Antibody Detection
Antibody Detection
Uploaded by
hamaadaCopyright:
Available Formats
Antibody Detection
Antibody Detection
Uploaded by
hamaadaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Antibody Detection
Antibody Detection
Uploaded by
hamaadaCopyright:
Available Formats
Antibody Detection & Crossmatch
The goal of antibody screening is to detect unexpected clinically significant red cell
antibodies. In general, clinically significant antibodies are antibodies known to have caused
Hemolytic Disease of the Newborn (HDN), hemolytic transfusion reaction, or shortened
survival of transfused red blood cells.
There are several ways to detect red cell antibodies. Each hospital or region determines its
method of antibody screening and compatibility testing. Regardless of the method or
enhancement media used, the method must be capable of detecting clinically significant
antibodies, which requires that the antibody screen method include a 37oC incubation with
reagent red cells that have not been pooled followed by an Indirect Antiglobulin Test (IAT),
or an alternate method that has documented capability to provide comparable sensitivity.
Methods of Antibody Detection & Crossmatch
1. Indirect Antiglobulin Test
- LISS
- PEG
2. MTS GEL Test (Gel-IAT)
3. Solid Phase Adherence Assay (SPAA)
Whenever the antibody screen is found to be positive, an
antibody investigation must be performed.
Crossmatch Methods
1. Immediate Spin Crossmatch
The Immediate Spin (IS) crossmatch is performed only after an antibody screen is
done and found to be negative on a current specimen. The patient should have no
history of clinically significant antibodies.
The immediate spin crossmatch is meant to detect ABO incompatibility. It can
also detect cold reactive (clinically insignificant) antibodies that react at room
temperature (RT).
If the patient's expected ABO antibodies are not reactive or weak at immediate
spin,donor units should be ABO confirmed prior to testing with this method.
2. Computer or Electronic Crossmatch
Further Reading
The Antihuman Globulin (AHG) Test
The antihuman globulin test is used in numerous ways in
pretransfusion and compatibility testing.
LISS IAT
PEG IAT
Many hospital transfusion services perform IAT antibody
screening and antibody identification but have switched to
the immediate spin or computer crossmatch to improve
efficiency. It is not necessary to perform an IAT crossmatch on patients with a negative
antibody screen and no history of clinically significant antibodies.
Principle
1. The Indirect Antiglobulin Test (IAT) is used to detect in-vitro sensitization and
detects anti-red cell antibodies in patient's serum or plasma. Procedural steps are as
follows:
- Patient's plasma or serum is incubated at 37oC with red cells (screen or panel cells
of known antigenic composition or donor cells of unknown antigenic composition)
- A potentiator may or may not be added
- During incubation, if an antibody is present in the plasma or serum and the
corresponding antigen is present on the red cells, the cells become sensitized by the
antibody adsorbing to antigens on the red cell surface
- After incubation, the red cells are washed with saline three to four times to remove
unbound antibody
- Antihuman globulin serum (anti-IgG or polyspecific AHG, usually the former) is
added and forms RBC agglutinates if the antibody has attached to the antigen sites
during incubation
- The test is read after centrifugation and careful resuspension of the red cells
2. The Direct Antiglobulin Test (DAT) is used to detect in-vivo sensitization and
detects antibodies on a patient's red cells. The procedural steps are as above, except
no incubation with serum or plasma is required. The red cells are washed and
polyspecific AHG is added.
Types
direct to detect in vivo sensitization
indirect to detect in vitro sensitization
Applications
antibody screening
antibody identification
antigen phenotyping using antisera that require the indirect antiglobulin test
direct antiglobulin test
Types of Antibodies Detected
IgG antibodies at the AHG phase
complement-binding IgM or IgG antibodies, if polyspecific AHG is used
IgM antibodies, if the test is read at 37oC
Advantages of the IAT Crossmatch
can detect antibodies to low incidence antigens on donor cells that are not present on
screening cells
provides a final check of ABO compatibility
acts as a double check on the antibody screen
Disadvantages of the IAT Crossmatch
time consuming blood must be prepared in advanceof anticipated transfusion, which
may result in high crossmatch/transfusion ratio and potentially suboptimal use of
technologist time
stressful in STAT situation because of testing time required
Low Ionic Strength Saline (LISS-IAT) Testing
LISS-IAT became well-established in the 1980s as a method done in test tubes (as was its
predecessor, the saline-IAT). LISS-IAT involves incubating patient serum (or plasma) with
LISS and screen cells at 37oC, followed by the antiglobulin phase.
The advantage of LISS (compared to saline methods) is its shorter incubation of 10 or 15
minutes. LISS methods can be read after 37oC (LISS 37oC phase) and also after the IAT.
Some transfusion services read only the LISS-IAT phase (see Judd et al, 1999 in Further
Reading).
The IAT can be performed using several methods and enhancement media, e.g., LISS-IAT,
gel-IAT, and PEG-IAT.
Some laboratories perform an IAT crossmatch routinely for all patients, even those with a
negative antibody screen. Many others reserve the IAT crossmatch for patients with clinically
significant antibodies, in which case it is mandatory.
Polyethylene Glycol (PEG-IAT)
PEG-IAT is done in test tubes and consists of an IAT phase only. Patient serum (or plasma) is
incubated with PEG and screen cells at 37oC, followed by the antiglobulin phase using anti-
IgG. PEG enhances reactions by physically taking up space and forcing antigens and
antibodies closer together. It is a sensitive method but has some precautions regarding
immunoglobulin precipitation (see Polski et al in Further Reading).
The Gel Test
The gel test was developed in Switzerland in the late 1980s
as a way to standardize the method of obtaining
agglutination and to provide a simple and reliable way to
read it. Unlike tube tests in the gel method, agglutination does not take place in a liquid phase
but rather in a gel contained in a special microtube.
The only licensed gel test available in Canada is the MTS gel technique distributed
exclusively by Ortho Clinical Diagnostics. The sole phase is the gel-IATno washing is
required prior to adding antihuman globulin serum. Microtubes are used instead of glass test
tubes.
Principle
Patient's plasma or serum is incubated at 37oC with red cells (screen or panel cells of
known antigenic composition or donor cells of unknown antigenic composition).
During incubation, if antibody is present in the plasma or serum and the
corresponding antigen is present on the red cells, the cells become sensitized (by the
antibody adsorbing to antigens on the red cell surface).
After incubation the gel card is centrifuged during which the red cells pass through
anti-IgG within the dextran-acrylamide gel.
Agglutinated red cells become trapped on or above the gel.
Unagglutinated cells pass through the gel and form a pellet at the bottom of the
microtube.
Types
IgG cards
Microtubes containing gel with specific antibody for phenotyping
IgG;C3d card (for direct antiglobulin testing)
Buffered gel card (used for reverse serum grouping)
Applications
Antibody Screening
Antibody Identification
Antigen Phenotyping
Direct Antiglobulin testing
Types of antibodies detected
IgG antibodies when IgG cards are used
Advantages
small volumes of patient specimen
enhanced sensitivity and specificity
automation possible for high volume and batch testing
no washing of antiglobulin tests
test results may be stored for confirmation reading by supervisor or staff on a different
shift
elimination of microscopic reading resulting in more objective interpretation of test
results
no red cell resuspension resulting in a more standardized procedure
Disadvantages
relatively expensive start-up costs (special incubators, centrifuges, sample dispensors)
expensive cost per test compared to tube antiglobulin testing
The Solid Phase Adherence Assay (SPAA)
SPAA for antibody identification uses dried red cells that have been bound to the surfaces of
polystyrene microtitration strip wells, and which capture IgG antibodies (if present) in patient
sera. The test is a modified IAT that detects antibody by addition of anti-IgG-coated red cells.
Immucor's Capture-R Ready ScreenTM is a commercial solid phase system distributed in
Canada by Dominion Biologicals that uses strip micro wells which are coated with dried
antibody screen cells. Automated systems using SPAA include Immucor's ABS 2000 and
Rosys Plato.
Principle
The SPAA for antibody detection uses red cell membranes that have been bound to the
surfaces of polystyrene microtitration strip wells, and which capture IgG antibodies in patient
sera.
Patient plasma or serum and an enhancement solution such as LISS are added to wells
coated with red cell membranes (screen cells).
After incubation at 37oC, unbound IgG is washed away (as in standard antiglobulin
tests).
Anti-IgG-coated indicator red cells are added.
Tests are centrifuged and read.
If patient IgG antibodies have attached to the cell membranes, the anti-IgG-coated
indicator red cells form anti-IgG-IgG complexes. As a result, the indicator cells
adhere to the wells as a second immobilized cell layer and form a dispersed conflux
("lawn") of cells, constituting a positive test.
Conversely, in negative tests, the indicator cells pellet to the bottom of the wells
forming a distinct, smaller cell button.
Types
red cell assays
platelet assays (IgG anti-platelet antibodies)
infectious disease assays (screen for anti-CMV)
Applications
antibody screening
antibody identification
antigen typing
Types of Antibodies Detected
IgG antibodies
Advantages
increased sensitivity
automation possible for high volume and batch testing
claims to have faster test performance times thereby saving technologist time
test results may be stored for confirmation reading by a supervisor or staff on a
different shift
elimination of microscopic reading resulting in more objective interpretation of test
results
no red cell resuspension resulting in a more standardized procedure
Disadvantages
relatively expensive start-up costs for automated systems
Computer-Assisted (Electronic)
Crossmatch
ABO-compatible units are prepared for patients with no history of clinically significant
antibodies, a negative antibody screen on a current specimen, and two independent ABO
groupings. Antibody detection must be done by IAT.
The computer system must have successfully undergone an on-site validation process prior to
implementation of the electronic crossmatch.
Principle
Using a validated computer system, patients with no history of clinically significant
antibodies and a negative antibody screen on the current specimen are issued ABO specific or
compatible donor units.
Standards
Specific standards must be met to implement this test.
1. Two independent determinations of the ABO
group of the patient
2. No history of clinically significant antibodies
3. A negative antibody screen on a current specimen
4. Donor units are ABO confirmed
5. The computer system is validated on site, results
are entered directly into the computer, and there is
logic in the system to recognize incompatibility
Validation
FDA. General Principles of Software Validation; Final Guidance for Industry and
FDA Staff
Advantages
Donor units may be prepared quickly (no patient specimen required)
Only a group (or type) and screen required for most patients
Disadvantages
Will NOT detect antibodies to low incidence antigens present on donor cells that are
not present on screening cells.
Will NOT detect donor cells with a positive direct antiglobulin test.
Donor unit must be ABO confirmed prior to placing in available inventory
You might also like
- Tooth by ToothDocument4 pagesTooth by Toothrakhee karNo ratings yet
- Troubleshooting in CXMDocument3 pagesTroubleshooting in CXMquerokeropi100% (1)
- B Blab 7 Panel Spring 2012Document16 pagesB Blab 7 Panel Spring 2012pzaballero7063No ratings yet
- Urinalysis and Body Fluids for Cls & MltFrom EverandUrinalysis and Body Fluids for Cls & MltNo ratings yet
- Study Stack - ASCP Coag Hematology Table ReviewDocument2 pagesStudy Stack - ASCP Coag Hematology Table Review장주연100% (1)
- Detection of AntibodiesDocument7 pagesDetection of AntibodiesJezreeljeanne Largo Caparoso100% (1)
- Wallis Budge Book of Am TuatDocument120 pagesWallis Budge Book of Am TuatRCEB100% (5)
- Phil Iri English 4 and 6Document6 pagesPhil Iri English 4 and 6JM GalvezNo ratings yet
- Wiki Abdomen Mcqs ExplainedDocument9 pagesWiki Abdomen Mcqs Explainedchemptnk100% (2)
- SPEAKER: Dr. Subhajit Das MODERATOR: Prof. Jyoti ShuklaDocument25 pagesSPEAKER: Dr. Subhajit Das MODERATOR: Prof. Jyoti Shuklaswaraj sharma100% (2)
- 2.5 Antibody ScreeningDocument5 pages2.5 Antibody ScreeningBALAJI100% (1)
- Antibody Screening - Kupang - 2016Document59 pagesAntibody Screening - Kupang - 2016yuni.kartika.ndoen92No ratings yet
- Antibody Detection and IdentificationDocument19 pagesAntibody Detection and IdentificationErika Leah ManaloNo ratings yet
- The Antiglobulin Test (Coomb's Test) Direct & Indirect: Group 1Document23 pagesThe Antiglobulin Test (Coomb's Test) Direct & Indirect: Group 1Marj Mendez100% (1)
- New Microsoft Word DocumentDocument7 pagesNew Microsoft Word DocumentDocAxi Maximo Jr AxibalNo ratings yet
- BB - Detection and Identification of AntibodiesDocument10 pagesBB - Detection and Identification of AntibodiesWayne VillalunaNo ratings yet
- Blood Component PreparationDocument24 pagesBlood Component PreparationLaiba ArshadNo ratings yet
- Blood Bank TypingDocument34 pagesBlood Bank TypingSkylarNo ratings yet
- Gel TechnologyDocument2 pagesGel TechnologyJai Carungay100% (1)
- Minor Blood Groups Part 1Document15 pagesMinor Blood Groups Part 1Mary Shikha ShaikeNo ratings yet
- Antibody Identification - IIDocument50 pagesAntibody Identification - IISimon Onsongo50% (2)
- Antibody ScreeningDocument57 pagesAntibody ScreeningSebastian Jake John100% (1)
- Abs Elu HandoutDocument6 pagesAbs Elu HandoutSiti Fadhilla TsabithaNo ratings yet
- Blood Group Systems ISBTDocument25 pagesBlood Group Systems ISBTkusumahpratiwi100% (1)
- Definitions: CLS 422 Clinical Immunohematology I Absorption and ElutionDocument6 pagesDefinitions: CLS 422 Clinical Immunohematology I Absorption and ElutionTrang HuynhNo ratings yet
- Miner Blood Group SystemDocument44 pagesMiner Blood Group SystemArshad RazaqNo ratings yet
- Immunohematology ASCPi Review Booklet (Part 1)Document22 pagesImmunohematology ASCPi Review Booklet (Part 1)Mark Justin OcampoNo ratings yet
- Antibody Screening and Identification ObjectivesDocument3 pagesAntibody Screening and Identification ObjectivesApril Sudario100% (1)
- Adverse Reaction Blood BankDocument10 pagesAdverse Reaction Blood BankyourfamilydoctorNo ratings yet
- Chapter 14 - Routine and Point of Care Testing in HematologyDocument10 pagesChapter 14 - Routine and Point of Care Testing in HematologyNathaniel Sim100% (1)
- Flashcards in Abo Blood GroupDocument10 pagesFlashcards in Abo Blood GroupVincent ReyesNo ratings yet
- 13 Other Blood Group SystemsDocument56 pages13 Other Blood Group SystemsCarinaJongLeeNo ratings yet
- Compatibility Testing: Week 5Document33 pagesCompatibility Testing: Week 5Bridgette100% (1)
- Coombs Test FreddyDocument11 pagesCoombs Test FreddyFreddy Vallejo LeonNo ratings yet
- Blood Bank2Document85 pagesBlood Bank22131443No ratings yet
- Compatibility Testing: Dr. Mohammed H Saiem Aldahr Blood Bank 3 Medical TechnologyDocument44 pagesCompatibility Testing: Dr. Mohammed H Saiem Aldahr Blood Bank 3 Medical TechnologyAnne Lorraine Margarette DulayNo ratings yet
- ABOsystemDocument52 pagesABOsystemJasmine HannahNo ratings yet
- Transfusion Training Checklist May 2015Document5 pagesTransfusion Training Checklist May 2015dhe100% (1)
- Lesson 07 PDFDocument14 pagesLesson 07 PDFIhsan UllahNo ratings yet
- Gel Card TechnologyDocument21 pagesGel Card TechnologyDominic BernardoNo ratings yet
- ABO Discrepancies - RahulDocument47 pagesABO Discrepancies - RahulNyxa AbdullaNo ratings yet
- ImmunohematologyDocument4 pagesImmunohematologyosama1381971100% (1)
- Blood Bak Process MapDocument1 pageBlood Bak Process MapspanwzNo ratings yet
- Antibody IdentificationDocument27 pagesAntibody Identificationhamaada100% (2)
- Red Cell and White Cell Counting, BloodDocument89 pagesRed Cell and White Cell Counting, BloodJovel Gangcuangco100% (1)
- ImmunohematologyDocument67 pagesImmunohematologyRainbow SherbetNo ratings yet
- Blood Bank EbookDocument14 pagesBlood Bank EbookNomer Formeloza BarlisNo ratings yet
- Resolution of Abo DiscrepanciesDocument4 pagesResolution of Abo DiscrepanciesPatrick MabugatNo ratings yet
- Antibody TitrationDocument14 pagesAntibody Titrationalibayaty1No ratings yet
- Blood Component TherapyDocument13 pagesBlood Component Therapymcbenze1607No ratings yet
- Lesson 22 PDFDocument5 pagesLesson 22 PDFfaeNo ratings yet
- Pocket Guide On Red Cells 2012Document8 pagesPocket Guide On Red Cells 2012Dave OrlandoNo ratings yet
- Blood Bank 4 DiscpDocument20 pagesBlood Bank 4 DiscpHector de la Cruz100% (1)
- Blood BankDocument84 pagesBlood Bankmanni1001100% (4)
- 1 Edited My Class Note 1 On Blood BankDocument42 pages1 Edited My Class Note 1 On Blood Bankmatewos100% (1)
- Correctly: IncorrectlyDocument70 pagesCorrectly: IncorrectlyDjdjjd Siisus100% (1)
- Blood Banking - Component PreparationDocument34 pagesBlood Banking - Component PreparationLentoOt EksDiiNo ratings yet
- Blood Bank IDocument136 pagesBlood Bank IPerlie CNo ratings yet
- Kursus IH ABO GROUPING v19082015 PDFDocument84 pagesKursus IH ABO GROUPING v19082015 PDFIlyasHasanNo ratings yet
- Blood BankingDocument7 pagesBlood BankingRoiland Atienza BaybayonNo ratings yet
- Tietz's Applied Laboratory MedicineFrom EverandTietz's Applied Laboratory MedicineMitchell G. ScottRating: 3 out of 5 stars3/5 (1)
- Special tests:) ١) ﺕﺎﻧﻮﺑﺮﻜﻴﺒﻟﺍ (Bicarbonate (Document4 pagesSpecial tests:) ١) ﺕﺎﻧﻮﺑﺮﻜﻴﺒﻟﺍ (Bicarbonate (hamaadaNo ratings yet
- Nilai University College Diploma in Medical Laboratory Technology MPAD 1221 Practical 5Document2 pagesNilai University College Diploma in Medical Laboratory Technology MPAD 1221 Practical 5hamaadaNo ratings yet
- ABO Grouping ProcedureDocument2 pagesABO Grouping ProcedurehamaadaNo ratings yet
- How To Use A BalanceDocument1 pageHow To Use A BalancehamaadaNo ratings yet
- Chitungwiza Central Hospital Laboratory DepartmentDocument2 pagesChitungwiza Central Hospital Laboratory DepartmenthamaadaNo ratings yet
- ABO Subgroups and Bombay GroupDocument15 pagesABO Subgroups and Bombay GrouphamaadaNo ratings yet
- ABO Forward TestingDocument2 pagesABO Forward TestinghamaadaNo ratings yet
- Cross-Matching: To Meet Wikipedia'sDocument5 pagesCross-Matching: To Meet Wikipedia'shamaadaNo ratings yet
- ABO Grouping ProcedureDocument2 pagesABO Grouping ProcedurehamaadaNo ratings yet
- Present VidasDocument24 pagesPresent Vidashamaada100% (1)
- Antibody IdentificationDocument27 pagesAntibody Identificationhamaada100% (2)
- 11-16 PaginaDocument40 pages11-16 Paginaclaudia ballester martinNo ratings yet
- Health Assessment: by Dr. Hala YehiaDocument115 pagesHealth Assessment: by Dr. Hala YehiaRazaCreciaLastrillaMenesesNo ratings yet
- 5 Living Things in Their Environment - 6 - People and Planet - QueDocument9 pages5 Living Things in Their Environment - 6 - People and Planet - Querashmi_harry100% (1)
- Biology - Local Heritage ThemesDocument5 pagesBiology - Local Heritage ThemesJerrycoNo ratings yet
- D D 5E Bestiary Journey Into The Realms PDFDocument7 pagesD D 5E Bestiary Journey Into The Realms PDFConnor GreenNo ratings yet
- Topic 4 Bio Peer Buddies AnsDocument3 pagesTopic 4 Bio Peer Buddies Ansamirahteaching95No ratings yet
- Manok Mabuhay (FINAL PAIR CASE)Document12 pagesManok Mabuhay (FINAL PAIR CASE)Eldon CalambaNo ratings yet
- MycologyDocument72 pagesMycologyDesa Refuerzo100% (1)
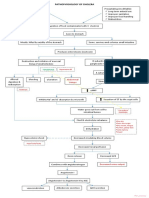
- Pathophysiology of Cholera PDFDocument1 pagePathophysiology of Cholera PDFRameshKrishnanNo ratings yet
- Bab Ii Tinjauan Teori: Benigna Prostatic Hyperplasia Adalah Pembesaran Jinak Kelenjar ProstatDocument27 pagesBab Ii Tinjauan Teori: Benigna Prostatic Hyperplasia Adalah Pembesaran Jinak Kelenjar Prostatdedi kurniawanNo ratings yet
- A Rough Guide To Drosophila Mating SchemesDocument39 pagesA Rough Guide To Drosophila Mating SchemesKirubes WaranNo ratings yet
- Anatomy of The Horse PDFDocument80 pagesAnatomy of The Horse PDFzemidahsalazarNo ratings yet
- Ujian Selaras 2 BI Paper 1Document9 pagesUjian Selaras 2 BI Paper 1Farah Anis IsmailNo ratings yet
- Evs Class 4 MDDocument3 pagesEvs Class 4 MDRohan DeopaNo ratings yet
- (The Natural History of The Crustacea) Les Watling, Martin Thiel (Eds.) - Functional Morphology and Diversity. 1-Oxford University Press (2013)Document515 pages(The Natural History of The Crustacea) Les Watling, Martin Thiel (Eds.) - Functional Morphology and Diversity. 1-Oxford University Press (2013)Yamaly Barragán MarínNo ratings yet
- Cell As A Unit of LifeDocument18 pagesCell As A Unit of LifeMohamad Abdul WahabNo ratings yet
- Teddy BearsDocument4 pagesTeddy BearsanaNo ratings yet
- Six Stages Four Levels San Jiao: ACR Class 5Document43 pagesSix Stages Four Levels San Jiao: ACR Class 5anon_70777627No ratings yet
- MenuDocument2 pagesMenuAlex ShparberNo ratings yet
- Coin 2023Document3 pagesCoin 2023samco.hienlvNo ratings yet
- A Detailed Lesson Plan in English 3Document10 pagesA Detailed Lesson Plan in English 3Mary Cres Deguma OtazaNo ratings yet
- BX Essentials - Cleric and Magic-User SpellsDocument37 pagesBX Essentials - Cleric and Magic-User SpellsArda Emirgeloğlu100% (2)
- GERUNDIODocument3 pagesGERUNDIOAntonio Javier Estaca AlarcónNo ratings yet
- DLL - English 4 - Q2 - W1Document5 pagesDLL - English 4 - Q2 - W1Allyza Fae DavidNo ratings yet
- BIP39 WordlistDocument1 pageBIP39 Wordlistcabal2979No ratings yet
- S1 1407010079 2018 JurnalDocument18 pagesS1 1407010079 2018 JurnalDaily Alman&momNo ratings yet