Nursing Diagnosis Risk For Impaired Skin Integrity
Nursing Diagnosis Risk For Impaired Skin Integrity
Uploaded by
Razz Domenique Reyes EscarosCopyright:
Available Formats
Nursing Diagnosis Risk For Impaired Skin Integrity
Nursing Diagnosis Risk For Impaired Skin Integrity
Uploaded by
Razz Domenique Reyes EscarosOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Nursing Diagnosis Risk For Impaired Skin Integrity
Nursing Diagnosis Risk For Impaired Skin Integrity
Uploaded by
Razz Domenique Reyes EscarosCopyright:
Available Formats
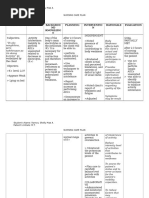
Need A C T I V I T Y
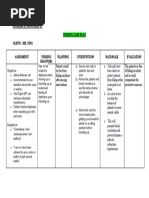
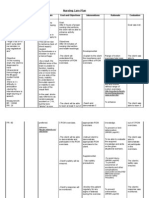
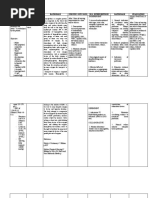
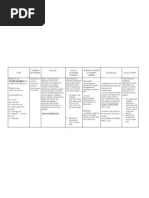
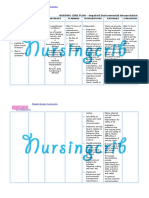
Nursing Diagnosis
Objective of Care
Nursing Intervention
Risk for Impaired Skin Integrity Related Extremes of Age. Rationale: Immobility, which leads to pressure, shear, and friction, is the factor most likely to put an individual at risk for altered skin integrity. Older patients skin is normally elastic and has
That within our 8 hours patient would be able to: A. Patients skin remains intact as evidenced by: Capillary Refill time of 3 or less than 3 seeconds. Absence of pressure ulcer. B. Verbalize the importance of preventive measures.
1. Reassess patients skin condition R = to know the extent of the damage. 2. Change the patients position frequently when at bed. R = Position changes relieve pressure, restore blood flow, and promote skin integrity. 3. Use pressure-relieving beds, mattress overlays, and chair cushions. R = Theses devices redistribute pressure when frequent position changes are not possible. 4. Apply lotion if not contraindicated. R = these prevent friction and shear. 5. Encourage to wear cotton fabric clothes. R = skin friction caused by stiff or rough clothes leads to irritation. 6. Emphasize the importance of adequate nutrition and oral fluid intake. R = improve nutrition and hydration will improve skin condition. 7. Encourage ambulation R = Ambulation reduces pressure on the skin from immobility. 8. Increase tissue perfusion by massaging around the affected area. R = massaging the actual reddened area may damage the skin further. 9. Limit chair sitting to 2 hours at any one time and encourage patient to shift weight every 15 minutes. R = pressure ober the sacrum may exceed 100mmHg pressure during sitting. The pressure necessary to close skin capillaries is aroung 32mmHg any pressure greater then 32 mmHg may result to ischemia
to span on nursing care our
E X E R C I S E
P A T T E R N
less moisture, making for higher risk of skin impairment.
My sister has been diagnosed with frontotemporal dementia. She is 57 years old. In August 2008 she didn't show up for work, and when I went to her home I discovered that she had started hoarding. I had not been to her house in several years. Whenever I went there she would meet me outside and would not invite me in. I found her inside lying on her bed in the same clothes as the day before. No sheets on the bed, and lying in urine. After we arrived at the hospital I asked them to run an MRI because she had had a brain tumor in 1988. After the MRI was examined I was told that she had a head trauma from a car accident. I knew she hadn't and kept pressing for more tests. They ran a CT scan and then another neurologist looked at her MRI and saw the disease. This has nothing to do with the brain tumor. She began forgetting to go work, getting angry at other drivers when driving, forgetting to pay bills and having crying episodes at work. In January she had an incident at work where she got mad and threw a box at someone. After that we had to put her on disability and take away her driving privileges. This has been hard for her to understand because she thinks she is fine. The hardest part for me was telling the doctors (in front of her) what was going on. This is only the beginning I know and I must find the courage to talk to her about plans for her future. I am her only sister. My brother helps but can do only so much. My parents are 80 and 81 and they are in better health than my sister. It has been 8 months, and I finally have her house clean. The dementia itself is enough to deal with. Now I also have to take care of her financial and medical decisions. I make sure that I still make the time to enjoy my 3 grandchildren and go away periodically with my husband and do nothing. Absolutely nothing. Right now she is at the point where she is child like and does not want to bathe, brush her teeth or go to bed. What comes next?
AUTHOR: Karen Loise SOURCE: Medscape URL: http://medscape.ucsf.edu/ftd/community-support/personal-stories/Karen
You might also like
- Assessment B - Short Answer SITXCOM005Document4 pagesAssessment B - Short Answer SITXCOM005Pahn Panrutai100% (3)
- Patriarca, Janna Mae H. Nursing Care Plan Client: Mr. YingDocument1 pagePatriarca, Janna Mae H. Nursing Care Plan Client: Mr. Yingjanna mae patriarca100% (2)
- Activity Intolerance Related To Decrease Blood FlowDocument3 pagesActivity Intolerance Related To Decrease Blood FlowDarkCeades100% (3)
- NCP BkaDocument4 pagesNCP BkaKeeshia CesnerosNo ratings yet
- NCP-Self Care DeficitDocument2 pagesNCP-Self Care DeficitJon Eric G. Co100% (2)
- "Mayroong Namuong Dugo Sa Utak Niya Kaya Hindi Maayos Ang Daloy NG Dugo Rito" As Verbalized by The Patient'sDocument4 pages"Mayroong Namuong Dugo Sa Utak Niya Kaya Hindi Maayos Ang Daloy NG Dugo Rito" As Verbalized by The Patient'sAllisson BeckersNo ratings yet
- Situación 2 - A Kindred SpiritDocument3 pagesSituación 2 - A Kindred SpiritgreenfaNo ratings yet
- Three Levels of Awareness by FreudDocument2 pagesThree Levels of Awareness by FreudL'Aurore100% (7)
- NCP - Acute PainDocument2 pagesNCP - Acute PainsAm_300% (1)
- NCP For Impaired Skin IntegrityDocument3 pagesNCP For Impaired Skin IntegrityAemz Alacasnap Ainegud100% (1)
- NCP Sleep DisturbanceDocument1 pageNCP Sleep DisturbanceIsrael Soria EsperoNo ratings yet
- Acute Pain NCPDocument1 pageAcute Pain NCPJed AvesNo ratings yet
- Impaired Skin IntegrityDocument3 pagesImpaired Skin IntegrityAubrey SungaNo ratings yet
- ASSESSMENT S: "Nanghihina Ako, Hindi Ko Magawa Yung Mga GustoDocument1 pageASSESSMENT S: "Nanghihina Ako, Hindi Ko Magawa Yung Mga GustoCherie MayNo ratings yet
- Self Care DeficitDocument3 pagesSelf Care DeficitAddie Labitad100% (2)
- Drug Study FinalDocument6 pagesDrug Study FinalJade HemmingsNo ratings yet
- NCP Disturbed Body ImageDocument2 pagesNCP Disturbed Body ImageDoneva Lyn MedinaNo ratings yet
- Activity IntoleranceDocument3 pagesActivity IntoleranceRheegell Ellar-Fuertes50% (2)
- NCP Sleep PatternDocument3 pagesNCP Sleep PatternRA Balaoing100% (1)
- Activity IntoleranceDocument3 pagesActivity Intolerancelouie roderos0% (1)
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument5 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationArian May MarcosNo ratings yet
- NCP For Impaired Physical MobilityDocument1 pageNCP For Impaired Physical Mobilityitzme_andreaNo ratings yet
- Nursing Care Plan Impaired CommunicationDocument3 pagesNursing Care Plan Impaired CommunicationRamiel ChristopherNo ratings yet
- Self Care DeficitDocument4 pagesSelf Care DeficitEllaine Ramirez100% (1)
- Impaired Physical MobilityDocument3 pagesImpaired Physical MobilityCharmaine ChuaNo ratings yet
- NCP: Acute GastroenteritisDocument3 pagesNCP: Acute GastroenteritishauteanicoleNo ratings yet
- NCP Impaired Physical Mobility-2Document4 pagesNCP Impaired Physical Mobility-2ejoanbNo ratings yet
- Activity IntoleranceDocument3 pagesActivity Intolerancelouie roderosNo ratings yet
- Assessment Diagnosis Background Knowledge Planning Intervention Rationale Evaluation SubjectiveDocument3 pagesAssessment Diagnosis Background Knowledge Planning Intervention Rationale Evaluation SubjectiveAngelaNo ratings yet
- NCP 1Document1 pageNCP 1hsiriaNo ratings yet
- NCP For Cervical SpondylosisDocument3 pagesNCP For Cervical Spondylosishannah0% (1)
- NCP Icu-CcuDocument6 pagesNCP Icu-CcuJohn CenasNo ratings yet
- Risk For SuffocationDocument2 pagesRisk For SuffocationKimberly Subade Mandilag100% (2)
- Impaired Physical Mobility Related To Pain and DiscomfortDocument2 pagesImpaired Physical Mobility Related To Pain and DiscomfortRis NapolisNo ratings yet
- Assessment Diagnosis Planning Nursing Interventions Rationale EvaluationDocument6 pagesAssessment Diagnosis Planning Nursing Interventions Rationale EvaluationChristine Denise Venus ValentinoNo ratings yet
- Acute Pain NCPDocument1 pageAcute Pain NCPRyan PanNo ratings yet
- Impaired Skin IntegrityDocument2 pagesImpaired Skin IntegrityRoseben SomidoNo ratings yet
- NCP Impaired Skintissue IntegrityDocument5 pagesNCP Impaired Skintissue IntegrityArt Christian RamosNo ratings yet
- NCP Delayed Wound RecoveryDocument5 pagesNCP Delayed Wound RecoveryDarkCeades100% (2)
- NCP AnxietyDocument2 pagesNCP AnxietyVanessa SumalbagNo ratings yet
- NCP - Activity IntoleranceDocument3 pagesNCP - Activity Intolerancejanelee2824No ratings yet
- Short Term: Nursing Care Plan Cues Nursing Diagnosis Objectives Interventions Rationale EvaluationDocument3 pagesShort Term: Nursing Care Plan Cues Nursing Diagnosis Objectives Interventions Rationale EvaluationChristy BerryNo ratings yet
- NCP Acute PainDocument3 pagesNCP Acute PainSheene Lysethea Sioteco AguilosNo ratings yet
- Ineffective Tissue PerfusionDocument3 pagesIneffective Tissue PerfusionMitsika AnadiaNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care PlanAldrein GonzalesNo ratings yet
- NCP Impaired Skin IntegrityDocument3 pagesNCP Impaired Skin IntegrityKingJayson Pacman06No ratings yet
- Assessment Diagnosis Planning Implementation Evaluation No Subjective Cues ObjectiveDocument3 pagesAssessment Diagnosis Planning Implementation Evaluation No Subjective Cues ObjectiveMaverick Lim100% (1)
- Nursing Care Plan: Cues Problem Scientific Reason Nursing Intervention Rationale EvaluationDocument1 pageNursing Care Plan: Cues Problem Scientific Reason Nursing Intervention Rationale Evaluationeihjay-bravo-8041No ratings yet
- Nursing Care Plan Risk For InjuryDocument1 pageNursing Care Plan Risk For InjuryAce Dioso TubascoNo ratings yet
- NCP Altered ComfortDocument2 pagesNCP Altered ComfortMadz Tajal0% (1)
- NCPDocument6 pagesNCPKyla Carbonel100% (2)
- NCP 1Document1 pageNCP 1Rommelie Caballero100% (1)
- Acute Pain Related To Tissue Trauma 2° To MVADocument1 pageAcute Pain Related To Tissue Trauma 2° To MVARachel Saavedra100% (3)
- Nursing Care Plan For Impaired Environmental Interpretaion NCPDocument4 pagesNursing Care Plan For Impaired Environmental Interpretaion NCPderic100% (3)
- NCP FinalDocument4 pagesNCP Finalmarkanthony39030% (1)
- NCP of Client With Cancer Servix With Multiple Bone MetastasisDocument17 pagesNCP of Client With Cancer Servix With Multiple Bone MetastasisHarismaPratamaNo ratings yet
- Ingles SssssDocument4 pagesIngles SssssNaimir GuarinoNo ratings yet
- Mother&child - Rights - Immigrants in NorwayDocument86 pagesMother&child - Rights - Immigrants in NorwayAy GunNo ratings yet
- James Clear Atomik Aliskanliklar Cinciva Mir - AzDocument258 pagesJames Clear Atomik Aliskanliklar Cinciva Mir - Azkuwatps4No ratings yet
- Transposition of The Great Arteries (TGA)Document4 pagesTransposition of The Great Arteries (TGA)Tommy JohnsonNo ratings yet
- Hard anodising paperDocument10 pagesHard anodising paperpvangraan95No ratings yet
- Commercial Management of Construction-SandeshDocument15 pagesCommercial Management of Construction-SandeshHaneefa Ch100% (1)
- WaterDocument30 pagesWaterPriya Gupta0% (1)
- Project Based LearningDocument2 pagesProject Based Learningsgaer100% (3)
- Chapter 14Document49 pagesChapter 14Ram SskNo ratings yet
- Chemistry Paper 1 2009Document7 pagesChemistry Paper 1 2009Robert EdwardsNo ratings yet
- Activity Report - DQXM With Boys BrigadeDocument6 pagesActivity Report - DQXM With Boys BrigadeDwayne Bob LerionNo ratings yet
- Application Form Declaration: Anabin WebsiteDocument2 pagesApplication Form Declaration: Anabin WebsiteManish VijayNo ratings yet
- Newsletter - 2017 (32 PG)Document32 pagesNewsletter - 2017 (32 PG)sweety kumariNo ratings yet
- CMR EnterprisesDocument5 pagesCMR EnterprisesPraveen Sangwan100% (2)
- FDS LAB MANUALDocument42 pagesFDS LAB MANUALpatiltanishka012No ratings yet
- Criteria 6 NaacDocument2 pagesCriteria 6 Naacravi03319No ratings yet
- Bcvs PPTDocument11 pagesBcvs PPTjg577wwtfyNo ratings yet
- Connoisseur of Chaos: SchnittkeDocument6 pagesConnoisseur of Chaos: SchnittkeRobert MorrisNo ratings yet
- Cost Sheet ProjectDocument12 pagesCost Sheet ProjectPowerPoint GoNo ratings yet
- Sample Request Format of Digital Forensic ExaminationDocument3 pagesSample Request Format of Digital Forensic ExaminationRura RecaNo ratings yet
- Chennai Institute of Technology Sarathy Nagar, Pudupedu, Chennai - 600 069. Multiple Choice QuestionsDocument14 pagesChennai Institute of Technology Sarathy Nagar, Pudupedu, Chennai - 600 069. Multiple Choice Questionssureshvk.20087147No ratings yet
- Physical PropertiesDocument17 pagesPhysical Propertiesjaime1234No ratings yet
- The Best Homemade Salsa For Canning - Delish KnowledgeDocument3 pagesThe Best Homemade Salsa For Canning - Delish KnowledgeAriHSPNo ratings yet
- Chapter 1 Philosophical Thoughts in Education - EditedDocument18 pagesChapter 1 Philosophical Thoughts in Education - EditedRaphael SamsonNo ratings yet
- The Daily Tar Heel For February 16, 2012Document12 pagesThe Daily Tar Heel For February 16, 2012The Daily Tar HeelNo ratings yet
- Step 3 - REP-REP-RAF0754-541070 - Removing and Installing Front Glass Slide Tilt Sunroof PanelDocument3 pagesStep 3 - REP-REP-RAF0754-541070 - Removing and Installing Front Glass Slide Tilt Sunroof PanelЖулиенИ.ВасилевNo ratings yet
- Only Q Components of Wind Energy Conversion SystemDocument20 pagesOnly Q Components of Wind Energy Conversion SystemPoyyamozhi Nadesan RanjithNo ratings yet
- Auto QtyDocument36 pagesAuto QtyKhan Muhammad AkramNo ratings yet
- Product Data: Carboguard 190 HDocument2 pagesProduct Data: Carboguard 190 HClarkFedele27100% (1)
- Limitless WDRR Installation Tech Manual HoneywellDocument47 pagesLimitless WDRR Installation Tech Manual HoneywellErnesto HcNo ratings yet
- De HSG Anh 9 2021-2022Document6 pagesDe HSG Anh 9 2021-2022hangngaqb2010No ratings yet
- Ge 4 Sim UpdatedDocument79 pagesGe 4 Sim UpdatedAna Llemit MionesNo ratings yet