0 ratings0% found this document useful (0 votes)
84 viewsAlfedson and Cook
Alfedson and Cook
Uploaded by
ppeterarmstrongAchilles tendinopathy affects athletes, recreational exercisers and even inactive people. The pathology is not inflammatory; it is a failed healing response. The source of pain in tendinopathy could be related to the neurovascular ingrowth seen in the tendon's response to injury.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Alfedson and Cook
Alfedson and Cook
Uploaded by
ppeterarmstrong0 ratings0% found this document useful (0 votes)
84 views6 pagesAchilles tendinopathy affects athletes, recreational exercisers and even inactive people. The pathology is not inflammatory; it is a failed healing response. The source of pain in tendinopathy could be related to the neurovascular ingrowth seen in the tendon's response to injury.
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Achilles tendinopathy affects athletes, recreational exercisers and even inactive people. The pathology is not inflammatory; it is a failed healing response. The source of pain in tendinopathy could be related to the neurovascular ingrowth seen in the tendon's response to injury.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
84 views6 pagesAlfedson and Cook
Alfedson and Cook
Uploaded by
ppeterarmstrongAchilles tendinopathy affects athletes, recreational exercisers and even inactive people. The pathology is not inflammatory; it is a failed healing response. The source of pain in tendinopathy could be related to the neurovascular ingrowth seen in the tendon's response to injury.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 6
REVIEW
A treatment algorithm for managing Achilles tendinopathy:
new treatment options
Hakan Alfredson, J Cook
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Br J Sports Med 2007;41:211216. doi: 10.1136/bjsm.2007.035543
Achilles tendinopathy affects athletes, recreational exercisers
and even inactive people. The pathology is not inflammatory; it
is a failed healing response. The source of pain in tendinopathy
could be related to the neurovascular ingrowth seen in the
tendons response to injury. The treatment of Achilles
tendinopathy is primarily conservative with an array of effective
treatment options now available to the primary care
practitioner. If conservative treatment is not successful, then
surgery relieves pain in the majority of cases. Directing a patient
through the algorithm presented here will maximise positive
treatment outcomes.
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
See end of article for
authors affiliations
. . . . . . . . . . . . . . . . . . . . . . . .
Correspondence to:
Dr J Cook, Musculoskeletal
Research Centre, La Trobe
University, Bundoora 3086,
Victoria, Australia;
J.Cook@.latrobe.edu.au
Accepted 22 January 2007
. . . . . . . . . . . . . . . . . . . . . . . .
P
ain in the Achilles tendon is relatively
common in recreational exercisers and indivi-
duals active in sports.
1
Achilles tendon pain
has also been reported in inactive individuals.
2
It is
seen most commonly in the mid-portion of the
tendon, but also occurs at the bonetendon
junction.
Overuse is considered to induce the condition,
3
but the aetiology and pathogenesis have not been
scientifically clarified. A study on chronic Achilles
tendinopathy (342 tendons) showed that physical
activity was not correlated with the extent of
histopathology, suggesting that physical activity
could be more important in provoking the symp-
toms than being the root cause of pathology.
4
The
lack of association between activity, pain and
structural abnormality has also been reported in
other tendons, and pathological changes are seen
on imaging in physically active asymptomatic
individuals.
5
Pathological change in the tendon can manifest
clinically as tendon swelling or nodules. It is also
clearly visible with standard soft-tissue imaging
techniques. This review focuses on treatment of
Achilles mid-tendon pain; management of rup-
ture, insertional pathology and peritendinopathy
are outside the scope of this article.
TENDON HI STOPATHOLOGY
The four cornerstones of tendon histopathology are
(1) cellular activation and increase in cell num-
bers, (2) increase in ground substance, (3)
collagen disarray and (4) neovascularisation. It is
not considered to be a primarily inflammatory
condition. Histological evaluation of Achilles ten-
don biopsies, intratendinous microdialysis
6 7
and
contemporary molecular biology techniques
(cDNA-arrays, real-time quantitative PCR) of
appropriately prepared biopsy tissue
8
all failed to
show evidence of prostaglandin-mediated inflam-
mation.
There are, however, signs of neurogenic inflam-
mation.
9
The presence of neuropeptides such as
substance P and calcitonin gene-related peptide
indicate that there still might be an inflammation
in the tendon.
10
Peripheral local noxious stimula-
tion makes peptidergic group IV fibres release
peptides from their terminals, starting various
pathophysiological processes contributing to neu-
rogenic inflammation.
WHERE DOES THE PAI N COME FROM?
It is well known that the chronic painful Achilles
and patellar tendons are difficult to treat, and the
pain mechanisms associated with these conditions
are not understood. Methods such as the above-
mentioned microdialysis, cDNA-arrays and PCR,
as well as ultrasonography combined with colour
Doppler, provide novel and potentially important
information about the chronic painful Achilles
tendon versus normal Achilles tendon.
Glutamate, a well known neurotransmitter and
very potent modulator of pain in the central
nervous system, is found in high levels in painful
tendons but not in normal tendons.
11
In conjunc-
tion with the findings of a local neurovascular
ingrowth
12
and promising results of pilot studies
with sclerosing injections, there is now some
evidence that the neural pathways associated with
tendinopathy could be associated with the neo-
vascularisation. Biopsies taken from an area with
tendinosis with neovascularisation showed nerve
structures in close relationship with the vessels;
12
studies have shown substance P nerves in the
vascular wall and calcitonin gene-related peptide
nerves close to the vascular wall.
12 13
Also, the
neurokinin-1 receptor, which is known to have a
high affinity for substance P, has been found in the
vascular wall.
14
The findings suggest, for the first
time, an explanation for the pain associated with
tendinosis. As interference with this neurovascular
ingrowth via sclerotherapy (see below) appears to
decrease pain, further research appears well
justified.
DI AGNOSI S
A correct clinical diagnosis can often be estab-
lished solely by clinical examination, especially if
the tendon exhibits focal or generalised swelling. If
a clinical diagnosis is not clear, ultrasonography or
Abbreviations: CSI, corticosteroid injection; NSAID, non-
steroidal anti-inflammatory drug
211
www.bjsportmed.com
MRI may reveal the pathology within the tendon.
15
Although
abnormalities detected by imaging are likely to be associated
with pain, it is possible that these morphological abnormalities
are painless and that pain may be arising from another source.
Clinical acumen is important to correlate clinical and imaging
examinations.
The first priority of clinical examination is to exclude acute
rupture, and the calf squeeze test has excellent validity.
16
After
demonstrating that the tendon is intact, the examination
should aim to provoke tendon pain during tendon-loading
activity. In most patients, simple single-leg heel raises will be
sufficient to cause pain. In more active individuals, however, it
may be necessary to ask the patient to hop on the spot, or hop
forward, to further load the tendon and reproduce pain.
Repetition of the loading test may be necessary in some
athletes to fully evaluate the tendon.
It is important to exclude other diagnoses such as posterior
ankle impingement, os trigonum syndrome, tenosynovitis or
dislocation of the peroneal or other plantar flexor tendons, an
accessory soleus muscle, irritation or neuroma of the sural
nerve and systemic inflammatory disease. These diagnoses
cause pain in and also around the Achilles tendon; true tendon
pain is nearly always confined to the tendon itself.
I MAGI NG
Imaging abnormalities in the tendon include hypoechoic areas
seen on ultrasound and areas with increased signal intensity
seen on MRI. These areas correspond with areas of altered
collagen fibre structure and increased interfibrillar ground
substance (proteoglycans and hydrophilic glycosaminogly-
cans).
17 18
Signal intensity on MRI has been associated with
the clinical outcome.
19
However, the pathology is also found in
tendons that appear normal on imaging.
20
Colour and power Doppler have recently added a new
dimension to standard ultrasound tendon imaging. This
imaging demonstrates blood flow in tissues. In the Achilles
tendon, blood flow is not detectable in normal tendons but
colour Doppler often reveals blood flow in pathological
tendons.
21
Such blood flow has been linked to greater pain
scores, poorer function and longer symptoms in the Achilles
tendon,
22
compared with control participants who have no
visible flow. The association, however, is not absolute.
23
The long-term clinical importance of blood vessels in
pathological tendons is not clear. Two longitudinal studies
have shown that the addition of colour Doppler at baseline
examination did not improve the diagnostic performance of
ultrasound
19
or indicate a poorer outcome.
24
Clinically, imaging should not be the sole guide for clinical
decisions; variation in symptoms such as morning stiffness and
load pain should direct treatment modification. Studies in
many tendons have indicated that clinical outcomes are
independent of imaging and change in imaging.
19 25 26
TREATMENT
Many treatments are offered to patients with painful tendons,
but the scientific evidence for most of the conservative and
surgical treatments remains sparse. Treatments that have some
evidential basis and have been investigated with randomised
controlled trials include eccentric exercise, glyceryl trinitrate
patches, electrotherapy (microcurrent and microwave), scleros-
ing injections and non-steroidal anti-inflammatory drugs
(NSAIDs). Of these, NSAIDs showed little or no effect on
outcome, and further discussion of medication has not been
included in this review.
27 28
There are no randomised or
prospective studies that compare different conservative and
surgical treatment regimens.
Conservative treatment is recommended as the initial
strategy by most authors.
29 30
This strategy includes identifica-
tion and correction of possible aetiological factors, and a
symptom-related approach. Generally, the initial treatment
consists of a multifactorial approach that may include a
combination of rest (complete or modified activity), medication
(NSAIDs, corticosteroids), orthotic treatment (heel lift, change
of shoes, corrections of malalignments), stretching and
strength training.
If conservative treatment fails, surgical treatment is insti-
tuted. It has been a general opinion that in about 25% of
patients with chronic painful conditions located in the
Achilles tendon, non-surgical treatment is not successful and
surgical treatment is needed.
31
For the Achilles tendon, fre-
quency of surgery has been shown to increase with patients
age, duration of symptoms and occurrence of tendinopathic
changes.
31 32
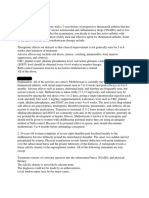
A treatment algorithm has been constructed to place these
treatment options in a clinical reasoning order (fig 1). This
order is appropriate for most individuals with Achilles tendon
pain, but may need to vary in special cases such as the elite
athlete, the person with acute tendon pain unable to fully bear
weight or the older individual who may be unable to complete
an exercise-based programme. The doctor must interpret
individual needs and modify the algorithm for each clinical
presentation.
NON-OPERATI VE TREATMENT METHODS
Eccent ri c muscul ot endi nous trai ni ng
Curwin,
33
and Curwin and Stanish
34
in 1984, stressed the
importance of eccentric training as a part of the rehabilitation
of tendon injuries. They demonstrated the success of a simple
6-week programme of progressive tendon load.
34
Alfredson et al
adapted this programme and scientifically evaluated an
eccentric calf muscle training programme for painful mid-
portion Achilles tendinopathy.
2 35
Alfredsons model of eccentric training involves no con-
centric loading and emphasises the need for patients to
complete the exercise protocol despite pain in the tendon. If
patients experience no tendon pain doing this programme,
the load should be increased until the exercises provoke
pain. Good short-term and long-term clinical results have
been reported.
3537
This 12-week programme is effective when
the other conventional treatments (rest, NSAIDs, change of
shoes, orthoses, physical therapy and ordinary training pro-
grammes) have failed and is successful in approximately
90% of those with mid-tendon pain and pathology.
Insertional Achilles tendon pain is not as responsive, and
good clinical results are achieved in approximately 30% of
tendons.
38
A follow-up study (mean 3.8 years later) of patients treated
with eccentric training indicated the majority of the patients
were satisfied and back to previous tendon-loading activity
level. Interestingly, the tendon thickness had decreased
significantly, and ultrasonographically the tendon structure
looked more normal.
39
The same 12-week programme resulted
in a decrease in tendon volume assessed with MRI, as well as a
decrease in tendon signal intensity by 23%.
40
Other exercise regimes that incorporate an eccentric compo-
nent are also effective,
41
but have not been as rigorously
evaluated as the Alfredson programme. A concentric calf-
muscle training programme (calf raises) did not prove as
effective as the eccentric (heel-drop) training programme.
42
In
the eccentric group, 82% of patients were satisfied and back
to previous activity level at the completion of treatment
compared with those doing concentric exercise (36% satisfied
patients).
212 Alfredson, Cook
www.bjsportmed.com
Why does eccent ri c exerci se reduce pai n i n
t endi nopat hy?
Although there are several possible explanations for the
effectiveness of eccentric exercise, none have been fully
investigated. Eccentric exercise alters tendon pathology in both
the short term and the long term. In the short term, a single
bout of exercise increases tendon volume and signal intensity
on MRI.
43
A programme of eccentric exercise affects type I
collagen production and, in the absence of ongoing insult, may
increase the tendon volume over the longer term.
44
As such, an
eccentric exercise programme may increase tensile strength in
the tendon over time. The effect of repetitive stretching, with a
lengthening of the muscletendon unit, may also have an
impact on capacity of the musculotendinous unit to effectively
absorb load.
Another possible mechanism of action relates to mechanical
insult of the pain-producing nerves. A unique feature of
Alfredsons eccentric training programme is that the patient is
encouraged to undertake painful heel-drop exercises. As the
nerve structures found in painful human tendons lie in close
proximity to the tendon vessels, and as these vessels disappear
with muscle contraction and stretch, the good clinical effects
demonstrated with eccentric training could be due to alteration
of the neovascularisation and accompanying nerves. The
number of repetitions (180 repetitions/day) may damage the
vessels and accompanying nerves as they traverse the soft tissue
outside the tendon into the dense tendinosis tissue. The finding
that patients satisfied with the result of the eccentric training
regimen had no neovascularisation remaining, and all patients
with a poor clinical result continued to have neovascularisa-
tion,
39
is consistent with this hypothesis. However, that
observation could also be the result of other upstream stimuli
that influence both pain and neovascular obliteration, so we are
not in a position to draw causal conclusions from an
observational study.
Topi cal gl yceryl tri ni t rat e
This substance has been investigated in randomised controlled
trials in the Achilles, elbow and supraspinatus tendons as an
adjunct to an eccentric exercise programme. The topical glyceryl
Figure 1 Algorithm for treating Achilles
tendinopathy. Timeframes are recommended
and should be modified as appropriate for
individual presentations. CSI, corticosteroid
injection; ESWT, extracorporeal shock wave
therapy; GTN, topical glyceryl trinitrate.
Clinical management of Achilles tendinopathy 213
www.bjsportmed.com
trinitrate was applied to the tendon as a patch that was
renewed each day for 6 months. The treatment was compared
with a placebo patch, and pain and function were measured
over 6 months. In the Achilles tendon, activity pain in the
treatment group was reduced at 12 and 24 weeks compared
with placebo, and it also improved outcomes at 6 months.
45
This study also supports the use of an eccentric exercise
programme, as 49% of the placebo group reported excellent
outcomes.
Ext racorporeal shock wave therapy
Although extracorporeal shock wave therapy has been trialled
in several tendons and fascial structures, there have been no
randomised controlled trials in the Achilles tendon.
46
In other
structures, extracorporeal shock wave therapy decreases pain
compared with a placebo,
47
and may be beneficial in relieving
pain, while rehabilitation of the musculotendinous structures
continues.
Corti costeroi d i nj ecti on
In other tendons, corticosteroid injection (CSI) appears to have
short-term pain-relieving effects but no effect or detrimental
effects in the longer term.
48
The short-term effect of CSI has
been shown in the Achilles tendon with improvement in
walking pain and reduction in tendon diameter as measured by
ultrasonography.
49
Intratendinous injection is contraindicated
because of the catabolic effects,
50
although a recent study of CSI
into intratendinous vessels in six tendons has shown promising
results.
51
Peritendinous injection has fewer effects on the
tendon and could be a worthwhile adjunct to a considered
management programme.
50
CSI may be most beneficial when
used to relieve pain while continuing to undertake exercise
programmes.
El ect rophysi cal agent s
The role of electrophysical agents in the treatment of tendino-
pathy remains poorly investigated in humans. Therapeutic
ultrasound increases protein synthesis in tendons,
52
but there is
an oversupply of poor-quality protein in tendons suffering from
overuse, so it may not improve clinical outcome to further
increase protein production.
A recent randomised trial compared the outcome after
hyperthermia with low-frequency microwave to traditional
ultrasound.
53
Significantly better outcomes were recorded by
the hyperthermia group after treatment and 1 month later.
Microcurrent applied for 2 weeks has been shown to decrease
pain at 12 months when compared with conventional treat-
ment.
54
Other treat ment s
A night splint has been shown to be an effective intervention
for Achilles tendinopathy.
37
A greater reduction in pain was
seen when the night splint was combined with a 12-week
eccentric exercise programme. In both cases, when used alone
and in conjunction with the eccentric exercise, a night splint
reduced pain for 12 months.
37
Biomechanical evaluation of the foot and leg is a clinically
important part of Achilles tendon management. Although there
is little empirical evidence to support the association between
foot posture and Achilles tendinopathy,
55
modification of foot
posture in some patients can reduce pain and increase the
capacity to load the tendon.
56
Similarly, massage of the calf complex can assist rehabilita-
tion, as can tendon mobilisation.
57
Frictions have been shown
to increase protein output of tendon cells;
58
however, similar to
the effect seen with ultrasonography, greater amounts of
collagen and ground substance may not alter pain or pathology
in a positive manner.
Scl erosi ng i nj ecti ons
The role of the neovascularisation in tendon pain has been
further examined in a pilot study where a vascular sclerosant
(Polidocanolan aliphatic non-ionised nitrogen-free substance
with a sclerosing and anaesthetic effect) was injected in the
area with neovascularisation anterior to the tendon. Short-term
(6 months) evaluation of this treatment showed that 8 of 10
tendons were pain free after a mean of two treatments.
59
The
tendons that were pain free had no neovascularisation either on
the outside or the inside, but in the two non-successfully
treated patients, vessels remained. A 2-year follow-up (our
unpublished data) of these patients showed that the same eight
patients remained pain free with no vessels in the tendon.
Ultrasonographically, tendon thickness had decreased and the
structure looked more normal. As vessel number has been
shown to correlate with tendon thickness,
23
treatment that
decreases vessel number is also likely to affect tendon
thickness.
In a double-blind, randomised controlled study comparing
the effects of injections of a sclerosing and a non-sclerosing
substance (lidocaine + epinephrine), the sclerosing substance
was clearly more effective.
60
The rehabilitation after sclerosing injection treatment
includes a period of rest (13 days), then gradually increased
tendon-loading activity, but no maximum loading (jumping,
fast runs, heavy strength training) during the first 2 weeks.
After 2 weeks, maximal tendon loading is allowed. After
treating 400 Achilles tendons, we have had two complications
that may be related to treatment. One patient who was treated
in the Achilles tendon insertion sustained a total rupture in the
proximal part of the tendon at the end of an 800 m track race
8 weeks after the treatment. Another patient who was treated
in the mid-portion sustained a partial rupture in an area where
he previously had four intratendinous CSIs. There have been no
other complications. This research suggests a clinical role for
sclerosing therapy in those who fail to respond to eccentric
exercise.
SURGI CAL TREATMENT
Surgical treatment for tendons that fail to respond to
conservative treatment can involve several procedures, all of
which are designed to irritate the tendon and initiate a
chemically mediated healing response. These procedures range
from more simple procedures such as percutaneous tenotomy
61
to open procedures and removal of tendon pathology.
Percutaneous tenotomy resulted in 75% of patients reporting
good or excellent results after 18 months. Open surgery for
Achilles tendinopathy has shown that the outcomes are
better for those tendons without a focal lesion compared
with those with a focal area of tendinopathy.
62
At 7 months
What t hi s study adds
N
A review of treatment options for Achilles tendinopathy
N
Suggested timeframes and sequential treatment strategies
for resistant Achilles tendinopathy
What i s al ready known about thi s topi c
N
There are many conservative and surgical treatment
options for Achilles tendinopathy
N
When and how to progress with treatment for recalcitrant
Achilles tendinopathy can be a difficult clinical decision
214 Alfredson, Cook
www.bjsportmed.com
after surgery, 67% had returned to physical activity, 88% from
the no-lesion group and 50% from the group with a focal
lesion.
Achilles tendon surgery requires extensive post-surgical
rehabilitation and the results after surgery may only be as
good as the strength and functional capacity that is regained.
Adequate attention to rehabilitation is likely to improve
outcomes for those who are surgically treated.
CONCLUSI ON
Achilles tendinopathy is a condition that can be effectively
treated by the primary care practitioner. There are many
simple and easily applied conservative treatment options that
can relieve most tendon pain. Most of those who fail to res-
pond to conservative care will find relief from surgical
treatment.
Authors affiliations
. . . . . . . . . . . . . . . . . . . . . . .
Hakan Alfredson, Sports Medicine Unit, Department of Surgical and
Perioperative Science, Umea University, Umea, Sweden
J Cook, Musculoskeletal Research Centre, La Trobe University, Bundoora,
Victoria, Australia
Competing interests: None declared.
Accepted 22 January 2007
Published Online First 20 February 2007
REFERENCES
1 Maffulli N, Khan KM, Puddu G. Overuse tendon conditions. Time to change a
confusing terminology. Arthroscopy 1998;14:8403.
2 Alfredson H, Lorentzon R. Chronic Achilles tendinosis: recommendations for
treatment and prevention. Sports Med 2000;29:13546.
3 Archambault JM, Wiley JP, Bray RC. Exercise loading of tendons and the
development of overuse injuries. A review of the current literature. Sports Med
1995;20:7789.
4 Astrom M. Partial rupture in Achilles tendinopathy. A retrospective analysis of
342 cases. Acta Orthop Scand 1998;69:4047.
5 Cook JL, Khan KM, Harcourt PR, et al. Patellar tendon ultrasonography in
asymptomatic active athletes reveals hypoechoic regions: a study of 320 tendons.
Clin J Sports Med 1998;8:737.
6 Alfredson H, Forsgren S, Thorsen K, et al. Glutamate NMDAR1 receptors
localised to nerves in human Achilles tendons. Implications for treatment? Knee
Surg Sports Traumatol Arthrosc 2000;9:1236.
7 Alfredson H, Thorsen K, Lorentzon R. In situ microdialysis in tendon tissue: high
levels of glutamate, but not protoglandin E
2
in chronic Achilles tendon pain. Knee
Surg Sports Traumatol Arthrosc 1999;7:37881.
8 Alfredson H, Lorentzon M, Backman S, et al. cDNA-arrays and real-time
quantitative PCR techniques in the investigation of chronic Achilles tendinosis.
J Orthop Res 2003;21:9705.
9 Hart DA, Frank CB, Bray RC. Inflammatory processes in repetitive motion and
overuse syndromes: potential role of neurogenic mechanisms in tendons and
ligaments. In: Gordon SL, Blair SJ, Fine LJ, eds. Repetitive motion disorders of the
upper extremity. Rosemont, IL: American Academy of Orthopaedic Surgeons,
1995:24762.
10 Scott A, Khan KM, Cook JL, et al. What do we mean by the term
inflammation? A contemporary basic science update for sports medicine.
Br J Sports Med 2004;38:37280.
11 Alfredson H, Forsgren S, Thorsen K, et al. In vivo microdialysis and
immunohistochemical analyses of tendon tissue demonstrated high amounts of
free glutamate and glutamate receptors, but no signs of inflammation, in
Jumpers knee. J Orthop Res 2001;19:8816.
12 Bjur D, Alfredson H, Forsgren S. The innervation pattern of the human Achilles
tendon: studies of the normal and tendinosis tendon with markers for general and
sensory innervation. Cell Tissue Res 2005;320:2016.
13 Ljung B, Alfredson H, Forsgren S. Neurokinin 1-receptors and sensory
neuropeptides in tendon insertions at the medial and lateral epicondyles of the
humerus. Studies on tennis elbow ad medial epicondylalgia. J Orthop Res
2004;22:3217.
14 Forsgren S, Danielsson S, Alfredson H. Vascular NK-1R receptor occurrence in
normal and chronic painful Achilles and patellar tendons. Studies on chemically
unfixed as well as fixed specimens. Regul Pept 2005;126:17381.
15 Campbell RSD, Grainger AJ. Current concepts in imaging in tendinopathy. Clin
Radiol 2001;56:25367.
16 Maffulli N. The clinical diagnosis of subcutaneous tear of the Achilles tendon. A
prospective study in 174 patients. Am J Sports Med 1998;26:26670.
17 Khan KM, Bonar F, Desmond PM, et al. Patellar tendinosis (jumpers knee):
findings at histopathologic examination, US and MR imaging. Radiology
1996;200:8217.
18 Movin T, Kristoffersen-Wiberg M, Shalabi A, et al. Intratendinous alterations as
imaged by ultrasound and contrast medium-enhanced magnetic resonance in
chronic achillodynia. Foot Ankle Int 1998;19:31117.
19 Khan KM, Forster BB, Robinson J, Cheong Y, Louis L, MacLean L, et al. Are
ultrasound and magnetic resonance imaging of value in assessment of Achilles
tendon disorders? A two-year prospective study. Br J Sports Med
2003;37:14954.
20 Paavola M, Paakkala T, Kannus P, et al. Untrasonography in the differential
diagnosis of Achilles tendon injuries and related disorders. Acta Radiol
1998;39:61219.
21 Ohberg L, Lorentzon R, Alfredson H. Neovascularisation in Achilles tendons with
painful tendinosis but not in normal tendons: an ultrasonographic investigation.
Knee Surg Sports Traumatol Arthrosc 2001;9:2338.
22 Peers K, Brys P, Lysens R. Correlation between power Doppler
ultrasonography and clinical severity in Achilles tendinopathy. Int Orthop
2003;27:1803.
23 Richards P, Win T, Jones P. The distribution of microvascular response in Achilles
tendonopathy assessed by colour and power Doppler. Skeletal Radiol
2005;34:33642.
24 Zanetti M, Metzdorf A, Kundert H-P, et al. Achilles tendons: clinical relevance of
neovascularization diagnosed with power Doppler US. Radiology
2003;227:55660.
25 Cook JL, Khan KM, Kiss ZS, et al. Asymptomatic hypoechoic regions on patellar
tendon US do not foreshadow symptoms of jumpers knee: a 4 year followup of
46 tendons. Scand J Sci Med Sports 2000;11:3217.
26 Khan KM, Visentini PJ, Kiss ZS, et al. Correlation of US and MR imaging with
clinical outcome after open patellar tenotomy: prospective and retrospective
studies. Clin J Sport Med 1999;9:12937.
27 Astrom M, Westlin N. No effect of piroxicam on Achilles tendinopathy. A
randomized study of 70 patients. Acta Orthop Scand 1992;63:6314.
28 Almekinders L, Temple J. Etiology, diagnosis, and treatment of tendonitis: an
analysis of the literature. Med Sci Sports Exerc 1998;30:118390.
29 Kannus P. Tendon pathology: basic science and clinical applications. Sports
Exerc Inj 1997;3:6275.
30 Kader D, Saxena A, Movin T, et al. Achilles tendinopathy: some aspects of basic
science and clinical management. Br J Sports Med 2002;36:23949.
31 Paavola M, Kannus P, Paakkala T, et al. Long-term prognosis of patients with
Achilles tendinopathy. An observational 8-year follow-up study. Am J Sports
Med 2000;28:63442.
32 Kvist M. Achilles tendon injuries in athletes. Sports Med 1994;18:173201.
33 Curwin S. The aetiology and treatment of tendinitis. In: Harries M, Williams C,
Stanish WD, Micheli LJ, eds. Oxford textbook of sports medicine. Oxford:
Oxford University Press, 1994.
34 Curwin S, Stanish WD. Tendinitis: its etiology and treatment. Lexington:
Collamore Press, 1984.
35 Alfredson H, Pietila T, Jonsson P, et al. Heavy-load eccentric calf muscle training
for the treatment of chronic Achilles tendinosis. Am J Sports Med
1998;26:3606.
36 Fahlstrom M, Jonsson P, Lorentzon R, et al. Chronic Achilles tendon pain treated
with eccentric calf-muscle training. Knee Surg Sports Traumatol Arthrosc
2003;11:32733.
37 Roos E, Engstrom M, Lagerquist A, et al. Clinical improvement after 6 weeks of
eccentric exercise in patients with mid-portion Achilles tendinopathy: a
randomized trial with 1-year follow-up. Scand J Med Sci Sports
2004;14:28695.
38 Fahlstrom M. Badminton and the Achilles tendon [PhD thesis]. Umea, Umea
University, 2001.
39 Ohberg L, Lorentzon R, Alfredson H. Eccentric training in patients with chronic
Achilles tendinosis: normalised tendon structure and decreased thickness at
follow up. Br J Sports Med 2004;38:811.
40 Shalabi A, Kristoffersen-Wilberg M, Svensson L, et al. Eccentric training of the
gastrocnemius-soleus complex in chronic Achilles tendinopathy results in
decreased tendon volume and intratendinous signal as evaluated by MRI.
Am J Sports Med 2004;32:128696.
41 Silbernagel K, Thomee R, Thomee P, et al. Eccentric overload training for patients
with chroinic Achilles tendon paina randomised testing of the evaluation
methods. Scand J Med Sci Sports 2001;11:197206.
42 Mafi N, Lorentzon R, Alfredson H. Superior short-term results with eccentric calf
muscle training compared to concentric training in a randomized prospective
multicenter study on patients with chronic Achilles tendinosis. Knee Surg Sports
Traumatol Arthrosc 2001;9:427.
43 Shalabi A, Kristoffersen-Wiberg M, Aspelin P, et al. Immediate Achilles tendon
response after strength training evaluated by MRI. Med Sci Sports Exerc
2004;36:18416.
44 Kjaer M, langberg H, Miller B, et al. Metabolic activity and colagen turnover in
human tendon in response to physical activity. J Musculoskelet Neuronal Interact
2005;5:4152.
45 Paoloni J, Appleyard R, Nelson J, et al. Topical glyceryl trinitrate treatment of
chronic noninsertional Achilles tendinopathy. J Bone Joint Surg 2004;86-
A:91621.
46 Lakshmanan P, ODoherty D. Chronic achilles tendinopathy: treatment with
extracorporeal shock waves. Foot Ankle Surg 2004;10:12530.
47 Chung B, Wiley J. Extracorporeal shockwave therapy. Sports Med
2002;32:85165.
48 Smidt N, Windt Dvd, Assendelft W, et al. Corticosteroid injections,
physiotherapy, or wait-and-see policy for lateral epicondylitis: a randomised
controlled trial. Lancet 2002;359:65762.
49 Fredberg U, Bolvig L, Pfeiffer-Jensen M, et al. Ultrasonography as a tool for
diagnosis, guidance of local steroid injection and, tigether with pressure
Clinical management of Achilles tendinopathy 215
www.bjsportmed.com
algometry, monitoring of the treatment of athletes with chromic jumpers knee
and Achilles tendinitis: a randomized double-blind, placebo-controlled trial.
Scand J Rheumatol 2004;33:94101.
50 Shrier I, Matheson G, Kohl G. Achilles tendinitis: are corticosteroid injections
useful or harmful? Clin J Sport Med 1996;6:24550.
51 Koenig MJ, Torp-pedersen S, Qvistgaard E, et al. Preliminary results of colour
Doppler-guided intratendinous glucocorticoid injection for Achilles tendonitis in
five patients. Scand J Med Sci Sports 2004;14:100.
52 Parvizi J, Wu C-C, Lewallen D, et al. Low-intensity ultrasound stimulates
proteoglycan syntyhesis in rat chondrocytes by increasing aggregcan gene
expression. J Orthop Res 1999;17:48894.
53 Giombini A, Cesare AD, Casciello G, et al. Hyperthermia at 434 MHz in the
treatment of overuse sport tendinopathies: a randomised controlled clinical trial.
Int J Sports Med 2002;23:20711.
54 Chapman-Jones D, Hill D. Novel microcurrent treatment is more effective than
conventional therapy for chronic Achilles tendinopathy. Physiotherapy
2002;88:4719.
55 Astrom M. On the nature and etiology of chronic Achilles tendinopathy [PhD
thesis]. Sweden, Lund University, 1997.
56 McCrory J, Martin D, Lowery R, et al. Etiologic factors associated with Achilles
tendinitis in runners. Med Sci Sports Exerc 1999;31:137481.
57 Hunter G. The conservative management of Achilles tendinopathy. Phys Ther
Sport 2000;1:614.
58 Davidson C, Ganion LR, Gehlsen G, et al. Rat tendon morphological and
functional changes resulting from soft tissue mobilization. Med Sci Sports Exerc
1997;29:31319.
59 Ohberg L, Alfredson H. Ultrasound guided sclerosis of neovessels in painful
chronic Achilles tendinosis: pilot study of a new treatment. Br J Sports Med
2002;36:1737.
60 Alfredson H, Ohberg L. Sclerosing injections to areas of neovascularisation
reduce pain in chronic Achilles tendinopathy: a double-blind randomised
controlled trial. Knee Surg Sports Traumatol Arthrosc 2005;13:33844.
61 Testa V, Capasso G, Maffulli N, et al. Ultrasound guided percutaneous
longitudinal tenotomy for the management of patellar tendinopathy. Med Sci
Sports Exerc 1999;31:150915.
62 Paavola M, Kannus P, Orava S, et al. Surgical treatment for chronic Achiles
tendinopathy: a prospective seven month follow up study. Br J Sports Med
2002;36:17882.
BMJ Clinical EvidenceCall for contributors
BMJ Clinical Evidence is a continuously updated evidence-based journal available worldwide on
the internet which publishes commissioned systematic reviews. BMJ Clinical Evidence needs to
recruit new contributors. Contributors are healthcare professionals or epidemiologists with
experience in evidence-based medicine, with the ability to write in a concise and structured way
and relevant clinical expertise.
Areas for which we are currently seeking contributors:
N
Secondary prevention of ischaemic cardiac events
N
Acute myocardial infarction
N
MRSA (treatment)
N
Bacterial conjunctivitis
However, we are always looking for contributors, so do not let this list discourage you.
Being a contributor involves:
N
Selecting from a validated, screened search (performed by in-house Information Specialists)
valid studies for inclusion.
N
Documenting your decisions about which studies to include on an inclusion and exclusion form,
which we will publish.
N
Writing the text to a highly structured template (about 15003000 words), using evidence from
the final studies chosen, within 810 weeks of receiving the literature search.
N
Working with BMJ Clinical Evidence editors to ensure that the final text meets quality and style
standards.
N
Updating the text every 12 months using any new, sound evidence that becomes available. The
BMJ Clinical Evidence in-house team will conduct the searches for contributors; your task is to
filter out high quality studies and incorporate them into the existing text.
N
To expand the review to include a new question about once every 12 months.
In return, contributors will see their work published in a highly-rewarded peer-reviewed
international medical journal. They also receive a small honorarium for their efforts.
If you would like to become a contributor for BMJ Clinical Evidence or require more information
about what this involves please send your contact details and a copy of your CV, clearly stating the
clinical area you are interested in, to CECommissioning@bmjgroup.com.
Call for peer reviewers
BMJ Clinical Evidence also needs to recruit new peer reviewers specifically with an interest in the
clinical areas stated above, and also others related to general practice. Peer reviewers are
healthcare professionals or epidemiologists with experience in evidence-based medicine. As a
peer reviewer you would be asked for your views on the clinical relevance, validity and
accessibility of specific reviews within the journal, and their usefulness to the intended audience
(international generalists and healthcare professionals, possibly with limited statistical knowledge).
Reviews are usually 15003000 words in length and we would ask you to review between 25
systematic reviews per year. The peer review process takes place throughout the year, and our
turnaround time for each review is 1014 days. In return peer reviewers receive free access to
BMJ Clinical Evidence for 3 months for each review.
If you are interested in becoming a peer reviewer for BMJ Clinical Evidence, please complete the
peer review questionnaire at www.clinicalevidence.com/ceweb/contribute/peerreviewer.jsp
216 Alfredson, Cook
www.bjsportmed.com
You might also like
- Anterior Knee Pain in The Young AthleteDocument7 pagesAnterior Knee Pain in The Young AthleteAngelica GarciaNo ratings yet
- Advanced Ultrasound-Guided Interventions For TenopathyDocument16 pagesAdvanced Ultrasound-Guided Interventions For TenopathyJuanMa Correa SanabriaNo ratings yet
- Tendinopathy GuidelinesDocument26 pagesTendinopathy GuidelinesArdis CaniNo ratings yet
- Charcot Shoulder and Elbow A Review of The LiteratureDocument9 pagesCharcot Shoulder and Elbow A Review of The Literatureoriana.perezgibsontpNo ratings yet
- Lumbar Disk HerniationDocument6 pagesLumbar Disk HerniationSyarifah Nadya ArfadNo ratings yet
- Entrapmentneuropathiesof Theupperextremity: Christopher T. Doughty,, Michael P. BowleyDocument14 pagesEntrapmentneuropathiesof Theupperextremity: Christopher T. Doughty,, Michael P. BowleydwiNo ratings yet
- Pain Practice - 2024 - Vanneste - 9 Chronic Knee PainDocument21 pagesPain Practice - 2024 - Vanneste - 9 Chronic Knee PainfernandomurcianoNo ratings yet
- Ankylosing Spondylitis BMJ RevDocument5 pagesAnkylosing Spondylitis BMJ RevsamarqandiNo ratings yet
- Shoulder 2 Ada MriDocument4 pagesShoulder 2 Ada MriNirmalasari AnirNo ratings yet
- Pan 1Document3 pagesPan 1Mithun CbNo ratings yet
- "Idiopathic" Shoulder Pain and Dysfunction From Carpal Tunnel Syndrome and Cubital Tunnel Syndrome - PMCDocument13 pages"Idiopathic" Shoulder Pain and Dysfunction From Carpal Tunnel Syndrome and Cubital Tunnel Syndrome - PMCArghya DebNo ratings yet
- Ultrasound-Guided Peripheral Nerve Stimulation For Shoulder Pain: Anatomic Review and Assessment of The Current Clinical EvidenceDocument14 pagesUltrasound-Guided Peripheral Nerve Stimulation For Shoulder Pain: Anatomic Review and Assessment of The Current Clinical EvidencefernandomurcianoNo ratings yet
- Ijspt 12 1150 IliopsoasDocument13 pagesIjspt 12 1150 Iliopsoasnikhilmascarenhas07No ratings yet
- Differential Diagnosis of Cervicobrachial PainDocument11 pagesDifferential Diagnosis of Cervicobrachial PainpuchioNo ratings yet
- Genicular Nerve Ablation Zeitlinger2019Document7 pagesGenicular Nerve Ablation Zeitlinger2019drjorgewtorresNo ratings yet
- Diagnosis and Treatment of Sciatica: Data SupplementDocument12 pagesDiagnosis and Treatment of Sciatica: Data SupplementAstie NomleniNo ratings yet
- Achilles TendinopathyDocument42 pagesAchilles TendinopathyAlberto GallariniNo ratings yet
- Uso de Ultrasonografia para Medial EpycondilitisDocument5 pagesUso de Ultrasonografia para Medial EpycondilitisSantiago BianchiNo ratings yet
- DN For Tumb PainDocument11 pagesDN For Tumb PainAgeng RestiNo ratings yet
- 709 1357 1 PBDocument13 pages709 1357 1 PBTri NoviantyNo ratings yet
- 2014 The Pain of Tendinopathy - Physiological or PathophysiologicalDocument15 pages2014 The Pain of Tendinopathy - Physiological or PathophysiologicalDavid Alejandro Cavieres AcuñaNo ratings yet
- Percutaneous Imaging-Guided Spinal Facet Joint InjectionsDocument6 pagesPercutaneous Imaging-Guided Spinal Facet Joint InjectionsAlvaro Perez HenriquezNo ratings yet
- Amit Murli Patel. Physical Therapy Management of Tuberculous Arthritis of The Elbow SRJI Vol - 2, Issue - 1, Year - 2013Document10 pagesAmit Murli Patel. Physical Therapy Management of Tuberculous Arthritis of The Elbow SRJI Vol - 2, Issue - 1, Year - 2013Dr. Krishna N. SharmaNo ratings yet
- 1 s2.0 S1297319X21002062 MainDocument7 pages1 s2.0 S1297319X21002062 Mainabood softNo ratings yet
- Regional AnalgesiaDocument5 pagesRegional AnalgesiajdjhdNo ratings yet
- Treatment of Gluteal Tendinopathy A Systematic Review and Stage-Adjusted Treatment RecommendationDocument12 pagesTreatment of Gluteal Tendinopathy A Systematic Review and Stage-Adjusted Treatment RecommendationDeivisonNo ratings yet
- Patellar Tendinopathy: Recent Developments Toward TreatmentDocument8 pagesPatellar Tendinopathy: Recent Developments Toward TreatmentVictor Andrés Olivares IbarraNo ratings yet
- Ni Hms 825760Document13 pagesNi Hms 825760Dea MustikaNo ratings yet
- Important MCQs Rheumatology2Document7 pagesImportant MCQs Rheumatology2little luluNo ratings yet
- Tendinopatía BarçaDocument26 pagesTendinopatía BarçaPAcoNo ratings yet
- Pain Practice - 2022 - Desai - Cluneal Neuropathy Background Diagnosis and TreatmentDocument10 pagesPain Practice - 2022 - Desai - Cluneal Neuropathy Background Diagnosis and TreatmentfernandomurcianoNo ratings yet
- Durerea Vertebrogenă PUBMEDDocument4 pagesDurerea Vertebrogenă PUBMEDIulia MoldovanNo ratings yet
- AnnRheumDis 2011 Beaudreuil 1613 8Document8 pagesAnnRheumDis 2011 Beaudreuil 1613 8Gabriel HenriqueNo ratings yet
- Transient SynovitisDocument9 pagesTransient SynovitisMuhammad Taufik AdhyatmaNo ratings yet
- Physiotherapy Management of SciaticaDocument6 pagesPhysiotherapy Management of SciaticaMuly Arafah ZakariaNo ratings yet
- Nerve Entrapment - UpdateDocument17 pagesNerve Entrapment - UpdatealobrienNo ratings yet
- Neurosurg Focus Article PE13Document15 pagesNeurosurg Focus Article PE13Bunga AlifatulNo ratings yet
- Pubalgia 1Document11 pagesPubalgia 1Carlos Alberto Mac-kay VillagranNo ratings yet
- June2008-RR-WoodleyDocument16 pagesJune2008-RR-WoodleyjacknatalieNo ratings yet
- Guided Interventions in Musculoskeletal UltrasoundDocument13 pagesGuided Interventions in Musculoskeletal UltrasoundomboNo ratings yet
- Pain Mechanism Classification Clinical Pearl Part 3Document5 pagesPain Mechanism Classification Clinical Pearl Part 3AlexsanderNo ratings yet
- Tennis Elbow 2003 PDFDocument4 pagesTennis Elbow 2003 PDFDiegoKosiakNo ratings yet
- Neurology - Research & Surgery: ISSN 2641-4333 Review ArticleDocument11 pagesNeurology - Research & Surgery: ISSN 2641-4333 Review ArticleScivision PublishersNo ratings yet
- 2017 Article 9386 TendinitisDocument9 pages2017 Article 9386 TendinitisKirana lupitaNo ratings yet
- Joint Denervation and Neurogenic InflammationDocument44 pagesJoint Denervation and Neurogenic InflammationHand SurgeryNo ratings yet
- Cureus 0012 00000008747Document8 pagesCureus 0012 00000008747Gustavo FredericoNo ratings yet
- Osteoarthritis in Older PeopleDocument22 pagesOsteoarthritis in Older PeoplenfacmaNo ratings yet
- Overuse Tendinosis, Not Tendinitis: Part 1: A New Paradigm For A Difficult Clinical ProblemDocument10 pagesOveruse Tendinosis, Not Tendinitis: Part 1: A New Paradigm For A Difficult Clinical ProblemTony100% (4)
- 2018-Bugada-Update On Selective Regional Analgesia For Hip Surgery PatientsDocument13 pages2018-Bugada-Update On Selective Regional Analgesia For Hip Surgery PatientsDr LAUMONERIENo ratings yet
- Exercise-Associated Numbness and Tingling in The Legs: For Editorial Comment See Page 1509Document4 pagesExercise-Associated Numbness and Tingling in The Legs: For Editorial Comment See Page 1509herpthederpNo ratings yet
- Pain Practice - 2023 - Gish - Neuromodulation For The Management of Chronic Pelvic Pain Syndromes A Systematic ReviewDocument20 pagesPain Practice - 2023 - Gish - Neuromodulation For The Management of Chronic Pelvic Pain Syndromes A Systematic ReviewfernandomurcianoNo ratings yet
- Growth and Regeneration of Intervertebral Discs byDocument22 pagesGrowth and Regeneration of Intervertebral Discs byenglish-exactlyNo ratings yet
- Trsum4: Interventional ForDocument5 pagesTrsum4: Interventional ForauliaNo ratings yet
- Herniated Nucleus Pulposus TreatmentDocument19 pagesHerniated Nucleus Pulposus Treatmentvicky174No ratings yet
- Bi Syndrome of The Knee Treated With Acupuncture With Patellofemoral Pain Syndrome As A CaseDocument4 pagesBi Syndrome of The Knee Treated With Acupuncture With Patellofemoral Pain Syndrome As A CaseInfohoggNo ratings yet
- Surgery For Degenerative Lumbar Spondylosis: Updated Cochrane ReviewDocument9 pagesSurgery For Degenerative Lumbar Spondylosis: Updated Cochrane Reviewchartreuse avonleaNo ratings yet
- Ultrasound and clinically guided Injection techniques on the musculoskeletal systemFrom EverandUltrasound and clinically guided Injection techniques on the musculoskeletal systemNo ratings yet
- Small Fiber Neuropathy and Related Syndromes: Pain and NeurodegenerationFrom EverandSmall Fiber Neuropathy and Related Syndromes: Pain and NeurodegenerationSung-Tsang HsiehNo ratings yet
- Pain Imaging: A Clinical-Radiological Approach to Pain DiagnosisFrom EverandPain Imaging: A Clinical-Radiological Approach to Pain DiagnosisMaria Assunta CovaNo ratings yet
- Advances in Intervertebral Disc Disease in Dogs and CatsFrom EverandAdvances in Intervertebral Disc Disease in Dogs and CatsJames FingerothNo ratings yet
- Implementation of The KDIGO Guideline On The Management of The Kidney Transplant Recipient in The UK 2010Document5 pagesImplementation of The KDIGO Guideline On The Management of The Kidney Transplant Recipient in The UK 2010ppeterarmstrongNo ratings yet
- Guide For Clinical Audit Leads 21 Mar 11Document40 pagesGuide For Clinical Audit Leads 21 Mar 11ppeterarmstrongNo ratings yet
- HbA1c Person Leaflet 0509Document2 pagesHbA1c Person Leaflet 0509ppeterarmstrongNo ratings yet
- RSscan BrochureDocument6 pagesRSscan BrochureppeterarmstrongNo ratings yet
- HbA1c Lab Leaflet 0509Document2 pagesHbA1c Lab Leaflet 0509ppeterarmstrongNo ratings yet
- Orthopedics Standard of Care GuidelinesDocument543 pagesOrthopedics Standard of Care GuidelinesppeterarmstrongNo ratings yet
- Guidelines For Preventing HealthcareDocument78 pagesGuidelines For Preventing HealthcareppeterarmstrongNo ratings yet
- Criteria For Progressing Rehabilitation and Determining Return-to-Play Clearance Following Hamstring Strain Injury: A Systematic ReviewDocument13 pagesCriteria For Progressing Rehabilitation and Determining Return-to-Play Clearance Following Hamstring Strain Injury: A Systematic ReviewRaúl GonzálezNo ratings yet
- Patellar Tendinopathy in Team Sports Preventive.4Document11 pagesPatellar Tendinopathy in Team Sports Preventive.4Martiniano Vera EnriqueNo ratings yet
- Heavy-Load Eccentric Calf Muscle Training For The Treatment of Chronic Achilles TendinosisDocument8 pagesHeavy-Load Eccentric Calf Muscle Training For The Treatment of Chronic Achilles TendinosisburgoschileNo ratings yet
- Analysis of The Aerial and Landing Phases of The Grand JeteDocument5 pagesAnalysis of The Aerial and Landing Phases of The Grand Jetesofia.spicbuksNo ratings yet
- The 4+2 Advanced Muscle-Building Method Delivers Superior GainsDocument11 pagesThe 4+2 Advanced Muscle-Building Method Delivers Superior GainsAlexandre ReisNo ratings yet
- Isometric Exercise (Static Exercise)Document18 pagesIsometric Exercise (Static Exercise)venkata ramakrishnaiah100% (3)
- Eccentric Strength Training: A Review of The Available TechnologyDocument16 pagesEccentric Strength Training: A Review of The Available TechnologyelmismoNo ratings yet
- Michael 2020Document13 pagesMichael 2020Matheus RenyerNo ratings yet
- Chris Beardsley - Strength Is Specific v2Document186 pagesChris Beardsley - Strength Is Specific v2pflucho100% (3)
- European J App Phys - Effectiveness of Using Wearable Vibration Therapy T PDFDocument9 pagesEuropean J App Phys - Effectiveness of Using Wearable Vibration Therapy T PDFFrancisco Javier Medina CaballeroNo ratings yet
- Advanced Strength and Power Training For The Elite.8Document7 pagesAdvanced Strength and Power Training For The Elite.8federicoNo ratings yet
- Five Steps in TrainingDocument14 pagesFive Steps in TrainingIvan Kulev100% (1)
- Step Into Life Berwick Fresh Air April HOF 2013Document10 pagesStep Into Life Berwick Fresh Air April HOF 2013Marko RadisicNo ratings yet
- 1080 White Paper Dowload Email 1Document16 pages1080 White Paper Dowload Email 1壮No ratings yet
- Protocol Hamstring Lengthened Eccentric Training 15214 PDFDocument9 pagesProtocol Hamstring Lengthened Eccentric Training 15214 PDFkang soon cheolNo ratings yet
- Petersen, J. (2011) Preventive Effect of Eccentric Training On Acute Hamstring Injuries in Mens SoccerDocument1 pagePetersen, J. (2011) Preventive Effect of Eccentric Training On Acute Hamstring Injuries in Mens SoccerMarko BrzakNo ratings yet
- Free Cali Blueprint EbookDocument18 pagesFree Cali Blueprint EbookmohammadarhabfirozNo ratings yet
- MixedFiber Phase2 CS Week7 12Document33 pagesMixedFiber Phase2 CS Week7 12Melina HidalgoNo ratings yet
- MSK2 Rotator Cuff Tendinopathy RX TableDocument2 pagesMSK2 Rotator Cuff Tendinopathy RX Tablepp ssNo ratings yet
- Lateral Epicondylitis: A Review of The LiteratureDocument12 pagesLateral Epicondylitis: A Review of The LiteratureAnanta MiaNo ratings yet
- Aspetar: Clinical Practice Guideline On Rehabilitation After ACLRDocument12 pagesAspetar: Clinical Practice Guideline On Rehabilitation After ACLROWL ANASNo ratings yet
- Eccentric TrainingDocument7 pagesEccentric TrainingAbinaya RanganathanNo ratings yet
- Brentano Kruel2011Document11 pagesBrentano Kruel2011merloy84No ratings yet
- A Comparison of The Immediate Effects of Eccentric Training vs. Static Stretch On Hamstring Flexibility in High School and College AthletesDocument6 pagesA Comparison of The Immediate Effects of Eccentric Training vs. Static Stretch On Hamstring Flexibility in High School and College AthletesBryan HuaritaNo ratings yet
- Strength Training For RunnersDocument83 pagesStrength Training For Runnerstarek_g100% (11)
- Supersets and Pre-Exhaustion: Advanced Training PracticesDocument47 pagesSupersets and Pre-Exhaustion: Advanced Training PracticesHamada MansourNo ratings yet
- The Effectiveness of Isometric Contractions Compared With Isotonic Contractions in Reducing Pain For In-Season Athletes With Patellar TendinopathyDocument4 pagesThe Effectiveness of Isometric Contractions Compared With Isotonic Contractions in Reducing Pain For In-Season Athletes With Patellar TendinopathyAlberto Saura RodríguezNo ratings yet
- Chapter 8 - Strength and Power PDFDocument76 pagesChapter 8 - Strength and Power PDFDDVNo ratings yet
- Scientific Basis For Eccentric Quasi Isometric.29Document14 pagesScientific Basis For Eccentric Quasi Isometric.29Yunus YataganNo ratings yet
- Accepted ManuscriptDocument18 pagesAccepted ManuscriptDyah SafitriNo ratings yet