0 ratings0% found this document useful (0 votes)
32 viewsShigella Infections in Children: New Insights: Shai Ashkenazi, MD, MSC
Shigella Infections in Children: New Insights: Shai Ashkenazi, MD, MSC
Uploaded by
merrycardinashigell
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Shigella Infections in Children: New Insights: Shai Ashkenazi, MD, MSC
Shigella Infections in Children: New Insights: Shai Ashkenazi, MD, MSC
Uploaded by
merrycardina0 ratings0% found this document useful (0 votes)
32 views7 pagesshigell
Original Title
Shigella n
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
shigell
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
32 views7 pagesShigella Infections in Children: New Insights: Shai Ashkenazi, MD, MSC
Shigella Infections in Children: New Insights: Shai Ashkenazi, MD, MSC
Uploaded by
merrycardinashigell
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 7
Shigella Infections in Children: New Insights
Shai Ashkenazi, MD, MSc
Shigellosis, the acute enteric infection caused by bacteria of the genus Shigella, has a
worldwide distribution with an estimated annual incidence of 164.7 million cases, of which
163.2 million occur in developing countries, and 1.1 million deaths. Sixty-nine percent of all
episodes and 61 percent of all Shigella-related deaths involve children younger than 5
years old. In the United States, 10,000 to 15,000 cases of shigellosis are reported each
year. Although usually conned to the colonic mucosa, shigellosis sometimes can cause
extraintestinal complications. Recent publications have shed light on the clinical charac-
teristics of Shigella-induced bacteremia, surgical complications, urogenital symptoms, and
neurologic manifestations, and on the unique manifestations in the neonatal period. The
mainstay of treatment of shigellosis in children is correction of the uid and electrolyte
loss, which often is achieved by the administration of oral rehydration solutions. Appro-
priate antibiotic therapy shortens the duration of both clinical symptoms and fecal excretion
of the pathogen. However, the increasing antimicrobial resistance of shigellae worldwide
constitutes a major problem. Regarding the pathophysiology of shigellosis and its compli-
cations, recent data not only elucidated the molecular mechanisms involved but also linked
manifestations of disease to the interplay of bacterial virulence factors and host responses.
The improved understanding of the pathophysiology is hoped to lead to innovative thera-
peutic approaches against shigellosis and new generations of vaccine candidates.
Semin Pediatr Infect Dis 15:246-252 2004 Elsevier Inc. All rights reserved.
S
higella is a genus of gram-negative bacilli that causes hu-
man gastrointestinal infections, sometimes with extraint-
estinal manifestations.
1
Four species (serogroups) are dened
on the basis of serologic or biochemical reactions, namely,
Shigella dysenteriae, serogroup A; Shigella exneri, serogroup
B; Shigella boydii, serogroup C; and Shigella sonnei, serogroup
D.
1,2
Species classication has important therapeutic impli-
cations because the species differ in both geographic distri-
bution and antimicrobial susceptibility.
1,3-5
In developed
countries, S. sonnei is the most common species; reports from
several locations showan increase in its relative prevalence in
the last several years.
2,4,6-9
In developing countries, S. exneri
is most common, with outbreaks that often are caused by S.
dysenteriae.
1,2,9
The serogroups are further classied into at
least 37 serotypes and 13 subserotypes.
1,2
To determine the global burden of Shigella infections,
Kotloff and coworkers
9
analyzed published reports from var-
ious locations and then estimated the number of cases world-
wide according to the worlds population as categorized into
developed and developing countries and into age groups.
9
They found that the annual number of Shigella episodes
throughout the world was 164.7 million, of which 163.2
million occurred in developing countries, with 1.1 million
deaths.
9
Sixty-nine percent of episodes and 61 percent of all
shigellosis-related deaths involved children younger than 5
years of age. According to surveillance reports of the Centers
for Disease Control and Prevention, 10,000 to 15,000 cases
of shigellosis have been documented each year during the last
30 years in the United States, for annual incidence rates of 5
to 10 per 100,000.
7
During this period, the relative preva-
lence of S. sonnei, the most common species, has increased.
7
This increase also was noted in other locations.
4,6,8
Shigella infection spreads by the fecal-oral route. Because
of the low infectious dose10 to 100 organismsperson-
to-person transmission probably is the most common.
1,8
However, transmission by contaminated food, drinking wa-
ter, swimming pools, and ies also has been documented.
2,10
The highest incidence of shigellosis is in young children,
usually those 1 to 5 years old.
2-4,8,9
Recent studies have shed
new light on the pathophysiologic, clinical, therapeutic, and
preventive aspects of Shigella infection in children. They are
discussed in detail below.
Department of Pediatrics A, Schneider Childrens Medical Center of Israel;
FMRC, Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel.
Address reprint requests to: Shai Ashkenazi, MD, Professor of Pediatrics,
Director, Department of Pediatrics A, Schneider Childrens Medical Cen-
ter of Israel, 14 Kaplan Street, Petah Tikva 49202, Israel. E-mail:
ashai@post.tau.ac.il.
246 1045-1870/04/$-see frontmatter 2004 Elsevier Inc. All rights reserved.
doi:10.1053/j.spid.2004.07.005
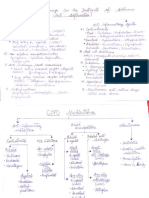
Pathophysiology
A key element in the pathogenesis of shigellosis is the ability
of the bacteria to invade colonic mucosa. The invasion pro-
cess depends on a 210- to 220-Kb plasmid, which is neces-
sary, but not sufcient, for full virulence.
2,10,11
New data not
only have elucidated the molecular mechanisms involved but
also have revealed that manifestations of disease depend on
the interplay of bacterial virulence factors and host re-
sponses, which results in inammation.
12,13
In addition, new
insights have been reported on the cellular and molecular
effectors of the innate immune system that eradicate the bac-
teria during primary infection and prevent systemic dissem-
ination, sometimes at the price of local tissue destruction in
the colon.
11,14-16
Shigella Determinants
of Pathogenicity
Virulence Plasmid
Sequencing the virulence plasmid of the S. exneri 5a strain
M90T has allowed investigators to identify the genes encod-
ing approximately 25 proteins secreted by the type III secre-
tion system.
16
This secretion system, like that in some other
gram-negative bacteria, translocates the Shigella effector mol-
ecules from the bacterial cytoplasm to the membrane and
cytoplasmof the host cell.
17
A31-kb segment of the virulence
plasmid, called the entry region or ipa/mxi-spa locus, com-
prises the pathogenicity island, which actually is sufcient for
entry of Shigella into intestinal epithelial cells, for apoptotic
death of macrophages, and for activation of polymorphonu-
clear leukocytes.
18,19
The island is organized into two diver-
gently transcribed operons.
15,18
One of the regions of the virulence plasma that is most
extensively studied is the invasive plasmid antigen (ipa) re-
gion.
11,18
It contains four genes, ipaA to ipaD, that encode
four proteins, IpaA to IpaD, necessary for invasion.
11,16,20
After the shigellae contact the host cells, IpaB and IpaC are
inserted as a single complex into the host membrane to form
a 25A pore, through which the other invasive proteins are
transported.
21
IpaB is essential for inducing apoptosis in mac-
rophages;
13
IpaB combined with IpaC, together with cyto-
plasmic chaperon IpgC, are required for lysis of the cell mem-
brane, which is needed for cell-to-cell spread.
22
The icsA (virG), virK, and sopA (icsP) genes play a role in
the ability of shigellae to move within the cytoplasm of in-
fected cells and to spread to other cells.
23
They encode, re-
spectively, the outer membrane protein directly involved in
intracellular spread,
24
the protein required for proper local-
ization of icsA,
25
and the outer membrane protease that
causes cleavage of icsA.
26
The virF gene regulates the virB
locus, which is required for positive regulation of the ipa
genes. The inv region is required for orientation of the Ipa
proteins into the outer membrane of the bacteria.
11,27
The
function of the 5-copy ipaH gene has not been claried yet.
Chromosomal Genes
Several chromosomal loci participate in the pathogenic pro-
cess by complementing the core virulence of the invasion
plasmid genes and are, therefore, needed for full virulence.
They can be categorized into two groups:
1. Genes regulating the expression of the plasmid viru-
lence genes. The virR gene encodes a histone-like mol-
ecule controlling the temperature-dependent expres-
sion of the Ipa and Mxi-Spa proteins, and the
keratoconjunctivitis provocation (kcpA) gene posi-
tively regulates virG.
11,28
2. Genes needed for bacterial survival in the intestine and
for resisting host defense mechanisms, such as those
encoding lipopolysaccharides (LPS) and siderophores.
Shigellae lacking complete LPS (rough colonies) are
avirulent.
2
Shigella Toxins
Shiga toxin, encoded chromosomally and found mainly in S.
dysenteriae serotype 1, is a potent protein-synthesis inhibitor
that targets primarily the vascular endothelium.
29,30
This
toxin mediates the severe complication of hemolytic-uremic
syndrome.
29,31
A similar syndrome may be seen after infec-
tions with enterohemorrhagic Escherichia coli, which produce
closely related toxins.
30,31
In addition, Shiga toxin might play
a role in the increased duration and severity of the diarrhea
caused by S. dysenteriae serotype 1.
2,32
Shigella spp. also produce two enterotoxins, ShET-1 and
ShET-2.
33
ShET-1 is produced mainly by S. exneri serotype
2a, whereas ShET-2 is produced by all Shigella spp.
33
These
enterotoxins may contribute to the high-volume, watery di-
arrhea often seen in the initial stages of the disease.
Host Responses
to Shigella Infection
Interactions of shigellae with host cells trigger inammatory
responses that lead to the histopathological changes that oc-
cur in the gut and the clinical presentation of shigellosis.
12,15
Cytokine and chemokine responses have been shown by im-
munohistochemistry studies of rectal samples both in the
sera and locally.
12,34
Although host responses cause the in-
ammation, they also are mandatory for controlling the in-
fection.
16
In a murine model, natural killer cell-mediated
interferon-gamma production was found to be essential for
host resistance to shigellosis.
14
Because the responses of the
various host cells to Shigella infection are somewhat distinct,
they are discussed briey below.
Shigella and Intestinal Epithelial Cells
Shigellae cross the colonic epithelium through M cells in the
follicle-associated epitheliumoverlying the Peyer patches.
2,15
At the dome area of the lymphoid follicle, the bacteria are
phagocytized by macrophages, which are killed by apopto-
sis.
13,35
With this strategy, shigellae reach the subepithelial
tissue and invade the colonic epithelial cells through their
Shigella infections in children 247
basolateral surface.
11
During the initial step of the entry pro-
cess, shigellae induce actin polymerization in the epithelial
cells with the formation of lopodes.
36
The process involves
activation of the Rho family of GRPases.
36,37
After entry, the
bacteria disrupt their membrane-bound vacuole, proliferate
in the cytoplasm, and use the actin-based motility, which is
dependent on the IcsA (virG) protein.
11,38
This process en-
ables their spread to neighboring cells by the formation of
nger-like protrusions.
15
In addition, intracellular shigellae
programthe colonic epithelial cells to express pro-inamma-
tory cytokines, such as interleukin (IL)-6 and IL-8, augment-
ing the local inammation.
12,39,40
Shigella and Macrophages
After crossing the colonic epithelium through the M cells,
shigellae are taken up by local macrophages. They later es-
cape fromthe phagosome and within 2 hours induce apopto-
sis of the macrophages and an inammatory reaction.
13,35,40
IpaB protein mediates the apoptosis by binding to caspase-1
or IL-1--converting enzyme, which cleaves the proinam-
matory cytokines IL-1- and IL-18 into their mature
form.
13,41
This inammatory response has been shown to be
important for eradicating the infection.
15
Shigella and Leukocytes
The massive recruitment of polymorphonuclear leukocytes is
mediated mainly by postinvasion intracellular Shigella LPS
via transcription factors.
15
The Shigella LPS also induce the
trafcking of toll-like receptor 4 (TLR4), the dominant me-
diator of the innate immune response.
16,42
The leukocyte
transmigration disrupts the intestinal epithelium.
15
Although
this disruption initially contributes to virulence by aiding
bacterial invasion, it actually limits the infection to the mu-
cosa and submucosa and ultimately eradicates it because the
bacteria are killed by polymorphonuclear leukocytes. This
process has been well demonstrated in the severe combined
immunodeciency decient mouse-human intestinal xeno-
graft model.
43
Clinical Features
Symptoms appear abruptly after an incubation period of 12
hours to approximately 2 days and include high fever, gen-
eralized toxicity, anorexia, nausea, crampy abdominal pain,
and diarrhea.
1,3,10
Typically, the diarrhea initially consists of
high-volume watery stools (small bowel disease), which may
be followed by frequent, small-volume, bloody, mucous
stools associated with urgency and painful defecation (large
bowel disease).
1,10
In children, most cases (50%) never
progress to bloody stools, although in some patients, the
initial stools are bloody.
1,3,10
Extraintestinal Complications of Shigellosis
Shigella Bacteremia
Although usually conned to the colonic mucosa, shigellosis
sometimes can cause extraintestinal complications. Bactere-
mia or septicemia rarely occurs during shigellosis and has
been reported mainly in developing countries.
2,44
For exam-
ple, according to one study from Bangladesh, 4 percent of
patients with shigellosis had Shigella bacteremia.
44
Bactere-
mia occurred more frequently in malnourished young infants
and in patients infected with S. dysenteriae serotype 1, and it
was associated with a signicant mortality rate. A recent
study from southern Israel described 15 children with Shi-
gella bacteremia.
45
Mean age was 20 months; 13 patients
(87%) failed to gain weight. Most (87%) of the isolates were
S. exneri, and none was S. dysenteriae serotype 1. No deaths
were reported.
45
Of note is that in patients with acquired
immunodeciency syndrome (AIDS),
46
shigellosis is not only
more common and more severe, but it also more often is
associated with bacteremia.
47,48
Surgical Complications
Miron and coworkers
49
reviewed reports published during a
40-year period of 57 children with surgical complications of
shigellosis. The complications were categorized into four
groups: appendicitis with or without perforation (n 16,
28%); colonic perforation (n 10, 17%); intestinal obstruc-
tion (n 30, 53%); and intraabdominal abscesses (n 1,
2%).
49
Thirteen children (23%) died, often despite having
received antimicrobial therapy. Many of the reports were
from developed countries.
49
Pediatricians should be alerted to the risk of surgical com-
plications of shigellosis, despite their rarity, because of the
signicant morbidity and mortality associated with a delayed
diagnosis. Establishing a diagnosis often is hampered by the
overlap of the signs and symptoms of shigellosis with those of
peritonitis.
49
Some authors recommend avoiding laparotomy
in the acute phase, even if signs of peritonitis are present,
unless the patient has evidence of perforation.
49
Nonetheless,
the pediatric surgeon should be consulted as soon as perito-
nitis is suspected.
Neurologic Manifestations
The neurologic manifestations of shigellosis usually are asso-
ciated with a favorable outcome, although a study from Ban-
gladesh noted a 29 percent mortality rate in affected children
compared with 6 percent in those without neurologic symp-
toms.
50
Seizures are the most common neurologic manifes-
tation, followed by lethargy and disorientation or coma,
which often are referred to as encephalopathy.
1,50,51
In the
minority of patients, the encephalopathy may be severe, un-
responsive to antibiotic therapy, and fatal, even in developed
countries.
52
The pathogenesis has not been elucidated. In
developed countries, where hypoglycemia and electrolyte ab-
normalities do not play a signicant pathogenic role, hypo-
natremia and early development of brain edema have been
reported.
50,51,53
Complementary studies in a murine model
documented the early development of brain edema and the
major pathogenetic role of host response factors, such as
tumor necrosis factor alpha, IL-1, and nitric oxide produc-
tion.
54-56
248 S. Ashkenazi
Urogenital System
Although rare occurrences, vulvovaginitis and urinary tract
infections caused by Shigella spp. are well-documented.
2,57
Recent publications from developed countries highlight the
problems in establishing the diagnosis and treating this in-
fection.
57,58
One case report fromthe United States described
a prepubertal child with chronic vulvovaginitis caused by S.
exneri.
58
Vaginal discharge and bleeding were the present-
ing symptoms. Nonspecic vulvovaginitis and hemorrhagic
cystitis initially were suspected, delaying the diagnosis. Fur-
thermore, several empiric antimicrobial courses failed be-
cause of the antimicrobial resistance of the pathogen. Finally,
after 3 years, 14-day treatment with ciprooxacin led to res-
olution of the vaginal discharge. In another study, resistant S.
sonnei caused a urinary tract infection that was cured only
after treatment with a third-generation cephalosporin.
57
Thus, because of the rarity of their infections, their diagnoses
often are delayed, and because of the antibiotic resistance of
Shigellae, empiric therapy often fails.
57,58
Neonatal Shigellosis
Arecent publication emphasized the unique problemof shig-
ellosis in the neonatal period.
59
Newborn infections account
for only 0.6 percent of all cases of shigellosis in the 0- to
10-year age group. Only 1.6 percent of all infants exposed to
the infection become ill.
2,4,59
This nding is explained by the
presence of maternal protective factors that pass through the
placenta or are transferred during breastfeeding.
2,60
Neonates with shigellosis may have only low-grade fever
with mild diarrhea, often not bloody. Complications, how-
ever, occur more commonly than in older children and in-
clude septicemia, meningitis, dehydration, colonic perfora-
tion, and toxic megacolon.
59
The mortality rate also is twice
as high as in older children, reaching 30 to 40 percent in
developing countries, although less than 1 percent in devel-
oped regions.
59
On logistic regression analysis, predictors
of infant mortality in developing countries were gram-
negative bacteremia, hyponatremia, hypoproteinemia, and
ileus.
59
Diagnosis
Stool culture to isolate the pathogen is still the cornerstone of
diagnosis.
2
This technique, however, has certain limitations:
it takes a few days, the organisms may not survive transpor-
tation, sensitivity is not higher than 80 percent, and the cul-
ture may become negative in children given previous antibi-
otic therapy.
2
Additional diagnostic techniques show promise, but they
have not been incorporated into practice yet. One large study
(n 300) reported that improved direct polymerase chain
reaction of stool specimens increased diagnosis by 50 percent
compared with culture.
61
Other authors successfully identi-
ed shigellae by microarrays using the gyrB genes.
62
This
novel approach also renders it possible to identify simulta-
neously other enteric pathogens, such as Salmonella spp. and
diarrheogenic Escherichia coli.
62
Immune assay with mono-
clonal antibodies to the IpaC protein detected both
Shigella spp. and enteroinvasive E. coli in 165 stool speci-
mens, with high sensitivity and specicity.
63
Treatment
Fluids and Nutrition
The mainstay of treatment of shigellosis in children is correc-
tion of the uid and electrolyte loss, which often can be
achieved by administering oral rehydration solutions.
2,64
Early feeding, even with a high-protein diet, is important,
especially in developing countries, to prevent malnutrition
and encourage optimal growth.
65
Antimicrobial Therapy
Appropriate antimicrobial therapy of shigellosis shortens the
duration of fever and diarrhea, and it apparently also reduces
the risk of developing complications.
10
Concomitantly, the
duration of excretion of the pathogen in stools is shortened
signicantly, thereby reducing the spread of infection.
10,66
However, the increasing antimicrobial resistance of shigellae
constitutes a major problem.
10
Although initially susceptible,
most Shigella isolates currently are resistant to ampicillin and
trimethoprim-sulfamethoxazole (TPM-SMX). These antimi-
crobial agents often are recommended for the treatment of
shigellosis,
5
but they currently are inappropriate for empiric
therapy unless local microbiologic data suggest susceptibil-
ity. Table 1
67-76
shows the percent of resistance by geographic
location. One should note that these values are based on all
Shigella isolates; S. sonnei, which is the most prevalent species
in developed countries and relatively more common in chil-
dren,
6
tends to be more resistant than is S. exneri.
5
For
example, in Israel, between 1998 and 2000, 97 percent of S.
sonnei were resistant to TMP-SMX, compared with 69 percent
of S. exneri (P 0.0001).
5
Quinolones
Although nalidixic acid proved to be efcacious against shig-
ellosis in one pediatric clinical study, other studies from
Bangladesh, Hong Kong, and Taiwan reported high resis-
tance to this agent (Table 1).
69,70,73
Rates of resistance in most
developed countries are below 2 percent (Table 1).
5,67,74
The
new uoroquinolones appear to have a high clinical and mi-
crobiological efcacy against shigellosis and frequently are
used in adults with suspected Shigella infections.
10,66,69
They
are not approved for children younger than 18 years of age
because of a risk of drug-induced damage to the immature
joints.
66
Some authors question this policy, owing to the
proven effectiveness of quinolones in children
77,78
and the
apparent safety of a short course.
10
Reduced susceptibility of
Shigella spp., especially S. dysenteriae serotype 1, to uoro-
quinolones has been reported and may be mediated by a
proton motive force (pmf)-dependent efux system.
79,80
Cephalosporins
First- and second-generation cephalosporins, such as cepha-
lexin, cefamandole, and cefaclor, are ineffective against shig-
Shigella infections in children 249
ellosis, often despite the susceptibility of the pathogen in
vitro.
10
Their main limitation is the delayed fecal eradication
of shigellae. Third-generation cephalosporins hold promise.
Among this group, ceftriaxone has been the one investigated
most extensively. Response was excellent, with two doses of
ceftriaxone being as effective as ve.
10,81
Cexime was effec-
tive in children infected mostly with S. sonnei, but it was less
effective in adults with severe shigellosis caused mostly by S.
dysenteriae and S. exneri.
10,82
Resistance to third-generation
cephalosporins, mediated by extended-spectrum beta-lacta-
mases, has been reported in several locations.
10,83
Azithromycin
Azithromycin, an azalide with a broad spectrum of antimi-
crobial activity, was found to be efcacious in adults with
shigellosis.
69
In a comparison of azithromycin and cexime
in a controlled study of 75 children with culture-proven shig-
ellosis in Paraguay,
84
researchers noted a similar clinical ef-
cacy for the two drugs but a better bacteriologic efcacy of
azithromycin (P 0.01), perhaps due to its better penetra-
tion into cells.
84
In summary, two parenteral doses of ceftriaxone is sug-
gested as the treatment of choice for severe shigellosis in
children, especially hospitalized patients. Oral treatment of
milder cases is more problematic and depends on local resis-
tance patterns. One should remember that many of the
agents discussed here are not approved yet by the Food and
Drug Administration for the treatment of shigellosis.
Prevention
Clean running water, appropriate sanitation, control of ies,
good personal hygiene, and breastfeeding are the main mea-
sures to reduce the spread of shigellosis.
2
Despite continuing
efforts for the last 50 years, researchers so far have failed to
produce a vaccine against Shigella spp. Several strategies to
develop a Shigella vaccine are being studied. The current
status of vaccine development is addressed elsewhere in this
volume with the other enteric vaccines (Nataro).
References
1. Ozuah PO: Shigella update. Pediatr Rev 19:100, 1998
2. Edwards BH: Salmonella and Shigella species. Clin Lab Med 19:469-
487, 1999
3. Finkelstein Y, Moran O, Avitzur Y, et al: Clinical dysentery in hospital-
ized children. Infection 30:132-135, 2002
4. Prado V, Lagos R, Nataro JP, et al: Population-based study of the inci-
dence of Shigella diarrhea and causative serotypes in Santiago, Chile.
Pediatr Infect Dis J 18:500-505, 1999
5. Ashkenazi S, Levy I, Kazaronovski V, et al: Growing antimicrobial
resistance of Shigella isolates. J Antimicrob Chemother 51:427-429,
2003
6. Ashkenazi S, May-Zahav M, Dinari G, et al: Recent trends in the epide-
miology of Shigella species in Israel. Clin Infect Dis 17:897-899, 1993
7. Centers for Disease Control and Prevention: Summaries of notiable
diseases, United States. MMWR 50:1-62, 2001
8. Yurdakok K, Sahin N, Ozmert E, et al: Shigella gastroenteritis: clinical
and epidemiological aspects, and antibiotic susceptibility. Acta Paediatr
Jpn 39:681-684, 1997
9. Kotloff KL, Winickoff JP, Ivanoff B, et al: Global burden of Shigella
infections: implications for vaccine development and implementation
of control strategies. Bull World Health Organ 77:651-666, 1999
10. Ashkenazi S: Shigella species, in Yu VL, Weber R, Raoult D (eds):
Antimicrobial therapy and vaccines, vol 1 (ed 2). NewYork, Apple Tree
Production, 2002, pp 615-621
11. Sansonetti PJP: Rupture, invasion and inammatory destruction of in-
testinal barrier by Shigella, making sense of prokaryote-eukaryote
cross-talks. Microbiol Rev 25:3-14, 2001
12. Raqib R, Wretlind B, Andersson J, et al: Cytokine secretion in acute
shigellosis is correlated to disease activity and directed more to stool
than to plasma. J Infect Dis 171:376-384, 1995
13. Zychlinsky A, Thirumalai K, Arondel J, et al: In vivo apoptosis in
Shigella exneri infections. Infect Immun 64:5357-5365, 1996
14. Way SS, Borczuk AC, Dominitz R, et al: An essential role for gamma
interferon in innate resistance to Shigella exneri infection. Infect Im-
mun 66:1342-138, 1998
15. Fernandez MI, Sansonetti PJ: Shigella interaction with intestinal epithe-
lial cells determines the innate immune response in shigellosis. Int
J Med Microbiol 293:55-5567, 2003
16. Buchrieser C, Glaser P, Rusniok C, et al: The virulence plasmid
pWR100 and the repertoire of proteins secreted by the type III secre-
tion apparatus of Shigella exneri. Mol Microbiol 38:760-771, 2000
17. Galan JE, Collmer A: Type III secretion machines: bacterial devices for
protein delivery into host cells. Science 284:1322-1328, 1999
18. Ingersoll M, Groisman EA, Zychlinsky A: Pathogenicity islands of Shi-
gella. Curr Top Microbiol Immunol 264:49-65, 2002
Table 1 Antimicrobial Resistance of Shigella Isolates in Various Geographic Locations According to Selected Publications from
1992 to 2003
Country
Years Isolates
Obtained
% Resistant to:
Nalidixic
Acid Ref AMP TMP-SMX
Israel 1998-2000 85 94 2 5
USA 1995-1998 63 59 0.3 67
USA 2001 80 47 2 68
Bangladesh - 73 80 51 69
Hong Kong 1994-1995 72 76 32 70
Greece 1996-1998 46 29 - 71
Brazil 1988-1993 90 84 8 72
Taiwan 1982-1987 52 10 25 73
Canada 1990 52 34 0 74
Saudi Arabia 1985-1990 54 72 - 75
Thailand 1990 90 81 - 76
* AMP, ampicillin; TMP-SM, trimethoprim-sulfamethoxazol
250 S. Ashkenazi
19. Sasakawa C, Kamata K, Sakai T, et al: Virulence-associated genetic
regions comprising 31 kilobases of the 230-kilobase plasmid in Shigella
exneri 2a. J Bacteriol 170:2480-2484, 1988
20. Maurelli AT, Baudry B, dHauteville H, et al: Cloning of plasmid DNA
sequences involved in invasion of HeLa cells by Shigella exneri. Infect
Immun 49:164-171, 1984
21. Blocker A, Gounon P, Larquet E, et al: The tripartite type III secretion of
Shigella exneri inserts IpaB and IpaC into host membranes. J Cell Biol
147:683-693, 1999
22. Page AL, Ohayon H, Sansonetti PJ, et al: The secreted IpaB and IpaC
invasions and their cytoplasmic chaperone IpgC invasins and their
cytoplasmic chaperone IpgC are required for intercellular dissemina-
tion of Shigella exneri. Cell Microbiol 1:183-193, 1999
23. Bernardini ML, Mounier J, dHauteville H, et al: Identication of icsA, a
plasmid locus of Shigella exneri that governs bacterial intra- and inter-
cellular spread through interaction with F-actin. Proc Natl Acad Sci
USA 86:3867-3871, 1989
24. Goldberg MB, Theriot JA: Shigella exneri surface protein IcsA is suf-
cient to direct actin-based motility. Proc Natl Acad Sci USA 92:6572-
6576, 1995
25. Nakata N, Sasakawa C, Okada N, et al: Identication and characteriza-
tion of virK, a virulence-associated large plasmid gene essential for
intercellular spreading of Shigella exneri. Mol Microbiol 6:2387-2395,
1992
26. Steinhauer J, Agha R, Pham T, et al: The unipolar Shigella surface
protein IcsA is targeted directly to the bacterial old pole: IcsP cleavage
of IcsA occurs over the entire bacterial surface. Mol Microbiol 32:367-
377, 1999
27. Adler B, Sasakawa C, Tobe T, et al: A dual transcriptional activation
system for the 230 kb plasmid genes coding for virulence-associated
antigens of Shigella exneri. Mol Microbiol 3:627-635, 1989
28. Maurelli AT, Sansonetti PJ: Identication of a chromosomal gene con-
trolling temperature regulated expression of Shigella virulence. Proc
Natl AACD Sci USA 85:2820-2824, 1988
29. Bitzan M, te Loo DM: Interaction of Shiga toxin with endothelial cells.
Methods Mol Med 73:243-262, 2003
30. Sandvig K: Shiga toxins. Toxicon 39:1629-1635, 2001
31. Ray PE, Liu XH: Pathogenesis of Shiga toxin-induced hemolytic uremic
syndrome. Pediatr Nephrol 16:823-839, 2001
32. Faruque AS, Teka T, Fuchs GJ: Shigellosis in children: a clinico-epide-
miological comparison between Shigella dysenteriae type I and Shigella
exneri. Ann Trop Paediatr 18:197-201, 1998
33. Vargas M, Gascon J, Jimenez-De-anta MT, et al: Prevalence of Shigella
enterotoxins 1 and 2 among Shigella strains isolated from patients with
travelers diarrhea. J Clin Microbiol 37:3608-3611, 1999
34. Raqib R, Lindberg AA, Wretlind B, et al: Persistence of local cytokine
production in shigellosis in acute and convalescent stages. Infect Im-
mun 63:289-296, 1995
35. Nonaka T, Kuwabara T, Mimuro H, et al: Shigella-induced necrosis and
apoptosis of U937 cells and J774 macrophages. Microbiology 149:
2513-2527, 2003
36. Adam T, Arpin M, Prevost MC, et al: Cytoskeletal rearrangements and
the functional role of T-plastin during entry of Shigella exneri into
HeLa cells. J Cell Biol 129:367-381, 1995
37. Hall A: Rho GT. Pases and the actin cytoskeleton. Science 279:509-
514, 1998
38. Goldberg MB, Barzu O, Parsot C, et al: Unipolar localization and AT-
Pase activity of IcsA, a Shigella exneri protein involved in intracellular
movement. Infect Agents Dis 2:210-211, 1993
39. Sansonetti PJ, Arondel J, Huerre M, et al: Interleukin-8 controls bacte-
rial transepithelial translocation at the cost of epithelial destruction in
experimental shigellosis. Infect Immun 67:1471-1480, 1999
40. Adam T: Exploitation of host factors for efcient infection by Shigella.
Int J Med Microbiol 291:287-298, 2001
41. Hilbi H, Moss JE, Hersh D, et al: Shigella-induced apoptosis is depen-
dent on casepase-1 which binds to IpaB. J Biol Chem 273:32895-
32900, 1998
42. Cario E, Brown D, McKee M, et al: Commensal-associated molecular
patterns induce selective toll-like receptor-trafcking from apical
membrane to cytoplasmic compartments in polarized intestinal
epithelium. Am J Pathol 160:1665-1673, 2002
43. Zhang Z, Jin L, Champion G, et al: Shigella infection in a SCID mouse-
human intestinal xenograft model: role for neutrophils in containing
bacterial dissemination in human intestine. Infect Immun 69:3240-
3247, 2001
44. Strulens MJ, Patte D, Kabir I, et al: Shigella septicemia: prevalence,
presentation, risk factors and outcome. J Infect Dis 152:784-790, 1985
45. Greenberg D, Marcu S, Melamed R, et al: Shigella bacteremia: a retro-
spective study. Clin Pediatr (Phila) 42:411-415, 2003
46. Baer JT, Vugia DJ, Reingold AL, et al: HIV infection as a risk factor for
shigellosis. Emerg Infect Dis 5:820-823, 1999
47. Huebner J, Czerwenka W, Gruner E, et al: Shigellemia in AIDS patients:
case report and review of the literature. Infection 21:122-124, 1993
48. Kirstjansson M, Viner B, Maslow JN: Polymicrobial and recurrent bac-
teremia with Shigella in a patient with AIDS. Scand J Infect Dis 26:411-
416, 1994
49. Miron D, Sochotnick I, Yardeni D, et al: Surgical complications of
shigellosis in children. Pediatr Infect Dis J 19:898-900, 2000
50. Khan WA, Dhar U, Salam MA, et al: Central nervous manifestations of
childhood shigellosis: prevalence, risk factors, and outcome. Pediatrics
103:E18, 1999
51. Perles Z, Bar-Ziv J, Granot E: Brain edema: an underdiagnosed compli-
cation of Shigella infection. Pediatr Infect Dis J 14:1114-1115, 1995
52. Plotz FB, Arets HG, Fleer A, et al: Lethal encephalopathy complicating
childhood shigellosis. Eur J Pediatr 158:550-552, 1999
53. Goren A, Freier S, Passwell J: Lethal toxic encephalopathy due to child-
hood shigellosis in a developed country. Pediatrics 89:1189-1193,
1992
54. Yuhas Y, Shulman L, Weizman A, et al: Involvement of tumor necrosis
factor alpha and interleukin-1beta in enhancement of pentylenetetra-
zole-induced seizures caused by Shigella dysenteriae. Infect Immun 67:
1455-1460, 1999
55. Balter-Seri J, Yuhas Y, Weizman A, et al: Role of nitric oxide in the
enhancement of pentylenetetrazole-induced seizures caused by Shigella
dysenteriae. Infect Immun 67:6364-6368, 1999
56. Yuhas Y, Weizman A, Ashkenazi S: Bidirectional concentration-depen-
dent effects of tumor necrosis factor alpha in Shigella dysenteriae-re-
lated seizures. Infect Immun 71:2288-2291, 2003
57. Anatoliotaki M, Galanakis E, Tsekoura T, et al: Urinary tract infection
caused by Shigella sonnei. Scand J Infect Dis 35:431-433, 2003
58. Baiulescu M, Hannon PR, Marcinak JF, Janda WM, Schreckenberger
PC: Chronic vulvovaginitis caused by antibiotic-resistant Shigella ex-
neri in a prepubertal child. Pediatr Infect Dis J 21:170-172, 2002
59. Viner Y, Miron D, Gottfried E, et al: Neonatal shigellosis. Isr Med Assoc
J 3:964-966, 2001
60. Gomez HF, Ochoa TJ, Carlin LG, et al: Human lactoferrin impairs
virulence of Shigella exneri. J Infect Dis 187:87-95, 2003
61. Dutta S, Chatterjee A, Dutta P, et al: Sensitivity and performance char-
acteristics of a direct PCR with stool samples in comparison to conven-
tional techniques for diagnosis of Shigella and enteroinvasive
Escherichia coli infection in children with acute diarrhoea in Calcutta,
India. J Med Microbiol 50:667-674, 2001
62. Kakinuma K, Fukushima M, Kawaguchi R: Detection and identication
of Escherichia coli, Shigella, and Salmonella by microarrays using the
gyrB gene Biotechnol Bioeng 83:721-726, 2003
63. Szakal DD, Schneider G, Pal T: A colony plot immune assay to identify
enteroinvasive Escherichia coli and Shigella in stool samples. Diagn Mi-
crobiol Infect Dis 45:165-171, 2003
64. Khan AM, Rabbani GH, Faruque AS, et al: WHO-ORS in treatment of
shigellosis. J Diarrhoeal Dis Res 17:88-89, 1999
65. Kabir I, Rahman MM, Haider R, et al: Increased height gain of children
fed a high-protein diet during convalescence from shigellosis: a six-
month follow-up study. J Nutr 128:1688-1691, 1998
66. Bhattacharya SK, Sur D: An evaluation of current shigellosis treatment.
Expert Opin Pharmacother 4:1315-1320, 2003
67. Replogle ML, Fleming DW, Cieslak PR: Emergence of antimicrobial-
resistant shigellosis in Oregon. Clin Infect Dis 30:515-519, 2000
68. CDC National Anticmicrobial Resistance Monitoring System. Available
Shigella infections in children 251
at: http://www.cdc.gov/narms/annual/2001/table/0125.htm; Internet;
accessed August 11, 2004
69. Khan WA, seas C, Dhar U et al. Azithromycin is equivalent to cipro-
oxacin in the treatment of shigellosis: results of a randomized, blinded
clinical trial. Abstract LM 29, 36
th
Interscience Conference of Antimi-
crobial Agents and Chemotherapy, NewOrleans, Louisiana, Sept. 1996
70. Chu YW, Houang ET, Lyon DJ, et al: Antimicrobial resistance in Shigella
exneri and Shigella sonnei in Hong Kong, 1986 to 1995. Antimicrob
Agents Chemother 42:440-443, 1998
71. Maraki S, Georgiladakis A, Christidou A, et al: Antimicrobial suscepti-
bilities and beta-lactamase production of Shigella isolates in Crete,
Greece, during the period 1991-1995. APMIS 106:879-883, 1998
72. Lima AA, Lima NL, Pinho MC, et al: High frequency of strains multiply
resistant to ampicillin, trimethoprim-sulfamethoxazole, streptomycin,
chloramphenicol, and tetracycline isolated from patients with shigello-
sis in northeastern Brazil during the period 1988 to 1993. Antimicrob
Agents Chemother 39:256-259, 1995
73. Lin SR, Chang SF: Drug resistance and plasmid prole of shigellae in
Taiwan. Epidemiol Infect 108:87-97, 1992
74. Harnett N: High level resistance to trimethoprim, cotrimoxazole and
other antimicrobial agents among clinical isolates of Shigella species in
Ontario, Canadaan update. Epidemiol Infect 109:463-472, 1992
75. Kagalwalla AF, Khan SN, Kagalwalla YA: Childhood shigellosis in Saudi
Arabia. Pediatr Infect Dis J 11:215-219, 1992
76. Thisyakorn U, Rienprayoon S: Shigellosis in Thai children: epidemio-
logic, clinical and laboratory features. Pediatr Infect Dis J 11:213-215,
1992
77. Salam MA, Dhar U, Khan WA, et al: Randomised comparison of cipro-
oxacin suspension and pivmecillinam for childhood shigellosis. Lan-
cet 352:522-527, 1998
78. The Dysentery Study Group. Multicenter, randomized, double blind
clinical trial of short course versus standard course oral ciprooxacin
for Shigella dysenteriae type 1 dysentery in children. Pediatr Infect Dis J
21:1136-1141, 2002
79. Sarkar K, Ghosh S, Niyogi SK, et al: Shigella dysenteriae type 1 with
reduced susceptibility to uoroquinolones. Lancet 361:785, 2003
80. Ghosh AS, Ahamed J, Chauhan KK, et al: Involvement of an efux
system in high-level uoroquinolone resistance of Shigella dysenteriae.
Biochem Biophys Res Commun 242:54-56, 1998
81. Eidlitz-Marcus T, Cohen YH, Nussinovitch M, et al: Comparative ef-
cacy of two- and ve-day courses of ceftriaxone for treatment of severe
shigellosis in children. J Pediatr 123:822-824, 1993
82. Ashkenazi S, Amir J, Waisman Y, et al: A randomized, double-blind
study comparing cexime and trimethoprim-sulfamethoxazole in the
treatment of childhood shigellosis. J Pediatr 123:817-821, 1993
83. Acikgoz ZC, Gulay Z, Bicmen M, et al: CTX-M-3 extended-spectrum
beta-lactamase in a Shigella sonnei clinical isolate. Scand J Infect Dis
35:503-505, 2003
84. Basualdo W, Arbo A: Randomized comparison of azithromycin versus
cexime for treatment of shigellosis in children. Pediatr Infect Dis J
22:374-377, 2003
252 S. Ashkenazi
You might also like
- Wolpert, Lewis - How We Live and Why We DieDocument4 pagesWolpert, Lewis - How We Live and Why We DieThamires Ribeiro de MattosNo ratings yet
- Essential Techniques of Alveolar Bone Augmentation in Implant Dentistry - 2022 - TolstunovDocument579 pagesEssential Techniques of Alveolar Bone Augmentation in Implant Dentistry - 2022 - TolstunovLuiz Guilherme FiorinNo ratings yet
- The Theory of Chronic Sorrow: Theorists: Georgene Gaskill Eakes, Mary Lermann Burke, & Margaret HainsworthDocument18 pagesThe Theory of Chronic Sorrow: Theorists: Georgene Gaskill Eakes, Mary Lermann Burke, & Margaret HainsworthKimberly Claire100% (1)
- Coidi 31 449Document6 pagesCoidi 31 449Kavyarani RathodNo ratings yet
- Arch Dis Child 1998 Ladhani 85 8Document5 pagesArch Dis Child 1998 Ladhani 85 8Dian Ayu Permata SandiNo ratings yet
- Gona Sarwat ShigellaDocument8 pagesGona Sarwat ShigellaDlzar AbubakrNo ratings yet
- Salmonella, The Host and Disease: A Brief ReviewDocument8 pagesSalmonella, The Host and Disease: A Brief ReviewPedro Albán MNo ratings yet
- PHD Thesis SalmonellaDocument4 pagesPHD Thesis Salmonellafqzaoxjef100% (2)
- Literature Review On SalmonellaDocument6 pagesLiterature Review On Salmonellac5r9j6zj100% (1)
- Malaria VaccineDocument3 pagesMalaria VaccinePrashant ChopdeyNo ratings yet
- Advances in LeishmaniasisDocument17 pagesAdvances in Leishmaniasisg_revelli2046No ratings yet
- E.coli Toxin ShigaDocument6 pagesE.coli Toxin ShigaVero VillarrealNo ratings yet
- 575 Full PDFDocument12 pages575 Full PDFandualemNo ratings yet
- Lister Ios IsDocument6 pagesLister Ios IsFede0No ratings yet
- Raffatellu Et Al. - 2007 - The Capsule Encoding The Viab Locus Reduces Interleukin-17 Expression and Mucosal Innate Responses in The BovDocument9 pagesRaffatellu Et Al. - 2007 - The Capsule Encoding The Viab Locus Reduces Interleukin-17 Expression and Mucosal Innate Responses in The Bovlpa.ufmt.enfNo ratings yet
- Amebiasis: Review ArticleDocument9 pagesAmebiasis: Review ArticleJouffrey Itaar MadridistaNo ratings yet
- Outer Membrane Protein C Is A Protective and UniquDocument12 pagesOuter Membrane Protein C Is A Protective and Uniquanushiyamani15No ratings yet
- NLF - Manuscript - Microbiology SpectrumDocument22 pagesNLF - Manuscript - Microbiology Spectrumrazib126No ratings yet
- Kimutai N Gideon Dennis Mutiso Moderator DR Songok 07 FEB 2011Document56 pagesKimutai N Gideon Dennis Mutiso Moderator DR Songok 07 FEB 2011drgiddie7640No ratings yet
- Paper Seminario 02Document18 pagesPaper Seminario 02Hans MenaresNo ratings yet
- J Immunol 2007 Rydström 5789 801Document14 pagesJ Immunol 2007 Rydström 5789 801susana1616No ratings yet
- Articulo 7 Mig OkDocument11 pagesArticulo 7 Mig Okoscarbio20090% (1)
- Within-Host Microevolution of Streptococcus Pneumoniae Is Rapid and Adaptive During Natural Colonisation - 2020 Nature ResearchDocument14 pagesWithin-Host Microevolution of Streptococcus Pneumoniae Is Rapid and Adaptive During Natural Colonisation - 2020 Nature ResearchTony NgNo ratings yet
- Shigella Review GuidelineDocument16 pagesShigella Review GuidelineAndi MuftyNo ratings yet
- Breaking Down BiofilmsDocument3 pagesBreaking Down Biofilmsleila.hiloutNo ratings yet
- Helicobacter Pylori PHD ThesisDocument12 pagesHelicobacter Pylori PHD Thesisgjfcp5jb100% (2)
- Neonatal Sepsis in The Very Low Birth Weight Preterm Infants: Part 1: Review of Patho-PhysiologyDocument10 pagesNeonatal Sepsis in The Very Low Birth Weight Preterm Infants: Part 1: Review of Patho-PhysiologyjukunkNo ratings yet
- The Molecular Genetics of Inflammatory, Autoimmune, and Infectious Diseases of The Sinonasal TractDocument9 pagesThe Molecular Genetics of Inflammatory, Autoimmune, and Infectious Diseases of The Sinonasal TractdaohailongNo ratings yet
- Rotavirus Case DiscussionDocument7 pagesRotavirus Case DiscussionNakajima AtsushiNo ratings yet
- Assessing Gut Microbiota Perturbations During The Early Phase of Infectious Diarrhea in Vietnamese ChildrenDocument18 pagesAssessing Gut Microbiota Perturbations During The Early Phase of Infectious Diarrhea in Vietnamese ChildrenKavyarani RathodNo ratings yet
- AmebiasisDocument10 pagesAmebiasisMuhammad RifkiNo ratings yet
- Meningitis NeonatoDocument24 pagesMeningitis NeonatoAldo Fernando Condori RiveraNo ratings yet
- Virulence Factors of Candida SpeciesDocument6 pagesVirulence Factors of Candida Specieslaura_ruiz_99No ratings yet
- 1 s2.0 S2949924023000046 MainDocument9 pages1 s2.0 S2949924023000046 Main7fkqx7zh7pNo ratings yet
- Infectious Diseases of The Female Genital TractDocument1,111 pagesInfectious Diseases of The Female Genital TractJohn Ntokos100% (2)
- Zii2043 PDFDocument10 pagesZii2043 PDFPablo VelazquezNo ratings yet
- Coxsackie VirusDocument10 pagesCoxsackie Virusjyothsna yarraNo ratings yet
- Streptococcus Group A InfectionsDocument13 pagesStreptococcus Group A InfectionsLidia GotoYourhappyplaceNo ratings yet
- The Role of The Gut Microbiota in SepsisDocument9 pagesThe Role of The Gut Microbiota in SepsisSyahrul HamidNo ratings yet
- Microbioma y OtorrinoDocument19 pagesMicrobioma y Otorrinodayenu barraNo ratings yet
- 12 IauujDocument9 pages12 IauujFaiz Yunanto MangoendiprodjoNo ratings yet
- Cimid 2015 AjayDocument7 pagesCimid 2015 AjayprashantcdriNo ratings yet
- J. Virol.-2003-Sullivan-9733-7Document6 pagesJ. Virol.-2003-Sullivan-9733-7Juan MoralesNo ratings yet
- 1471 2431 11 29 PDFDocument6 pages1471 2431 11 29 PDFCeleste SantiNo ratings yet
- Human Trophoblasts Confer Resistance To Viruses ImDocument8 pagesHuman Trophoblasts Confer Resistance To Viruses Imonline videoNo ratings yet
- Pathogens: Herpes Simplex Virus Establishment, Maintenance, and Reactivation: in Vitro Modeling of LatencyDocument14 pagesPathogens: Herpes Simplex Virus Establishment, Maintenance, and Reactivation: in Vitro Modeling of LatencyrehanaNo ratings yet
- T8 - Intestinal Phages Interact With Bacteria and Are Involved in Human DiseasesDocument23 pagesT8 - Intestinal Phages Interact With Bacteria and Are Involved in Human DiseasesdggdgfgdfNo ratings yet
- Candida Albicans: Pathogenicity and Epithelial ImmunityDocument4 pagesCandida Albicans: Pathogenicity and Epithelial ImmunityIstna Sofia AuliaNo ratings yet
- Researcharticle Open Access: Veterinary ResearchDocument13 pagesResearcharticle Open Access: Veterinary ResearchASOCIATIA EUROVETERINARIANNo ratings yet
- Assaignment01 MIC407Document8 pagesAssaignment01 MIC407c4jcydrgwqNo ratings yet
- The Role of Bacterial Biofilm in Persistent Infections and Control StrategiesDocument8 pagesThe Role of Bacterial Biofilm in Persistent Infections and Control StrategiesJenny TaylorNo ratings yet
- Malaria Pathogenesis: Louis H. Miller, Michael F. Good, Genevieve MilonDocument6 pagesMalaria Pathogenesis: Louis H. Miller, Michael F. Good, Genevieve MilonElroy Magnus QuinlanNo ratings yet
- Prenatal Investigation and Management of Non-Immune Hydrops FetalisDocument13 pagesPrenatal Investigation and Management of Non-Immune Hydrops FetalisHana AgustinNo ratings yet
- Empyema 2Document9 pagesEmpyema 2phobicmdNo ratings yet
- Alterations in Macrophage-Produced CytokinesDocument8 pagesAlterations in Macrophage-Produced CytokinessanielNo ratings yet
- nature+impDocument17 pagesnature+impAzraNo ratings yet
- Streptococcus Pneumoniae: Invasion and in Ammation: Allister J. Loughran, Carlos J. Orihuela, and Elaine I. TuomanenDocument18 pagesStreptococcus Pneumoniae: Invasion and in Ammation: Allister J. Loughran, Carlos J. Orihuela, and Elaine I. TuomanenSantiago Basto CruzNo ratings yet
- Papillomaviruses - Viral Evolution, Cancer and Evolutionary MedicineDocument20 pagesPapillomaviruses - Viral Evolution, Cancer and Evolutionary MedicineWilliam PeiNo ratings yet
- Bacteriophage Therapy: An Alternative To Conventional AntibioticsDocument4 pagesBacteriophage Therapy: An Alternative To Conventional AntibioticsAnandNo ratings yet
- Gamberini Et AlDocument9 pagesGamberini Et AlDeboraXiningNo ratings yet
- Uso de Vacunas de ADN vs. Salmonella EntericaDocument10 pagesUso de Vacunas de ADN vs. Salmonella EntericaalferezhassanNo ratings yet
- Thesis On Group B StreptococcusDocument4 pagesThesis On Group B Streptococcusbskb598g100% (2)
- Comprehensive Insights into Escherichia coli Infections: From Pathogenesis to Novel InterventionsFrom EverandComprehensive Insights into Escherichia coli Infections: From Pathogenesis to Novel InterventionsNo ratings yet
- Frequencies: FREQUENCIES VARIABLES Umur Pendidikan Masakerja Pelatihan Pengetahuan Praktik /ORDER ANALYSISDocument13 pagesFrequencies: FREQUENCIES VARIABLES Umur Pendidikan Masakerja Pelatihan Pengetahuan Praktik /ORDER ANALYSISmerrycardinaNo ratings yet
- Infliximab (Remicade) For Paediatric Ulcerative Colitis - Second Line September 2011Document7 pagesInfliximab (Remicade) For Paediatric Ulcerative Colitis - Second Line September 2011merrycardinaNo ratings yet
- 05 Traumatic EmergenciesDocument15 pages05 Traumatic EmergenciesmerrycardinaNo ratings yet
- Iskandar Japardi50.pdf: Mink Radiologic Imaging. Vol 1.: United StatesDocument1 pageIskandar Japardi50.pdf: Mink Radiologic Imaging. Vol 1.: United StatesmerrycardinaNo ratings yet
- Acid-Base Disorders: Acidosis and AlkalosisDocument21 pagesAcid-Base Disorders: Acidosis and AlkalosisKim BuguinaNo ratings yet
- Homology Modeling TutorialDocument11 pagesHomology Modeling TutorialNata ShaNo ratings yet
- Dst-2425-Sample Paper-Class-Viii-P2-Ntse-S&mDocument9 pagesDst-2425-Sample Paper-Class-Viii-P2-Ntse-S&mSeema KumariNo ratings yet
- The Horse and The Indian AryansDocument31 pagesThe Horse and The Indian AryansPremendra Priyadarshi100% (2)
- Chi Square Practice ProblemsDocument4 pagesChi Square Practice ProblemsRujula SharmaNo ratings yet
- Bio LiteDocument1 pageBio LitesepthyaniNo ratings yet
- Lab 5Document12 pagesLab 5api-272723910No ratings yet
- Abrasive Blasting AllDocument6 pagesAbrasive Blasting Alllara_rajkumar667No ratings yet
- Laboratory Methods - Chap 03. BAM - Aerobic Plate CountDocument9 pagesLaboratory Methods - Chap 03. BAM - Aerobic Plate CountPhuong LeNo ratings yet
- Chapter 2 Chemistry Comes AliveDocument11 pagesChapter 2 Chemistry Comes AliveKianna PaytonNo ratings yet
- Science Magazine 5693 2004-10-01Document107 pagesScience Magazine 5693 2004-10-01WillimSmith100% (1)
- Amberchele Non Duality Almighty Mackerel Sample PDFDocument33 pagesAmberchele Non Duality Almighty Mackerel Sample PDFJune BugNo ratings yet
- Mekanisme Toksisitas Ind 2018Document40 pagesMekanisme Toksisitas Ind 2018Gigih Lingga PNo ratings yet
- Emotional IntelligenceDocument11 pagesEmotional IntelligenceKEREN MILLETNo ratings yet
- Binomial Nomenclature: - Genus + Species - ExamplesDocument19 pagesBinomial Nomenclature: - Genus + Species - ExamplestiaraNo ratings yet
- Geography SyllabusDocument4 pagesGeography SyllabusmvrthedocNo ratings yet
- Principles of Behavior ChangeDocument10 pagesPrinciples of Behavior ChangeGuillermo ThomasNo ratings yet
- How To Draw Flowers - Reda WaazizDocument128 pagesHow To Draw Flowers - Reda WaazizLucas Di Stasio GrünNo ratings yet
- Mark Scheme (FINAL) January 2009: GCE Biology (6104/03)Document14 pagesMark Scheme (FINAL) January 2009: GCE Biology (6104/03)Mageswary SivalingamNo ratings yet
- ESO219 - Lecture 7 Transmission GeneticsDocument15 pagesESO219 - Lecture 7 Transmission GeneticsArvind RathoreNo ratings yet
- Descriptive Essay of The Botanical GardenDocument1 pageDescriptive Essay of The Botanical GardenTruicaIonutAndrei100% (1)
- By:Hend Eldeeb: Complete The Following SentencesDocument6 pagesBy:Hend Eldeeb: Complete The Following SentencesAhmed J AlhindaweNo ratings yet
- Chapter 2 Literature ReviewDocument30 pagesChapter 2 Literature ReviewSemana HumedalesNo ratings yet
- Cardiorespiratory Endurance: in This Chapter Student Web ResourcesDocument9 pagesCardiorespiratory Endurance: in This Chapter Student Web ResourcesChaye DomingoNo ratings yet
- Diablo Ka MarbelDocument30 pagesDiablo Ka MarbeljannaNo ratings yet
- Burung Air DeliDocument7 pagesBurung Air DeliAgus SatriyonoNo ratings yet
- Classifications of DrugsDocument10 pagesClassifications of DrugsHarshitaNo ratings yet