Chapter 08 Electron Beams
Chapter 08 Electron Beams
Uploaded by
Đình Quý DươngCopyright:
Available Formats
Chapter 08 Electron Beams
Chapter 08 Electron Beams
Uploaded by
Đình Quý DươngOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Chapter 08 Electron Beams
Chapter 08 Electron Beams
Uploaded by
Đình Quý DươngCopyright:
Available Formats
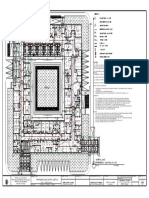
Chapter 8: Electron Beams: Physical
and Clinical Aspects
Set of 91 slides based on the chapter authored by
W. Strydom, W. Parker, and M. Olivares
of the IAEA publication (ISBN 92-0-107304-6):
Radiation Oncology Physics:
A Handbook for Teachers and Students
Objective:
To familiarize the student with the basic principles of radiotherapy
with megavoltage electron beams.
Slide set prepared in 2006
by E.B. Podgorsak (Montreal, McGill University)
Comments to S. Vatnitsky:
dosimetry@iaea.org
Version 2012
IAEA
International Atomic Energy Agency
CHAPTER 8.
8.1.
8.2.
8.3.
TABLE OF CONTENTS
Central axis depth dose distributions in water
Dosimetric parameters of electron beams
Clinical considerations in electron beam therapy
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1 Slide 1
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
Megavoltage electron beams represent an important
treatment modality in modern radiotherapy, often
providing a unique option in the treatment of superficial
tumours.
Electrons have been used in radiotherapy since the early
1950s.
Modern high-energy linacs typically provide, in addition to
two photon energies, several electron beam energies in
the range from 4 MeV to 25 MeV.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1 Slide 1
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.1 General shape of the depth dose curve
The general shape of the central axis depth dose curve
for electron beams differs from that of photon beams.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.1 Slide 1
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.1 General shape of the depth dose curve
Electron beam central axis percentage depth dose curve
exhibits the following characteristics:
Surface dose is relatively high
(of the order of 80 % 100 %).
Maximum dose occurs at a
certain depth referred to as the
depth of dose maximum zmax.
Beyond zmax the dose drops off
rapidly and levels off at a small
low level dose called the
bremsstrahlung tail (of the order
of a few per cent).
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.1 Slide 2
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.1 General shape of the depth dose curve
Electron beams are almost monoenergetic as they leave
the linac accelerating waveguide.
In moving toward the patient through:
Waveguide exit window
Scattering foils
Transmission ionization chamber
Air
and interacting with photon collimators, electron cones
(applicators) and the patient, bremsstrahlung radiation is
produced. This radiation constitutes the bremsstrahlung tail
of the electron beam PDD curve.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.1 Slide 3
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.2 Electron interactions with absorbing medium
As the electrons propagate through an absorbing medium,
they interact with atoms of the absorbing medium by a
variety of elastic or inelastic Coulomb force interactions.
These Coulomb interactions are classified as follows:
Inelastic collisions with orbital electrons of the absorber atoms.
Inelastic collisions with nuclei of the absorber atoms.
Elastic collisions with orbital electrons of the absorber atoms.
Elastic collisions with nuclei of the absorber atoms.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.2 Slide 1
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.2 Electron interactions with absorbing medium
Inelastic collisions between the incident electron and
orbital electrons of absorber atoms result in loss of incident
electrons kinetic energy through ionization and excitation
of absorber atoms (collision or ionization loss).
The absorber atoms can be ionized through two types of
ionization collision:
Hard collision in which the ejected orbital electron gains enough
energy to be able to ionize atoms on its own (these electrons are
called delta rays).
Soft collision in which the ejected orbital electron gains an
insufficient amount of energy to be able to ionize matter on its own.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.2 Slide 2
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.2 Electron interactions with absorbing medium
Elastic collisions between the incident electron and nuclei
of the absorber atoms result in:
Change in direction of motion of the incident electron (elastic
scattering).
A very small energy loss by the incident electron in individual
interaction, just sufficient to produce a deflection of electrons path.
The incident electron loses kinetic energy through a
cumulative action of multiple scattering events, each event
characterized by a small energy loss.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.2 Slide 3
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.2 Electron interactions with absorbing medium
Electrons traversing an absorber lose their kinetic energy
through ionization collisions and radiation collisions.
The rate of energy loss per gram and per cm2 is called the
mass stopping power and it is a sum of two components:
Mass collision stopping power
Mass radiation stopping power
The rate of energy loss for a therapy electron beam in
water and water-like tissues, averaged over the electrons
range, is about 2 MeV/cm.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.2 Slide 4
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.3 Inverse square law (virtual source position)
In contrast to a photon beam,
which has a distinct focus located
at the accelerator x ray target, an
electron beam appears to originate
from a point in space that does not
coincide with the scattering foil or
the accelerator exit window.
The term virtual source position
was introduced to indicate the
virtual location of the electron
source.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.3 Slide 1
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.3 Inverse square law (virtual source position)
Effective source-surface distance SSDeff is defined as the
distance from the virtual source position to the edge of the
electron cone applicator.
The inverse square law may be used for small SSD
differences from the nominal SSD to make corrections to
absorbed dose rate at zmax in the patient for variations in
air gaps g between the actual patient surface and the
nominal SSD.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.3 Slide 2
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.3 Inverse square law (virtual source position)
A common method for determining SSDeff consists of
measuring the dose rate at zmax in phantom for various air
gaps g starting with Dmax (g 0) at the electron cone.
The following inverse square law relationship holds:
Dmax (g 0) SSDeff zmax g
SSD
z
Dmax (g )
eff
max
The measured slope of the linear plot is:
1
SSDeff zmax
The effective SSD is then calculated from: SSDeff
IAEA
1
zmax
k
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.3 Slide 3
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.3 Inverse square law (virtual source position)
Typical example of data measured in determination of
virtual source position SSDeff normalized to the edge of the
electron applicator (cone).
SSDeff
IAEA
1
zmax
k
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.3 Slide 4
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.3 Inverse square law (virtual source position)
For practical reasons the nominal SSD is usually a fixed
distance (e.g., 5 cm) from the distal edge of the electron
cone (applicator) and coincides with the linac isocentre.
Although the effective SSD (i.e., the virtual electron source
position) is determined from measurements at zmax in a
phantom, its value does not change with change in the
depth of measurement.
The effective SSD depends on electron beam energy and
must be measured for all energies available in the clinic.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.3 Slide 5
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.4 Range concept
By virtue of being surrounded by a Coulomb force field,
charged particles, as they penetrate into an absorber
encounter numerous Coulomb interactions with orbital
electrons and nuclei of the absorber atoms.
Eventually, a charged particle will lose all of its kinetic
energy and come to rest at a certain depth in the
absorbing medium called the particle range.
Since the stopping of particles in an absorber is a
statistical process several definitions of the range are
possible.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.4 Slide 1
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.4 Range concept
Definitions of particle range: (1) CSDA range
In most encounters between the charged particle and absorber
atoms the energy loss by the charged particle is minute so that it
is convenient to think of the charged particle as losing its kinetic
energy gradually and continuously in a process referred to as the
continuous slowing down approximation (CSDA - Berger and
Seltzer).
The CSDA range or the mean path length of an electron of initial
kinetic energy E0 can be found by integrating the reciprocal of the
total mass stopping power over the energy from E0 to 0:
RCSDA
E0
IAEA
S (E )
dE
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.4 Slide 2
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.4 Range concept
CSDA ranges for electrons in air and water
Electron
energy
(MeV)
CSDA
range
in air
(g/cm2)
6
7
8
9
10
20
30
3.255
3.756
4.246
4.724
5.192
9.447
13.150
IAEA
CSDA
range
in water
(g/cm2)
3.052
3.545
4.030
4.506
4.975
9.320
13.170
The CSDA range is a calculated
quantity that represents the
mean path length along the
electrons trajectory.
The CSDA range is not the the
depth of penetration along a
defined direction.
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.4 Slide 3
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.4 Range concept
Several other range definitions are in use for electron beams:
Maximum range Rmax
Practical range Rp
Therapeutic range R90
Therapeutic range R80
Depth R50
Depth Rq
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.4 Slide 4
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.4 Range concept
Maximum range Rmax is defined
as the depth at which the
extrapolation of the tail of the
central axis depth dose curve
meets the bremsstrahlung
background.
Rmax is the largest penetration
depth of electrons in absorbing
medium.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.4 Slide 5
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.4 Range concept
Practical range Rp is defined
as the depth at which the
tangent plotted through the
steepest section of the
electron depth dose curve
intersects with the
extrapolation line of the
bremsstrahlung tail.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.4 Slide 6
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.4 Range concept
Depths R90, R80, and R50 are
defined as depths on the
electron PDD curve at which
the PDDs beyond the depth
of dose maximum zmax attain
values of 90 %, 80 %, and
50 %, respectively.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.4 Slide 7
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.4 Range concept
Depth Rq is defined
as the depth where
the tangent through
the dose inflection point
intersects the maximum
dose level.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.4 Slide 8
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.5 Buildup region
Buildup region for electron beams, like
for photon beams, is the depth region
between the phantom surface and the
depth of dose maximum zmax.
Surface dose for megavoltage electron
beams is relatively large (typically
between 75 % and 95 %) in contrast to
the surface dose for megavoltage photon
beams which is of the order of 10 % to
25 %.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.5 Slide 1
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.5 Buildup region
Unlike in photon beams, the
percentage surface dose in
electron beams increases
with increasing energy.
In contrast to photon beams,
zmax in electron beams does
not follow a specific trend
with electron beam energy;
it is a result of machine
design and accessories used.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.5 Slide 2
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.6 Dose distribution beyond zmax
Dose beyond zmax, especially at relatively low
megavoltage electron beam energies, drops off sharply as
a result of the scattering and continuous energy loss by
the incident electrons.
As a result of bremsstrahlung energy loss by the incident
electrons in the head of the linac, air and the patient, the
depth dose curve beyond the range of electrons is
attributed to the bremsstrahlung photons.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.6 Slide 1
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.6 Dose distribution beyond zmax
Bremsstrahlung contamination of electron beams depends
on electron beam energy and is typically:
Less than 1 % for
4 MeV electron beams.
Less than 2.5 % for
10 MeV electron beams.
Less than 4 % for
20 MeV electron beams.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.6 Slide 2
8.1 CENTRAL AXIS DEPTH DOSE DISTRIBUTIONS
8.1.6 Dose distribution beyond zmax
Electron dose gradient G
is defined as follows:
G
Rp
Rp Rq
Dose gradient G for lower
electron beam energies is
steeper than that for higher
electron energies.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.1.6 Slide 3
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.1 Electron beam energy specification
Spectrum of the electron beam is very complex and is
influenced by the medium the beam traverses.
Just before exiting the waveguide through the beryllium exit
window the electron beam is almost monoenergetic.
The electron energy is degraded randomly when electrons pass
through the exit window, scattering foil, transmission ionization
chamber and air. This results in a relatively broad spectrum of
electron energies on the patient surface.
As the electrons penetrate into tissue, their spectrum is
broadened and degraded further in energy.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.1 Slide 1
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.1 Electron beam energy specification
Spectrum of the electron beam depends on the point of
measurement in the beam.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.1 Slide 2
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.1 Electron beam energy specification
Several parameters are used for describing the beam
quality of an electron beam:
Most probable energy EKp (0) of the electron beam on phantom
surface.
Mean energy EK (0) of the electron beam on the phantom surface.
Half-value depth R50 on the percentage depth dose curve of the
electron beam.
Practical range Rp of the electron beam.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.1 Slide 3
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.1 Electron beam energy specification
The most probable energy EKp (0) on the phantom surface
is defined by the position of the spectral peak.
EKp (0) is related to the practical range Rp (in cm) of the
electron beam through the following polynomial equation:
EKp (0) C1 C2Rp C3Rp2
For water: C1 0.22 MeV
C 2 1.98 MeV/cm
C3 0.0025 MeV/cm2
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.1 Slide 4
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.1 Electron beam energy specification
The mean electron energy EK (0) of the electron beam on
the phantom surface is slightly smaller than the most
probable energy EKp (0) on the phantom surface as a result
of an asymmetrical shape of the electron spectrum.
The mean electron energy EK (0) is
related to the half-value depth R50 as:
EK (0) CR50
The constant C for water is 2.33 MeV/cm.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.1 Slide 5
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.1 Electron beam energy specification
Harder has shown that the most probable energy EKp (z)
and the mean energy E(z) of the electron beam at a
depth z in the phantom or patient decrease linearly with z.
Harders relationships are expressed as follows:
z
E ( z ) E (0) 1
Rp
p
K
Note:
IAEA
p
K
and
z
E ( z ) E (0) 1
Rp
EKp (z 0) EKp (0)
E(z 0) E(0)
EKp (z Rp ) 0
E(z Rp ) 0
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.1 Slide 6
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.2 Typical depth dose parameters as a function of energy
Typical electron beam depth dose parameters that should
be measured for each clinical electron beam
Energy
(MeV)
R90
(cm)
R80
(cm)
R50
(cm)
Rp
(cm)
E(0)
(MeV)
Surface
dose %
1.7
1.8
2.2
2.9
5.6
81
2.4
2.6
3.0
4.0
7.2
83
10
3.1
3.3
3.9
4.8
9.2
86
12
3.7
4.1
4.8
6.0
11.3
90
15
4.7
5.2
6.1
7.5
14.0
92
18
5.5
5.9
7.3
9.1
17.4
96
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.2 Slide 1
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.3 Percentage depth dose
Similarly to PDDs for photon beams, the PDDs for
electron beams, at a given source-surface distance SSD,
depend upon:
Depth z in phantom (patient).
Electron beam kinetic energy
EK(0) on phantom surface.
Field size A on phantom
surface.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.3 Slide 1
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.3 Percentage depth dose
PDDs of electron beams are measured with:
Cylindrical, small-volume ionization chamber in water phantom.
Diode detector in water phantom.
Parallel-plate ionization chamber in water phantom.
Radiographic or radiochromic film in solid water phantom.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.3 Slide 2
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.3 Percentage depth dose
Measurement of electron beam PDDs:
If ionization chamber is used, the measured depth ionization
distribution must be converted into a depth dose distribution by
using the appropriate stopping power ratios, water to air, at depths
in phantom.
If diode is used, the diode ionization signal represents the dose
directly, because the stopping power ratio, water to silicon, is
essentially independent of electron energy and hence depth.
If film is used, the characteristic curve (H and D curve) for the
given film should be used to determine the dose against the film
density.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.3 Slide 3
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.3 Percentage depth dose
Dependence of PDDs on electron beam field size.
For relatively large field sizes the PDD distribution at a
given electron beam energy is essentially independent of
field size.
When the side of the electron field is smaller than the
practical range Rp, lateral electronic equilibrium will not
exist on the beam central axis and both the PDDs as well
as the output factors exhibit a significant dependence on
field size.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.3 Slide 4
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.3 Percentage depth dose
PDDs for small electron fields
For a decreasing field size,
when the side of the field
decreases to below the Rp
value for a given electron
energy:
Depth dose maximum
decreases.
Surface dose increases.
Rp remains essentially
constant, except when the field
size becomes very small.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.3 Slide 5
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.3 Percentage depth dose
PDDs for oblique incidence.
Angle of obliquity is defined as the angle between the
electron beam central axis and the normal to the
phantom or patient surface. Angle 0 corresponds to
normal beam incidence.
For oblique beam incidences, especially at large angles
the PDD characteristics of electron beams deviate
significantly from those for normal beam incidence.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.3 Slide 6
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.3 Percentage depth dose
Percentage depth dose for oblique beam incidence
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.3 Slide 7
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.3 Percentage depth dose
Depth dose for oblique beam incidence
Obliquity effect becomes significant for angles of
incidence exceeding 45o.
Obliquity factor OF( ,z) accounts for the change in depth
dose at a given depth z in phantom and is normalized to
0
1.00 at zmax at normal incidence
.
Obliquity factor at zmax is larger than 1 (see insets on
previous slide).
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.3 Slide 8
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.4 Output factors
The output factor for a given electron energy and field
size (delineated by applicator or cone) is defined as the
ratio of the dose for the specific field size (applicator) to
the dose for a 1010 cm2 reference field size
(applicator), both measured at depth zmax on the beam
central axis in phantom at a nominal SSD of 100 cm.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.4 Slide 1
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.4 Output factors
When using electron beams
from a linac, the photon
collimator must be opened to
the appropriate setting for a
given electron applicator.
Typical electron applicator
sizes at nominal SSD are:
Circular with diameter: 5 cm
Square: 10x10 cm2; 1515 cm2;
2020 cm2; and 2525 cm2.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.4 Slide 2
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.4 Output factors
Often collimating blocks made of lead or a low melting
point alloy (e.g., Cerrobend) are used for field shaping.
These blocks are attached to the end of the electron cone
(applicator) and produce the required irregular field.
Output factors, normalized to the standard 1010 cm2
electron cone, must be measured for all custom-made
irregular fields.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.4 Slide 3
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.4 Output factors
For small irregular field sizes the extra shielding affects
not only the output factors but also the PDD distribution
because of the lack of lateral scatter.
For custom-made small fields, in addition to output
factors, the full electron beam PDD distribution should be
measured.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.4 Slide 4
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.5 Therapeutic range
Depth of the 90 % dose level on the beam central axis
(R90) beyond zmax is defined as the therapeutic range for
electron beam therapy.
R90 is approximately equal to EK/4 in cm of water, where
EK is the nominal kinetic energy in MeV of the electron
beam.
R80, the depth that corresponds to the 80 % PDD beyond
zmax, may also be used as the therapeutic range and is
approximated by EK/3 in cm of water.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.5 Slide 1
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.6 Profiles and off-axis ratio
A dose profile represents a
plot of dose at a given
depth in phantom against
the distance from the
beam central axis.
Profile is measured in a
plane perpendicular to the
beam central axis at a
given depth z in phantom.
Dose profile measured at a depth
of dose maximum zmax in water for
a 12 MeV electron beam and
2525 cm2 applicator cone.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.6 Slide 1
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.6 Profiles and off-axis ratio
Two different normalizations are used for beam profiles:
The profile data for a given depth in phantom may be normalized
to the dose at zmax on the central axis (point P). The dose value
on the beam central axis for z zmax then represents the central
axis PDD value.
The profile data for a given depth in phantom may also be
normalized to the value on the beam central axis (point Q). The
values off the central axis for z zmax are then referred to as the
off-axis ratios (OARs).
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.6 Slide 2
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.7 Flatness and symmetry
According to the International
Electrotechnical Commission (IEC)
the specification for beam flatness of
electron beams is given for zmax
under two conditions:
Distance between the 90 % dose
level and the geometrical beam
edge should not exceed 10 mm
along major field axes and 20 mm
along diagonals.
Maximum value of the absorbed
dose anywhere within the region
bounded by the 90 % isodose
contour should not exceed 1.05
times the absorbed dose on the
axis of the beam at the same depth.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.7 Slide 1
8.2 DOSIMETRIC PARAMETERS OF ELECTRON BEAMS
8.2.7 Flatness and symmetry
According to the International Electrotechnical Commission (IEC)
the specification for symmetry of electron beams requires that the
cross-beam profile measured at depth zmax should not differ by
more than 3 % for any pair of symmetric points with respect to the
central ray.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.2.7 Slide 2
8.3 CLINICAL CONSIDERATIONS
8.3.1 Dose specification and reporting
Electron beam therapy is usually applied in treatment of
superficial or subcutaneous disease.
Treatment is usually delivered with a single direct electron
field at a nominal SSD of 100 cm.
The dose is usually prescribed at a depth that lies at, or
beyond, the distal margin of the target.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.1 Slide 1
8.3 CLINICAL CONSIDERATIONS
8.3.1 Dose specification and reporting
To maximize healthy tissue sparing beyond the tumour
and to provide relatively homogeneous target coverage
treatments are usually prescribed at zmax, R90, or R80.
If the treatment dose is specified at R80 or R90, the skin
dose may exceed the prescription dose.
Since the maximum dose in the target may exceed the
prescribed dose by up to 20 %, the maximum dose should
be reported for all electron beam treatments.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.1 Slide 2
8.3 CLINICAL CONSIDERATIONS
8.3.2 Small field sizes
The PDD curves for electron beams do not depend on field
size, except for small fields where the side of the field is
smaller than the practical range of the electron beam.
When lateral scatter equilibrium
is not reached at small electron
fields:
Dose rate at zmax decreases
Depth of maximum dose, zmax,
moves closer to the surface
PDD curve becomes less steep,
in comparison to a 1010 cm2
field.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.2 Slide 1
8.3 CLINICAL CONSIDERATIONS
8.3.3 Isodose distributions
Isodose curves are lines
connecting points of equal
dose in the irradiated
medium.
Isodose curves are usually
drawn at regular intervals
of absorbed dose and are
expressed as a percentage
of the dose at a reference
point, which is usually
taken as the zmax point on
the beam central axis.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.3 Slide 1
8.3 CLINICAL CONSIDERATIONS
8.3.3 Isodose distributions
As electron beam penetrates a
medium (absorber), the beam
expands rapidly below the
surface because of electron
scattering on absorber atoms.
The spread of the isodose
curves varies depending on:
IAEA
Isodose level.
Energy of the beam.
Field size.
Beam collimation.
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.3 Slide 2
8.3 CLINICAL CONSIDERATIONS
8.3.3 Isodose distributions
A particular characteristic of
electron beam isodose curves
is the bulging out of the low
value isodose curves (<20 %)
as a direct result of the
increase in electron scattering
angle with decreasing electron
energy.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.3 Slide 3
8.3 CLINICAL CONSIDERATIONS
8.3.3 Isodose distributions
At energies above 15 MeV
electron beams exhibit a lateral
constriction of the higher value
isodose curves (>80 %). The
higher is the electron beam
energy, the more pronounced
is the effect.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.3 Slide 4
8.3 CLINICAL CONSIDERATIONS
8.3.3 Isodose distributions
The term penumbra generally defines the region at the
edge of the radiation beam over which the dose rate
changes rapidly as a function of distance from the beam
central axis.
The physical penumbra of an electron beam may be
defined as the distance between two specified isodose
curves at a specified depth in phantom.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.3 Slide 5
8.3 CLINICAL CONSIDERATIONS
8.3.3 Isodose distributions
In determination of the
physical penumbra of an
electron beam the ICRU
recommends that:
The 80 % and 20 % isodose
curves be used.
The specified depth of
measurement be R85/2, where
R85 is the depth of the 85 %
dose level beyond zmax on the
electron beam central ray.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.3 Slide 6
8.3 CLINICAL CONSIDERATIONS
8.3.3 Isodose distributions
In electron beam therapy, the air gap is defined as the
separation between the patient and the end of the
applicator cone. The standard air gap is 5 cm.
With increasing air gap:
Low value isodose curves diverge.
High value isodose curves converge toward the central axis of the
beam.
Physical penumbra increases.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.3 Slide 7
8.3 CLINICAL CONSIDERATIONS
8.3.4 Field shaping
To achieve a more customized electron field shape, a lead
or metal alloy cut-out may be constructed and placed on
the applicator as close to the patient as possible.
Field shapes may be determined from conventional or
virtual simulation, but are most often prescribed clinically
by a physician prior to the first treatment.
As a rule of thumb, divide the practical range Rp by 10 to
obtain the approximate thickness of lead required for
shielding (<5 %).
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.4 Slide 1
8.3 CLINICAL CONSIDERATIONS
8.3.4 Field shaping
For certain treatments, such as treatments of the lip,
buccal mucosa, eyelids or ear lobes, it may be
advantageous to use an internal shield to protect the
normal structures beyond the target volume.
Internal shields are usually coated with low atomic number
materials to minimize the electron backscattering into
healthy tissue above the shield.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.4 Slide 2
8.3 CLINICAL CONSIDERATIONS
8.3.4 Field shaping
Extended SSDs have various effects on electron beam
parameters and are generally not advisable.
In comparison with treatment at nominal SSD of 100 cm at
extended SSD:
Output is significantly lower
Beam penumbra is larger
PDD distribution changes minimally.
An effective SSD based on the virtual source position is
used when applying the inverse square law to correct the
beam output at zmax for extended SSD.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.4 Slide 3
8.3 CLINICAL CONSIDERATIONS
8.3.5 Irregular surface correction
Uneven air gaps as a result of curved patient surfaces are
often present in clinical use of electron beam therapy.
Inverse square law corrections can be made to the dose
distribution to account for the sloping surface.
D(SSDeff g, z )
SSDeff z
Do (SSDeff , z )
SSD
z
)
eff
From F.M. Khan:
The Physics of
Radiation Therapy
IAEA
g = air gap
z = depth below surface
SSDeff = distance between the
virtual source and surface
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.5 Slide 1
8.3 CLINICAL CONSIDERATIONS
8.3.5 Irregular surface correction
Inverse square correction alone does not account for
changes in side scatter as a result of beam obliquity which:
Increases side scatter at the depth of maximum dose, zmax
Shifts zmax toward the surface
Decreases the therapeutic depths R90 and R80.
D(SSDeff g, z )
2
SSDeff z
Do (SSDeff , z )
OF( , z )
SSDeff g z )
From F.M. Khan:
The Physics of
Radiation Therapy
IAEA
OF(z, ) = obliquity factor which
accounts for the change in depth
dose at a point in phantom at depth z
for a given angle of obliquity but
same SSDeff as for 0
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.5 Slide 2
8.3 CLINICAL CONSIDERATIONS
8.3.6 Bolus
Bolus made of tissue equivalent material, such as wax, is
often used in electron beam therapy:
To increase the surface dose.
To shorten the range of a given electron beam in the patient.
To flatten out irregular surfaces.
To reduce the electron beam penetration in some parts of the
treatment field.
Although labour intensive, the use of bolus in electron
beam therapy is very practical, since treatment planning
software for electron beams is limited and empirical data
are normally collected only for standard beam geometries.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.6 Slide 1
8.3 CLINICAL CONSIDERATIONS
8.3.6 Bolus
The use of computed tomography (CT) for treatment
planning enables accurate determination of tumour shape
and patient contour.
If a wax bolus is constructed such that the total distance
from the bolus surface to the required treatment depth is
constant along the length of
the tumour, then the shape
of the resulting isodose
curves will approximate
the shape of the tumour
as determined with
CT scanning.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.6 Slide 2
8.3 CLINICAL CONSIDERATIONS
8.3.7 Inhomogeneity corrections
The dose distribution from an electron beam can be
greatly affected by the presence of tissue inhomogeneities
(heterogeneities) such as lung or bone.
The dose inside an inhomogeneity is difficult to calculate
or measure, but the effect of an inhomogeneity on the
dose beyond the inhomogeneity is relatively simple to
measure and quantify.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.7 Slide 1
8.3 CLINICAL CONSIDERATIONS
8.3.7 Inhomogeneity corrections
The simplest correction for a tissue inhomogeneity
involves the scaling of the inhomogeneity thickness by
its electron density relative to that of water and the
determination of the coefficient of equivalent thickness
(CET).
Electron density of an inhomogeneity is essentially
equivalent to the mass density of the inhomogeneity.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.7 Slide 2
8.3 CLINICAL CONSIDERATIONS
8.3.7 Inhomogeneity corrections
CET is used to determine the effective depth in water
equivalent tissue zeff through the following expression:
zeff z t(1 CET)
z = actual depth of the point of interest
in the patient
t = thickness of the inhomogeneity
For example:
Lung has approximate density of 0.25 g/cm3 and a CET of 0.25.
A thickness of 1 cm of lung is equivalent to 0.25 cm of tissue.
Solid bone has approximate density of 1.6 g/cm3 and a CET of 1.6.
A thickness of 1 cm of bone is equivalent to 1.6 cm of tissue.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.7 Slide 3
8.3 CLINICAL CONSIDERATIONS
8.3.7 Inhomogeneity corrections
Effect of lung inhomogeneity on the PDD distribution of an
electron beam (energy: 15 MeV, field: 1010 cm2).
Thickness t of lung
inhomogeneity: 6 cm
Tissue equivalent thickness:
zeff = 1.5 cm
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.7 Slide 4
8.3 CLINICAL CONSIDERATIONS
8.3.7 Inhomogeneity corrections
If an electron beam strikes the interface between two
materials either tangentially or at a large oblique angle, the
resulting scatter perturbation will affect the dose
distribution at the interface.
Lower density material will receive a higher dose, due to
the increased scattering of electrons from the higher
density side.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.7 Slide 5
8.3 CLINICAL CONSIDERATIONS
8.3.7 Inhomogeneity corrections
Edge effects need to be considered in the following
situations:
Inside a patient, at the interfaces between internal structures of
different density.
On the surface of a patient, in regions of sharp surface irregularity.
On the interface between lead shielding and the surface of the
patient, if the shielding is placed superficially on the patient or if it is
internal shielding.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.7 Slide 6
8.3 CLINICAL CONSIDERATIONS
8.3.8 Electron beam combinations
Occasionally, the need arises to abut electron fields. When
abutting two electron fields, it is important to take into
consideration the dosimetric characteristics of electron
beams at depth in the patient.
The large penumbra and bulging isodose lines produce hot
spots and cold spots inside the target volume.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.8 Slide 1
8.3 CLINICAL CONSIDERATIONS
8.3.8 Electron beam combinations
In general, it is best to avoid using adjacent electron fields.
If the use of abutting fields is absolutely necessary, the
following conditions apply:
Contiguous electron beams should be parallel to one another in
order to avoid significant overlapping of the high value isodose
curves at depth in the patient.
Some basic film dosimetry should be carried out at the junction of
the fields to ensure that no significant hot or cold spots in dose
occur.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.8 Slide 2
8.3 CLINICAL CONSIDERATIONS
8.3.8 Electron beam combinations
Electron - photon field matching is easier than electron electron field matching.
A distribution for photon fields is readily available from a
treatment planning system (TPS) and the location of the
electron beam treatment field as well as the associated hot
and cold spots can be determined relative to the photon
field treatment plan.
Matching of electron and photon fields on the skin will
produce a hot spot on the photon side of the treatment.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.8 Slide 3
8.3 CLINICAL CONSIDERATIONS
8.3.9 Electron arc therapy
Electron arc therapy is a special radiotherapeutic
treatment technique in which a rotational electron beam
is used to treat superficial tumour volumes that follow
curved surfaces.
While its usefulness in treatment of certain large
superficial tumours is well recognized, the technique is
not widely used because it is relatively complicated and
cumbersome, and its physical characteristics are poorly
understood.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.9 Slide 1
8.3 CLINICAL CONSIDERATIONS
8.3.9 Electron arc therapy
The dose distribution in the target volume for electron
arc therapy depends in a complicated fashion on:
Electron beam energy
Field width w
Depth of the isocentre di
Source-axis distance f
Patient curvature
Tertiary collimation
Field shape as defined by the secondary collimator
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.9 Slide 2
8.3 CLINICAL CONSIDERATIONS
8.3.9 Electron arc therapy
Two approaches to electron arc therapy have been
developed:
Electron pseudo-arc based on a series of overlapping stationary
electron fields.
Continuous electron arc using a continuous rotating electron beam.
Calculation of dose distributions in electron arc therapy is a
complicated procedure that generally cannot be performed
reliably with the algorithms used for standard electron beam
treatment planning.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.9 Slide 3
8.3 CLINICAL CONSIDERATIONS
8.3.9 Electron arc therapy
Characteristic angle concept represents a semiempirical technique for treatment planning in electron
arc therapy.
Characteristic angle for an
arbitrary point A on the patient
surface is measured between
the central axes of two rotational
electron beams positioned in
such a way that at point A the
frontal edge of one beam
crosses the trailing edge of the
other beam.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.9 Slide 4
8.3 CLINICAL CONSIDERATIONS
8.3.9 Electron arc therapy
Characteristic angle represents a continuous rotation
in which a surface point A receives a contribution from all ray
lines of the electron beam starting with the frontal edge and
finishing with the trailing edge of the rotating electron beam.
w is the nominal field size.
f is the virtual source isocentre distance.
di is the isocentre depth.
IAEA
2di sin
di
1 cos
f
2
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.9 Slide 5
8.3 CLINICAL CONSIDERATIONS
8.3.9 Electron arc therapy
Characteristic angle is uniquely determined by three
treatment parameters
Source-axis distance f
Depth of isocentre di
Field width w
2di sin
1
di
cos
f
2
Electron beams with combinations of di and w that give
the same characteristic angle exhibit very similar radial
percentage depth dose distributions even though they
may differ considerably in individual di and w.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.9 Slide 6
8.3 CLINICAL CONSIDERATIONS
8.3.9 Electron arc therapy
PDDs for rotational electron
beams depend only on:
Electron beam energy.
Characteristic angle .
When a certain PDD is required
for patient treatment one may
choose a that will give the
required beam characteristics.
Since di is fixed by the patient
contour, the required is
obtained by choosing the
appropriate w.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.9 Slide 7
8.3 CLINICAL CONSIDERATIONS
8.3.9 Electron arc therapy
Photon contamination of the electron beam is of concern
in electron arc therapy, since the photon contribution from
all beams is added at the isocentre and the isocentre may
be at a critical structure.
Comparison between two dose distributions
measured with film in a humanoid phantom:
(a) Small of 10o (small field width) exhibiting
a large photon contamination at the isocentre
(b) Large of 100o exhibiting a relatively small
photon contamination at the isocentre.
In electron arc therapy the bremsstrahlung dose
at the isocentre is inversely proportional to the
characteristic angle .
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.9 Slide 8
8.3 CLINICAL CONSIDERATIONS
8.3.9 Electron arc therapy
Shape of secondary collimator defining the field width w in
electron arc therapy is usually rectangular and the resulting
treatment volume geometry is cylindrical, such as foe
example in the treatment of the chest wall.
When sites that can only be approximated with spherical
geometry, such as lesions of the scalp, a custom built
secondary collimator defining a non-rectangular field of
appropriate shape must be used to provide a homogeneous
dose in the target volume.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.9 Slide 9
8.3 CLINICAL CONSIDERATIONS
8.3.10 Electron therapy treatment planning
Complexity of electron-tissue interactions makes treatment planning for electron beam therapy difficult and
look up table type algorithms do not predict well the
dose distribution for oblique incidence and tissue
inhomogeneities.
Early methods in electron beam treatment planning were
empirical and based on water phantom measurements
of PDDs and beam profiles for various field sizes,
similarly to the Milan-Bentley method developed for use
in photon beams.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.10 Slide 1
8.3 CLINICAL CONSIDERATIONS
8.3.10 Electron therapy treatment planning
Early methods in electron treatment planning accounted
for tissue inhomogeneities by scaling the percentage
depth doses using the CET approximation which provides
useful parameterization of the electron depth dose curve
but has nothing to do with the physics of electron
transport.
Fermi-Eyges multiple scattering theory considers a broad
electron beam as being made up of many individual pencil
beams that spread out laterally in tissue following a
Gaussian function.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.10 Slide 2
8.3 CLINICAL CONSIDERATIONS
8.3.10 Electron therapy treatment planning
Pencil beam algorithm can account for tissue inhomogeneity,
patient curvature and irregular field shape.
Rudimentary pencil beam algorithms deal with lateral
dispersion but ignore angular dispersion and backscattering
from tissue interfaces.
Despite applying both the stopping powers and scattering
powers, the modern refined pencil beam, multiple scattering
algorithms generally fail to provide accurate dose
distributions for most general clinical conditions.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.10 Slide 3
8.3 CLINICAL CONSIDERATIONS
8.3.10 Electron therapy treatment planning
The most accurate and reliable way to calculate electron
beam dose distributions is through Monte Carlo techniques.
The main drawback of the current Monte Carlo approach to
treatment planning is the relatively long computation time.
With increased computing speed and decreasing hardware
cost, it is expected that Monte Carlo based electron dose
calculation algorithms will soon become available for
routine electron beam treatment planning.
IAEA
Radiation Oncology Physics: A Handbook for Teachers and Students - 8.3.10 Slide 5
You might also like
- Government Surveillance Thesis StatementDocument7 pagesGovernment Surveillance Thesis Statementashleygomezalbuquerque100% (1)
- TR 35 A Proposed Training Model For The Microbiological Function in The Pharmaceutical Industry 2001Document32 pagesTR 35 A Proposed Training Model For The Microbiological Function in The Pharmaceutical Industry 2001Sheetal Agree100% (2)
- Bizzle Tips For IMRT PlanningDocument1 pageBizzle Tips For IMRT Planningcnsouza2000No ratings yet
- Canadian Med Phys ExamDocument85 pagesCanadian Med Phys ExamKurt Van DelinderNo ratings yet
- Developing With Magnolia CmsDocument14 pagesDeveloping With Magnolia CmsĐình Quý DươngNo ratings yet
- Chey Khana Research by Arif HussainDocument17 pagesChey Khana Research by Arif HussainArif KhanNo ratings yet
- Lecture 7 Chapter 06 Photon BeamsDocument87 pagesLecture 7 Chapter 06 Photon BeamsggggNo ratings yet
- Chapter 09 Calibration of Radiotherapy Beams PDFDocument95 pagesChapter 09 Calibration of Radiotherapy Beams PDFabdul rafiNo ratings yet
- Chapter 07 Treatment PlanningDocument232 pagesChapter 07 Treatment PlanningAhmed Ridwan Oladotun100% (1)
- Chapter 03 Radiation Dosimeters PDFDocument113 pagesChapter 03 Radiation Dosimeters PDFJose Ivan MejiaNo ratings yet
- Radiobiology Iaea DiapositivasDocument88 pagesRadiobiology Iaea DiapositivasLida Velasquez SierraNo ratings yet
- Calibration of Dosimeters Used in Radiation TherapyDocument122 pagesCalibration of Dosimeters Used in Radiation TherapySOHON SINHA MAHAPATRANo ratings yet
- Physics of Nuclear MedicineDocument101 pagesPhysics of Nuclear Medicinedrqazi777No ratings yet
- Chapter 02 Dosimetric PrinciplesDocument131 pagesChapter 02 Dosimetric PrinciplesLida Velasquez SierraNo ratings yet
- 01 Materi 1Document98 pages01 Materi 1levina almiraNo ratings yet
- Slide Set of 195 Slides Based On The Chapter Authored by E.B. Podgorsak of The IAEA Publication (ISBN 92-0-107304-6)Document195 pagesSlide Set of 195 Slides Based On The Chapter Authored by E.B. Podgorsak of The IAEA Publication (ISBN 92-0-107304-6)SaRaNo ratings yet
- Radiation Therapy Dosimetry - A Practical HandbookDocument505 pagesRadiation Therapy Dosimetry - A Practical Handbooknewhopeclub03reeceNo ratings yet
- Practical Approach To Electron Beam Dosimetry at Extended SSDDocument10 pagesPractical Approach To Electron Beam Dosimetry at Extended SSDAhmet Kürşat ÖzkanNo ratings yet
- Chapter 06 Photon BeamsDocument170 pagesChapter 06 Photon Beamsmitza05No ratings yet
- Part 3 Week 9 - IMRT - VMATDocument38 pagesPart 3 Week 9 - IMRT - VMATdanNo ratings yet
- Controversies in Medical PhysicsDocument560 pagesControversies in Medical PhysicsDeybith Venegas100% (1)
- Raphex Answers 2010Document15 pagesRaphex Answers 2010Ant MenNo ratings yet
- Icrp 60Document211 pagesIcrp 60JithinNo ratings yet
- Therapy Physics Review Course - Radiation GeneratorsDocument31 pagesTherapy Physics Review Course - Radiation Generatorszazoo17No ratings yet
- EANM 2017 TEchGuide QualityControlDocument168 pagesEANM 2017 TEchGuide QualityControlnapoleonNo ratings yet
- Chapter 16 Radiation Protection and Safety PDFDocument236 pagesChapter 16 Radiation Protection and Safety PDFAshutosh SinghNo ratings yet
- Dose CalculationDocument5 pagesDose CalculationAbdul Al-FattahNo ratings yet
- Aapm Report No. 16 Protocol For HeavyDocument60 pagesAapm Report No. 16 Protocol For HeavyLaurentiu Radoi100% (1)
- Chapter 13 Brachytherapy PDFDocument163 pagesChapter 13 Brachytherapy PDFJorge CifuentesNo ratings yet
- WEBB - The Physics of Three-Dimensional Radiation TherapyDocument368 pagesWEBB - The Physics of Three-Dimensional Radiation TherapyMiguelNo ratings yet
- Radiation Safety in BrachytherapyDocument26 pagesRadiation Safety in Brachytherapykarthickmech1987No ratings yet
- On-Board Imaging System - Board Imaging System HammoudQADocument120 pagesOn-Board Imaging System - Board Imaging System HammoudQAyumekiNo ratings yet
- Characteristics and Limitations of A Secondary Dose Check Software For VMAT Plan CalculationDocument8 pagesCharacteristics and Limitations of A Secondary Dose Check Software For VMAT Plan Calculationkaren CarrilloNo ratings yet
- Estro - Practical Guide in Brachytherapy Qa PDFDocument270 pagesEstro - Practical Guide in Brachytherapy Qa PDFanamariatornero50% (2)
- Calibration of Ionisation ChamberDocument76 pagesCalibration of Ionisation ChamberArmin DurakovićNo ratings yet
- Calculation of Air-Kerma Strength and Dose Rate Constant For New BEBIG 60co HDR Brachytherapy Source An EGSnrc Monte Carlo StudyDocument28 pagesCalculation of Air-Kerma Strength and Dose Rate Constant For New BEBIG 60co HDR Brachytherapy Source An EGSnrc Monte Carlo Studyanwar01726100% (1)
- Monaco 5.11.02 Training GuideDocument1,294 pagesMonaco 5.11.02 Training GuidereginafalancaNo ratings yet
- Aapm Mu CalculationDocument34 pagesAapm Mu CalculationemirNo ratings yet
- Quality Assurance of External Beam RadiotherapyDocument73 pagesQuality Assurance of External Beam RadiotherapybeenoegrahaNo ratings yet
- Class PDD TPR BSFDocument48 pagesClass PDD TPR BSFFrancisco HernandezNo ratings yet
- Orthovoltage Vs MegavoltageDocument7 pagesOrthovoltage Vs MegavoltageEmmanuel Cuevas MisNo ratings yet
- CT SimulatorDocument7 pagesCT SimulatorRaras HanifatunnisaNo ratings yet
- Chapter 10 Acceptance Testing and CommissioningDocument189 pagesChapter 10 Acceptance Testing and CommissioningKurt Van DelinderNo ratings yet
- Independent Dose Calculations Concepts and ModelsDocument104 pagesIndependent Dose Calculations Concepts and ModelsMuhammad Nauman UsmaniNo ratings yet
- Purdue University General-Medical-Physics-Core-CoursesDocument2 pagesPurdue University General-Medical-Physics-Core-Courseskirim mammoNo ratings yet
- Medical Physics ResourcesDocument10 pagesMedical Physics ResourceschanderNo ratings yet
- Iaea TRS 469 PDFDocument86 pagesIaea TRS 469 PDFClaudia Morales UlloaNo ratings yet
- BrachytherapyDocument5 pagesBrachytherapyChiara Tenorio Ü100% (1)
- Handbook of Radiotherapy Physics - RosenwaldDocument1,425 pagesHandbook of Radiotherapy Physics - RosenwaldDeize GrodniskiNo ratings yet
- Notes - Radioactivity and Nuclear EnergyDocument28 pagesNotes - Radioactivity and Nuclear EnergyUlwindass Victor Gorge100% (1)
- Radiation Targets 1: DNA, Chromosome and Chromatid Damage and RepairDocument71 pagesRadiation Targets 1: DNA, Chromosome and Chromatid Damage and RepairmarrajoanaNo ratings yet
- Icrp 60Document25 pagesIcrp 60Muhammad NaveedNo ratings yet
- Cell Survival Curve 2Document16 pagesCell Survival Curve 2Ahmed Ridwan OladotunNo ratings yet
- Csi Plan Writeup Portion Turn in PDFDocument13 pagesCsi Plan Writeup Portion Turn in PDFapi-481226212No ratings yet
- Automatic Treatment Planning For VMAT-based TotalDocument12 pagesAutomatic Treatment Planning For VMAT-based TotalAmra IbrahimovicNo ratings yet
- IMRT Part 1 BJRDocument9 pagesIMRT Part 1 BJRsusdoctorNo ratings yet
- Haris Linear AcceleratorDocument66 pagesHaris Linear AcceleratorHarisrahmanNo ratings yet
- Chapter 01 Basics Radiation PhysicsDocument195 pagesChapter 01 Basics Radiation PhysicsJose Ivan MejiaNo ratings yet
- Qa PhysicsDocument4 pagesQa PhysicstuNo ratings yet
- CRHPDocument4,229 pagesCRHPbcurrier10100% (1)
- Radiation Safety of Accelerator Based Radioisotope Production Facilities: Specific Safety GuideFrom EverandRadiation Safety of Accelerator Based Radioisotope Production Facilities: Specific Safety GuideNo ratings yet
- Comprehensive Audits of Radiotherapy Practices: A Tool for Quality ImprovementFrom EverandComprehensive Audits of Radiotherapy Practices: A Tool for Quality ImprovementNo ratings yet
- Non-ionizing Radiation Protection: Summary of Research and Policy OptionsFrom EverandNon-ionizing Radiation Protection: Summary of Research and Policy OptionsNo ratings yet
- CoC-Khí Nitro Hydro HeliDocument3 pagesCoC-Khí Nitro Hydro HeliĐình Quý DươngNo ratings yet
- Radiations MacLaurin DeadtimeDocument3 pagesRadiations MacLaurin DeadtimeĐình Quý DươngNo ratings yet
- The Geiger CounterDocument44 pagesThe Geiger CounterĐình Quý DươngNo ratings yet
- Bai Tap Giai Tich Tap 3 - Tran Duc LongDocument94 pagesBai Tap Giai Tich Tap 3 - Tran Duc LongĐình Quý Dương100% (3)
- Gamma Spectrum: U (V) N (Counts/30s)Document4 pagesGamma Spectrum: U (V) N (Counts/30s)Đình Quý DươngNo ratings yet
- Scalp PDFDocument7 pagesScalp PDFduranduran11No ratings yet
- Eating DisorderDocument65 pagesEating DisorderVanessa MartinNo ratings yet
- Christian Aid (2005) Unearthing The Truth, Mining in Peru. A Christian Aid ReportDocument50 pagesChristian Aid (2005) Unearthing The Truth, Mining in Peru. A Christian Aid ReportcqnvalNo ratings yet
- Health9 q2 Mod1of2 Drug Scenario in The Philippines v2Document19 pagesHealth9 q2 Mod1of2 Drug Scenario in The Philippines v2yhannaNo ratings yet
- Key Counselling Skills: ExplainedDocument5 pagesKey Counselling Skills: Explainedpaulino MalakasNo ratings yet
- ÔN TẬP GK 1. ANH 11Document4 pagesÔN TẬP GK 1. ANH 11hanguyen3288hhtNo ratings yet
- Pharmaceutical CalculationsDocument20 pagesPharmaceutical CalculationsMonique PendijitoNo ratings yet
- Antibacterial Potential of Ethanol From Banana Peel ExtractDocument7 pagesAntibacterial Potential of Ethanol From Banana Peel ExtractJasmen Sabroso PasiaNo ratings yet
- BBLK Surabaya: National Tuberculosis Reference Laboratory For Culture/Drug Susceptibility TestingDocument12 pagesBBLK Surabaya: National Tuberculosis Reference Laboratory For Culture/Drug Susceptibility TestingMas Paijo PeloukNo ratings yet
- CEL2103 - Writing Portfolio Task 1 - Brainstorm FormDocument2 pagesCEL2103 - Writing Portfolio Task 1 - Brainstorm FormmohddartleNo ratings yet
- JC 5Document63 pagesJC 5Shraddha PatilNo ratings yet
- Vocabulary 1Document3 pagesVocabulary 1LUIS ADRIAN COQUE SERRANONo ratings yet
- 8.9.1.22 - GC-1202 - Hazardous Area ClassificationDocument3 pages8.9.1.22 - GC-1202 - Hazardous Area Classificationkagasaw023No ratings yet
- Introduction To Special Education: Taylor-White Elementary SchoolDocument23 pagesIntroduction To Special Education: Taylor-White Elementary SchoolEric D. ValleNo ratings yet
- COSHH Form - HF-Beta ZeoliteDocument2 pagesCOSHH Form - HF-Beta ZeoliteshashanebonnitaNo ratings yet
- Pinlight/Led 15 Watts Flourescent Lamp Led: LegendDocument1 pagePinlight/Led 15 Watts Flourescent Lamp Led: LegendTuti EncinasNo ratings yet
- O15062020011 PDFDocument50 pagesO15062020011 PDFakshat tiwariNo ratings yet
- ManeirDocument24 pagesManeirIlidioo Kaifaz Kaifaz KaifazNo ratings yet
- RR No. 11-2018Document47 pagesRR No. 11-2018Micah Adduru - Robles100% (1)
- Case Study On Polyester Fiber Synthesis & Fire Protection Facilities at Reliance Industries Barabanki Manufacturing UnitDocument57 pagesCase Study On Polyester Fiber Synthesis & Fire Protection Facilities at Reliance Industries Barabanki Manufacturing Unitवात्सल्य कृतार्थNo ratings yet
- CHA 2019 Medical Staff Bylaw SampleDocument167 pagesCHA 2019 Medical Staff Bylaw SampleBradNo ratings yet
- Basic-Information - Yankee-Dryer-Service Teoria Inspeccion YankeeDocument14 pagesBasic-Information - Yankee-Dryer-Service Teoria Inspeccion YankeeJohny PastusanoNo ratings yet
- APA Practice Guideline For The Treatment of Patients With Substance Use DisordersDocument276 pagesAPA Practice Guideline For The Treatment of Patients With Substance Use DisordersRaja Ahmad Rusdan MusyawirNo ratings yet
- Bcop SV Slo Budget-System Voljc EngDocument45 pagesBcop SV Slo Budget-System Voljc EngmilenastokanovicNo ratings yet
- VCQW4142 1 PDFDocument4 pagesVCQW4142 1 PDFDamodar SinghNo ratings yet
- English UasDocument15 pagesEnglish UasNurul NurhasanahNo ratings yet
- JSA - Doc Job Safety Analysis NewDocument3 pagesJSA - Doc Job Safety Analysis NewKali MuthuNo ratings yet