100%(1)100% found this document useful (1 vote)
227 viewsEpi
Epi
Uploaded by
shenric16This document provides information on tuberculosis (TB) including:
1. TB is caused by Mycobacterium tuberculosis and is transmitted through droplet infection. It most commonly affects the lungs but can also affect other organs. Symptoms vary depending on the site of infection.
2. The National TB Control Program in the Philippines aims to reduce TB prevalence and mortality through its DOTS strategy of ensuring accessible and compliant treatment. It has objectives to improve diagnosis and treatment, increase community awareness, and strengthen management of TB services.
3. Treatment involves a combination of anti-TB drugs administered under direct observation. Treatment regimens vary depending on the type and severity of TB case. Strict dosage guidelines are provided based on
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Epi
Epi
Uploaded by
shenric16100%(1)100% found this document useful (1 vote)
227 views10 pagesThis document provides information on tuberculosis (TB) including:
1. TB is caused by Mycobacterium tuberculosis and is transmitted through droplet infection. It most commonly affects the lungs but can also affect other organs. Symptoms vary depending on the site of infection.
2. The National TB Control Program in the Philippines aims to reduce TB prevalence and mortality through its DOTS strategy of ensuring accessible and compliant treatment. It has objectives to improve diagnosis and treatment, increase community awareness, and strengthen management of TB services.
3. Treatment involves a combination of anti-TB drugs administered under direct observation. Treatment regimens vary depending on the type and severity of TB case. Strict dosage guidelines are provided based on
Original Description:
EPI
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
This document provides information on tuberculosis (TB) including:
1. TB is caused by Mycobacterium tuberculosis and is transmitted through droplet infection. It most commonly affects the lungs but can also affect other organs. Symptoms vary depending on the site of infection.
2. The National TB Control Program in the Philippines aims to reduce TB prevalence and mortality through its DOTS strategy of ensuring accessible and compliant treatment. It has objectives to improve diagnosis and treatment, increase community awareness, and strengthen management of TB services.
3. Treatment involves a combination of anti-TB drugs administered under direct observation. Treatment regimens vary depending on the type and severity of TB case. Strict dosage guidelines are provided based on
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
100%(1)100% found this document useful (1 vote)
227 views10 pagesEpi
Epi
Uploaded by
shenric16This document provides information on tuberculosis (TB) including:
1. TB is caused by Mycobacterium tuberculosis and is transmitted through droplet infection. It most commonly affects the lungs but can also affect other organs. Symptoms vary depending on the site of infection.
2. The National TB Control Program in the Philippines aims to reduce TB prevalence and mortality through its DOTS strategy of ensuring accessible and compliant treatment. It has objectives to improve diagnosis and treatment, increase community awareness, and strengthen management of TB services.
3. Treatment involves a combination of anti-TB drugs administered under direct observation. Treatment regimens vary depending on the type and severity of TB case. Strict dosage guidelines are provided based on
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 10
Lecture Notes on EPI Diseases / National TB Control Program (DOTS)
Prepared By: Mark Fredderick R Abejo RR, MAN
Clinical Instructor
1
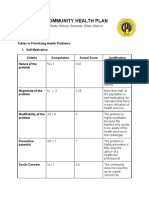
EPI TARGET DISEASES
Disease Causative
Agent
Mode of
Transmission
Clinical
Manifestation
Reservoir Diagnostic
Exam
Treatment Nursing
Implication
Tuberculosis
Primary
Complex is less
than 3 years old
- any child who
does not return to
normal health after
measles or
whooping cough.
Most hazardous
period: first 6-12
months after
infection
Highest in risk
of developing:
under 3 years old
Mycobacterium
Tuberculosis
Droplet Infection
( inhalation of
bacilli from
patient who
coughs and
sneeze)
Degree of
Communicability
Depends upon:
- num.of bacilli
- virulence of
bacilli
- environmental
conditions
General weakness
Loss of weight,
cough and wheeze
which does not
respond to antibiotic
therapy.
Fever and night
sweat
Abdominal swelling
with a hard painless
mass and free fluid
Hemoptysis and
chest pain
Painful firm or soft
swelling in a group of
superficial lymph
nodes.
Note:
In young children the
only sign of pulmonary
TB may be stunted
growth or failure to
thrive
Man
And
Diseased
Cattle
(Bovine TB)
Sputum
Exam
3 sample are
taken with 24
hrs:
- spot sample
(1
st
visit)
- early
morning
specimen
- spot sample
(2
nd
visit)
Note: at least 2
sample are
positive
Chest Xray
Mantoux
Test
- .1 cc
injection of
PDD and 48-
72 hours
reading
* 10 mm +
5 mm + (HIV
pt.)
DOTS
- patient is
required to take
the Ant-Tb
drugs in the
presence of a
health care
provider to
ensure
compliance to
treatment
regimen
Anti-TB drugs:
(RIPES)
Rifampicin
Isoniazid
Pyrazinamide
Ethambutol
Streptomycin
Pointers for
teaching on Anti-
TB drugs:
Rifampicin: taken
befor meals,
causes red urine
urine
Isoniazide: causes
peripheral neuritis,
given with Vit.B6
Pyrazinamide:
cause
hyperurucemia
Ethambutol:
causes optic
neuritis/ blurring
of vision
Streptomycin:
cause tinnitus, loss
of hearing balance,
damage to 8
th
cranial nerve
Note: After 2-4
weeks of
treatment, patient
is no longer
contagious
Lecture Notes on EPI Diseases / National TB Control Program (DOTS)
Prepared By: Mark Fredderick R Abejo RR, MAN
Clinical Instructor
2
The National Tuberculosis Control Program
Vision: A country where Tb is no longer a public health problem
Mission: Ensure that TB DOTS services are available, accessible and
affordable to the communities in collaboration with the LGUs
and other partners
Goal: To reduce prevalence and mortality from TB by half the year
2015 ( Millennium Development Goal )
Targets:
1. Cure at least 85% of the sputum smear- positive TB patient discovered.
2. Detect at least 70% of the estimated new sputum smear-positive TB cases.
NTP Objectives and Strategies
Objective A:
Improve access to and quality of services provided to TB patients, TB
symptomatics and communities by health care institutions and providers
Strategies:
Enhance quality of TB diagnosis.
Ensure TN patients treatment compliance.
Ensure public and private health care providers adherence to the
implementation of national standards of care for TB patients.
Improve access to services through innovative service delivery mechanisms for
patients living in challenging areas.
Objective B:
Enhance the health-seeking behavior on TB by communities, especially
the TB symptomatics
Strategies:
Develop effective, appropriate and culturally-responsive IEC/communication
materials.
Organize barangay advocacy groups
Objective C:
I ncrease and sustain support and financing for TB
control activities
Strategies:
Facilitate implementation of TB-DOTS Center certification and
accreditation
Build TB coalitions among different sectors
Advocate for counterpart input from local government units
Mobilize/extend other resources to address program limitations
Objective D:
Strengthen management (technical and operational) of TB
control services at all levels
Strategies:
Enhance managerial capability of all NTP program managers at all
levels
Establish an efficient data management system for both public and
private sectors.
Implement a standardized recording and reporting system.
Conduct regular monitoring and evaluation at all levels.
Advocate for political support through effective local governance
KEY POLICIES
Case Finding
1. DSSM ( Direct Sputum Smear Microscopy ) shall be the
primary diagnostic tool in NTP case finding.
Note: No TB diagnosis shall be made based on Xray result alone
likewise
result of PDD skin test (Mantoux Test)
2. All TB symptomatic identified shall undergo DSSM for diagnosis
before start of treatment
Note: Only contraindication for sputum collection is hemoptysis
Lecture Notes on EPI Diseases / National TB Control Program (DOTS)
Prepared By: Mark Fredderick R Abejo RR, MAN
Clinical Instructor
3
3. After three sputum specimen yielding negative result X-ray and culture
are necessary
Note: Diagnosis based on Xray shall be made by the TB Diagnostic
Committee.
4. Only trained medical technologist or microscopist shall perform DSSM.
Patients with the following conditions shall be recommended for
hospitalization:
massive hemoptysis
pleural effusion
military TB ( TB of the Spine Pots Disease)
TB meningitis
TB pneumonia
and those requiring surgical intervention
Anti-TB drugs:
(RIPES)
Rifampicin
Isoniazid
Pyrazinamide
Ethambutol
Streptomycin
Two Formulation of Anti-TB Drugs
1. Fixed-Dose Combination ( FDCs) two or more first line anti-TB drugs
are combined in one tablet. There are 2,3, or 4 drug fixed dose
combinations.
2. Single Drug Formulation (SDF) each drug is prepared individually.
Isoniazid, Pyrazinamide and Ethambuto are in tablet form while
Rifampicin is in capsule form and streptomycin is injectable.
RECOMMENDED CATEGORY OF TREATMENT REGIMEN
Category
Type of TB
Patient
Treatment Regimen
Intensive
Phase
Continuation
Phase
Total
Period
I
New smear
positive PTB
New smear
positive PTB
with extensive
parenchymal
lesion
EPTB and
Severe
concomitant
HIV disease
2 RIPE
4 RI
6
mos.
II
Treatment
Failure
Relapse
Return after
default
2 RIPES
/1 RIPE
5 RIE
8
mos.
III
New smear-
negative PTB
With minimal
parenchymal
lession
2 RIP
4 RI
6
mos.
IV
Chronic ( still
smear-positive
after supervised
re-treatment )
Refer to
or DOTS
to City
Specialized
Plus Center
Provincial
Coordinator
facility
refer
NTP
Lecture Notes on EPI Diseases / National TB Control Program (DOTS)
Prepared By: Mark Fredderick R Abejo RR, MAN
Clinical Instructor
4
DOSAGE PER CATEGORY OF TRATMENT REGIMEN
A. Fixed-Dose Combination Formulation
The number of tablets of FDCs per patient will depend on the body
weight.
Categories I and I II : 2 RIPE / 4 RI ( FDC)
Body Weight
(kg)
No.of tablets per day
Intensive Phase
( 2 months )
FDC-A ( RIPE)
No. of tablets per day
Continuation Phase
( 4 months )
FDC-B (RI)
30 - 37 2 2
38 54 3 3
55 70 4 4
More than 70 5 5
Categories I I : 2 RI PES / RI PE / 4RI E (FDC)
Body
Weight
Intensive
Phase
Continuation Phase
First
Two (2)
Months 3
rd
Month
FDC-B
( RI )
E
400
mg
FDC-A
(RIPE)
Streptomycin FDC-A
(RIPE)
30 37 2 0.75 g 2 2 1
38 54 3 0.75 g 3 3 2
55 70 4 0.75 g 4 4 3
More
than 70
5 0.75 g 5 5 3
B. Single Dose Formulation ( SDF )
Simply add 1 tablet of Isoniazid ( 100mg) , Pyrazinamide
(500mg) and Ethambutol ( 400mg) each for the patient weighing more
than 50kg before treatment initiation. Modify drug dosage within
acceptable limits according to patients body weight, particularly those
weighing less than 30 kg at the time of diagnosis.
Categories I and I II : 2 RIPE / 4 RI (SDF)
Anti-TB Drugs No. of tablets per day
Intensive Phase
( 2 months )
No. of tablets per day
Continuation Phase
( 4 months )
Rifampicin 1 1
Isoniazid 1 1
Pyrazinamide 2
Ethambutol 2
Categories I I: 2 RI PES / 1 RI PE / 5 RI E
Anti-TB
Drugs
No. of Tablets /
Intensive
(3months )
Vial per day
Phase
No.of Tablets per
day
Continuation Phase
( 5 months )
First 2 months 3
rd
months
Rifampicin 1 1 1
Isoniazid 1 1 1
Pyrazinamide 2 2
Ethambutol 2 2 2
Streptomycin 1 vial per day
Note: 56 vials of Streptomycin for two months
Lecture Notes on EPI Diseases / National TB Control Program (DOTS)
Prepared By: Mark Fredderick R Abejo RR, MAN
Clinical Instructor
5
Drug Dosage per Kg. Body Weight
Anti-TB Drugs
Dose per Kg Body Weight and Maximum Dose
Rifampicin 5 ( 4 6 ) mg/kg and not to exceed 400 mg daily
Isoniazid 10 ( 8 12 ) mg/kg and not to exceed 600 mg daily
Pyrazinamide 25 ( 20 30 ) mg/kg and not to exceed 2 mg daily
Ethambutol 15 ( 15 20 ) mg/kg and not to exceed 1.2 g daily
Streptomycin 15 ( 12 18 ) mg/kg and not to exceed 1 g daily
D.O.T.S ( Directly-Observed Treatment Shortcourse ) TuTok Gamutan
5 Elements of D.O.T.S
Sustained political commitment
Access to quality-assured sputum microscopy
Standardized short-course chemotherapy for all cases of TB
Uninterrupted supply of essential drugs
Recording and reporting system enabling outcome assessment of all patients
and assessment of overall program performance.
MANAGEMENT OF CHILDREN WITH TB
Prevention
BCG vaccination shall be given to all infants.
BCG vaccine is moderately effective. It has a protective efficacy of:
50 % against any TB disease
64 % against TB meningitis
74 % against death from TB
Case Finding
Cases of TB in children are reported and identified in two instances:
- The patient sought consultation.
- The patient was reported to have been exposed to an adult with TB
All TB symptomatic children 0-9 years old, except sputum positive
child shall subject to PDD testing
- Only trained nurse and midwife shall do the PDD test and recording
- Testing and reading shall be conducted once a week either on Monday
or
Tuesday.
Note: 10 children shall be gathered for testing to avoid wastage.
A child shall be suspected as having TB and considered symptomatic
if with any three (3) of the following sign and symptoms:
cough and wheezing for 2 weeks or more
unexplained fever for 2 weeks or more
loss of appetite, loss of weight, failure to gain weight
failure to respond to a 2 weeks of appropriate antibiotic therapy
failure to regain state of health 2 weeks after a viral infection or after
having measles.
A child shall be clinically diagnosed or confirmed of having TB if he
has any three (3) of the following condition:
positive history of exposure to an adult/ adolescent TB case
presence of sign and symptoms suggestive of TB
positive Mantoux Test
abnormal chest radiograph suggestive of TB
Management
For children with exposure to TB
Should undergo physical examination and PDD testing (Mantoux Test)
A child with productive cough shall be referred for DSSM, if found
positive, treatment shall be started immediately. PDD testing shall no
longer needed.
Children without sign/symptoms of TB but with positive Mantoux Test
and those with symptoms of TB but negative Mantoux Test shall
referred for chest x-ray examination.
Lecture Notes on EPI Diseases / National TB Control Program (DOTS)
Prepared By: Mark Fredderick R Abejo RR, MAN
Clinical Instructor
6
For children with signs and symptoms of TB
A child to have signs and symptoms of TB with either known or unknown
exposure shall be referred for Mantoux test.
For children with known contact but with negative Mantoux and those
unknown contact but with positive Mantoux shall be referred for chest x-ray
examination.
For a negative x-ray report, Mantoux test shall be repeated after 3 months.
Chemoprophylaxis of Isoniazid for 3 months shall be given to children less
than 5 years old with negative chest x-ray after which Mantoux test shall be
repeated
Treatment
D.O.T.S will still be followed just like in adult
Short course regimen:
- at least 3 anti-TB drugs for 2 months ( intensive phase )
- 2 anti-TB drugs for 4 months ( continuation phase )
* For Extra Pulmonary TB Cases:
- 4 anti-TB drugs for 2 months ( intensive phase )
- 2 anti-TB drugs for 10 months ( continuation phase )
Domiciliary treatment shall be the preferred mode of care
No treatment shall be initiated unless the patient and health worker has agreed
upon a caseholding mechanism for treatment compliance.
Treatment Regimen
A. Pulmonary TB
Drugs Daily Dose (mg/kg per body
weight )
Duration
Intensive Phase
Rifampicin
Isoniazid
Pyrazinamide
10-15 mg/kg body weight
10-15 mg/kg body weight
20-30 mg/kg body weight
2 months
Continuation
Phase
Rifampicin
Isoniazid
10-15 mg/kg body weight
10-15 mg/kg body weight
4 months
B. Extra Pulmonary TB
Drugs Daily Dose (mg/kg per body weight ) Duration
Intensive Phase
Rifampicin
Isoniazid
Pyrazinamide
Plus
Ethambutol
OR
Streptomycin
10-15 mg/kg body weight
10-15 mg/kg body weight
20-30 mg/kg body weight
15-25 mg/kg body weight
20-30 mg/kg body weight
2
months
Continuation
Phase
Rifampicin
Isoniazid
10-15 mg/kg body weight
10-15 mg/kg body weight
10
months
Public Health Nurse Responsibilities ( Childhood TB )
1. Interview and open treatment cards for identified TB children.
2. Perform Mantoux testing and reading to eligible children
3. Maintain NTP records
4. Manage requisition and distribution of drugs
5. Assist the physician in supervising the other health workers of the
RHU in the proper implementation of the policies and guidelines
on TB in children.
6. Assist in the training of other health workers on Mantoux testing
and reading.
Lecture Notes on EPI Diseases / National TB Control Program (DOTS)
Prepared By: Mark Fredderick R Abejo RR, MAN
Clinical Instructor
7
EPI TARGET DISEASES
Disease Causative
Agent
Mode of
Transmission
Clinical
Manifestation
Reservoir Diagnostic
Exam
Treatment Nursing
Implication
Diphteria it is an
acute pharyngitis,
acute
nasopharyngitis
or acute laryngitis
with Pseudo
membrane
grayish white in
color with leathery
consistency in the
throat and on the
tonsil
Corynebacterium
diphtheriae
Respiratory
Droplets
Nasal
dryness of the
upper lip
serosanguinous
secretion in the
nose
Pharyngeal
Bullneck
appearance
because of the
enlarge cervical
lymph nodes.
Laryngeal
sore throat
hoarseness
brassy metallic
cough
Man
Schicks Test
- test for the
susceptibility to
Diptheria
Moloney Test
- for hyper-
sensitivity to
Diptheria toxin
Antibiotics
Pen G
Potassium
Erythromycin
Isolate patient
until 2-3 cultures
taken at least
24hrs apart are
negative
Small frequent
feeding
Promote
absolute rest
Use ice collar to
relieve pain of
sore throat
May put on soft
diet
Pertussis
- 100 days cough
- Whooping cough
- tuspirina
Bordetella
Pertussis
Airborne
droplet
Primarily by
direct contact
with he
discharge from
respiratory
mucous
membranes of
infected person
At first, the
infected child may
have a common
cold with runny
nose, sneezing
and mild cough
Intermittent
episode of
paroxysmal
cough followed
by a whoop
ending vomiting
Man
Bordet-
Gengou Agar
Plate
- used for
culture medium
Erythromycin
Ampicillin
- is given 5-7 days
Place the patient
on NPO during
paroxysmal stage
to prevent
aspiration
Position prone
for infants and
upright for older
Lecture Notes on EPI Diseases / National TB Control Program (DOTS)
Prepared By: Mark Fredderick R Abejo RR, MAN
Clinical Instructor
8
Neonatal Tetanus
Clostridium
Tetani
- which produces
the exotoxins:
Tetanolysin
Tetanospasmin
Unhygienic
cutting of
umbilical cord
Improper
handling of cord
stump esp. when
treated with
contaminated
substance
Assess the
NEWBORN for a
history of all 3 of the
following:
Normal suck and
cry for the first 2
days of life
Onset of illness
between 3 and 28
days
Inability to suck
followed by
stiffness of the
body and
convulsion
In OLDER
CHI LDREN, the
following may be
observed:
Trismus
lockjaw
Opisthotonus
arching of the
neck and back
Ridus
Sardonicus
sardonic smile
Soil
Intestinal
canal of
animal
Man
Blood Culture
CSF analysis
Penicillin
Erythromycin
Tetracycline
- administered
within 4 hours of
injury
Prevention
Aseptic
handling of the
neonatal
umbilical cord
Tetanus Toxiod
immunization for
mothers
Active
immunization of
DPT
Lecture Notes on EPI Diseases / National TB Control Program (DOTS)
Prepared By: Mark Fredderick R Abejo RR, MAN
Clinical Instructor
9
Poliomyelitis
Infantile
Paralysis
3 Types of Polio
Virus
Type I
Brunhilde
Type II
Lansing
Type III Leon
Fecal-oral route
Oral route
through
pharyngeal
secretion
Contact with
infected person
Abortive - did not
progress to systemic
infection
Non-paralytic
slight involvement
of the CNS
Poker spine or
stiffness of the
spinal column
Spasms of the
hamstring
With paresis
Paralytic severe
involvement of CNS
Hoynes Sign
head falls back
when he is in
supine with
shoulder elevated
Paralysis
Head log/drop
Tripod position
extend his arm
behind for support
when he sits up
Kernigs sign
Brudzinski sign
Man
Throat swab
Stool exam
Lumbar exam
Pandys test
- for CSF
analysis
Strict Isolation
Hot moist
compress to
relieve spasm
Use protective
devices:
- handroll to
prevent claw hand
- trochanter roll, to
prevent outer
rotation of femur
- footboard
Lecture Notes on EPI Diseases / National TB Control Program (DOTS)
Prepared By: Mark Fredderick R Abejo RR, MAN
Clinical Instructor
10
Hepatitis B
- it is liver
infection caused by
the B type of
hep.virus.
It attacks livers the
liver often
resulting in
inflammation
Hepa B Virus
3 Ps
Person to person
Parenteral
Placental
Prodromal/pre-
icteric
Symptoms of
URTI
Weight loss
Anorexia
RUQ pain
Malaise
Icteric
Jaundice
Acholic stool
bile-colored
urine
Man
Liver
Function Test
Increase CHO
Moderate fat
Low CHON
Observed universal
precaution
Measles
Paramyxo Virus
Droplet
3 Cs
Conjunctivitis
Coryza
Cough
Kopliks spot
bluish gray spot on
the buccal mucosa.
Generalized blotch
rash
Man
Observe
respiratory
isolation
Should kept out
of school for at
least 4 days after
rash appear
For
Photophobic,
darkened room,
sunglasses
You might also like
- 100 Item Comprehensive Exam With Answers and RationaleDocument21 pages100 Item Comprehensive Exam With Answers and RationaleAijem Ryan93% (15)
- Robin Murphy Repertory - A New Approach To Clinical HomeopathyDocument5 pagesRobin Murphy Repertory - A New Approach To Clinical Homeopathysocialhompath17% (6)
- Community Health Nursing Practice Questions With RationalesDocument15 pagesCommunity Health Nursing Practice Questions With RationalesFelice Lamzon Labrador100% (3)
- Community Health Nursing Practice Questions With RationalesDocument15 pagesCommunity Health Nursing Practice Questions With RationalesFelice Lamzon Labrador100% (3)
- Community Health Nursing Practice Questions With RationalesDocument15 pagesCommunity Health Nursing Practice Questions With RationalesFelice Lamzon Labrador100% (3)
- Hand Hygiene: Alcohol Based Hand RubDocument2 pagesHand Hygiene: Alcohol Based Hand RubKIERSTINE MARIE BARCELONo ratings yet
- An Case Study - WebsiteDocument5 pagesAn Case Study - Websiteapi-249707182No ratings yet
- Professional Adjustment Leadership Management and ResearchDocument10 pagesProfessional Adjustment Leadership Management and Researchshenric16100% (1)
- Fundamentals of NursingDocument31 pagesFundamentals of NursingAngelica Soriano93% (14)
- Infraction ToothDocument45 pagesInfraction ToothanmolNo ratings yet
- NCP Acute PainDocument2 pagesNCP Acute PainDanielJosephLimNo ratings yet
- 8 Point Action Agenda For 2023 2028 For LGUsDocument16 pages8 Point Action Agenda For 2023 2028 For LGUsGinalyn Gine- Garduque100% (1)
- Expanded Program On ImmunuzationDocument37 pagesExpanded Program On ImmunuzationRose AnnNo ratings yet
- Child Immunization ProgramDocument14 pagesChild Immunization ProgramShane DamianNo ratings yet
- Business Proposal SampleDocument3 pagesBusiness Proposal SampleIan TattaoNo ratings yet
- HyperthyroidismDocument17 pagesHyperthyroidismDante SalesNo ratings yet
- Graduate Tracer Study of LORMA CollegesDocument1 pageGraduate Tracer Study of LORMA CollegesLEO ALCANTARANo ratings yet
- Narrative Report Day 4Document2 pagesNarrative Report Day 4Maria Arabella LanacaNo ratings yet
- Administration of Pneumococcal VaccineDocument24 pagesAdministration of Pneumococcal VaccineJay AdamzNo ratings yet
- Case Presentation RamosDocument35 pagesCase Presentation RamosJose Bryan NacillaNo ratings yet
- STS ReviewerDocument6 pagesSTS ReviewerKurogamiNo ratings yet
- The EPI Routine Schedule of Immunization in The PhillippinesDocument21 pagesThe EPI Routine Schedule of Immunization in The PhillippinesJesse Martin100% (1)
- Leprosy Control Program: Vision: Mission: ObjectivesDocument5 pagesLeprosy Control Program: Vision: Mission: ObjectivesAngelica VillalonNo ratings yet
- Movie Reflection For Im Not Ashamed and MagnificoDocument6 pagesMovie Reflection For Im Not Ashamed and MagnificoJesselle Hannah Agbayani Ancheta-Ruiz100% (2)
- PCMC Journal Vol 15 1Document102 pagesPCMC Journal Vol 15 1Amadea WPNo ratings yet
- HRH 4S Strategy For DengueDocument9 pagesHRH 4S Strategy For DengueIereen PiansayNo ratings yet
- CHN Lec 1 5Document7 pagesCHN Lec 1 5Altea PasiaNo ratings yet
- Cavite State University: I. ObjectivesDocument7 pagesCavite State University: I. ObjectivesChamy CruzNo ratings yet
- MNCHN RNHealsDocument58 pagesMNCHN RNHealstinea nigraNo ratings yet
- Nurse Deployment Project 2014: Implementing GuidelinesDocument6 pagesNurse Deployment Project 2014: Implementing GuidelinesGee RidadNo ratings yet
- Mitotic InhibitorsDocument17 pagesMitotic InhibitorsSamuel CamoronganNo ratings yet
- The Community Health Nursing and Communicable DiseasesDocument40 pagesThe Community Health Nursing and Communicable DiseasesericNo ratings yet
- Expanded Program On ImmunizationDocument9 pagesExpanded Program On ImmunizationJesena Salve100% (1)
- Cover LetterDocument7 pagesCover LetterKrishia Angelie FloresNo ratings yet
- Prelims 219 QDocument6 pagesPrelims 219 QAloha ItsmeNo ratings yet
- Expanded Program On ImmunizationDocument4 pagesExpanded Program On ImmunizationKrizle AdazaNo ratings yet
- Expanded Program On Immunization (Philippines)Document10 pagesExpanded Program On Immunization (Philippines)Karen Bianca Espinola, MD. DPBA.No ratings yet
- Multi Drug Resistant TBDocument28 pagesMulti Drug Resistant TBmedeviNo ratings yet
- 3B GRP 2 Community Health PlanDocument14 pages3B GRP 2 Community Health PlanIsabelle Hazel BenemileNo ratings yet
- Mental IllnessDocument15 pagesMental Illnessjunjun04No ratings yet
- Cellular AberrationDocument70 pagesCellular Aberrationmatrixtrinity100% (2)
- Fatima Community Diagnosis ToolDocument5 pagesFatima Community Diagnosis Toolkrisfred14100% (2)
- Doh Health Programs (Adolescent Program)Document9 pagesDoh Health Programs (Adolescent Program)Wilma Nierva Beralde100% (1)
- Children's Emergency Relief & Protection Act of 2016Document6 pagesChildren's Emergency Relief & Protection Act of 2016Sam Albert RenaciaNo ratings yet
- CHN211 Week 7 PPT - National Immunization ProgramDocument85 pagesCHN211 Week 7 PPT - National Immunization ProgramZEPHANNY ANNE TABBAYNo ratings yet
- Ra 1054 & Ra 124Document3 pagesRa 1054 & Ra 124ulcNo ratings yet
- Daily Time Record Daily Time Record: Saturday SundayDocument13 pagesDaily Time Record Daily Time Record: Saturday Sundaysingle ladyNo ratings yet
- Week 1 CoparDocument9 pagesWeek 1 CoparSansaiNo ratings yet
- Infomercial Rabies Script d2Document9 pagesInfomercial Rabies Script d2Irish AlonzoNo ratings yet
- Diphtheria HandoutsDocument8 pagesDiphtheria HandoutsRachelle Mae DimayugaNo ratings yet
- ESR Verification Form - Dec2015Document2 pagesESR Verification Form - Dec2015Sandro Redoble100% (2)
- Health Education PlanDocument1 pageHealth Education PlanDahnel MagumparaNo ratings yet
- Case Scenario 10Document1 pageCase Scenario 10Mart Juaresa YambaoNo ratings yet
- NCM 117 Rle - Self-AwarenessDocument3 pagesNCM 117 Rle - Self-AwarenessKate Angelique RodriguezNo ratings yet
- DOH ProgramsDocument6 pagesDOH ProgramsMichael VillavertNo ratings yet
- Journal Study Regarding PCAP WashingtonDocument1 pageJournal Study Regarding PCAP WashingtonLuis WashingtonNo ratings yet
- TB Teaching PlanDocument5 pagesTB Teaching PlanTrisha Fae Loyola Balagot100% (1)
- CA Exam UndergraduateDocument3 pagesCA Exam UndergraduateMilagros Fuertes YosoresNo ratings yet
- Review CHN Midterm ExamDocument10 pagesReview CHN Midterm ExamAira Shane Marges100% (1)
- Initial ManuscriptDocument26 pagesInitial ManuscriptDennisse CastillonNo ratings yet
- Gordons Health PatternsDocument2 pagesGordons Health PatternsLaurence ZernaNo ratings yet
- Chapter 1 Reproductive Health EpidemiologyyDocument13 pagesChapter 1 Reproductive Health EpidemiologyyAnnisa NurrachmawatiNo ratings yet
- 1 Unang YakapDocument3 pages1 Unang Yakapyra capiliNo ratings yet
- Expanded Program of Immunization (Source: DOH)Document12 pagesExpanded Program of Immunization (Source: DOH)Jefferson Dungca94% (35)
- RABE 3 CHN 2sem 22Document5 pagesRABE 3 CHN 2sem 22Basa, Rica Mae P.No ratings yet
- Roth 10e Nclex Chapter 06Document3 pagesRoth 10e Nclex Chapter 06jennaaahhh100% (1)
- Sample FCP GDocument21 pagesSample FCP GKeren GaciasNo ratings yet
- God Is Good All The TimeDocument27 pagesGod Is Good All The TimeEsther Faith GabrielNo ratings yet
- Communicablediseases 110227001506 Phpapp02 PDFDocument30 pagesCommunicablediseases 110227001506 Phpapp02 PDFCrystal Ann Monsale TadiamonNo ratings yet
- Evidence Based Nursing PracticeDocument21 pagesEvidence Based Nursing Practiceshenric16No ratings yet
- Uhc Irr DraftDocument107 pagesUhc Irr Draftshenric16No ratings yet
- Health Teaching PDFDocument1 pageHealth Teaching PDFshenric16No ratings yet
- Fhsis Annual 2018Document496 pagesFhsis Annual 2018shenric16No ratings yet
- Palmer Complete Edited Royal PentagonDocument26 pagesPalmer Complete Edited Royal Pentagonshenric16100% (1)
- Evidence Based Nursing PracticeDocument21 pagesEvidence Based Nursing Practiceshenric16No ratings yet
- Nursing Board Exam Test Drill 3Document2 pagesNursing Board Exam Test Drill 3Kira100% (15)
- Cognitive DisordersDocument2 pagesCognitive DisordersSherrizah Alexis Naag NavaNo ratings yet
- Maternity Nursing ReviewDocument37 pagesMaternity Nursing Reviewshenric16No ratings yet
- Patient Positioning in The Operating RoomDocument33 pagesPatient Positioning in The Operating Roomshenric16No ratings yet
- Anti Psychotic DrugsDocument2 pagesAnti Psychotic DrugsJohn Corpuz100% (1)
- Maternal Ob NotesDocument37 pagesMaternal Ob Notesshenric16No ratings yet
- Nle - July 2011Document12 pagesNle - July 2011shenric16100% (2)
- Course Audit Professional AdjustmentDocument9 pagesCourse Audit Professional Adjustmentshenric16No ratings yet
- Reviewer For NleDocument14 pagesReviewer For Nleshenric16No ratings yet
- Community Health NursingDocument49 pagesCommunity Health Nursingshenric16No ratings yet
- Maternal Ob NotesDocument37 pagesMaternal Ob Notesshenric16No ratings yet
- Community Health NursingDocument49 pagesCommunity Health Nursingshenric16No ratings yet
- Final Outline Psychiatric NursingDocument52 pagesFinal Outline Psychiatric Nursingshenric16100% (1)
- Maternal and Child Health Nursing: KeepsDocument32 pagesMaternal and Child Health Nursing: Keepsshenric16No ratings yet
- Medicationpart1 110202192115 Phpapp02Document10 pagesMedicationpart1 110202192115 Phpapp02Jessamine Rochelle Reyes Esberto100% (1)
- Ms Penta NotesDocument84 pagesMs Penta Notesshenric16No ratings yet
- Maternal and Child Health Nursing: KeepsDocument32 pagesMaternal and Child Health Nursing: Keepsshenric16No ratings yet
- Pediatric Nursing Edison O Dangkeo RNDocument59 pagesPediatric Nursing Edison O Dangkeo RNshenric16100% (1)
- Surgery Syllabus 2010.12Document7 pagesSurgery Syllabus 2010.12AsterzebuleNo ratings yet
- Oral Rehydration SaltDocument3 pagesOral Rehydration SaltVincent ManganaanNo ratings yet
- Causes of Female Infertility - UpToDateDocument11 pagesCauses of Female Infertility - UpToDateBreno AlmeidaNo ratings yet
- Voxra - PI - GSK - SAHPRA Format 24 October 2019Document20 pagesVoxra - PI - GSK - SAHPRA Format 24 October 2019Vit MNo ratings yet
- Hypertensive CrisisDocument30 pagesHypertensive CrisisAfraDewitaNo ratings yet
- MorbiliDocument43 pagesMorbiliNur AtikaNo ratings yet
- Viral Disease of The Upper RSDocument19 pagesViral Disease of The Upper RSAries Gonzales CaraganNo ratings yet
- Nhs Bronchiolitis Pathway Acute Setting South East Coast SCNDocument2 pagesNhs Bronchiolitis Pathway Acute Setting South East Coast SCNdrgrizahNo ratings yet
- Jawaban Compound Exercise 2Document4 pagesJawaban Compound Exercise 2Evoria ManurungNo ratings yet
- Acute Rheumatic FeverDocument26 pagesAcute Rheumatic FeverAshvanee sharma100% (1)
- Determination of Stress, Depression and Burnout Levels of Front Line Nurses During Covid-19 PandemicDocument11 pagesDetermination of Stress, Depression and Burnout Levels of Front Line Nurses During Covid-19 PandemicZahra'a AlmeerNo ratings yet
- High-Yield Endocrine Q&ADocument9 pagesHigh-Yield Endocrine Q&ALillian Bezares100% (1)
- 1 Mechanisms of Disease in Small Animal SurgeryDocument5 pages1 Mechanisms of Disease in Small Animal SurgeryhillsunitedNo ratings yet
- ENEMADocument4 pagesENEMAMariah Alexis EncinaNo ratings yet
- NCP Pain TeresitoDocument3 pagesNCP Pain TeresitoTheresa Reyes De JesusNo ratings yet
- NSTP Lecture 4 Drug AddictionDocument11 pagesNSTP Lecture 4 Drug AddictionRona CabuguasonNo ratings yet
- Kala Pathar IntoxicationDocument5 pagesKala Pathar IntoxicationSyed AsharNo ratings yet
- Analytical Exposition Text Kel 5Document11 pagesAnalytical Exposition Text Kel 5Oja JamaludinNo ratings yet
- Robert Koch - Microbiology Notes of Sridhar Rao P.NDocument2 pagesRobert Koch - Microbiology Notes of Sridhar Rao P.NBijaya kumar PatraNo ratings yet
- Breast AbscessDocument2 pagesBreast AbscessAbrish RaoNo ratings yet
- Case Management: Leira Dith R. Castro, MD Presentor 1 Year Im ResidentDocument64 pagesCase Management: Leira Dith R. Castro, MD Presentor 1 Year Im ResidentAlvin Germo PasuquinNo ratings yet
- Drug StudyDocument5 pagesDrug StudyKristoff CamposNo ratings yet
- Leg Calve Perthes MR NomiDocument27 pagesLeg Calve Perthes MR Nomiagnes trianaNo ratings yet
- Pathophysiology of Tuberculosis: Group 5 Latosa, Selene Lee, Guk Lim, Johanna Magalona, Stephen Mendoza, ColeenDocument22 pagesPathophysiology of Tuberculosis: Group 5 Latosa, Selene Lee, Guk Lim, Johanna Magalona, Stephen Mendoza, ColeenAlexander Santiago ParelNo ratings yet
- Patofisiologi Polisitemia VeraDocument2 pagesPatofisiologi Polisitemia VeraErni PanjaitanNo ratings yet
- Psychopathology and Basic Concepts: Dictionary of PhenomenologyDocument12 pagesPsychopathology and Basic Concepts: Dictionary of PhenomenologyskNo ratings yet
- Principles of Tissue Biopsy in Oral and MaxillofacialDocument34 pagesPrinciples of Tissue Biopsy in Oral and MaxillofacialEdmond Apriza DrgNo ratings yet