased heart rate, increased respirations, and withdrawal within 48 hours of admission Identify, verbalize, and demonstrate techniques to control anxiety such as deep breathing, guided imagery, and journaling prior to discharge. Have posture, facial expressions, gestures, and activity levels that reflect decreased distress; affect that demonstrates appropriate coping prior to discharge. Demonstrate some ability to reassure self through the use of anxiety controlling techniques learned while hospitalized. Nursing interventions with rationales & references 1. If the situational response is rational, use empathy to encourage the client to interpret the anxiety symptoms as normal. The way a nurse interacts with a client influences his/her quality of life. Providing psychological and social support can reduce the symptoms and problems associated with anxiety (Wagner & Bear, 2009). 2. Older adults report less worry than younger adults. There were no age differences in the report of somatic and affective symptoms. Thus, worry appears to play a less Patient response to interventions
1. Some anxiety is beneficial but when it becomes detrimental and negatively influences health, a need is identified. The client was encouraged to express his concern and understand that there was nothing wrong with having some anxiety. He replied in an affirmative manner.
2. The client did not expressly state that he had any anxiety, only that he had concerns about his vision not coming back. The concerns as stated by the client can be translated
prominent role in the presentation of anxiety in older adults. These findings suggest that older adults do experience anxiety differently than younger adults (Brenes, 2006). 3. Provide a quiet environment with diversion. Excessive noise increases anxiety; involvement in a quiet activity can be soothing to the elderly (Chaudhury, 2006).
to anxiety in medical terms and as such should demonstrate a moderate level of anxiety based on the evidence provided in the intervention. 3. The client sat quietly in his room reading a newspaper and doing the crossword puzzle for much of the morning. This environment seemed to be conducive for him to relax. However, it was during this time that the client had expressed concerns about his vision and seeing the ophthalmologist. 4. This intervention did not occur. However, I am sure if the right nurse (female) were to have implemented this intervention it would have been received and successful.
4. Provide alternative interventions such as massage therapy, guided imagery, aroma therapy to complement traditional medical regimens. Massage intervention significantly reduced pain and anxiety in elderly clients (Manskey & Wallerstadt, 2006; Carrington et al, 2008).
Evaluation: (Summarize impressions of patients progress towards outcomes) The clients anxiety was not alleviated or did not appear to be alleviated until his doctor came in and spoke with him about his condition and confirmed that he had a small stroke. He was also informed that he would have to see the ophthalmologist to determine if his peripheral vision would return but that it was not likely. The clients anxiety was also reduced with the arrival of his family. This demonstrates the notion that support systems are very impactful on recovery and increasing ones emotional state.
Problem # _7_ & Nursing Diagnosis: Disturbed sensory perception (visual) r/t a stroke (physiological process) and loss of peripheral vision in the right eye AEB partial loss of peripheral vision in right eye as assessed for neurological function, verbalization of only being able to see in a straight line. General Goal: Adapt to partial loss of vision Behavioral Outcome Objective(s): The client will: Explain plan to modify lifestyle to accommodate visual impairment following discharge education. Incorporate use of lighting to maximize visual abilities prior to discharge. Remain free of physical harm resulting from decreased balance and loss of peripheral vision during hospitalization. Nursing interventions with rationales & references 1. Keep call light button within client's reach, and check location of call light button before leaving the room. This will reinforce the use of the call light to help prevent injuries and falls and begin to assist the client in adjusting to the new disability. A study demonstrated that a large percentage of hospitalized clients are unable to utilize the call light button and are very vulnerable as a result (Ackley, B., 2012). 2. Recommend client have vision evaluated by optometrist or ophthalmologist as appropriate to determine if an improvement in visual acuity is possible. Clients Patient response to interventions
1. The call light was kept on the left side of the client at all times as this eye was not affected during the clients TIA. The client used the call light twice during the period of care.
2. The client already had a referral to see an ophthalmologist prior to the period of care. However, when discussed with the client, he was not aware of the time or date of the
may not have the correct prescription for their visual acuity (Ackley, B., 2012).
appointment. The client and his family should have been included in the planning of this appointment to increase empowerment and collaboration between the nurses, doctors, and client. This would also increase compliance. 3. The clients family stated that they have night lights in their kitchen and bathroom that have automatic sensors. They both confessed that they do not put their glasses on in the middle of the night to go to the bathroom but after education stated they would try to remember to use them at all times.
3. Educate the client about increasing the amount of light in the environment for elderly eyes; ensuring it is nonglare lighting such as night lights and lights that are low wattage. Increased lighting can help compensate for some of the visual changes of aging including reduced visual acuity, reduced contrast sensitivity, and reduced color discrimination (Ackley, B., 2012).
4. Explore with the client the potential 4. This was not assessed as this advantages of a vision loss selfintervention was not provided. management program and make However, as a part of his referral to appropriate recommendations for home health, community resource referrals. Obtain a list of education was also included for the community resources that will help home health nurse. the client better adjust to the new disability. Clients often do not recognize the value of learning problem solving for their disabilities(Ackley, B., 2012). Evaluation: (Summarize impressions of patients progress towards outcomes) Client seems to rely on his spouse for support and care outside of the hospital. While the client has a strong support network, this may lead the spouse to some care giver role strain. Based on reporting from the client and spouse, the home has some adjustments that will assist the client in making some lifestyle modifications related to his recent disability. Prior to discharge the client did not have any accidents or physical harm.
References Ackley, Betty. (2012). Nursing diagnosis handbook: A guide to planning care, (9 th Ed.) St. Louis: Mosby. Brenes, G. (2006). Age differences in the presentation of anxiety. Aging & Mental Health, 10(3), 298-302. Celli, B. W., & MacNee, W. (2004). Standards for the diagnosis and treatment of patients with COPD. European Respiratory Journal, 23(6), 932-946. doi: 10.1183/09031936.04.00014304. Chaudhury, H., Mahmood, A., & Valente, M. (2006). Nurses' perception of singleoccupancy versus multioccupancy rooms in acute care environments: an exploratory comparative assessment. Applied Nursing Research, 19(3), 118-125. Considine, J. (2005). The role of nurses in preventing adverse events related to respiratory dysfunction: literature review, Journal of Advanced Nursing 49(6):624-633, 2005. 21.Djousse L. & Granziano M. (2007). Breakfast cereals and risk of heart failure in the physicians' health study I, Arch Int Med 167(19):2080-2085. Doenges, M. E., Moorhouse, M. F., & Murr, A. C. (2011).Nurses pocket guide, diagnoses, prioritized interventions, and rationales. (12 ed.). F A Davis Co.
McConnell J.S., Fox, T.J., Josson, J.P. & Subramanian A. (2007). About a cupful: a prospective study into accuracy of volume estimation by medical and nursing staff, Accident and Emergency Nursing 15(2):101-105, 2007. Simmons, Patrik & Simmons, Mary. (2004). Informed nursing practice: the administration of oxygen to patients with COPD, Medsurg Nursing 13(2):82-85, 2004. 14.Zarowitz B, and Lefkovitz A. (2008). Recognition and treatment of hyperkalemia, Geriatric Nursing 29(5):333-339, 2008.
You might also like
- Jared Griffin Care PlanDocument14 pagesJared Griffin Care PlanKarina Rodriguez100% (4)
- Christopher Parrish Care PlanDocument7 pagesChristopher Parrish Care PlanKarina Rodriguez100% (2)
- 8 Sample Care Plans For ACDFDocument11 pages8 Sample Care Plans For ACDFacasulla98No ratings yet
- 10 CaritosDocument3 pages10 CaritosDARREN EDMARK100% (4)
- System Disorder - Cystic FibrosisDocument1 pageSystem Disorder - Cystic Fibrosisjorge herreraNo ratings yet
- Cramp Pages 1Document10 pagesCramp Pages 1masi10No ratings yet
- Cognitive Distortions: Carrie L. Yurica and Robert A. DitomassoDocument2 pagesCognitive Distortions: Carrie L. Yurica and Robert A. DitomassoIrsanti sasmitaNo ratings yet
- Nursing Care Plan Format Name: - Medical Diagnosis: Myasthenia Gravis DateDocument2 pagesNursing Care Plan Format Name: - Medical Diagnosis: Myasthenia Gravis DateSheryl Ann Barit Pedines100% (1)
- Nursing Care Plan: Interaction Immediate Cause Goal: Effectivenes SDocument6 pagesNursing Care Plan: Interaction Immediate Cause Goal: Effectivenes SCatherine Kaye Marquez RoxasNo ratings yet
- Lewis COPD Case StudyDocument2 pagesLewis COPD Case Studyatarisgurl08No ratings yet
- Case Study - EmphysemaDocument6 pagesCase Study - Emphysemamackie_041992No ratings yet
- NANDA Nursing DiagnosesDocument8 pagesNANDA Nursing DiagnosesShreejana PrajapatiNo ratings yet
- Nursing care process in patients with chronic obstructive pulmonary diseaseFrom EverandNursing care process in patients with chronic obstructive pulmonary diseaseNo ratings yet
- Plan of Care For:: Nursing Diagnosis: Excess Fluid VolumeDocument3 pagesPlan of Care For:: Nursing Diagnosis: Excess Fluid VolumeKenji CadizNo ratings yet
- Activity Intolerance Care Plan For CFDocument8 pagesActivity Intolerance Care Plan For CFapi-314197645No ratings yet
- Guide Mse For Vsim Sharon ColeDocument3 pagesGuide Mse For Vsim Sharon Cole002No ratings yet
- Aortic Aneurysm (Abdominal AneurysmDocument3 pagesAortic Aneurysm (Abdominal AneurysmMenly SusadaNo ratings yet
- Copd Case StudyDocument5 pagesCopd Case StudyJake Yvan DizonNo ratings yet
- Student Nurses' Community: Nursing Care Plan Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocument3 pagesStudent Nurses' Community: Nursing Care Plan Assessment Diagnosis Inference Planning Intervention Rationale Evaluationgreyciee은No ratings yet
- Nursing Care Plans For UTIDocument2 pagesNursing Care Plans For UTIHannah Pin67% (3)
- Nursing Care Plans WideDocument232 pagesNursing Care Plans WideTomohiro Horie100% (5)
- Septic ShockDocument1 pageSeptic ShockShaine Wolfe100% (1)
- Nursing Care Plan FinalDocument16 pagesNursing Care Plan FinalErickson OcialNo ratings yet
- Nursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Document9 pagesNursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Gayu Patel0% (1)
- Nursing Care Plan of Client With Fluid and Electrolyte ImbalanceDocument28 pagesNursing Care Plan of Client With Fluid and Electrolyte ImbalanceCj Aguilar50% (2)
- Care Plan For Excess Fluid Volume ExampleDocument3 pagesCare Plan For Excess Fluid Volume ExampleVette Angelikka Dela CruzNo ratings yet
- Imbalanced Nutrition: Less Than Body RequirementDocument10 pagesImbalanced Nutrition: Less Than Body RequirementDangz SkiiNo ratings yet
- Activity Intolerance Care PlanDocument4 pagesActivity Intolerance Care Planapi-315890029No ratings yet
- Prepu Psych Chapter 1Document329 pagesPrepu Psych Chapter 1nana100% (1)
- Nusing CareplanDocument3 pagesNusing Careplanardec_143No ratings yet
- Peptic Ulcer DiseaseDocument1 pagePeptic Ulcer DiseaseEunice CortésNo ratings yet
- Nursing Care Plans All PresentationsDocument23 pagesNursing Care Plans All PresentationsKaren Joyce Costales Magtanong100% (3)
- Congestive Heart FailureDocument37 pagesCongestive Heart FailurePierre Aseron ManuelNo ratings yet
- SBAR Report To Physician About A Critical SitutionDocument3 pagesSBAR Report To Physician About A Critical SitutionRandolph DjanieNo ratings yet
- NANDA Nursing Diagnosis List 2012-2014Document1 pageNANDA Nursing Diagnosis List 2012-2014athena190% (1)
- NCPDocument4 pagesNCPShella CondezNo ratings yet
- Risk For Falls Aeb Loss of BalanceDocument4 pagesRisk For Falls Aeb Loss of BalanceAlexandrea MayNo ratings yet
- Acute Pain Care PlanDocument1 pageAcute Pain Care Planstacie4roher4smith100% (1)
- CC Concept MapDocument9 pagesCC Concept Mapapi-606252228No ratings yet
- Mushtaq Ahmad: Running Head: REFLECTIVE LOG 1Document5 pagesMushtaq Ahmad: Running Head: REFLECTIVE LOG 1Shafiq Ur RahmanNo ratings yet
- Pain Care PlanDocument18 pagesPain Care Planjordanw0613No ratings yet
- Medical Surgical Nursing IIDocument52 pagesMedical Surgical Nursing IItwinkle143No ratings yet
- Gordon's 11 Functional Health PatternsDocument4 pagesGordon's 11 Functional Health Patternsnina angelaNo ratings yet
- Hip Fracture Concept MapDocument2 pagesHip Fracture Concept MapPriyal ParikhNo ratings yet
- NCP AnginaDocument3 pagesNCP AnginaShie LA100% (1)
- 116 ExamDocument14 pages116 ExamZhailyn Joy DumlaoNo ratings yet
- Nursing Diagnosis & Careplan SamplesDocument5 pagesNursing Diagnosis & Careplan SamplesE94% (18)
- Risk For Aspiration: Risk For Aspiration: at Risk For Entry of Gastrointestinal Secretions, Oropharyngeal SecretionDocument6 pagesRisk For Aspiration: Risk For Aspiration: at Risk For Entry of Gastrointestinal Secretions, Oropharyngeal SecretionAngie MandeoyaNo ratings yet
- Example of Nursing Care Plan (Pathophysiology)Document5 pagesExample of Nursing Care Plan (Pathophysiology)Elizabeth ZamoraNo ratings yet
- Pico PaperDocument11 pagesPico Paperapi-250046004100% (4)
- Ineffective Cerebral Tissue Perfusion Related ToDocument7 pagesIneffective Cerebral Tissue Perfusion Related TohannahNo ratings yet
- Medical Surgical Nursing 2nd Edition Osborn Test BankDocument17 pagesMedical Surgical Nursing 2nd Edition Osborn Test BankdimyjebaNo ratings yet
- Hypovolemic Shock Concept MapDocument1 pageHypovolemic Shock Concept MapJM AsentistaNo ratings yet
- NANDA NursingDocument11 pagesNANDA Nursingesteffie21No ratings yet
- Nursing Care PlanDocument22 pagesNursing Care PlanjamNo ratings yet
- Management of Patients With Gastric and Duodenal DisordersDocument47 pagesManagement of Patients With Gastric and Duodenal DisordersJor GarciaNo ratings yet
- Respiratory Comp: Nursing DiagnosisDocument1 pageRespiratory Comp: Nursing DiagnosisMaria Francheska OsiNo ratings yet
- Nanda Needs ListDocument24 pagesNanda Needs ListObrian ReidNo ratings yet
- Teaching Plan Assignment Template Assessment (These Are Possible Assessment Elements)Document4 pagesTeaching Plan Assignment Template Assessment (These Are Possible Assessment Elements)api-402048659No ratings yet
- Tagum Doctors College, Inc.: Mahogany ST., Rabesubd., Tagum City E-MailDocument4 pagesTagum Doctors College, Inc.: Mahogany ST., Rabesubd., Tagum City E-MailRoel John Atamosa CasilacNo ratings yet
- Chicago Review Press NCLEX-PN Practice Test and ReviewFrom EverandChicago Review Press NCLEX-PN Practice Test and ReviewRating: 4 out of 5 stars4/5 (4)
- Vipragen-Brochure-v3.0 FinalDocument8 pagesVipragen-Brochure-v3.0 Finaldear14us1984No ratings yet
- Submandibular Salivary Sialolith: A Case Report With Review of LiteratureDocument4 pagesSubmandibular Salivary Sialolith: A Case Report With Review of LiteraturejoaompradoNo ratings yet
- Renal Calculi: Ahmednagar Homoeopathic Medical College & Hospital AhmednagarDocument15 pagesRenal Calculi: Ahmednagar Homoeopathic Medical College & Hospital AhmednagarSuhas IngaleNo ratings yet
- Section16 - Questions and AnswersDocument62 pagesSection16 - Questions and Answersdivine venturoNo ratings yet
- Unit V: Conti Upper Respiratory Tract Infection: PharyngitisDocument17 pagesUnit V: Conti Upper Respiratory Tract Infection: PharyngitisshaistaNo ratings yet
- Hemodialysis PDFDocument14 pagesHemodialysis PDFerikazoku moNo ratings yet
- The Ultimate Microbial CleanseDocument12 pagesThe Ultimate Microbial Cleanseromalfio100% (3)
- Food and Nutrition in EmergencyDocument44 pagesFood and Nutrition in EmergencyStefania WidyaNo ratings yet
- Low Carb Diet For Weight Loss and Diabetes - Unwin 2014 PDFDocument4 pagesLow Carb Diet For Weight Loss and Diabetes - Unwin 2014 PDFPaul MayNo ratings yet
- Health DLP STAGES OF INFECTIONDocument9 pagesHealth DLP STAGES OF INFECTIONmarielabianaNo ratings yet
- Optimum Levels of IodineDocument14 pagesOptimum Levels of IodineK AnjaliNo ratings yet
- PD 856 - Sanitation Code PDFDocument36 pagesPD 856 - Sanitation Code PDFskylark74100% (3)
- Features Extraction and Classification For Detection of Kidney Stone Region in Ultrasound ImagesDocument3 pagesFeatures Extraction and Classification For Detection of Kidney Stone Region in Ultrasound Imagesfardous ahmedNo ratings yet
- Challanage Case in Autoimmune DiseaeDocument349 pagesChallanage Case in Autoimmune DiseaeheshamNo ratings yet
- Zohar SanacionDocument3 pagesZohar SanacionMartin RomeroNo ratings yet
- Grade 1 Nutritional StatusDocument13 pagesGrade 1 Nutritional StatusbogtikNo ratings yet
- Genetics Review Questions KeyDocument37 pagesGenetics Review Questions KeyRyan Christian PatriarcaNo ratings yet
- Corazon y Mente CercanosDocument3 pagesCorazon y Mente CercanosFernando VegaNo ratings yet
- Salient Points of The Philippine Blood Banking LawsDocument76 pagesSalient Points of The Philippine Blood Banking LawsAngelica Parreñas BayonaNo ratings yet
- Xi Cleft (Accumulation Point) : DiagnosisDocument4 pagesXi Cleft (Accumulation Point) : DiagnosisZareen FNo ratings yet
- 2020 11 07 XII Economics 1Document17 pages2020 11 07 XII Economics 1Sjft6hd FfNo ratings yet
- Research Paper On Isolation of YeastDocument8 pagesResearch Paper On Isolation of Yeastefgncpe8100% (1)
- English Language "Bacteria" Dosen Pembimbing Aulia Suryasari S.PDDocument4 pagesEnglish Language "Bacteria" Dosen Pembimbing Aulia Suryasari S.PDIsmilNo ratings yet
- Study of Foreign Body OesophagusDocument3 pagesStudy of Foreign Body OesophagusAnonymous ST1Ot2GAHxNo ratings yet
- A 7 Day Weight Loss Plan - The Times of IndiaDocument9 pagesA 7 Day Weight Loss Plan - The Times of IndiaAlphonse Raj DavidNo ratings yet
- ABC of Red EyeDocument5 pagesABC of Red Eyeakmar887100% (1)
- Antimanic DrugsDocument22 pagesAntimanic DrugsMarlet N. Ortega100% (2)
- Effects of Textile Dyes On Health and The Environment and Bioremediation Potential of Living OrganismsDocument17 pagesEffects of Textile Dyes On Health and The Environment and Bioremediation Potential of Living OrganismsfikaNo ratings yet