Wikipedia - Semen Analysis (CHECKED)
Wikipedia - Semen Analysis (CHECKED)
Uploaded by
vitruvianxyzCopyright:
Available Formats
Wikipedia - Semen Analysis (CHECKED)
Wikipedia - Semen Analysis (CHECKED)
Uploaded by
vitruvianxyzOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Wikipedia - Semen Analysis (CHECKED)
Wikipedia - Semen Analysis (CHECKED)
Uploaded by
vitruvianxyzCopyright:
Available Formats
Semen analysis - Wikipedia, the free encyclopedia
https://en.wikipedia.org/wiki/Semen_analysis
Semen analysis
From Wikipedia, the free encyclopedia
A semen analysis (plural: semen analyses) evaluates
certain characteristics of a male's semen and the
sperm contained therein. It is done to help evaluate
male fertility, whether for those seeking pregnancy or
verifying the success of vasectomy. Depending on the
measurement method, just a few characteristics may
be evaluated (such as with a home kit) or many
characteristics may be evaluated (generally by a
diagnostic laboratory). Collection techniques and
precise measurement method may influence results.
Contents
1 Reasons for testing
2 Relation to fertility
3 Collection methods
4 Parameters
4.1 Sperm count
4.2 Motility
4.3 Morphology
4.4 Volume
4.5 Fructose level
4.6 pH
4.7 Liquefaction
4.8 MOT
4.9 Total motile spermatozoa
4.10 Others
5 Abnormalities
6 Factors that influence results
7 Measurement methods
8 See also
9 References
10 External links
Semen analysis
Diagnostics
Human sperm stained for semen quality testing in
the clinical laboratory.
MedlinePlus 003627
HCPCS-L2 G0027 (http://www.icd9data.com
/HCPCS/2011/G/G0027.htm)
Reasons for testing
The most common reasons for laboratory semen analysis in humans are as part of a couple's infertility
investigation and after a vasectomy to verify that the procedure was successful. It is also commonly used
for testing human donors for sperm donation, and for animals semen analysis is commonly used in stud
farming and farm animal breeding.
1 of 8
7/11/15, 0:31
Semen analysis - Wikipedia, the free encyclopedia
https://en.wikipedia.org/wiki/Semen_analysis
Occasionally a man will have a semen analysis done as part of routine pre-pregnancy testing. At the
laboratory level this is rare, as most healthcare providers will not test the semen and sperm unless
specifically requested or there is a strong suspicion of a pathology in one of these areas discovered
during the medical history or during the physical examination. Such testing is very expensive and
time-consuming, and in the U.S. is unlikely to be covered by insurance. In other countries, such as
Germany, the testing is covered by all insurances.
Relation to fertility
The characteristics measured by semen analysis are only some of the factors in semen quality. One
source states that 30% of men with a normal semen analysis actually have abnormal sperm function.[1]
Conversely, men with poor semen analysis results may go on to father children.[2] In NICE guidelines,
mild male factor infertility is defined as when 2 or more semen analyses have 1 or more variables below
the 5th percentile, and confers a chance of pregnancy occurring naturally through vaginal intercourse
within 2 years similar to people with mild endometriosis.[3]
Collection methods
Different methods used for semen collection are masturbation, coitus interruptus, condom collection,
epididymal extraction, etc.
Parameters
Examples of parameters measured in a semen analysis are: sperm count, motility, morphology, volume,
fructose level and pH.
Sperm count
Sperm count, or sperm concentration to avoid confusion
with total sperm count, measures the concentration of sperm
in a man's ejaculate, distinguished from total sperm count,
which is the sperm count multiplied with volume.[4] Over 15
million sperm per milliliter is considered normal, according
to the WHO in 2010.[5] Older definitions state 20 million.
[1][2] A lower sperm count is considered oligozoospermia. A
vasectomy is considered successful if the sample is
azoospermic. Some define success with rare non-motile
sperm are observed (fewer than 100,000 per millilitre).[6]
Others advocate obtaining a second semen analysis to verify
the counts are not increasing (as can happen with
re-canalization) and others still may perform a repeat
vasectomy for this situation.
The average sperm count today is between 20 and 40
million per milliliter in the Western world, having decreased
by 1-2% per year from a substantially higher number
2 of 8
Approximate pregnancy rate varies with
amount of sperm used in an artificial
insemination cycle. Values are for
intrauterine insemination, with sperm
number in total sperm count, which may
be approximately twice the total motile
sperm count.
7/11/15, 0:31
Semen analysis - Wikipedia, the free encyclopedia
https://en.wikipedia.org/wiki/Semen_analysis
decades ago.[7]
Chips for home use are emerging that can give an accurate estimation of sperm count after three samples
taken on different days. Such a chip may measure the concentration of sperm in a semen sample against
a control liquid filled with polystyrene beads.[8]
Motility
The World Health Organization has a value of 50% and this must be measured within 60 minutes of
collection. WHO also has a parameter of vitality, with a lower reference limit of 60% live
spermatozoa.[5] A man can have a total number of sperm far over the limit of 20 million sperm cells per
milliliter, but still have bad quality because too few of them are motile. However, if the sperm count is
very high, then a low motility (for example, less than 60%) might not matter, because the fraction might
still be more than 8 million per millilitre. The other way around, a man can have a sperm count far less
than 20 million sperm cells per millilitre and still have good motility, if more than 60% of those
observed sperm cells show good forward movement.
A more specified measure is motility grade, where the motility of sperm are divided into four different
grades:[9]
Grade a: Sperm with progressive motility. These are the strongest and swim fast in a straight line.
Sometimes it is also denoted motility IV.
Grade b: (non-linear motility): These also move forward but tend to travel in a curved or crooked
motion. Sometimes also denoted motility III.
Grade c: These have non-progressive motility because they do not move forward despite the fact
that they move their tails. Sometimes also denoted motility II.
Grade d: These are immotile and fail to move at all. Sometimes also denoted motility I.
Morphology
Regarding sperm morphology, the WHO criteria as described in
2010 state that a sample is normal (samples from men whose
partners had a pregnancy in the last 12 months) if 4% (or 5th
centile) or more of the observed sperm have normal morphology.
[5][10]
Morphology is a predictor of success in fertilizing oocytes during
in vitro fertilization.
Up to 10% of all spermatozoa have observable defects and as
such are disadvantaged in terms of fertilising an oocyte.[11]
Also, sperm cells with tail-tip swelling patterns generally have
lower frequency of aneuploidy.[12]
A motile sperm organelle morphology examination (MSOME) is
a particular morphologic investigation wherein an inverted light
microscope equipped with high-power optics and enhanced by digital imaging is used to achieve a
3 of 8
7/11/15, 0:31
Semen analysis - Wikipedia, the free encyclopedia
https://en.wikipedia.org/wiki/Semen_analysis
magnification above x6000, which is much higher than the magnification used habitually by
embryologists in spermatozoa selection for intracytoplasmic sperm injection (x200 to x400).[13] A
potential finding on MSOME is the presence of sperm vacuoles, which are associated with sperm
chromatin immaturity, particularly in the case of large vacuoles.[14]
Volume
WebMD advises that semen volumes between 1.0 mL and 6.5 mL are normal;[2] WHO regards 1.5 ml as
the lower reference limit.[5] Low volume may indicate partial or complete blockage of the seminal
vesicles, or that the man was born without seminal vesicles.[1] In clinical practice, a volume of less than
2 mL in the setting of infertility and absent sperm should prompt an evaluation for obstructive
azoospermia. A caveat to this is be sure it has been at least 48 hours since the last ejaculation to time of
sample collection.
Fructose level
Regarding the level of fructose in the semen, WebMD lists normal as at least 3 mg/mL.[2] WHO
specifies a normal level of 13 mol per sample. Absence of fructose may indicate a problem with the
seminal vesicles.[1]
pH
WebMD lists a normal pH range of 7.1-8.0;[2] WHO criteria specify normal as 7.2-7.8.[1] Acidic
ejaculate (lower pH value) may indicate one or both of the seminal vesicles are blocked. A basic
ejaculate (higher pH value) may indicate an infection.[1] A pH value outside of the normal range is
harmful to sperm.[2]
Liquefaction
The liquefaction is the process when the gel formed by proteins from the seminal vesicles is broken up
and the semen becomes more liquid. It normally takes less than 20 minutes for the sample to change
from a thick gel into a liquid. In the NICE guidelines, a liquefaction time within 60 minutes is regarded
as within normal ranges.[15]
MOT
MOT is a measure of how many million sperm cells per ml are highly motile,[16] that is, approximately
of grade a (>25 micrometer per 5 sek. at room temperature) and grade b (>25 micrometer per 25 sek. at
room temperature). Thus, it is a combination of sperm count and motility.
With a straw [17] or a vial volume of 0.5 milliliter, the general guideline is that, for intracervical
insemination (ICI), straws or vials making a total of 20 million motile spermatozoa in total is
recommended. This is equal to 8 straws or vials 0.5 ml with MOT5, or 2 straws or vials of MOT20. For
intrauterine insemination (IUI), 1-2 MOT5 straws or vials is regarded sufficient.[18] In WHO terms, it is
thus recommended to use approximately 20 million grade a+b sperm in ICI, and 2 million grade a+b in
IUI.
4 of 8
7/11/15, 0:31
Semen analysis - Wikipedia, the free encyclopedia
https://en.wikipedia.org/wiki/Semen_analysis
Total motile spermatozoa
Total motile spermatozoa (TMS)[19] or total motile sperm count (TMSC)[20] is a combination of sperm
count, motility and volume, measuring how many million sperm cells in an entire ejaculate are motile.
Use of approximately 20 million sperm of motility grade c or d in ICI, and 5 million ones in IUI may be
an approximate recommendation.
Others
The NICE guidelines also include testing vitality, with normal ranges defined as more than 75% of
sperm cells alive.[15]
The sample may also be tested for white blood cells. A high level of white blood cells in semen is called
leucospermia and may indicate an infection.[1] Cutoffs may vary, but an example cutoff is over 1 million
white blood cells per milliliter of semen.[1]
Abnormalities
Aspermia: absence of semen
Azoospermia: absence of sperm
Hypospermia: low semen volume
Hyperspermia: high semen volume
Oligozoospermia: Very low sperm count
Asthenozoospermia: poor sperm motility
Teratozoospermia: sperm carry more morphological defects than usual
Necrozoospermia: all sperm in the ejaculate are dead
Leucospermia: a high level of white blood cells in semen
Factors that influence results
Apart from the semen quality itself, there are various methodological factors that may influence the
results, giving rise to inter-method variation.
Compared to samples obtained from masturbation, semen samples from collection condoms have higher
total sperm counts, sperm motility, and percentage of sperm with normal morphology. For this reason,
they are believed to give more accurate results when used for semen analysis.
If the results from a man's first sample are subfertile, they must be verified with at least two more
analyses. At least 2 to 4 weeks must be allowed between each analysis.[21] Results for a single man may
have a large amount of natural variation over time, meaning a single sample may not be representative of
a man's average semen characteristics.[22] In addition, sperm physiologist Joanna Ellington believes that
the stress of producing an ejaculate sample for examination, often in an unfamiliar setting and without
any lubrication (most lubricants are somewhat harmful to sperm), may explain why men's first samples
often show poor results while later samples show normal results.[23]
A man may prefer to produce his sample at home rather than at the clinic. The site of semen collection
5 of 8
7/11/15, 0:31
Semen analysis - Wikipedia, the free encyclopedia
https://en.wikipedia.org/wiki/Semen_analysis
does not affect the results of a semen analysis.[24]
Measurement methods
Volume can be determined by measuring the weight of the sample container, knowing the mass of the
empty container. Sperm count and morphology can be calculated by microscopy. Sperm count can also
be estimated by kits that measure the amount of a sperm-associated protein, and are suitable for home
use.[25]
Computer Assisted Semen Analysis (CASA) is a catch-all phrase for automatic or semi-automatic
semen analysis techniques. Most systems are based on image analysis, but alternative methods exist
such as tracking cell movement on a digitizing tablet.[26][27] Computer-assisted techniques are
most-often used for the assessment of sperm concentration and mobility characteristics, such as velocity
and linear velocity. Nowadays, there are CASA systems, based on image analysis and using new
techniques, with near perfect results, and doing full analysis in a few seconds. With some techniques,
sperm concentration and motility measurements are at least as reliable as current manual methods.[28]
Raman spectroscopy has made progress in its ability to perform characterization, identification and
localization of sperm nuclear DNA damage.[29]
See also
Semen quality
Artificial insemination for more details of how semen parameters affects pregnancy rate
References
1. "Understanding Semen Analysis" (http://www.uhmc.sunysb.edu/urology/male_infertility
/SEMEN_ANALYSIS.html). Stonybrook, State University of New York. 1999. Retrieved 2007-08-05.
2. Essig, Maria G.; Edited by Susan Van Houten and Tracy Landauer, Reviewed by Martin Gabica and Avery L.
Seifert (2007-02-20). "Semen Analysis" (http://www.webmd.com/infertility-and-reproduction/guide/semenanalysis). Healthwise. WebMD. Retrieved 2007-08-05.
3. Fertility: assessment and treatment for people with fertility problems (http://guidance.nice.org.uk/CG156).
NICE clinical guideline CG156 - Issued: February 2013
4. sharedjourney.com - Male Infertility Testing (http://www.sharedjourney.com/define/semen.html)
5. Cooper TG, Noonan E, von Eckardstein S, Auger J, Baker HW, Behre HM, Haugen TB, Kruger T, Wang C,
Mbizvo MT, Vogelsong KM (MayJun 2010). "World Health Organization reference values for human
semen characteristics." (http://www.who.int/reproductivehealth/topics/infertility/cooper_et_al_hru.pdf) (PDF).
Human reproduction update 16 (3): 23145. doi:10.1093/humupd/dmp048 (https://dx.doi.org
/10.1093%2Fhumupd%2Fdmp048). PMID 19934213 (https://www.ncbi.nlm.nih.gov/pubmed/19934213).
6. Rajmil O, Fernndez M, Rojas-Cruz C, Sevilla C, Musquera M, Ruiz-Castae E (2007). "Azoospermia
should not be given as the result of vasectomy". Arch. Esp. Urol. (in Spanish) 60 (1): 558. PMID 17408173
(https://www.ncbi.nlm.nih.gov/pubmed/17408173).
Dhar NB, Bhatt A, Jones JS (2006). "Determining the success of vasectomy". BJU Int. 97 (4): 7736.
doi:10.1111/j.1464-410X.2006.06107.x (https://dx.doi.org/10.1111%2Fj.1464-410X.2006.06107.x).
PMID 16536771 (https://www.ncbi.nlm.nih.gov/pubmed/16536771).
7. The sperm count has been decreasing steadily for many years in Western industrialized countries: Is there an
endocrine basis for this decrease? (http://www.ispub.com/ostia/index.php?xmlFilePath=journals/iju/vol2n1
/sperm.xml) The Internet Journal of Urology TM. ISSN: 1528-8390
6 of 8
7/11/15, 0:31
Semen analysis - Wikipedia, the free encyclopedia
https://en.wikipedia.org/wiki/Semen_analysis
8. New Chip Provides Cheap At-Home Sperm Counting (http://www.popsci.com/technology/article/2010-01
/counting-chip-provides-cheap-home-sperm-counting) By Stuart Fox Posted 01.26.2010 in Popular Science
9. Shared Journey: Semen Analysis (http://www.sharedjourney.com/define/semen2.html)
10. Rothmann SA, Bort AM, Quigley J, Pillow R (2013). "Sperm morphology classification: a rational method
for schemes adopted by the world health organization.". Methods in molecular biology (Clifton, N.J.) 927:
2737. doi:10.1007/978-1-62703-038-0_4 (https://dx.doi.org/10.1007%2F978-1-62703-038-0_4).
PMID 22992901 (https://www.ncbi.nlm.nih.gov/pubmed/22992901).
11. Sadler, T. (2010). Langman's medical embryology. (11th ed. ed.). Philadelphia: Lippincott William &
Wilkins. p. 30. ISBN 978-0-7817-9069-7.
12. Pang MG, You YA, Park YJ, Oh SA, Kim DS, Kim YJ (June 2009). "Numerical chromosome abnormalities
are associated with sperm tail swelling patterns". Fertil. Steril. 94 (3): 10121020.
doi:10.1016/j.fertnstert.2009.04.043 (https://dx.doi.org/10.1016%2Fj.fertnstert.2009.04.043).
PMID 19505688 (https://www.ncbi.nlm.nih.gov/pubmed/19505688).
13. Oliveira JB, Massaro FC, Mauri AL, Petersen CG, Nicoletti AP, Baruffi RL, Franco JG (2009). "Motile
sperm organelle morphology examination is stricter than Tygerberg criteria". Reproductive biomedicine
online 18 (3): 320326. doi:10.1016/S1472-6483(10)60088-0 (https://dx.doi.org
/10.1016%2FS1472-6483%2810%2960088-0). PMID 19298729 (https://www.ncbi.nlm.nih.gov/pubmed
/19298729). [1] (http://www.crh.com.br/45.pdf)
14. Perdrix A, Rives N (2013). "Motile sperm organelle morphology examination (MSOME) and sperm head
vacuoles: State of the art in 2013". Human Reproduction Update 19 (5): 527541. doi:10.1093/humupd
/dmt021 (https://dx.doi.org/10.1093%2Fhumupd%2Fdmt021). PMID 23825157
(https://www.ncbi.nlm.nih.gov/pubmed/23825157).
15. [2] (http://www.nice.org.uk/nicemedia/pdf/CG011publicinfoenglish.pdf) Fertility: Assessment and Treatment
for People with Fertility Problems. London: RCOG Press. 2004. ISBN 1-900364-97-2.
16. Cryos International - What does MOT mean? (http://dk.cryosinternational.com/private-customers/questionsanswers.aspx#7175)
17. Cryos International - What is a straw? (http://dk.cryosinternational.com/private-customers/questionsanswers.aspx#7179)
18. Cryos International - How much sperm should I order? (http://dk.cryosinternational.com/private-customers
/questions-answers.aspx#7169)
19. Merviel P, Heraud MH, Grenier N, Lourdel E, Sanguinet P, Copin H (November 2008). "Predictive factors
for pregnancy after intrauterine insemination (IUI): An analysis of 1038 cycles and a review of the
literature". Fertil. Steril. 93 (1): 7988. doi:10.1016/j.fertnstert.2008.09.058 (https://dx.doi.org
/10.1016%2Fj.fertnstert.2008.09.058). PMID 18996517 (https://www.ncbi.nlm.nih.gov/pubmed/18996517).
20. Pasqualotto EB, Daitch JA, Hendin BN, Falcone T, Thomas AJ, Nelson DR, Agarwal A (October 1999).
"Relationship of total motile sperm count and percentage motile sperm to successful pregnancy rates
following intrauterine insemination" (http://www.kluweronline.com/art.pdf?issn=1058-0468&volume=16&
page=476) (PDF). J. Assist. Reprod. Genet. 16 (9): 47682. doi:10.1023/A:1020598916080 (https://dx.doi.org
/10.1023%2FA%3A1020598916080). PMC 3455631 (https://www.ncbi.nlm.nih.gov/pmc/articles
/PMC3455631). PMID 10530401 (https://www.ncbi.nlm.nih.gov/pubmed/10530401).
21. Weschler, Toni (2002). Taking Charge of Your Fertility (Revised ed.). New York: HarperCollins. p. 189.
ISBN 0-06-093764-5.
22. "Adequate Analysis Frequency" (http://www.fertilityformen.com/info_why.php#frequency). Kokopelli
Technologies. 2007. Retrieved 2007-08-11.
23. Ellington, Joanna. Slippery When Wet: One Womans Journey Through The Mystery of Sex
(http://www.amazon.com/Slippery-When-Wet-Journey-Through/dp/099072820X/ref=sr_1_2?ie=UTF8&
qid=1418420270&sr=8-2&keywords=slippery+when+wet). Dr. E Publishing, LLC: 2014. Print.
24. Licht RS, Handel L, Sigman M (2007). "Site of semen collection and its effect on semen analysis
parameters". Fertil Steril. 89 (2): 3957. doi:10.1016/j.fertnstert.2007.02.033 (https://dx.doi.org
/10.1016%2Fj.fertnstert.2007.02.033). PMID 17482174 (https://www.ncbi.nlm.nih.gov/pubmed/17482174).
25. dailyprogress.com > Charlottesville company sends out its home male sterility tests
(http://www.dailyprogress.com/cdp/news/local/article
/charlottesville_company_sends_out_its_home_male_sterility_tests/40086/) By Brian McNeill. Published:
May 14, 2009
26. Mortimer ST (1 July 2000). "CASA--practical aspects" (http://www.andrologyjournal.org/cgi/reprint
/21/4/515). J. Androl. 21 (4): 51524. PMID 10901437 (https://www.ncbi.nlm.nih.gov/pubmed/10901437).
Retrieved 2007-08-05.
7 of 8
7/11/15, 0:31
Semen analysis - Wikipedia, the free encyclopedia
https://en.wikipedia.org/wiki/Semen_analysis
27. Hinting A, Schoonjans F, Comhaire F (1988). "Validation of a single-step procedure for the objective
assessment of sperm motility characteristics". Int. J. Androl. 11 (4): 27787.
doi:10.1111/j.1365-2605.1988.tb01001.x (https://dx.doi.org/10.1111%2Fj.1365-2605.1988.tb01001.x).
PMID 3170018 (https://www.ncbi.nlm.nih.gov/pubmed/3170018).
28. Testing of Accubead in: Tomlinson MJ, Pooley K, Simpson T, Newton T, Hopkisson J, Jayaprakasan K,
Jayaprakasan R, Naeem A, Pridmore T (April 2010). "Validation of a novel computer-assisted sperm analysis
(CASA) system using multitarget-tracking algorithms". Fertil. Steril. 93 (6): 191120.
doi:10.1016/j.fertnstert.2008.12.064 (https://dx.doi.org/10.1016%2Fj.fertnstert.2008.12.064).
PMID 19200972 (https://www.ncbi.nlm.nih.gov/pubmed/19200972).
29. Mallidis C, Sanchez V, Wistuba J, Wuebbeling F, Burger M, Fallnich C, Schlatt S (2014). "Raman
microspectroscopy: shining a new light on reproductive medicine". Hum. Reprod. Update 20 (3): 40314.
doi:10.1093/humupd/dmt055 (https://dx.doi.org/10.1093%2Fhumupd%2Fdmt055). PMID 24144514
(https://www.ncbi.nlm.nih.gov/pubmed/24144514).
External links
Geneva Foundation for Medical Education and Research (http://www.gfmer.ch/Endo/Lectures_09
/semen_analysis.htm) - complete list of parameters.
Semen analysis (http://labtestsonline.org/understanding/analytes/semen/tab/test) - Lab Tests
Online
Retrieved from "https://en.wikipedia.org/w/index.php?title=Semen_analysis&oldid=667802846"
Categories: Fertility medicine Semen
This page was last modified on 20 June 2015, at 19:11.
Text is available under the Creative Commons Attribution-ShareAlike License; additional terms
may apply. By using this site, you agree to the Terms of Use and Privacy Policy. Wikipedia is a
registered trademark of the Wikimedia Foundation, Inc., a non-profit organization.
8 of 8
7/11/15, 0:31
You might also like
- CBC ReportDocument1 pageCBC Reportdivyanshuglmp937No ratings yet
- Wikipedia - Hyperalgesia (CHECKED)Document5 pagesWikipedia - Hyperalgesia (CHECKED)vitruvianxyzNo ratings yet
- Semen AnalysisDocument6 pagesSemen AnalysisMuhal SahibNo ratings yet
- Sperm CountDocument2 pagesSperm CountRamanasarmaNo ratings yet
- Macleod 1Document8 pagesMacleod 1rakibhossainNo ratings yet
- 38 - Semen - Analysis TerjemahanDocument27 pages38 - Semen - Analysis TerjemahanShofia CahyaNo ratings yet
- Interpretation of The Semen Analysis and Initial Male Factor ManagementDocument10 pagesInterpretation of The Semen Analysis and Initial Male Factor ManagementRosangela Mazariegos CastilloNo ratings yet
- Semen AnalysisDocument34 pagesSemen AnalysisYurizaNo ratings yet
- Sperm Test and Semen Analysis Semen AnalysisDocument2 pagesSperm Test and Semen Analysis Semen Analysismahendra_choudhary07No ratings yet
- Sperm AnalysisDocument2 pagesSperm AnalysisChristoffer SamaristaNo ratings yet
- Chapter 11: Semen: Specimen CollectionDocument27 pagesChapter 11: Semen: Specimen Collectionangela tanteoNo ratings yet
- 12 SeminalysisDocument38 pages12 SeminalysissalumngusaNo ratings yet
- Lab 10 Semen AnalysisDocument45 pagesLab 10 Semen AnalysisFeroz KhanNo ratings yet
- Sesión 16. The Value of Canine Semen Evaluation For PractitionersDocument9 pagesSesión 16. The Value of Canine Semen Evaluation For PractitionersPavel Hunter RamírezNo ratings yet
- Semen - PPT No. 2Document18 pagesSemen - PPT No. 2Banan SulaimanNo ratings yet
- RPS3-K11 Analisis Sperma - 230921 - 142054Document21 pagesRPS3-K11 Analisis Sperma - 230921 - 14205432 sebastian Josia N.No ratings yet
- Jurnal Analisis Sperma - Analisis-spermatozoa-AsiaDocument8 pagesJurnal Analisis Sperma - Analisis-spermatozoa-AsiaMuzas88No ratings yet
- Gen Bio Sperm AnalysisDocument6 pagesGen Bio Sperm AnalysisJoshua Akim SinghNo ratings yet
- Seminal Fluid...Document10 pagesSeminal Fluid...Reign Aiken M. LaraNo ratings yet
- Chapter 5 Semen AnalysisDocument50 pagesChapter 5 Semen Analysisreshad nuredinNo ratings yet
- Final Seminal Fluid AnalysisDocument53 pagesFinal Seminal Fluid AnalysisMajdiBilbisi100% (1)
- Semen AnalysisDocument69 pagesSemen Analysismicheal1960No ratings yet
- Semen AnalysisDocument3 pagesSemen AnalysisAnonymous tojT5nNo ratings yet
- Semen AnalysisDocument9 pagesSemen AnalysisGlydenne Glaire Poncardas GayamNo ratings yet
- Impact of The New WHO Guidelines On Diagnosis and Practice of Male InfertilityDocument9 pagesImpact of The New WHO Guidelines On Diagnosis and Practice of Male InfertilitymostecocNo ratings yet
- semen Analysis ppt EDITEDDocument57 pagessemen Analysis ppt EDITEDNithin Krishnan CNo ratings yet
- SpermDocument1 pageSpermEve Karen PobleteNo ratings yet
- Semen AnalysisDocument22 pagesSemen Analysisjoshuamayokun19No ratings yet
- Approach To InfertilityDocument120 pagesApproach To InfertilityMohammed Ahmed BamashmosNo ratings yet
- AUBF Semen AnalysisDocument46 pagesAUBF Semen AnalysistachefjshowziNo ratings yet
- Spurm CountDocument4 pagesSpurm CountAsif AliNo ratings yet
- 2 PDFDocument6 pages2 PDFCésar EscalanteNo ratings yet
- Ajac 2016072717374752Document14 pagesAjac 2016072717374752Nina NinaNo ratings yet
- Sperma Analisis PaperDocument6 pagesSperma Analisis PaperFedrik Monte Kristo LimbongNo ratings yet
- Semen AnalysisDocument32 pagesSemen Analysisnivetha26082000No ratings yet
- The Effect of Intrauterine Insemination Time On Semen ParametersDocument4 pagesThe Effect of Intrauterine Insemination Time On Semen ParametersRamadhan AkmalNo ratings yet
- Semen Analysis PDFDocument34 pagesSemen Analysis PDFfikyad93No ratings yet
- Viscosity - Aubf (Hazel)Document17 pagesViscosity - Aubf (Hazel)Janielle Medina FajardoNo ratings yet
- Bio Zoology AssignmentDocument13 pagesBio Zoology Assignmentkishorecht149No ratings yet
- 10-Seminal Fluid AnalysisDocument69 pages10-Seminal Fluid AnalysisAhmed AliNo ratings yet
- Surgical Management of Male Infertility: An Update: Monica Velasquez, Cigdem TanrikutDocument13 pagesSurgical Management of Male Infertility: An Update: Monica Velasquez, Cigdem TanrikutIrvan PutraNo ratings yet
- EAU GUIDELINES ON MALE Infertility PDFDocument16 pagesEAU GUIDELINES ON MALE Infertility PDFsachinNo ratings yet
- Jurnal BiosensorDocument7 pagesJurnal BiosensorMushofatul FitriaNo ratings yet
- Semen FFFDocument12 pagesSemen FFFHabtamu MollaNo ratings yet
- Infertility: Dr. Amit Kumar Assistant Professor (Department of OBG) Madhav Homeopathic Medical College, Abu Road, SirohiDocument49 pagesInfertility: Dr. Amit Kumar Assistant Professor (Department of OBG) Madhav Homeopathic Medical College, Abu Road, Sirohirakhivermakalwar18No ratings yet
- Semen Analysis (Himalaya)Document14 pagesSemen Analysis (Himalaya)ubafran92No ratings yet
- Mila Chich 2020Document20 pagesMila Chich 2020MD LarasatiNo ratings yet
- Semen AnalysisDocument50 pagesSemen Analysismedooslah2No ratings yet
- usg evaluation female infertilityDocument14 pagesusg evaluation female infertilitytarasantraNo ratings yet
- Semen AnalysisDocument43 pagesSemen AnalysisKunal Katyayan100% (1)
- analysis of seminal plasmaDocument20 pagesanalysis of seminal plasma23051322No ratings yet
- Sperm Chromatin Structure Assay Results in Nigerian Men With Unexplained InfertilityDocument5 pagesSperm Chromatin Structure Assay Results in Nigerian Men With Unexplained InfertilityTantonio Tri PutraNo ratings yet
- ACROSIN TEST SPERM ( HABILITY TO FECUNDATION) AND RELATION TO OXIDATIVE STRESSDocument7 pagesACROSIN TEST SPERM ( HABILITY TO FECUNDATION) AND RELATION TO OXIDATIVE STRESSDurgaNo ratings yet
- ARTDocument36 pagesARTTtyyfff Fyyu89-No ratings yet
- Case 7 - Prostate Cancer PatientDocument21 pagesCase 7 - Prostate Cancer Patientmarcojempleo019No ratings yet
- Sperm Evaluation Services/sperm-Evaluation/sperm-And-Semen-Testing - PHPDocument12 pagesSperm Evaluation Services/sperm-Evaluation/sperm-And-Semen-Testing - PHPFahmiBudimanNo ratings yet
- Optimizing The First-Line Fertility Treatment: Gynecological EndocrinologyDocument6 pagesOptimizing The First-Line Fertility Treatment: Gynecological EndocrinologyKarlin ReyesNo ratings yet
- Elite 610Document8 pagesElite 610Umber Ranjana PandeyNo ratings yet
- Semen AnalysidsDocument44 pagesSemen Analysidsanamikavcsg1995No ratings yet
- New Concepts in Daignosis and Therapy of Repeat BreedingDocument7 pagesNew Concepts in Daignosis and Therapy of Repeat BreedinggnpobsNo ratings yet
- Wikipedia - Vasovagal Response (CHECKED)Document7 pagesWikipedia - Vasovagal Response (CHECKED)vitruvianxyzNo ratings yet
- Wikipedia - Post-Thrombotic Syndrome (CHECKED)Document5 pagesWikipedia - Post-Thrombotic Syndrome (CHECKED)vitruvianxyzNo ratings yet
- Wikipedia - Anion Gap (CHECKED)Document6 pagesWikipedia - Anion Gap (CHECKED)vitruvianxyzNo ratings yet
- Blood Tests: Normal Values - Normal Laboratory Values - Merck Manual Professional VersionDocument11 pagesBlood Tests: Normal Values - Normal Laboratory Values - Merck Manual Professional Versionvitruvianxyz0% (1)
- Wikipedia - Vulvar Cancer (For CHECK)Document7 pagesWikipedia - Vulvar Cancer (For CHECK)vitruvianxyzNo ratings yet
- Wikipedia - Coombs Test (For CHECK)Document6 pagesWikipedia - Coombs Test (For CHECK)vitruvianxyzNo ratings yet
- Platelets - The Lancet 2000Document9 pagesPlatelets - The Lancet 2000bluemleinNo ratings yet
- 01 - Blood-Function and CompositionDocument45 pages01 - Blood-Function and Compositionsylvester GelacNo ratings yet
- HbA1c Units Converter Chart PercentagesDocument7 pagesHbA1c Units Converter Chart Percentagesrodipo80No ratings yet
- Complete Blood Count (CBC) : Biological Reference Interval Result Parameter UnitDocument4 pagesComplete Blood Count (CBC) : Biological Reference Interval Result Parameter UnitSachin KumarNo ratings yet
- Q-23-185 Hematology Analyzer BC-5000-1Document3 pagesQ-23-185 Hematology Analyzer BC-5000-1AlaaAlMesmarNo ratings yet
- Polisi Operasi Transfusi 2023Document24 pagesPolisi Operasi Transfusi 2023labhtampinNo ratings yet
- Rotem Pocket Guide 2 Page Final cs5Document2 pagesRotem Pocket Guide 2 Page Final cs5Ronei Renato RubboNo ratings yet
- Blood Transfusion Guide 19ed 2017Document545 pagesBlood Transfusion Guide 19ed 2017Celeste Rosas100% (1)
- Complete Blood Count: at A GlanceDocument6 pagesComplete Blood Count: at A Glancecsy123No ratings yet
- Hemolytic Anemia: IAP UG Teaching Slides 2015-16Document38 pagesHemolytic Anemia: IAP UG Teaching Slides 2015-16Kathir100% (1)
- NCMMCA2Document12 pagesNCMMCA2Romm JacobNo ratings yet
- CBC (Complete Blood Count)Document1 pageCBC (Complete Blood Count)Roshan kumar giriNo ratings yet
- RH Isoimmunization 2021Document24 pagesRH Isoimmunization 2021Muhammad Omar Wasim AbdullahNo ratings yet
- Formulir Surat Pengantar Pemeriksaan Kesehatan (SPPK) (2021.01.06)Document1 pageFormulir Surat Pengantar Pemeriksaan Kesehatan (SPPK) (2021.01.06)Candra TrickswerNo ratings yet
- Rhodes Index of Nausea VomitingDocument1 pageRhodes Index of Nausea VomitingHasdiman Samania0% (1)
- Merged Immunohematology Lec Prelims Finals 1Document181 pagesMerged Immunohematology Lec Prelims Finals 1Cruz JenniferNo ratings yet
- Packed Cell Volume (Hematocrit) : PlasmDocument3 pagesPacked Cell Volume (Hematocrit) : PlasmS ANo ratings yet
- Congenital Coagulation Disorders: Danielle Sterrenberg and Sucha NandDocument22 pagesCongenital Coagulation Disorders: Danielle Sterrenberg and Sucha NandacNo ratings yet
- Blood Lymphatic and Immune System TerminologyDocument3 pagesBlood Lymphatic and Immune System TerminologySoniyaJI84No ratings yet
- Dr. Uleng Bahrun SP - PK (K), PHD - LED Sebagai Penanda Inflamasi 04062022Document32 pagesDr. Uleng Bahrun SP - PK (K), PHD - LED Sebagai Penanda Inflamasi 04062022Herbanu PramonoNo ratings yet
- Blood Transfusion in Hemorrhagic ShockDocument28 pagesBlood Transfusion in Hemorrhagic Shocklas100% (2)
- Sysmex SEED Platelet Detection and The Importance of A Reliable CountDocument7 pagesSysmex SEED Platelet Detection and The Importance of A Reliable CountMuhammad Khoirut TNo ratings yet
- Case Study - Hemophilia FinalDocument9 pagesCase Study - Hemophilia FinalCielo Louise Rivera Dominguez100% (1)
- f72f6676-ff46-41f0-848d-3643ca86f1b5Document2 pagesf72f6676-ff46-41f0-848d-3643ca86f1b5ParasNo ratings yet
- Table of Blood Group Antigens Within Systems v12.5 26-FEB-2024Document5 pagesTable of Blood Group Antigens Within Systems v12.5 26-FEB-2024Myat Noe Suu KyiNo ratings yet
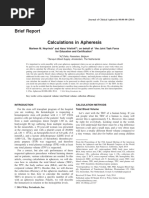
- Calculation in ApheresisDocument5 pagesCalculation in Apheresismilica cucuzNo ratings yet
- Blood Bank 1Document13 pagesBlood Bank 1Khaldoun AlmomaniNo ratings yet
- PlateletDocument15 pagesPlateletFafha Fafha100% (1)
- Hematology Week 8Document3 pagesHematology Week 8Rose Neil LapuzNo ratings yet