Medical Record Audit Tool PDF
Medical Record Audit Tool PDF
Uploaded by
nurhaidahCopyright:
Available Formats
Medical Record Audit Tool PDF
Medical Record Audit Tool PDF
Uploaded by
nurhaidahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Medical Record Audit Tool PDF
Medical Record Audit Tool PDF
Uploaded by
nurhaidahCopyright:
Available Formats
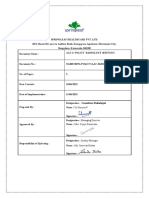
MEDICAL RECORD AUDIT TOOL
OPEN Nursing Review for Inpatient Adult and Pediatric Units
Page 1 of 4
REVIEW WITH MANAGER by the 5th of the month and FAX completed form to by the 10th of the month:
April Bowles at 982-6838 or MAIL to Box 800476.
Please audit the complete paper medical record
9CHECK THE APPROPRIATE BOX, EITHER: 9Y = Yes 9N = No 9NA = Not Applicable
Unit:
Manager Name:
CHART 1
CHART 2
Date Manager Reviewed:
CHART 3
CHART 4
Medical Record Number:
Admit Date:
Audit Date:
Reviewer(s):
Print Name
1. BLUE CHART
CHART:
Y N NA Y N NA Y N NA Y N NA
1.01 Patients name, sex, address, date of birth, admission diagnosis and
authorized representative or emergency contact are available in the record
(face sheet, EMR, database)?
1.02 If the patient is on Isolation, is there an information sheet from Infection Control in a page
protector? (NA if not on Isolation)
If the patient had a procedure(s) are the following in the chart? Check NA if no procedures
identified.
(Preprocedure checklist, Bedside form #050475, OR/Procedure #33033)
1.03 Was the Preprocedure verification section completed?
1.04 Was the Side/Body Site Verification section completed? (N/A if site verification not needed)
1.05 Is there an informed consent form? (NA if consent form not needed)
2. INFORMED CONSENT (LIP)
CHART:
Y N NA Y N NA Y N NA Y N NA
If Informed Consent was needed, consent form includes each of the following: (NA if no consent needed)
2.01 The nature of the proposed care, treatment, services, medications, interventions or procedures.
2.02 The potential benefits, risks, or side effects, including potential problems that might occur
during recuperation.
2.03 Reasonable alternatives as well as the relevant risks, benefits and side effects related to
alternatives, including the possible results of not receiving care, treatment and services.
2.04 Anesthesia type is accurately documented.
2.05 Was Informed Consent signed by patient or appropriate legal surrogate?
2.06 If applicable, blood consent obtained and includes the potential benefits, risks, side effects and
potential problems that might occur and is signed by patient or surrogate? (NA if no blood consent)
3. ADMITTING HISTORY AND PHYSICAL (LIP)
CHART:
Y N
3.01 Was an H&P completed within 30 days before or 24 hours after admission and placed in the
patients medical record within 24 hours after admission or registration but before surgery?
3.02 If H&P is less than 30 days, was updated examination completed and documented in the patients
medical record within 24 hours of admission or registration but before surgery?
Does the H&P include each of the following:
3.03 Chief complaint
3.04 Relevant past medical history
3.05 Details of present illness/injury
3.06 Social history
3.07 Allergies
3.08 Complete medication list including name, dose, route and frequency
3.09 Family history
3.10 Physical examination pertinent to diagnosis (including normal and abnormal findings
pertinent to care)
3.11 Planned course of action
2
Y N
3
Y N
4
Y N
To see related Joint Commission Standards see the Joint Commission Hospital Manual located as a computer desktop icon.
FORM 090801
NOT A CHART DOCUMENT
(REV 8/24/10)
To reorder, log onto http://www.virginia.edu/uvaprint/HSC/hs_forms.pl
MEDICAL RECORD AUDIT TOOL
4. INITIAL SCREENING (DATABASE)
CHART:
4.01 If Database blank, was at least 1 attempt made to obtain information if patient/family
unable to provide on admission? (NA if database is completed)
Note the Unit patient admitted to (information for Unit Manager)
4.02 Was initial screening by the RN initiated within 8 hours of admission to hospital and
completed within 24 hours? NOTE: IF Critical Care or L&D screening must be Initiated
AND completed within 8 hours.
4.03 If applicable, was person identified by patient notified of hospital admit? (NA if pt answers no)
Page 2 of 4
1
Y N NA Y N NA Y N NA Y N NA
4.04 For patient 18 years or older and patient able to answerIs there an answer marked to the
question, Do you have an Advance Directive? (NA if less than 18 years old)
4.05 If the patient has a resuscitative (code) status order in MIS is there a copy in the Red Page
Protector? (NA if patient is full code)
Were the following Initial screenings completed?
4.06 Learning (including barriers)
4.07 Pain
4.08 Function/Safety
4.09 Nutrition/Integumentary
4.10 Psychosocial (including abuse, neglect)
4.11 Discharge Factors and Family Strengths
5. NURSING ASSESSMENT (May be printout of electronic documentation)
Each section should show WDL, exceptions or score. Should be no NAs.
(Systems Assessment on admission and every 12 hours)
CHART:
Note the number of total number of assessments in the chart in this box.
5.01 Pain
5.02 CAM Screening complete
5.03 Neurological
5.04 Respiratory
5.05 Cardiovascular/PVS
5.06 Abdominal
5.07 Integumentary including location of lines, drains, tubes, wounds, pressure ulcers
5.08 Musculoskeletal/Mobility
5.09 Psychosocial including suicide assessment
5.10 Genitourinary
5.11 Braden Scale (completed with each assessment)
5.12 Fall Risk completed
5.13 Safety needs addressed, as appropriate
6. HAND-OFF OF CARE (HOC)
CHART:
1
Y N
2
Y N
3
Y N
4
Y N
Y N NA Y N NA Y N NA Y N NA
If patient transferred, documentation of hand-off includes: (NA if no transfer)
Note number of hand-off reports (last page with signatures) in chart (in progress notes)
6.01 Did the sending unit complete and sign the report and/or provide hand-off documentation on
the flow sheet?
6.02 Did the receiving unit complete and sign the report and/or provide hand-off documentation
on flow sheet?
6.03 If the patient returns to the sending unit (as from a test/procedure) is the hand-off report
completed by the receiving nurse and/or documentation on the flow sheet?
7. FLOWSHEET
(May be a print-out of electronic documentation)
CHART:
Note the total number of flowsheets in the chart.
For each flowsheet there should be documentation as below.
7.01 Was implementation of comfort plan initiated within 1 hour after pain identified and
assessed? (NA if no pain)
7.02 Pain Intervention was documented within 1 hour of pain score unacceptable to pt
(N/A if no pain or pain within pts comfort goal)
7.03 Were there clinical triggers noted that would indicate activation of the MET, PERT or NERT
team? (N/A if no clinical indication for a team)
7.04 Was the team activated? (See MET/PERT/NERT flowsheet) (N/A if no triggers)
Y N NA Y N NA Y N NA Y N NA
MEDICAL RECORD AUDIT TOOL
8. DAILY CARE PLAN
CHART:
Page 3 of 4
1
Note the total number of Care Plans
Y N NA Y N NA Y N NA Y N NA
8.01 Are general goals initiated or continued daily? Patient admitted to hospital
8.02 Are general goals initiated or continued daily? Patient admitted to hospital
8.03 If unique needs are identified, are corresponding interventions noted?
(NA if no unique needs)
8.04 If unique needs are identified, are corresponding interventions noted?
(NA if no unique needs)
9. PATIENT AND FAMILY EDUCATION
Nights
Days
Nights
Days
CHART:
Y N NA Y N NA Y N NA Y N NA
Patient/family/significant other are provided education specific to their needs, condition and care?
Note total number of education sessions.
When education was provided, did each session include each of the following?
9.01 Teaching is amended to address any learning barriersNoted in Comments.
(NA if no barriers.)
9.02 Learner
9.03 Method
9.04 Response
Documentation of topic taught during admission. Check any topics taught during admission:
9.05 General
9.06 Diagnosis/Illness/Injury
9.07 Before/after surgery/procedures/treatment
9.08 Safety
9.09 Activity/mobility
9.10 Self-care/ADLs
9.11 Pain management
9.12 Medications
9.13 Equipment/supplies
9.14 Diet/nutrition
9.15 Coping
9.16 Infection prevention and control
9.17 Wounds/lines/drains/airways
9.18 Discharge/followup
10. INTERDISCIPLINARY PATIENT CARE
PLANNING ROUNDS (Interdisciplinary Plan of Care,
CHART:
Social Work D/C Note, PTP, Therapy Notes/Discharge Plan)
10.01 Is there evidence of an individualized plan of care, treatment and services based on screening/
1
Y N
2
Y N
3
Y N
4
Y N
assessment that provides the opportunity to involve patients and families as appropriate?PS Goal 13
10.02 Was interdisciplinary discharge planning started within 48 hours of admission?
10.03 Coordination is noted among disciplines providing care, treatment, teaching and services.
11. OVERALL DOCUMENTATION All patient medical record entries must
be legible, complete, and authenticated (in written or electronic form) by the responsible
person, consistent with hospital policies and procedures. All documentation must have
CHART:
name/signature and/or PIC plus date/time.
11.01 Overall, does documentation meet this standard?
11.02 If there are any abbreviations, are they approved? Do not use U, IU, QD, QOD, MS,
MSO4, or MgS04
If NO is checked, note date/time/providers:
Y N
Y N
Y N
Y N
MEDICAL RECORD AUDIT TOOL
CLOSED CHART Nursing Review within 7 Days of Discharge
Page 4 of 4
12. DISCHARGE INFORMATION REVIEW FOUR CLOSED (POST-DISCHARGE) CHARTS WITHIN 7 DAYS OF DISCHARGE.
PLEASE AUDIT THE COMPLETE PAPER MEDICAL RECORD
9CHECK THE APPROPRIATE BOX, EITHER: 9Y = Yes 9N = No 9NA = Not Applicable
Unit:
CHART 1
CHART 2
CHART 3
CHART 4
Medical Record Number:
Admit Date:
Audit Date:
Reviewer(s):
(Progress Notes, SW D/C Note, D/C Instructions, Therapy Notes, Home Health Referral, CHART:
1
2
3
4
MD Discharge Summary)
Y N NA Y N NA Y N NA Y N NA
12.01 Was the patient/family given information about discharge including (as applicable):
reason, how to obtain further care, treatment and services to meet his/her needs;
pain management plan?
12.02 If applicable, did the hospital help arrange for services to meet the patients needs after
discharge? (NA if no services needed)
12.03 Was a list of medicines provided to the patient/family?
12.04 Were discharge instructions and other teaching tools given to the patient/family and did the
patient/family demonstrate understanding?
12.05 If patient does not speak English was an interpreter (live or phone) used to provide instructions?
(NA if patient spoke English)
12.06 If applicable, was patient given choice of services/agencies? (NA if no services offered)
If the patient was discharged to a facility or home with home health, clinical information was provided
including: (NA if standard discharge to home)
12.07 Reason for discharge, physical, and psychosocial status.
12.08 A summary of care, treatment, and services provided and progress toward goals.
12.09 Community resources or referrals or other specific needs after discharge
FOR PATIENTS LESS THAN 18 YEARS OLD
13. PEDIATRIC CARE ASSESSMENT ADDENDUM
CHART:
For children (under 18 years)
Does the assessment of infants, children and adolescents include?
13.02 Length/height
13.03 Weight
13.04 Immunization status
13.05 If applicable, newborn care (NA if not newborn)
13.06 Are the specific academic educational needs of the child or youth identified
and implemented?
13.07 Are family/guardian expectations for and involvement in the assessment, initial treatment,
and continuing care of the patient documented?
RELATED MEDICAL CENTER POLICIES
0125 Diagnostic Testing
0129 Hospital Education
0146 Blood Use
0153 Conscious Sedation
0159 Restraints
0197 Suicide Precautions
0213 Abuse & Neglect
Y N NA Y N NA Y N NA Y N NA
13.01 Developmental age
0024 Consent
0025 Discharge Planning
0026 Pt Rights & Responsibilities
0063 Inpatient Transfers
0091 Infection Control & Prevention
0094 Documentation
0097 Bed Assignment
0239 Pain
0259 Medications
0965 Emergency Response
0269 Patient Education
CCS Documentation Guidelines
You might also like
- Medical Records Audit ChecklistDocument2 pagesMedical Records Audit ChecklistSrinivas Polikepati94% (47)
- Code Pink Drill Report - 13.03.2023Document6 pagesCode Pink Drill Report - 13.03.2023saravana kumar100% (4)
- Apex Quality ManualDocument141 pagesApex Quality ManualDiksha Gumber100% (2)
- Republic of The Philippines Department of Health Southern Isabela Medical CenterDocument5 pagesRepublic of The Philippines Department of Health Southern Isabela Medical Centerkrull243100% (3)
- Antibiotics Audit ChecklistDocument1 pageAntibiotics Audit ChecklistPrabhat Kumar100% (1)
- Nursing Care Plan For AppendectomyDocument5 pagesNursing Care Plan For Appendectomyvanessajane0989% (45)
- Medical Record Review FormDocument3 pagesMedical Record Review FormSimon Dzokoto100% (1)
- Nursing Clinical Privileges Department: ICU /NICU /LRDocument3 pagesNursing Clinical Privileges Department: ICU /NICU /LRKUMARJIT SAHA80% (5)
- Apex Quality Manual-Ashwini Ver 2Document101 pagesApex Quality Manual-Ashwini Ver 2MANORANJANNo ratings yet
- Quality Indicators 5th Edition WordDocument14 pagesQuality Indicators 5th Edition Wordtanisha100% (2)
- Mortuary Services Checklist - Random 202335531Document4 pagesMortuary Services Checklist - Random 202335531Marion KonesNo ratings yet
- CSSD Audit Check List PDFDocument2 pagesCSSD Audit Check List PDFashav62580% (5)
- Clinical Audit - RestraintDocument19 pagesClinical Audit - Restraintsanisani1020100% (2)
- Ipsg ChecklistDocument2 pagesIpsg ChecklistRAJAN KUMAR thakur100% (3)
- Checklist of Quality Indicators For NABH Accreditation PreparationDocument11 pagesChecklist of Quality Indicators For NABH Accreditation PreparationQUALITY SIDARTH HOSPITALS100% (3)
- Quality IndicatorsDocument10 pagesQuality IndicatorsKanna Nikitha100% (1)
- Patient Safety and Quality Improvement (PSQ) Manual: Document Name Document Number Date of IssueDocument30 pagesPatient Safety and Quality Improvement (PSQ) Manual: Document Name Document Number Date of IssueSooraj ThomasNo ratings yet
- Medical Records Audit ChecklistDocument2 pagesMedical Records Audit ChecklistAmbika Ghosh67% (3)
- Infection Control Checklist Nursing DepartmentDocument5 pagesInfection Control Checklist Nursing DepartmentKhaskheli Nusrat100% (2)
- Committee and Meetings (Infection Control)Document3 pagesCommittee and Meetings (Infection Control)Lua CJ100% (5)
- Sop of Code BlueDocument5 pagesSop of Code Bluesucharita Das100% (1)
- MRD ProtocolDocument27 pagesMRD ProtocolVarun Marar67% (3)
- Emergency Department Crowd ManagementDocument4 pagesEmergency Department Crowd ManagementPrabhat Kumar100% (1)
- Checklist of Housekeeping Services For NABH AccreditationDocument4 pagesChecklist of Housekeeping Services For NABH AccreditationDnyanesh Aitalwad100% (3)
- 2019 Audit ChecklistDocument27 pages2019 Audit ChecklistChhaiyaAgrawalNo ratings yet
- In Patient Wardrs ChecklistDocument4 pagesIn Patient Wardrs ChecklistDnyanesh Aitalwad0% (1)
- Nursing ICUDocument2 pagesNursing ICUKomal Tomar67% (3)
- Nursing PrivilegesDocument116 pagesNursing PrivilegesHrishikesh KalgaonkarNo ratings yet
- Privileging - Resident Medical OfficerDocument6 pagesPrivileging - Resident Medical OfficerAjaiwant Cheema100% (1)
- QSP 07 Quality Assurance Programme For Intensive Care Units & HduDocument10 pagesQSP 07 Quality Assurance Programme For Intensive Care Units & HduAniruddha ChatterjeeNo ratings yet
- Nabh FormDocument14 pagesNabh Formakshay raneNo ratings yet
- Departmental Nursing Orientation ChecklistDocument2 pagesDepartmental Nursing Orientation ChecklistMero Hassan67% (3)
- NABH Traing Schedule 2Document7 pagesNABH Traing Schedule 2umeshbharti100% (2)
- Initial Sheet Medical Case Sheet AuditDocument2 pagesInitial Sheet Medical Case Sheet AuditSrinivas Polikepati0% (1)
- Manual Medical Records NabhDocument21 pagesManual Medical Records NabhSadaf SadafNo ratings yet
- Checklist of Training Topics (Department Wise) : Top Management Training Topic Coverage Relevant ToDocument14 pagesChecklist of Training Topics (Department Wise) : Top Management Training Topic Coverage Relevant ToEka B50% (4)
- Chapter-PSQ PSQ 1Document6 pagesChapter-PSQ PSQ 1balaji srinivasan0% (1)
- Kpi Wards 2021 - A WingDocument48 pagesKpi Wards 2021 - A WingPriya LaddhaNo ratings yet
- Crash Cart AuditDocument1 pageCrash Cart AuditGAGANJOT85100% (1)
- Surgical Site Marking PolicyDocument11 pagesSurgical Site Marking PolicymiraNo ratings yet
- PROSPECT APACHE II Calculation WorksheetDocument1 pagePROSPECT APACHE II Calculation WorksheetHamza MahmoudNo ratings yet
- Hospital Infection Control ManualDocument59 pagesHospital Infection Control Manualابراهيم الحربيNo ratings yet
- Apollo KH Hospital: Nursing ManualDocument5 pagesApollo KH Hospital: Nursing ManualSheela Solomon100% (5)
- Cqi Indicators As Per Nabh 4Th Edition: S. No. Standard Ref. Deptt. KPI Formula FrequencyDocument6 pagesCqi Indicators As Per Nabh 4Th Edition: S. No. Standard Ref. Deptt. KPI Formula FrequencyNatasha Bhasin100% (1)
- INDICATORSDocument15 pagesINDICATORSMonish ParmarNo ratings yet
- Updated Code Blue Mockdrill SheetDocument5 pagesUpdated Code Blue Mockdrill SheetChandu Pandit100% (1)
- Nursing Self Assessment ToolkitDocument19 pagesNursing Self Assessment ToolkitJasmeet KaurNo ratings yet
- Medical Case Sheet AuditDocument2 pagesMedical Case Sheet AuditSrinivas PolikepatiNo ratings yet
- Deficiency of Case SheetDocument15 pagesDeficiency of Case SheetberliyaNo ratings yet
- MRD Checklist: All Patient Sr. No. IPD ResponsibilitiesDocument1 pageMRD Checklist: All Patient Sr. No. IPD Responsibilitiesamit100% (5)
- Emergency Admission & Transfer RegisterDocument21 pagesEmergency Admission & Transfer RegisterAnkur Singh0% (1)
- ICN Daily Round ChecklistDocument1 pageICN Daily Round Checklistrenu100% (1)
- NABH QI ListDocument9 pagesNABH QI ListMangesh VirkarNo ratings yet
- AAC.6 FinalDocument5 pagesAAC.6 FinalJatoveda HaldarNo ratings yet
- Nabh IdicatorsDocument61 pagesNabh IdicatorsStacy King100% (6)
- Hospital Staffing PlanDocument1 pageHospital Staffing PlanMilin Anik'sNo ratings yet
- Report On HIRA in Fortis Hospital AmritsarDocument15 pagesReport On HIRA in Fortis Hospital AmritsarUmar LoneNo ratings yet
- Hic ManualDocument260 pagesHic ManualVamshi Narean Naidu100% (3)
- Checklist For CSSD For NABH Preparation and Its Quality IndicatorsDocument3 pagesChecklist For CSSD For NABH Preparation and Its Quality IndicatorsPayal Thakker100% (1)
- 5thEdGuidelines Converted1Document226 pages5thEdGuidelines Converted1ravi4ramaniNo ratings yet
- Generic, Nursing, Icu Ca Tool - Updated 28 January 2023-1 - Day OneDocument786 pagesGeneric, Nursing, Icu Ca Tool - Updated 28 January 2023-1 - Day Oneangela mwakalileNo ratings yet
- DR Bach Flower Remedies - lLATEST BOOK 29-04-2015 Inside Copier 2000 CopiesDocument50 pagesDR Bach Flower Remedies - lLATEST BOOK 29-04-2015 Inside Copier 2000 CopiesTsathiesh KumarNo ratings yet
- Rut Kow 2003Document24 pagesRut Kow 2003Raja VeerappanNo ratings yet
- BookchaptercraniofacialDocument12 pagesBookchaptercraniofacialzeeshan bangashNo ratings yet
- Leica M820 F19 Bro enDocument12 pagesLeica M820 F19 Bro enklim56No ratings yet
- Fabs and Onco Post TestDocument20 pagesFabs and Onco Post TestJe KirsteneNo ratings yet
- Epidural Anesthesia: Factors Affecting Height and Local Anesthetic UsedDocument65 pagesEpidural Anesthesia: Factors Affecting Height and Local Anesthetic UsedRamli MustaphaNo ratings yet
- The Standards of Care For Gender Identity DisordersDocument31 pagesThe Standards of Care For Gender Identity DisorderskatecchinNo ratings yet
- 3503 EZ Slide Operating TableDocument8 pages3503 EZ Slide Operating TablesigmakarsaNo ratings yet
- Masters in Hand Surgery Faculty ProfileDocument8 pagesMasters in Hand Surgery Faculty ProfileVaikunthan RajaratnamNo ratings yet
- Dr. Vicky Resume - 2024Document3 pagesDr. Vicky Resume - 20245ydkgm94ckNo ratings yet
- Cardiac Surgery TextbookDocument2 pagesCardiac Surgery Textbookoguzguneri2010No ratings yet
- Alan Immerman - Health Unlimitred PDFDocument95 pagesAlan Immerman - Health Unlimitred PDFHMNo ratings yet
- Calbayog District Hospital (CDH)Document6 pagesCalbayog District Hospital (CDH)Nelin BarandinoNo ratings yet
- SVC200203 - ST Vincent's Clinic A4 Booklet Web FinalDocument84 pagesSVC200203 - ST Vincent's Clinic A4 Booklet Web Finalkeerthi.sakthi0794No ratings yet
- Venous Association of IndiaDocument178 pagesVenous Association of IndiaKriti KumariNo ratings yet
- Medical Negligence Coverage of The Profession DutiDocument7 pagesMedical Negligence Coverage of The Profession DutiAnggreanyAshariNo ratings yet
- Fractal Robots Seminar ReportDocument27 pagesFractal Robots Seminar ReportAkhil ThomasNo ratings yet
- VistaDent 3DDocument4 pagesVistaDent 3DJay Ramachandran100% (1)
- 135 Infections of The External EarDocument12 pages135 Infections of The External EarDickyJuliandaNo ratings yet
- G.R. No. 198501 Kestrel Shipping Inc. v. MunarDocument12 pagesG.R. No. 198501 Kestrel Shipping Inc. v. MunarJa RuNo ratings yet
- Đề olympic 1Document22 pagesĐề olympic 1tranttthuy2010No ratings yet
- 2 51 1630666840 9ijmpsdec20219Document8 pages2 51 1630666840 9ijmpsdec20219TJPRC PublicationsNo ratings yet
- Pro MetricsDocument129 pagesPro MetricslianausinNo ratings yet
- Principles of Oncology NursingDocument12 pagesPrinciples of Oncology NursingДария Коваленко100% (2)
- RT 220 B C AirwaystudyguideDocument25 pagesRT 220 B C Airwaystudyguiderpebdani0% (2)
- Pattern and Categorisation of Neurosurgical Emergencies: Conference ProceedingDocument3 pagesPattern and Categorisation of Neurosurgical Emergencies: Conference ProceedingarshadNo ratings yet
- Kam Musika Hospital ProfileDocument11 pagesKam Musika Hospital ProfileEmmanuel John MsovelaNo ratings yet
- CPG Recommendations For Patient Safety and Minimal Monitoring Standards During Anaesthesia and Recovery PDFDocument21 pagesCPG Recommendations For Patient Safety and Minimal Monitoring Standards During Anaesthesia and Recovery PDFDzarrinNo ratings yet