Blood Pressure Variability: How To Deal?: NR Rau, Gurukanth Rao
Blood Pressure Variability: How To Deal?: NR Rau, Gurukanth Rao
Uploaded by
Rully SyahrizalCopyright:
Available Formats
Blood Pressure Variability: How To Deal?: NR Rau, Gurukanth Rao
Blood Pressure Variability: How To Deal?: NR Rau, Gurukanth Rao
Uploaded by
Rully SyahrizalOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Blood Pressure Variability: How To Deal?: NR Rau, Gurukanth Rao
Blood Pressure Variability: How To Deal?: NR Rau, Gurukanth Rao
Uploaded by
Rully SyahrizalCopyright:
Available Formats
Blood Pressure Variability: How to deal?
3:3
NR Rau, Gurukanth Rao, Manipal
Affecting 1 billion people worldwide, hypertension remains the most common, readily identifiable,
and reversible risk factor for myocardial infarction, stroke, heart failure, atrial fibrillation, aortic
dissection, and peripheral arterial disease. Because of escalating obesity and population aging, the
global burden of hypertension is rising and projected to affect 1.5 billion personsone third of the
worlds populationby the year 2025. Currently, high blood pressure (BP) causes about 54% of
stroke and 47% of ischemic heart disease worldwide.1
BP varies considerably in individual subjects and may vary significantly throughout the day. This
variation causes considerable difficulties in identifying individuals who have hypertension. The
differing BP values are due to both biologic variation (variations of pressures within a given individual)
and variation in the measurement itself. Errors in measurement can be minimized by attention to
the proper technique for recording Blood Pressure. Biologic variation is addressed by repeated BP
measurement at a given visit (at least two pressures taken at least 5 minutes apart or additional BP
measurements if there is a 5-mm Hg difference between repeated measures). In addition, in most
patients with milder forms of hypertension, repeated measurements during different clinic visits over
time are recommended to approach the true Blood pressure.
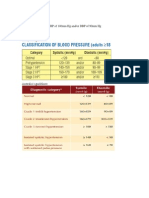
Definition
Hypertension currently is defined as a usual BP of 140/90 mm Hg or higher, for which the benefits
of drug treatment have been definitively established. This conservative definition has been called
into question by epidemiologic data showing continuous positive relationships between the risk of
coronary artery disease (CAD) and stroke deaths with systolic or diastolic BP down to values as low
as 115/75 mm Hg. This artificial dichotomy between hypertension and normotension can delay
medical treatment until vascular health has been irreversibly compromised by elevated BP values
previously considered to be normal. Thus, for certain high-risk patients, especially those with CAD,
the recommended medical treatment threshold recently has been lowered to 130/80 mm Hg
Labile Hypertension
Most guidelines for treating hypertension focus on the average blood pressure (BP) assessed from
either home or office readings. Little attention is paid, however, to BP lability. Virtually all physicians
are familiar with the term labile hypertension, yet there are no quantitative criteria to define or diagnose
it. Its effects on cardiovascular (CV) outcome are unclear, and there are no guidelines for its treatment.
The effect of treating the labile component of hypertension on CV outcome is also unknown. Despite
this, labile BP elevation is a commonplace clinical dilemma.
It is normal for BP to fluctuate from moment to moment and from day to day. BP fluctuation is related
to many factors such as physical activity, emotion, position, respiratory cycle, diet, salt intake, alcohol
ingestion, sleep deprivation, and others. Even in otherwise normotensive individuals, BP fluctuation
can be substantial during momentsof physical or emotional stress or even without overt provocation.
In physicians offices, readings can be very stable in some patients, while varying markedly in others.
117
Medicine Update 2012 Vol. 22
coat hypertension. Surprisingly, studies show that patients
with white coat hypertension do not have abnormal lability
outside of physicians offices.4
Table 1 : Blood Pressure Lability as a Clinical Dilemma
The alerting phenomenon (white coat hypertension)
Labile hypertension (including preprocedural hypertension)
Paroxysmal hypertension
Normal lability in patients with vulnerable underlying conditions
Cerebral aneurysm
Chronic aortic dissection
Amyloid angiopathy
Marfan syndrome
Angina
Labile Hypertension
BP VARIABILITY REACTIVITY AND LABILITY
In describing the tendency of BP to fluctuate, the terms
variability, reactivity, and lability have been widely used.
BP variability is usually defined as the average variation of
BP throughout the day, quantitated as the standard deviation
of ambulatory BP readings. It is increased in hypertensive
individuals and increases with aging.
BP reactivity is defined as the response to environmental
stressors, usually quantitated as responses to standardized
laboratory stressors. In both the laboratory and clinical realms,
individuals with increased reactivity are sometimes referred
to as hot reactors.
BP reactivity is difficult to quantitate because an individuals
reactivity differs from stressor to stressor and even upon
retesting with the same stressor.2 Further obscuring its
meaningfulness, reactivity in the laboratory is not strongly
predictive of reactivity to real-life stressors. Although many
have suspected that BP reactivity is predictive of future
development of hypertension and of CV risk, studies have
not found this to be true.3
BP lability is characteristic of human BP, and there is no clear
definition that differentiates normal from abnormal lability.
The term labile hypertension, although widely used, also lacks
an accepted definition and is more a clinical impression than
a specific diagnosis.
LABILE COMPONENT OF BP AS A CLINICAL
DILEMMA
Four circumstances in which the labile component of BP is
a clinical issue are listed in Table 1 and are discussed below.
As indicated in the Table 1, the terms labile hypertension and
paroxysmal hypertension are used to denote different disorders
of BP lability. They appear to have different characteristics
and require different treatment.
The Alerting Phenomenon
The alerting phenomenon is the tendency of BP to rise at
the time of measurement, usually, but not always, due to
consciously perceived anxiety over the measurement.Although
typically described as occurring during measurement by a
physician, it can also occur during measurement at home.
When limited to physicians offices, it is regarded as white
Patients with labile hypertension experience transient but
substantial increases in BP. The increases often, but not always,
occur in the setting of emotional distress, particularly anxiety,
and are likely mediated by sympathetic activation. Labile
hypertension can be asymptomatic or can be accompanied
by symptoms such as headache, palpitations or flushing.
The BP usually falls spontaneously without intervention. BP
elevation is usually readily attributed to emotional stress, by
both physician and patient.
Paroxysmal Hypertension (Pseudopheochromocytoma)
In contrast to patients with labile hypertension, inpatients with
paroxysmal hypertension(pseudopheochromocytoma), BP
elevation generally occurs in the absence of overt emotional
distress, with most patients describing the paroxysms as having
occurred out of the blue.5 Paroxysms characteristically
begin very abruptly and can last minutes, hours, or even
days5. Abrupt BP elevation is accompanied by prominent
and very distressing physical symptoms, such as headache,
palpitations, flushing, weakness, or dyspnea5. The paroxysms
often provoke a marked fear of imminent death or stroke;
the fear follows rather than precedes the onset of physical
symptoms. Fear of recurrent symptomatic paroxysms can lead
to restriction of lifestyle and functioning.
Biochemical screening for a pheochromocytoma is mandatory,
although such a tumor is found in<2% of patients with
paroxysmal hypertension. Catecholamine studies are usually
normal but can be mildly abnormal either during or even
between paroxysms, reflecting activation of the sympathetic
nervous system.6
Normal Lability in Patients with Vulnerable Underlying
Conditions
Although fluctuation of BP is a normal phenomenon, even
normal lability would seem potentially harmful in patients
with certain medical conditions. For example, in patients
with chronic aortic dissection, Marfan syndrome, angina, or
cerebral aneurysm, and possibly in patients with recurrent
nonhypertensive cerebral hemorrhage from amyloid
angiopathy, transient BP elevation might be deleterious and
reduction of even normal lability could be beneficial.
TREATMENT
To date, the treatment of hypertension has focused on
measurement of resting BP. Virtually no attention has been
given to the indications for, and benefit of, treatment of the
labile component of BP elevation or to the drug treatment
strategies that might best reduce BP lability.
118
Blood Pressure Variability: How to deal?
Table 2 : Suggested Indications and Regimens for
Pharmacologic Treatment of Labile Forms of Hypertension
Preprocedural blood pressure (BP) elevation
Prophylactic management
Oral -blocker + -blocker for 23 days and or anxiolytic
agent
Acute management
Intravenous (IV) labetalol and or anxiolytic agent (oral or IV)
Severe labile hypertension
Acute management
Indications for acute management not established
Consider intravenous labetalol if severe or symptomatic
elevation
Chronic management
Oral -blocker + -blocker + other agents if resting BP is
elevated
Runaway anxiety about BP readings
Acute management
Not indicated
Chronic management
Oral -blocker + -blocker
to reduce BP variability. Monotherapy with either a diuretic,
angiotensin-converting enzyme (ACE) inhibitor, blocker, or
-blocker does not reduce BP reactivity to stressors, although
lowering of resting BP will predictably lower peak pressure
as well.
Contrary to widespread belief, studies consistently show
that -blocker monotherapy does not reduce BP reactivity to
stressors.7 It mitigates the increase in heart rate and cardiac
output but does not reduce BP reactivity, which is maintained
instead by an increase in peripheral resistance.
Similarly, -blocker monotherapy blocks the increase in
peripheral resistance, but BP reactivity is unaltered due to an
increase instead in cardiac output. In contrast, studies suggest
that the combination of an - and -blocker, which blocks
increases in both cardiac output and peripheral resistance,
does reduce BP reactivity.8
APPROACH TO DRUG THERAPY FOR
BPLABILITY
Paroxysmal hypertension
Acute management of paroxysms
Severe paroxysm (e.g., systolic BP >220 mm Hg or diastolic
BP >130 mm Hg, or lower readings depending on clinical
circumstances) or severe symptoms
IV labetalol or IV nitroprusside
Milder paroxysms
Central -agonist (e.g., oral clonidine ) and or anxiolytic
Or oral -blocker + -blocker with fairly rapid onset
(e.g., labetalol or metoprolol + prazosin)
Chronic preventive management
Less intensive regimen: for mild to moderate recurring
paroxysms
-Blocker + -blocker
More intensive regimen
(if frequent, severe paroxysms despite - -blockade and
or reduced functioning resulting from recurring paroxysms):
Antidepressant agent (SSRI or tricyclic or other antidepressant
agent),probably with -blocker + -blocker
Normal lability in patients with vulnerable underlying
conditions
Chronic management
Oral -blocker + -blocker combined with other agents
to achieve lowest acceptable resting BP
Treatment of BP Variability and BP Reactivity
Little attention has been paid to the effect of drug treatment on
BP variability or reactivity or to the effect of such treatment on
CV outcome. Antihypertensive drug therapy does not appear
Eliminating BP lability is not possible but reducing it is often
achievable. A regimen that antagonizes sympathetically
mediated BP elevation would seem more logical than
treatment with agents directed at other mechanisms, such as
ACE inhibitors, ARBS or diuretics, the mainstays of treatment
of sustained hypertension
The clear relationship between sympathetic activation and
BP reactivity to emotional distress and the documented effect
of combined -blockade on sympathetically mediated BP
reactivity to laboratory stressors suggest a role for combined
-blockade in treating patients with labile hypertension.
Carvedilol and labetalol each provides both and -blocking
effects but might not be ideal because of unpredictable
bioavailability resulting from first-pass hepatic metabolism.9,10
Alternatively, two separate agents, a -blocker, preferably one
whose -blocking effect is not greatly affected by hepatic
metabolism (e.g., atenolol, nadolol, bisoprolol, betaxolol, or
nebivolol), combined with an -blocker, such as prazosin,
can be prescribed.
The Alerting Phenomenon and White
Coat Hypertension
The treatment of white coat hypertension has engendered
considerable controversy. It would seem unnecessary, and
perhaps harmful, to prescribe antihypertensive drugs if home
readings are truly normal, as treatment could confer the risk
of iatrogenic hypotension. However, given the increased
likelihood of developing sustained hypertension, patients need
to be observed for progressive elevation of home readings over
time. Treatment should be aimed at reducing home BP, if it is
elevated, using the usual pharmacologic agents.
119
Medicine Update 2012 Vol. 22
Labile Hypertension (Including Preprocedural BP Elevation)
There are no recognized criteria for treating labile hypertension,
other than the mean 24-hour BP observed on ambulatory
monitoring. Frequent home monitoring, which can foster
anxiety and elevated readings, should be discouraged. In
patients whose hypertension is characterized by frequent
severe elevations, e.g., systolic readings >180mm Hg, or who
have runaway anxiety about their BP, treatment to achieve
more normal readings can be helpful both in lowering BP
and in reducing the vicious cycle of anxiety. Here, institution
of a regimen combining an - and -blocker, at their usual
dosages, would seem preferable to an as-needed regimen that
perpetuates the constant rechecking of BP.
In patients who repeatedly experience marked and problematic
BP elevation when presenting for medical or surgical
procedures, intravenous administration of an anxiolytic
agent and/or the -blocker labetalol can acutely lower BP. A
prophylactic regimen consisting of an - and a-blocker (any
standard -blocker given in combination with an -blocker,
such as prazosin (2.5-5mg once or twice daily), given for 2 or
3 days, can often mitigate the preprocedural elevation in BP. If
necessary, an anxiolytic agent, such as lorazepam (0.52 mg),
or alprazolam (0.251 mg), can also be administered shortly
before the procedure.
Temporary treatment with a central -agonist, such as
clonidine, is another possible alternative, usually given at a
dose of 0.1 to 0.2 mg every 8 hours.
Paroxysmal Hypertension
The difficult problem of treating paroxysmal hypertension,
which can be disabling, has recently been reviewed.
Pharmacologic, psychopharmacologic, and psychologically
based interventions alone or in combination can eliminate
paroxysms in most patients and enable resumption of a normal
life. Treatment may involve acute management to lower BP and
reduce symptoms during paroxysms or chronic management
to prevent recurrent paroxysms, or both (Table 2).
Acute Management of Hypertensive Paroxysms: Pharmacologic and Psychopharmacologic Agents
For patients with severe BP elevation, a rapid-acting
intravenous agent, such as labetalol can be administered. An
intravenous bolus of 10 mg to 20 mg can be given, followed by
repeat boluses of 20 mg to80 mg at 10- to 15-minute intervals
until a response is seen. In the absence of a response or in
the presence of extreme BP elevation nitroprusside can be
administered.
In patients with less severe BP elevation, oral therapy with
clonidine or the combination of an and a-blocker can be
given as an alternative to intravenous treatment. Clonidine can
be given at a dose of 0.1 mg or 0.2 mg repeated after 90 minutes
in nonresponders. - -Blockade can be given as labetalol 100
mg to 300 mg every 6 to 8 hours, with response expected within
1.5 to 2.5 hours or alternatively as a -blocker with fairly rapid
onset of action, such as metoprolol (2550 mg orally every
6 hours), combined with prazosin (1 mg orally every 812
hours). Milder paroxysms can be managed in some patients
with a rapid-acting anxiolytic agent, such as alprazolam,
given alone or in combination with an antihypertensive agent.
Under a physicians supervision, reliable patients who have
responded well to clonidine and or an anxiolytic agent can
self-administer either or both drugs at home during subsequent
paroxysms rather than seek emergency department care for
each attack. Clonidine can be taken at a dosage of0.1 mg or
0.2 mg and repeated at 6- to 8-hourintervals.
Chronic Preventive Management: Pharmacologic and Psychopharmacologic
Agents
Chronic therapy with an -blocker combined with ablocker given orally has been reported to reduce severity of
BP elevation during paroxysms. Extended use of a central
-agonist such as clonidine has not been reported and in many
cases its use would be limited by side effects, particularly
fatigue.
The use of antidepressant and anxiolytic agents to prevent
attacks was suggested by the similarity of the syndrome to
panic disorder. Antidepressant agents, including selective
serotonin reuptake inhibitors and tricyclic antidepressants,
have been reported to prevent recurrent paroxysms in most
patients at dosages recommended for treating panicdisorder.11
For patients with mild or infrequent paroxysms, acute
management with alprazolam or clonidine and or maintenance
therapy with combined a- and b-blockade is usually sufficient.
An antidepressant should be considered mainly in patients
with severe and recurrent hypertensive paroxysms or in those
in whom the disorder has resulted in impaired functioning.
Psychological Interventions
Reassurance
Symptomatic hypertensive paroxysms are terrifying to most
patients, and the fear of dying during an attack can come to
dominate their life. A physicians confident reassurance that
the disorder can be treated and that a catastrophic event or
death during a paroxysm is very unlikely can help reduce the
terror and possibly the number and severity of attacks.
Awareness
In some cases, gaining awareness of the origin of the disorder
in repressed emotions can reduce or eliminate recurrence of
paroxysms. In patients open to such awareness, subsequent
psychotherapy can be helpful. However, most patients who
120
Blood Pressure Variability: How to deal?
are survivors of severe trauma will continue to defend against
awareness of potentially overwhelming emotion. They are
unlikely to be interested in or benefit from psychotherapy and
should not be coerced into it. Among patients who do not have
a history of trauma but who have a lifelong tendency to repress
emotions, psychotherapy is an option, although a repressive
coping style is difficult to alter.
Normal Lability in Patients with Vulnerable Underlying Conditions
Treatment of the labile component of BP inpatients with
underlying comorbidities (Table 1) is also an area that has
been inadequately studied. In the example of patients with
chronic aortic dissection, most physicians focus on achieving
the lowest possible resting BP. Treatment with combined
and b-blockade, given its observed effects on BP reactivity, in
addition to its ability to lower resting BP, would seem logical
and merits consideration for both further study as well as
empiric use.
References
1.
2. Grassi G. Evaluating sympathetic and hemodynamic responses to mental stressors: hankering or achievement? J Hypertens
1996;14:11551157
3.
Krantz DS, Manuck SB. Acute psychophysiologic reactivity and
risk of cardiovascular disease: a review and methodologic critique. Psychol Bull 1984;96:435464.
4.
Munakata M, Hiraizumi T, Tomiie T, et al. Psychobehavioral factors involved in the isolated office hypertension: comparison with
stress-induced hypertension. J Hypertension 1998;16:4194122.
5.
Mann SJ. Severe paroxysmal hypertension (pseudopheochromocytoma): understanding its cause and treatment. Arch Intern Med
1999;159:670674.
6.
Sharabi Y, Goldstein DS, Bentho O, et al. Sympathoadrenal function in patients with paroxysmal hypertension: pseudopheochromocytoma. J Hypertens 2007;25:22862295.
7.
Mills PJ, Dimsdale JE. Cardiovascular reactivity to psychosocial
stressors. A review of the effects of beta blockade. Psychosomatics 1991;32:209220.
8.
Julius S. The blood pressure seeking properties of the central nervous system. J Hypertens 1988;6:177185.
9.
Morgan T. Clinical pharmacokinetics and pharmacodynamics of
carvedilol. Clin Pharmacokinet 1994;26:335346.
CONCLUSIONS
Although the management of labile forms of hypertensions
a frequently encountered clinical dilemma, specific criteria
for diagnosing labile hypertension and clinical trials to
guide management do not exist. The clinical spectrum of
this problem and a treatment approach based on published
reports and physiologic principles has been presented. Studies
to assess the effects of labile hypertension and outcome of
treatment are needed.
Lawes CM, Vander HS, Rodgers A: Global burden of blood-pressure-related disease, 2001. Lancet 2008;371:1513.
10. Richards DA, Prichard BNC. Clinical pharmacology of labetalol.
Br J Clin Pharmacol 1979;8:89s93s.
11. Mann SJ. Severe paroxysmal hypertension. An autonomic syndrome and its relationship to repressed emotions. Psychosomatics
1996;37:444450.
121
You might also like
- Teaching Plan For HypertensionDocument22 pagesTeaching Plan For HypertensionSheila Mae Alcaide Dagdag80% (15)
- SLE Made EasyDocument482 pagesSLE Made EasySumayyia Qamar100% (1)
- 2009 WHO Lifestyle Manual Module1 Overview NCDDocument49 pages2009 WHO Lifestyle Manual Module1 Overview NCDRazel Kinette AzotesNo ratings yet
- Dissertation-The Work of Byron Katie-Fabrice Nye 2011Document128 pagesDissertation-The Work of Byron Katie-Fabrice Nye 2011Anonymous 0PYZofvGS100% (3)
- Paul Bragg Healthy HeartDocument260 pagesPaul Bragg Healthy Heartdeborah81100% (9)
- Acute Coronary SyndromeDocument2 pagesAcute Coronary SyndromeRenz Castañaday100% (1)
- Health Teaching PlanDocument10 pagesHealth Teaching PlanMariel Colminas100% (2)
- Dent Clin N Am 50 (2006) 547-562Document16 pagesDent Clin N Am 50 (2006) 547-562lalajanNo ratings yet
- Variabilitatea TADocument13 pagesVariabilitatea TADaniel StaniloaieNo ratings yet
- Essential HypertensionDocument13 pagesEssential HypertensionIvan KurniadiNo ratings yet
- Makalah Bahasa InggrisDocument9 pagesMakalah Bahasa Inggriswina mersiliaNo ratings yet
- Hypertensive Emergency PDFDocument14 pagesHypertensive Emergency PDFOsiithaa CañaszNo ratings yet
- Uncontrolled Blood PressureDocument6 pagesUncontrolled Blood PressureFika SilviaNo ratings yet
- HypertensionDocument8 pagesHypertensionsalahoveNo ratings yet
- Crisis HipertensivaDocument11 pagesCrisis HipertensivaJakeline MenesesNo ratings yet
- CH 33 Key PointsDocument4 pagesCH 33 Key PointsKara Dawn MasonNo ratings yet
- Sample Questions - True Learn Family MedicineDocument11 pagesSample Questions - True Learn Family MedicinelarazahabiNo ratings yet
- Hypertension, Hypertensive Crisis, and Hypertensive Emergency: Approaches To Emergency Department CareDocument11 pagesHypertension, Hypertensive Crisis, and Hypertensive Emergency: Approaches To Emergency Department CarePebrian SyahNo ratings yet
- Hypertension in ElderlyDocument6 pagesHypertension in ElderlyRamesh RajNo ratings yet
- Hypertension An ApproachDocument47 pagesHypertension An ApproachAhmed Magdy YoussifNo ratings yet
- Hypertension: "The Silent Killer" Because It Generally Has No Symptoms Until Serious Complications DevelopDocument24 pagesHypertension: "The Silent Killer" Because It Generally Has No Symptoms Until Serious Complications Developmaryam ijazNo ratings yet
- HypertensionDocument29 pagesHypertensionمبدر حامدNo ratings yet
- HypertensionDocument5 pagesHypertensiongoinggreen91No ratings yet
- Hypertensive Vascuar Disease (HVD) : By. DR - WondifrawDocument57 pagesHypertensive Vascuar Disease (HVD) : By. DR - WondifrawSebliNo ratings yet
- Hypertension ESC Guideline 2018Document78 pagesHypertension ESC Guideline 2018Theresia KennyNo ratings yet
- Bhagani 2018Document7 pagesBhagani 2018rifky kurniawanNo ratings yet
- Hypertension and Their Management in Dentistry - 2020Document19 pagesHypertension and Their Management in Dentistry - 2020nabilahNo ratings yet
- Hypertension: Definition and EtiologyDocument23 pagesHypertension: Definition and EtiologyharryNo ratings yet
- 2017 Guideline For The Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults - Key Point To RememberDocument6 pages2017 Guideline For The Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults - Key Point To RememberSandy Kartika PurnomoNo ratings yet
- Hypertensive CrisisDocument7 pagesHypertensive CrisisAbdul Hannan Ali100% (1)
- Nursing Care of Gerontik "Hypertension"Document11 pagesNursing Care of Gerontik "Hypertension"Pradhevi Angelita WijayaNo ratings yet
- HypertensionDocument10 pagesHypertensionaa zzNo ratings yet
- Hypertension OutlineDocument14 pagesHypertension OutlineMaria CayacoNo ratings yet
- Nursing Care For Patient With HypertensionDocument13 pagesNursing Care For Patient With HypertensionSachin MadhukarNo ratings yet
- Cardiovascular Effects of HypertensionDocument12 pagesCardiovascular Effects of HypertensionEdwin F. Freecss WoworNo ratings yet
- Health EducationDocument12 pagesHealth EducationGerome T. ManantanNo ratings yet
- Thesis Blood PressureDocument7 pagesThesis Blood PressureJackie Gold100% (1)
- Introduction To HPNDocument4 pagesIntroduction To HPNKarla May Manalastas BorromeoNo ratings yet
- HypertensionDocument6 pagesHypertensionMatthew Michael100% (1)
- Hypertensive CrisisDocument60 pagesHypertensive CrisisDzikrul Haq KarimullahNo ratings yet
- Hypertension Management:: An UpdateDocument10 pagesHypertension Management:: An UpdatePriya RanjanNo ratings yet
- HYPERTENSIONDocument38 pagesHYPERTENSIONtenny21092000No ratings yet
- Management of Hypertension 2018Document55 pagesManagement of Hypertension 2018Mohd Johari Mohd ShafuwanNo ratings yet
- New Microsoft Word DocumentDocument11 pagesNew Microsoft Word DocumentNikitha SinduNo ratings yet
- Cute Hypertension and Hypertensive Crisis in Children: A. George KoshyDocument9 pagesCute Hypertension and Hypertensive Crisis in Children: A. George KoshyAimhigh_PPMNo ratings yet
- HypertensionDocument2 pagesHypertensionRohimahNo ratings yet
- HypertensionDocument14 pagesHypertensiondhearawrsNo ratings yet
- Hypertension KLP 10Document16 pagesHypertension KLP 10Tri ArdiyaniNo ratings yet
- 5 HypertensionDocument219 pages5 Hypertensionrojas.josemanuelNo ratings yet
- Pediatric Hypertension: Why The Rise in Childhood Hypertension?Document9 pagesPediatric Hypertension: Why The Rise in Childhood Hypertension?Peace ManNo ratings yet
- Adults Are Hypertensive.: HypertensionDocument4 pagesAdults Are Hypertensive.: HypertensionNoemi GarciaNo ratings yet
- HypertensionDocument4 pagesHypertensionAnthony Philip Patawaran CalimagNo ratings yet
- Persistent Elevation of SBP of 140mm HG And/or DBP of 90mm HG Classifications Malaysia's GuidelinesDocument4 pagesPersistent Elevation of SBP of 140mm HG And/or DBP of 90mm HG Classifications Malaysia's GuidelinesLaughin KowNo ratings yet
- Definition and Classification of Hypertension - An UpdateDocument4 pagesDefinition and Classification of Hypertension - An UpdateHaidee JavierNo ratings yet
- MergeResult 2023 08 21 10 03 52Document29 pagesMergeResult 2023 08 21 10 03 52gadheaniket00No ratings yet
- JNC 7Document12 pagesJNC 7Theresia KennyNo ratings yet
- The Seventh Report of The Joint National Committee On Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7)Document33 pagesThe Seventh Report of The Joint National Committee On Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7)Wi KuNo ratings yet
- Case HistoryDocument8 pagesCase HistoryjabeensarwarNo ratings yet
- Drchirag Hypertension NoteDocument61 pagesDrchirag Hypertension NoteChirag PatelNo ratings yet
- Hypertension: Solomon E QuaysonDocument47 pagesHypertension: Solomon E QuaysonseadiabaNo ratings yet
- A Simple Guide to Hypertension and Heart DiseasesFrom EverandA Simple Guide to Hypertension and Heart DiseasesRating: 5 out of 5 stars5/5 (1)
- Beating High Blood Pressure Naturally: Your Complete Guide to Self-Care, Healthy Eating, and Herbal Remedies: Self Care, #1From EverandBeating High Blood Pressure Naturally: Your Complete Guide to Self-Care, Healthy Eating, and Herbal Remedies: Self Care, #1No ratings yet
- Lower Your High Blood Pressure Naturally - How To Control High Blood Pressure Without MedicationFrom EverandLower Your High Blood Pressure Naturally - How To Control High Blood Pressure Without MedicationNo ratings yet
- Managing High Blood Pressure: Causes, Prevention, and TreatmentFrom EverandManaging High Blood Pressure: Causes, Prevention, and TreatmentNo ratings yet
- Laporan Pagi Anestesi Operasi Cito Jam DinasDocument1 pageLaporan Pagi Anestesi Operasi Cito Jam DinasRully SyahrizalNo ratings yet
- Bab IiDocument18 pagesBab IiRully SyahrizalNo ratings yet
- Emergency Room Morning Report: October 16th 2017Document68 pagesEmergency Room Morning Report: October 16th 2017Rully SyahrizalNo ratings yet
- Lumbar Laminectomy Diskectomy Fusion PDFDocument3 pagesLumbar Laminectomy Diskectomy Fusion PDFRully SyahrizalNo ratings yet
- Journal Reading: "Direct Current Stimulation of The Ear in Tinnitus Treatment: A Double-Blind Placebo-Controlled Study"Document16 pagesJournal Reading: "Direct Current Stimulation of The Ear in Tinnitus Treatment: A Double-Blind Placebo-Controlled Study"Rully SyahrizalNo ratings yet
- Slide OG MRDocument7 pagesSlide OG MRRully SyahrizalNo ratings yet
- Mapping Tulip 2B (Bangsal Cempaka) : Ny. Nurhayati/ 40 / Kista Ovarium Curiga GanasDocument1 pageMapping Tulip 2B (Bangsal Cempaka) : Ny. Nurhayati/ 40 / Kista Ovarium Curiga GanasRully SyahrizalNo ratings yet
- Mrs. Afiah /29 TH MRS Tgl. 23-03-2017 Pkl. 22:15 WITA SubjectiveDocument5 pagesMrs. Afiah /29 TH MRS Tgl. 23-03-2017 Pkl. 22:15 WITA SubjectiveRully SyahrizalNo ratings yet
- LGM LGM D 09 1Document7 pagesLGM LGM D 09 1Rully SyahrizalNo ratings yet
- Practice Essentials: Essential Updates: Distinguishing Between Left-And Right-Sided Atrial TachycardiaDocument28 pagesPractice Essentials: Essential Updates: Distinguishing Between Left-And Right-Sided Atrial TachycardiaRully SyahrizalNo ratings yet
- Fever Assessment 2013Document9 pagesFever Assessment 2013Rully SyahrizalNo ratings yet
- CHF Case StudyDocument20 pagesCHF Case StudyDelia Soriano AlingayaoNo ratings yet
- Oxford American Cardiology Library HypertensionDocument190 pagesOxford American Cardiology Library HypertensionWesker Albert100% (1)
- 2022 Non-Cardiac SurgeryDocument105 pages2022 Non-Cardiac Surgeryhosameldin ahmedNo ratings yet
- Dyslipidemias in Chronic Kidney Disease: Current Guidelines and Future PerspectivesDocument5 pagesDyslipidemias in Chronic Kidney Disease: Current Guidelines and Future PerspectivesAn-Nisa Khoirun UmmiNo ratings yet
- Anredera Cordifolia Leaves Extract As Antihyperlipidemia and Endothelial Fat Content Reducer in Male Wistar RatDocument5 pagesAnredera Cordifolia Leaves Extract As Antihyperlipidemia and Endothelial Fat Content Reducer in Male Wistar RatRigotti BrNo ratings yet
- 14 To 20 Sep2019Document56 pages14 To 20 Sep2019M KumarNo ratings yet
- Cardiovascular System Abbas HayatDocument35 pagesCardiovascular System Abbas HayatFiaz medicoNo ratings yet
- The Effectiveness of Early Position Change Postcardiac Catheterization On Patient's Outcomes A Randomized Controlled TrialDocument9 pagesThe Effectiveness of Early Position Change Postcardiac Catheterization On Patient's Outcomes A Randomized Controlled TrialAdelia putriNo ratings yet
- Acute Coronary SyndromeDocument48 pagesAcute Coronary SyndromeAchmad ulil Albab100% (1)
- First Day Exam: Physical EducationDocument24 pagesFirst Day Exam: Physical EducationSolstice OshiroNo ratings yet
- PostDocument10 pagesPostNenang SandraNo ratings yet
- Chapter 2 Measuring Health and Disease Occurrence IiDocument32 pagesChapter 2 Measuring Health and Disease Occurrence IiNoly Moh HussinNo ratings yet
- Exams MedsurgDocument29 pagesExams MedsurgUy Jezrielle MicahNo ratings yet
- Health Benefits of Wheat and Its Nutritional ValueDocument13 pagesHealth Benefits of Wheat and Its Nutritional ValueJaime BallesterosNo ratings yet
- Abbreviations KettenbachDocument5 pagesAbbreviations Kettenbachimthebossmc995No ratings yet
- Diabetes Book THAI-ENGDocument100 pagesDiabetes Book THAI-ENGNaharuthai BumrungratanayosNo ratings yet
- Anaphylactic Death FinalDocument73 pagesAnaphylactic Death Finalkhaled eissaNo ratings yet
- Angiographic Profile and Treadmill Test RelationshDocument9 pagesAngiographic Profile and Treadmill Test RelationshRajesh SoaNo ratings yet
- Ekg PJKDocument113 pagesEkg PJKdevipuspaNo ratings yet
- Agustus 2019Document20 pagesAgustus 2019pkmjemursariNo ratings yet
- Perinatal Asphyxia in Term and Late Preterm Infants - UpToDateDocument31 pagesPerinatal Asphyxia in Term and Late Preterm Infants - UpToDateRocio GNo ratings yet
- Convert CSVDocument2,498 pagesConvert CSVSunnt BandiNo ratings yet
- Fasting Insulin Levels Independently Associates With Coronary Heart Diseade in Non-Diabetic Turkish Men and WomenDocument9 pagesFasting Insulin Levels Independently Associates With Coronary Heart Diseade in Non-Diabetic Turkish Men and WomenJanne AraújoNo ratings yet
- NCM 31112L Midterm Exams: RationalizationDocument202 pagesNCM 31112L Midterm Exams: RationalizationWen SilverNo ratings yet
- Coronary Artery AtherosclerosisDocument21 pagesCoronary Artery AtherosclerosisfikriadityaNo ratings yet