Noi Gmi A4 Postersx7
Noi Gmi A4 Postersx7
Uploaded by
Ar Hitesh ParmarCopyright:
Available Formats
Noi Gmi A4 Postersx7
Noi Gmi A4 Postersx7
Uploaded by
Ar Hitesh ParmarCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Noi Gmi A4 Postersx7
Noi Gmi A4 Postersx7
Uploaded by
Ar Hitesh ParmarCopyright:
Available Formats
2
N
e
u
r
o
O
r
t
h
o
p
a
e
d
i
c
I
n
s
t
i
t
u
t
e
|
w
w
w
.
n
o
i
g
r
o
u
p
.
c
o
m
w
w
w
.
g
r
a
d
e
d
m
o
t
o
r
i
m
a
g
e
r
y
.
c
o
m
The
Graded Motor Imagery
Handbook
G. Lorimer Moseley
David S. Butler
Timothy B. Beames
Thomas J. Giles
References
1/ Graded motor imagery is effective for long-standing
complex regional pain syndrome: a randomised controlled
trial., Moseley, G.L., Pain 2004
2/ Is successful rehabilitation of complex regional pain
syndrome due to sustained attention to the affected limb?
A randomised clinical trial. Moseley, G.L., Pain 2005
3/ Graded motor imagery for pathologic pain: A randomized
controlled trial. Moseley, G.L., Neurology 2006
4/ Does evidence support physiotherapy management of adult
Complex Regional Pain Syndrome Type One? A systematic
review. Daly, A. E., Biolocerkowski, A. E., European Journal
of Pain, 2008.
CONCLUSIONS: Graded motor imagery should be used
to reduce pain in adult CRPS-1 patients. Further, the results
of this review should be used to update the CRPS-1 clinical
guidelines.
Graded Motor Imagery
GMI is an individually tailored treatment process which has successfully been
used for persistent and complex pain states
1,2,3,4
. It aims to give exibility and
creativity back to the brain via graded exposure.
The Graded Motor Imagery Handbook,
Moseley GL, Butler DS, Beames TB, Giles TJ.
Noigroup Publications, Adelaide, Australia, 2012
2
N
e
u
r
o
O
r
t
h
o
p
a
e
d
i
c
I
n
s
t
i
t
u
t
e
|
w
w
w
.
n
o
i
g
r
o
u
p
.
c
o
m
w
w
w
.
g
r
a
d
e
d
m
o
t
o
r
i
m
a
g
e
r
y
.
c
o
m
What is normal?
Broad guidelines are:
You dont know you are
mentally moving
Premotor cells modify
primary motor cells
without activating them
Less likely to activate the
pain neurotag
Implicit Motor Imagery (left/right judgements)
References
Parsons LM., Integrating cognitive psychology, neurology and
neuroimaging. Acta Psychologica 2001;107:155-81.
Schwoebel J, Coslett HB, Bradt J, et al. Pain and the body
schema: effects of pain severity on mental representations of
movement. Neurology 2002;59:775-7.
Wallwork S, Butler DS, Darmawan I, et al., Motor Imagery
of the neck. Age, gender, handedness and image rotation
affect performance on a left/right neck rotation judgement
task. Submitted 2012.
Bowering J, Butler DS, Fulton I, et al., Implicit motor imagery
in people with a history of back pain, current back pain,
both or neither. Submitted 2012.
Aim for accuracy of 80% and above
Similar results for left and right (no bias)
Aim for response time (speed) of 1.6 seconds
+/- 0.5 seconds for necks and backs
Aim for response time (speed) of 2 seconds
+/- 0.5 seconds for hands and feet
Consistent over a period of at least a week
B - Acute left hand injury
looking at left hand
R
e
s
p
o
n
se time
R
e
s
p
o
n
se time
A
c
c
u
racy
A
c
c
u
racy
L
L
L
L
R
R
R
R
Wrong choice,
start again
Wrong choice,
start again
X
X
A
c
u
t
e
L
E
F
T
h
a
n
d
in
jury looking a
t R
IG
H
T
h
a
n
d
A
c
u
t
e
L
E
F
T
h
a
n
d
in
jury looking a
t L
E
F
T
h
a
n
d
C
h
r
o
n
i
c
L
E
F
T
h
a
n
d
in
jury looking
a
t R
IG
H
T
h
a
n
d
C
h
r
o
n
i
c
L
E
F
T
h
a
n
d
in
jury looking
a
t L
E
F
T
h
a
n
d
Acute
Chronic
A - Acute left hand injury
looking at right hand
C - Chronic left hand injury
looking at right hand
D- Chronic left hand injury
looking at left hand
A
B
C
D
Difcult decision,
Safest to presume its
LEFT hand because
my LEFT hand is
injured choose
LEFT hand
Mentally move
LEFT hand
Mentally
move RIGHT
hand
Correct!
Correct!
Mentally move
LEFT hand
Difcult decision,
Safest to presume
its LEFT hand
because my LEFT
hand is injured
choose LEFT hand
Difcult decision,
Safest to presume
its RIGHT hand
because my LEFT
hand is in trouble
and Im protecting it
by not focusing on it
Mentally move
RIGHT hand
Correct!
Difcult decision,
Safest to presume
its RIGHT hand
because my LEFT
hand is in trouble
and Im protecting it
by not focusing on it
Correct!
Mentally
move LEFT
hand
Mentally move
RIGHT hand
2
N
e
u
r
o
O
r
t
h
o
p
a
e
d
i
c
I
n
s
t
i
t
u
t
e
|
w
w
w
.
n
o
i
g
r
o
u
p
.
c
o
m
w
w
w
.
g
r
a
d
e
d
m
o
t
o
r
i
m
a
g
e
r
y
.
c
o
m
Where do I practice explicit motor imagery?
At home, work, school, on the bus, in the
bath?
Do I keep my eyes open or closed during
motor imagery?
What position do I adopt during imagery?
Sitting, standing, lying?
Do I think of myself moving (rst person) or
someone else moving
(third person)?
How long should I perform imagery for and
how many times a day?
What is the task complexity and intensity
and how does it tie in with grading my
exposure?
What words should the therapist use to
describe or talk through the process?
What words should the user think of when
going through the process?
What cues can be used to heighten the
process? Sounds, memories, smells?
Should there be prior demonstration of the
movement by another person (therapist,
family member)?
Do I use relaxation or meditation in
conjunction?
How much do I know about the changes in
the brain that I can achieve with imagery?
Thinking about moving without actually moving imagined movements.
There are many different ways to go through the process and the most common method used in GMI is a
rst person perspective of feeling your own movement and postures. Graded activation of the brain through
observation, imagining movements and actual movements.
Explicit Motor Imagery
References
Ehrson HH., et al,. Imagery of voluntary movement of ngers,
toes, and tongue activates corresponding body-part-
specic motor representations. J Neurophysiol. 2003
Nov;90(5):3304-16.
Ideas board
Observing
movement
Imagining
movement
Performing
movement
2
N
e
u
r
o
O
r
t
h
o
p
a
e
d
i
c
I
n
s
t
i
t
u
t
e
|
w
w
w
.
n
o
i
g
r
o
u
p
.
c
o
m
w
w
w
.
g
r
a
d
e
d
m
o
t
o
r
i
m
a
g
e
r
y
.
c
o
m
Using a mirror box
In this situation the problematic limb is hidden in the box.
Looking at the mirror image of the left limb gives the illusion
of seeing the hidden right limb.
Therapist as illusionist
Mirror therapy means looking into a mirror to see the reection of the limb or body
part in front of it. The mirror will effectively give the illusion that you are looking
at the limb that is hidden. Brain activation during mirror therapy is less than actual
movement but slightly more compared with imagining the same movement.
Mirror Therapy (1)
References
Diers M., et al. Mirrored, imagined and executed
movements differentially activate sensorimotor
cortex in amputees with and without phantom
limb pain. Pain 2010
2
N
e
u
r
o
O
r
t
h
o
p
a
e
d
i
c
I
n
s
t
i
t
u
t
e
|
w
w
w
.
n
o
i
g
r
o
u
p
.
c
o
m
w
w
w
.
g
r
a
d
e
d
m
o
t
o
r
i
m
a
g
e
r
y
.
c
o
m
Tips and examples of progression
for using a mirror box
Mirror Therapy (2)
Keep the hand still/resting in a comfortable position Keep the hand still/resting in the same position as
the hand in the box just observe the refection
INSIDE THE BOX OUTSIDE THE BOX
More
sensitive
Rotate the hand Keep the hand still/resting
Oppose each fnger separately Keep the hand still/resting
Bend the wrist up and down through its full range of movement Bend the wrist up and down within the limit of pain
Oppose the fngers and press with some force together Oppose the fngers and gently touch together
Make a fst and squeeze in repetitions Make a fst, pushing into some discomfort.
Then repeat in time with the hand outside the box
Copy the hand in the box through a full range of movement Rotate the hand and wrist fully
Copy the hand in the box Move both hands fully and include some extra tasks,
e.g., squeezing a ball or writing
Copy the hand in the box Include tools that are more threatening such as a knife
Less
sensitive
Make a fst then slowly relax; repeat Keep the hand resting with a slight bend in the fngers
2
N
e
u
r
o
O
r
t
h
o
p
a
e
d
i
c
I
n
s
t
i
t
u
t
e
|
w
w
w
.
n
o
i
g
r
o
u
p
.
c
o
m
w
w
w
.
g
r
a
d
e
d
m
o
t
o
r
i
m
a
g
e
r
y
.
c
o
m
A graded approach for treating pain
It appears necessary that GMI is offered in a sequential manner. A strong grounding in the
science underpinning GMI is essential for all users to be able to decide best when to move
forwards, sideways or backwards through the treatment process.
The ideal sequential progression of the different elements of graded motor imagery:
GMI: a graded approach (1)
Left/right
discrimination
Explicit
motor imagery
Mirror
therapy
Regain
function
Watching
movements
Is this a left
or right
movement?
Imagining
moving, touching
and feeling
Enriching my
experience by using
a mirror, diferent
moods, circumstances,
places
Am I standing on
a balance beam, in
tall grass or on the
beach?
Using mirrors
I can trick my
brain
How do my
clothes feel on
my skin?
Backs and necks
are twisting
which way?
Is this a left or
a right side?
2
N
e
u
r
o
O
r
t
h
o
p
a
e
d
i
c
I
n
s
t
i
t
u
t
e
|
w
w
w
.
n
o
i
g
r
o
u
p
.
c
o
m
w
w
w
.
g
r
a
d
e
d
m
o
t
o
r
i
m
a
g
e
r
y
.
c
o
m
GMI: a graded approach (2)
Left/right
judgements
Hands and feet
2 minutes every
waking hour
Left/right
judgements
Feet only
1 minute every
waking hour
Watching
Sitting in a cafe watching the
other diners
Increase 1 minute per day
~
Piano movies, sister typing,
Indian dancing
5 minutes x 5 per day
Left/right
judgements
Hands and feet
10 images / hour
Increase by 1 image
every day
Explicit motor
imagery
Hands and
feet
10 images/hr
Increase by 1
image per day
Mirror therapy
Hands and feet
5 minutes/hour
Increase by 1
minute every day
0
1
2
3
4
5
6
7
8
9
10
0 - 2 weeks 3 - 4 weeks 5 - 11 weeks 12 - 14 weeks 15 - 17 weeks 18 - 20 weeks
Pain on movement
Resting pain
A case study
Lucy Loo presented with marked CRPS
affecting her arm, leg and face. We treated
her with GMI for two minutes every waking
hour for the rst two weeks. Her pain
worsened. You can see this by the slightly
upward trajectory of the diamonds, which
reect pain on movement of her thumb, and
the circles, which reect pain at rest.
We then reduced her training and worked
on GMI of the feet instead. Two weeks later
no worse but really no better. We then
did some motor empathy we asked her
to watch movies of people playing on the
piano, watching her sisters hands as she
typed at the computer, and to watch other
movements. She clearly began to improve.
We progressed that, spending more time and
watching more functional activities, for seven
weeks. Then we tried GMI again and this
time she responded.
It took another nine weeks to get through
the GMI programme, but at 20 weeks
after the initial appointment, Lucy started
functional exposure. Six months later she
had only a small amount of pain when she
worked with her hands for half an hour or so.
The trick with her? We had to get under
the radar by abandoning GMI and starting
instead with motor and functional empathy.
You might also like
- Explain Pain SuperchargedDocument246 pagesExplain Pain SuperchargedGUSTAVO100% (8)
- Cellular HealingDocument1 pageCellular HealingAr Hitesh Parmar100% (3)
- Musculoskeletal Clinical Translation FrameworkDocument1 pageMusculoskeletal Clinical Translation FrameworkRafaelNo ratings yet
- Graded Motor ImageryDocument82 pagesGraded Motor Imageryvalitahmia100% (1)
- Explain Pain Supercharged Chapter PreviewDocument7 pagesExplain Pain Supercharged Chapter Previewgimnasio kineNo ratings yet
- Tim Cocks - Graded Motor ImageryDocument38 pagesTim Cocks - Graded Motor ImagerygabitorNo ratings yet
- Workbook 031512 With Cover PDFDocument197 pagesWorkbook 031512 With Cover PDFIndah Yulantari100% (2)
- Pain Science: How To Talk To Your Patients When They Are Hurting 07.07.16Document22 pagesPain Science: How To Talk To Your Patients When They Are Hurting 07.07.16Phil Watson100% (4)
- Spinal Cord Injuries and FeldenkraisDocument35 pagesSpinal Cord Injuries and Feldenkraisextratorrential100% (5)
- Daat12i2p394conversion Disorder and Physical TherapyDocument4 pagesDaat12i2p394conversion Disorder and Physical Therapydonleo153100% (1)
- NATA 2015 Presentation - Dan Houglum PDFDocument77 pagesNATA 2015 Presentation - Dan Houglum PDFRaunaq Salat100% (1)
- Achieving Oneness With The Higher Soul: Know Yourself Through Meditation and Experience Inner Peace & Bliss..Document2 pagesAchieving Oneness With The Higher Soul: Know Yourself Through Meditation and Experience Inner Peace & Bliss..Ar Hitesh ParmarNo ratings yet
- Usui Shiki Ryoho: Your Name Here Reiki Master/TeacherDocument1 pageUsui Shiki Ryoho: Your Name Here Reiki Master/TeacherAr Hitesh ParmarNo ratings yet
- Healing A BusinessDocument2 pagesHealing A BusinessAr Hitesh Parmar100% (7)
- Case Study Cerebral InfarctDocument11 pagesCase Study Cerebral InfarctRodel MorlaNo ratings yet
- Reading B2 All DocumentsDocument18 pagesReading B2 All Documentsgaby1680No ratings yet
- Releasing the Rotator Cuff: A complete guide to freedom of the shoulderFrom EverandReleasing the Rotator Cuff: A complete guide to freedom of the shoulderNo ratings yet
- L Gifford Tissue and Input Related MechanismsDocument10 pagesL Gifford Tissue and Input Related MechanismsRoar SyltebøNo ratings yet
- Pain Science Patient and Therapist Workbook January 2015Document31 pagesPain Science Patient and Therapist Workbook January 2015gabitor100% (1)
- The Effect of Manual Therapy and Neuroplasticity Education On Chronic Low Back Pain: A Randomized Clinical TrialDocument9 pagesThe Effect of Manual Therapy and Neuroplasticity Education On Chronic Low Back Pain: A Randomized Clinical TrialAlvaro Alarcon ValenzuelaNo ratings yet
- Gmi PDFDocument71 pagesGmi PDFAlma GlinacNo ratings yet
- Angela Hand and Upper ExtremityDocument59 pagesAngela Hand and Upper ExtremityJenny RajanNo ratings yet
- Chapter 7 - Management of The Hypermobile AdultDocument19 pagesChapter 7 - Management of The Hypermobile AdultDavid MansoNo ratings yet
- Tom J Sciatica SlidesDocument45 pagesTom J Sciatica Slidesgemichan26100% (1)
- Bodily Relearning Chapter 1 Sample 1Document11 pagesBodily Relearning Chapter 1 Sample 1Auxilio MedesmayoNo ratings yet
- Home Hand Exercise Program PDFDocument5 pagesHome Hand Exercise Program PDFAleksaNo ratings yet
- Piriformis ExercisesDocument8 pagesPiriformis ExercisesVENKATESH PAINo ratings yet
- Clinical Neurodynamics and Sports Medicine: Origins and DevelopmentDocument8 pagesClinical Neurodynamics and Sports Medicine: Origins and DevelopmentWahid NasrudinNo ratings yet
- Rehabilitation of Shoulder Arthroplasty ModulDocument36 pagesRehabilitation of Shoulder Arthroplasty ModulvirginiaNo ratings yet
- Spine Rehabilitation in 2022 and BeyondDocument276 pagesSpine Rehabilitation in 2022 and BeyondAhmed Abdel MoneimNo ratings yet
- Nds Lower Quarter Course Manual PDFDocument105 pagesNds Lower Quarter Course Manual PDFMskola Karlovac100% (1)
- ApproachDocument37 pagesApproachAshu AshNo ratings yet
- Evidence-Based Evaluation & Management of Common Spinal Conditions: A Guide for the Manual PractitionerFrom EverandEvidence-Based Evaluation & Management of Common Spinal Conditions: A Guide for the Manual PractitionerRating: 5 out of 5 stars5/5 (1)
- Unlocking Pathways of Pain: Stories of Innovative Treatments and How They WorkFrom EverandUnlocking Pathways of Pain: Stories of Innovative Treatments and How They WorkNo ratings yet
- McKenzie ExplainedDocument4 pagesMcKenzie ExplainedEd BegsNo ratings yet
- Mulligan Concept of Manual TherapyDocument2 pagesMulligan Concept of Manual TherapySuMitra MohaNtyNo ratings yet
- Tendon Neuroplastic TrainingDocument8 pagesTendon Neuroplastic TrainingFrantzesco KangarisNo ratings yet
- Lumbar Strain: Dr. Lipy Bhat PT Faculty, Physiotherapy SrhuDocument38 pagesLumbar Strain: Dr. Lipy Bhat PT Faculty, Physiotherapy SrhuKapil LakhwaraNo ratings yet
- Movement System Impairment SyndromesDocument37 pagesMovement System Impairment SyndromesChris0% (1)
- MOVIMIENTO Gray Cook Assessing Movement Part One TranscriptDocument22 pagesMOVIMIENTO Gray Cook Assessing Movement Part One TranscriptFranco Suazo MoralesNo ratings yet
- Front Matter - 2020 - Guccione S Geriatric Physical Therapy PDFDocument1 pageFront Matter - 2020 - Guccione S Geriatric Physical Therapy PDFGamalia Marta0% (1)
- Roja Ramani Vasamshetty MPT IiDocument37 pagesRoja Ramani Vasamshetty MPT Iideepuphysio100% (3)
- Bogduk 2009Document3 pagesBogduk 2009Borys100% (1)
- Upper Extremity Toolkit 2017Document66 pagesUpper Extremity Toolkit 2017lolocy LNo ratings yet
- Physical Therapy Protocols For The Conditions of Hip RegionDocument50 pagesPhysical Therapy Protocols For The Conditions of Hip RegionAnita GajariNo ratings yet
- 10.A.Cools Kinetic Chain PDFDocument22 pages10.A.Cools Kinetic Chain PDFWalter PelaezNo ratings yet
- Examination of The Shoulder The Complete Guide PDFDocument2 pagesExamination of The Shoulder The Complete Guide PDFJasmine0% (2)
- Lumbopelvic Stability: SyllabusDocument13 pagesLumbopelvic Stability: Syllabusrapannika100% (3)
- Stroke UE ToolkitDocument69 pagesStroke UE ToolkitWhitney JosephNo ratings yet
- List of Common Compensation Patterns and Movement Dysfunctions - PreHab ExercisesDocument17 pagesList of Common Compensation Patterns and Movement Dysfunctions - PreHab ExercisesEmiliano BezekNo ratings yet
- Shoulder HEPDocument4 pagesShoulder HEPomboNo ratings yet
- Dermoneuromodulation Rev 03Document57 pagesDermoneuromodulation Rev 03dasamoro100% (1)
- McKenzie Classification of Mechanical Spinal PainDocument7 pagesMcKenzie Classification of Mechanical Spinal PainVictor Andrés Olivares Ibarra100% (2)
- PNF PatternsDocument19 pagesPNF PatternsDany VirgilNo ratings yet
- Explaining Pain Science: What We Know and Who Can HelpDocument53 pagesExplaining Pain Science: What We Know and Who Can HelpSara DuranNo ratings yet
- Know Pain, Know GainDocument4 pagesKnow Pain, Know GainCarlos Millan PerezNo ratings yet
- Eyal Lederman - Process Approach in PTDocument72 pagesEyal Lederman - Process Approach in PTYuldash100% (1)
- Integrando Terapia Manual e Neurociencia Da DorDocument274 pagesIntegrando Terapia Manual e Neurociencia Da DorÁtila Hanemann100% (1)
- Postural Exercises On The Foam RollDocument3 pagesPostural Exercises On The Foam RollTomBrambo100% (1)
- Role of Physio in Neurological Disorders.Document17 pagesRole of Physio in Neurological Disorders.Maheen AnwaarNo ratings yet
- Subsystems of BodyDocument30 pagesSubsystems of BodyAjishAbrahamNo ratings yet
- Instructions For Filling & Submission of Online Application Form For RegistrationDocument3 pagesInstructions For Filling & Submission of Online Application Form For RegistrationAr Hitesh ParmarNo ratings yet
- Concrete Preplacement ChecklistDocument5 pagesConcrete Preplacement ChecklistAr Hitesh ParmarNo ratings yet
- Spirit Science Guide To CrystalsDocument2 pagesSpirit Science Guide To Crystalsstudmuffin8558100% (1)
- Gujarati Books AddressDocument1 pageGujarati Books AddressAr Hitesh ParmarNo ratings yet
- Diploma 2Document1 pageDiploma 2Ar Hitesh ParmarNo ratings yet
- Gujarati Books AddressDocument1 pageGujarati Books AddressAr Hitesh ParmarNo ratings yet
- Spiritual Seeker - Access Bars - A Not-So-Great ExperienceDocument4 pagesSpiritual Seeker - Access Bars - A Not-So-Great ExperienceAr Hitesh Parmar60% (5)
- Irctcs E Ticketing Service Electronic Cancellation Slip (Personal User)Document2 pagesIrctcs E Ticketing Service Electronic Cancellation Slip (Personal User)Ar Hitesh ParmarNo ratings yet
- Lead Generation TacticsDocument19 pagesLead Generation TacticsAr Hitesh ParmarNo ratings yet
- Company Turnover in Crores 2015 2014 2013 2012 2011 2010 Amway 2288Document2 pagesCompany Turnover in Crores 2015 2014 2013 2012 2011 2010 Amway 2288Ar Hitesh ParmarNo ratings yet
- Vestige Products India Price List - Vestige Business and MarketingDocument5 pagesVestige Products India Price List - Vestige Business and MarketingAr Hitesh Parmar100% (9)
- 6 - Diary of A Wimpy Kid - Cabin FeverDocument228 pages6 - Diary of A Wimpy Kid - Cabin FeverTobith Tobith100% (1)
- Dimensions Basement Door PDFDocument1 pageDimensions Basement Door PDFaskjhd askdhjaNo ratings yet
- User's Handbook For IC4Document61 pagesUser's Handbook For IC4grr100% (1)
- Operation Manual Dse 5220Document32 pagesOperation Manual Dse 5220Jose TomassettiNo ratings yet
- CBRN TeamDocument30 pagesCBRN TeamDinesh YadavNo ratings yet
- AAIR BOA - Complete File - November 23Document54 pagesAAIR BOA - Complete File - November 23Rex LimNo ratings yet
- World of Animals - Issue 3 "A Tiger's Tale"Document9 pagesWorld of Animals - Issue 3 "A Tiger's Tale"International Fund for Animal WelfareNo ratings yet
- Sekolah Menengah Kebangsaan Sungai Layar, 08000 SG Petani, KedahDocument4 pagesSekolah Menengah Kebangsaan Sungai Layar, 08000 SG Petani, KedahAsoda VaNo ratings yet
- Class II AS - 2023-24Document7 pagesClass II AS - 2023-24محمدضيأ الدينNo ratings yet
- E3-E4 - PPT - Chapter 2. Intepersonal SkillDocument13 pagesE3-E4 - PPT - Chapter 2. Intepersonal SkillericmscNo ratings yet
- Watch John Holmes Shoot His Comedy Wad: Hot & Saucy Pizza GirlsDocument18 pagesWatch John Holmes Shoot His Comedy Wad: Hot & Saucy Pizza GirlsYouWeirdTube1No ratings yet
- Photon BrochureDocument1 pagePhoton Brochureshwetha281889242No ratings yet
- Roche 9180 Electrolyte Analyzer User ManualDocument158 pagesRoche 9180 Electrolyte Analyzer User Manualunclebk100No ratings yet
- June Accounting QuestionsDocument6 pagesJune Accounting QuestionsallhomeworktutorsNo ratings yet
- PCT Q&aDocument10 pagesPCT Q&aOke OluwafemiNo ratings yet
- Investor ReportDocument36 pagesInvestor ReportAlexandre CauetNo ratings yet
- Hostel Management SystemDocument11 pagesHostel Management SystemMaryamNo ratings yet
- The History of The Integrated CircuitDocument38 pagesThe History of The Integrated CircuitDwaipayan BhattacharyaNo ratings yet
- Mothers LoveDocument45 pagesMothers LovePoonamSidhu53% (19)
- MplsDocument124 pagesMplsmgitecetechNo ratings yet
- Teaching Profession Activities On Modules 1 2Document9 pagesTeaching Profession Activities On Modules 1 2Ana Lea AlmazanNo ratings yet
- Lesson Plan Budgeting 2 2Document2 pagesLesson Plan Budgeting 2 2Alexander QuemadaNo ratings yet
- Lecture 22CAs20Document29 pagesLecture 22CAs20mzNo ratings yet
- 2Js Coffee Shop FS FinalDocument75 pages2Js Coffee Shop FS FinalRascel SumalinogNo ratings yet
- Foreign Language 101Document2 pagesForeign Language 101Fanwa MichaelNo ratings yet
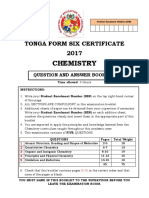
- F6 Chemistry 2017Document15 pagesF6 Chemistry 2017LitiaMikoNo ratings yet
- Production of Transgenic Goats Expressing Human Coagulation Factor IX in The Mammary Glands After Nuclear Transfer Using Transfected Fetal Fibroblast CellsDocument9 pagesProduction of Transgenic Goats Expressing Human Coagulation Factor IX in The Mammary Glands After Nuclear Transfer Using Transfected Fetal Fibroblast CellsMaira QuintanaNo ratings yet
- Overflow12 PDFDocument11 pagesOverflow12 PDFTayyaba NafeesNo ratings yet