Skin PDF
Skin PDF
Uploaded by
LanaAmerieCopyright:
Available Formats
Skin PDF
Skin PDF
Uploaded by
LanaAmerieOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Skin PDF
Skin PDF
Uploaded by
LanaAmerieCopyright:
Available Formats
Pathology: SKIN INFECTIONS Verruca plantaris and palmaris (palmoplantar wart=both)
Viral Skin Infections Occur on the soles (Verruca plantaris) and palms
1. Verrucae (Verruca Palmaris)
2. Herpes Simplex Virus infection Rough scaly lesions, 1-2 cm in diameter; may
3. Varicella –Zoster coalesce and be confused with calluses
4. Molluscum contagiosum
Morphology:
I. Verrucae (warts)
Common lesions of children and adolescents but may
be encountered at any age
Caused by human papilloma viruses
Transmission: direct contact
Generally self-limited, regressing spontaneously
within 6 months up to 2 years
Classification based on Location and Clinical Morphology:
Verruca vulgaris
Verruca plana
Verruca plantaris / palmaris (Palmoplantar wart)
Condyloma acuminatum
Verruca vulgaris
Condyloma acuminatum
Common wart
Venereal wart, Anogenital wart
Associated with HPV-2,4, and 7
Occurs on the penis, female genitalia, urethra,
Occur at any site but most frequently on the dorsal
perianal area and rectum
aspect of the finger and hands
Appear as soft, tan, cauliflower- like masses
Painless, circumscribed, firm, elevated, papules 1-
Low risk: HPV 6, 11 (BENIGN)
10mm in size with papillomatous (“verrucous” )
High risk: HPV 16,18,31,33 associated with
hyperkeratotic surfaces
anogenital cancers(MALIGNANT)
Generally self-limited but may persist for a few
months up to several years
Koebner phenomenon : formation of new warts at
sites of trauma(pagkamot dagdag ng warts)
Histopathology: Verucae
Acanthosis, papillomatosis, hyperkeratosis,
parakeratosis
Verruca plana : same histologic features as verruca
Circumscribed, firm, elevated, papules 1-10mm in size
vulgaris but “without papillomatosis”(reason kung
with papillomatous (“verrucous” ) hyperkeratotic
bakit sya flat)
surfaces
Verruca plana
Flat wart
Common on the face and or the dorsal surfaces of the
hand
Slightly elevated, flat, smooth, tan papules generally
smaller than verruca vulgaris
Paid Advertisement:
Peetz By: Dr. Pre
II. Herpes simplex infection
Herpes simplex virus type 1- orofacial type
Ex. Acute gingivostomatitis, Lips (herpes labialis, or
“cold sores”), any part of the skin, oral mucosa
Herpes simplex virus type 2 – genital type
Ex. Herpes Genitalis
Transmitted through the exchange of saliva, semen,
cervical fluid or vesicle fluid from active lesions
Koilocytic cells in the upper stratum malphigii
and in the granular layer Pathogenesis:
Produce acute and latent infections
Koilocytes : small, round, deeply basophilic Replicate in the skin and mucous membranes at the
nuclei surrounded by a clear halo and pale- site of entrance (usually oropharynx or genitals)
staining cytoplasm produce infectious virions vesicular lesions of the
epidermis
Spread to sensory neurons establish latent infection
Gross:
Cold sores
Blisters and vesicles around mucosal orifices (lips,
nose)
Formed by intercellular edema and ballooning
degeneration of epidermal cells
Gingivostomatitis
Usually encountered in children; HSV-1
Vesicular eruption extending from the tongue to
Clumped keratohyaline the retropharynx; (+) cervical lymphadenopathy
granules(Hypergranulosis) Patient will have painful swallowing
Genital herpes
HSV-2
Vesicles on genital mucous membranes and
external genitalia burst ulcerate
Can be transmitted to neonates during passage
through the birth canal (herpes keratitis,
fulminant infection)
Verrucus growth pattern
Koilocytic change of the cells
Paid Advertisement:
Peetz By: Dr. Pre
Histopathology:
Ballooning degeneration of epidermal cells
Acantholysis
Shingles- Herpes Zoster
Gross:
Activation of latent infection
Affects the elderly
Grouped vesicles along the course of a sensory nerve
Vesicle bases frequently hemorrhagic, some necrotic and
may ulcerate
Some lesions indistinguishable from Varicella
Cowdry type A inclusions:
Large, pink to purple intranuclear inclusions
Contain intact and disrupted virions
Multinucleated cells(Glassy nuclei)
III. Varicella zoster
Chicken pox and shingles
Acute infection : chicken pox (varicella)
Reactivation: shingles (herpes zoster)
Pathogenesis:
Infects mucous membranes, skin, and neurons
Self-limited primary infection in immunocompetent
individuals
Establishes latent infection in sensory ganglia
Transmitted in epidemic fashion by aerosols Re-activation of infections appear on the dermatomal lines
Disseminates hematogenously widespread
vesicular skin lesions Histopathology:
Infects neurons and/or satellite cells around
neurons in the dorsal root ganglia
Localized recurrence is most frequent and most
painful in dermatomes innervated by trigeminal
ganglia
Chicken pox- varicella
90% of cases occur in children (< 14 y/o)
Rash occurs approximately 2 weeks after
respiratory infection
Centrifugal distribution
Macule vesicle (“dew drops on a rose petal”)
In ganglia: (+) lymphoplasmacytic infiltrates with
Vesicle: contains intranuclear inclusions
intranuclear inclusions within neurons
Lesions in varying stages are present at one time
Vesicles rupture crust over heal by
regeneratiion
Complications: pneumonitis, encephalitis
Paid Advertisement:
Peetz By: Dr. Pre
Tzanck smear Bacterial Skin Infections
1. Impetigo
2. Furuncle
3. Carbuncle
4. SSSS
5. Erysipelas
6. Cellulitis
7. Leprosy
I. Impetigo
Scrapings are subjected to PAP Smear Caused by group A- beta hemolytic Streptococci and
Multinucleated giant cells andinclusion bodies Staphylococcus aureus
are found on tzanck smear Impetigo contagiosa (nonbullous impetigo) : Strep
Impetigo bullosa : Staph
IV. Molluscum contagiosum Involves exposed skin, i.e. face and hands
Common, self-limited Erythematous macule pustule shallow erosions
Caused by Poxvirus covered with drying serum (honey colored crust)
Transmission : direct bodily contact or indirectly
via fomites Gross:
Multiple lesions on the skin and mucous
membranes (trunk, and anogenital areas)
Gross:
Histopathology:
Lesions are firm, often pruritic, pink to skin- Accumulation of neutrophils beneath stratum corneum
colored, umbilicated papules (0.2-0.4cm) Subcorneal pustules
Curd-like material may be expressed from Crust: serum, neutrophils and debris
umbilication
Molluscum bodies
Nuclei are pushed toward the periphery
Paid Advertisement:
Peetz By: Dr. Pre
II. Furuncle
Focal suppurative inflammation of skin and
subcutaneous tissue
Also known as “Boil” or Pigsa
Recurrent
Solitary or multiple
Moist, hairy areas (face, groin, legs, axillae, and
submammary folds)
Etiology: S.aureus
Begins in a single hair follicle abscess thinning
and rupturing the overlying skin
RITTER’S DISEASE
-Caused by S. aureus
Gross:
Split in granular layer
Dermal edema, no necrosis of epidermis
Acantholysis may be present
DDx:
Toxic Epidermal Necrolysis (Lyell’s disease)
-Caused by Drug interaction
III. Carbuncle
Deeper suppuration that spreads laterally beneath
the deep subcutaneous fascia
Eventually burrows superficially to erupt in multiple
adjacent skin sinuses
Appear beneath the skin, upper back and posterior
neck
May progress into osteomyelitis
Etiology: S.aureus
V. Cellulitis
Acute, diffuse spreading, edematous, suppurative
inflammation of deep subcutaneous tissue
Lower extremities, periorbital area, scrotum
Spreading infection, affecting deeper tissues
Warm, tender, ill-defined margins
Associated lymphangitis and lymphadenitis
Necrotizing fasciitis : Involvement of underlying fascia and
muscle
May ulcerate / necrose
IV. Staphylococcal Scalded Skin Syndrome: Ritter’s Disease
Toxin-mediated, exfoliative dermatitis
In children with Staph infection of nasopharynx and
skin
Sunburn-like rash bullae formation partial or
total skin loss sheared off
Associated infection or source :
URTI, conjunctivitis, umbilical sepsis or occult
infection
Blister formation secondary to toxin that
specifically cleaves desmoglein 1 molecule
(responsible for cell to cell adhesion)
Mortality: 2-3%
Paid Advertisement:
Peetz By: Dr. Pre
Histopathology: Histopathology:
Extensive Infllammation and invasion of
inflammatory cells
Diffuse, acute, edematous, neutrophilic, interstitial
reaction : dermis, epidermis and subcutaneous tissue
VI. Erysipelas Perivascular(surround blood vessels) and
Middle-aged, warm climates periadnexal(surround eccrine glands and hair follicles of
Caused by exotoxins from superficial infections the skin) microabscess
with S. pyogenes Tissue necrosis may be minor
Rapidly spreading, erythematous cutaneous
swelling VII. Mycobacteria
May begin on the face, or less commonly, on the
body or extremity LEPROSY (Hansen’s Disease)
Well-demarcated, serpiginous border : Slowly progressive infection of skin and peripheral nerves
“butterfly” on face Mycobacterium leprae
Transmission: person-to-person via aerosols from lesions
in the upper respiratory tract
Grows in cool places like skin and extremity
Low communicability=needs large amount of pathogen
before eliciting an infection
“Zeil-Neehlsen”-stain used for identifying acid fast
bacilli(look up nyo spelling di ko maalala tamang spelling)
Pathogenesis:
Obligate intracellular, acid-fast organism
Grows poorly in culture
Grows at 32-34 C : human skin
Cell-mediated immunity
No toxins, virulence based on cell wall properties
Paid Advertisement:
Peetz By: Dr. Pre
A. TUBERCULOID LEPROSY Gross:
Less severe form Skin, peripheral nerves (ulnar and peroneal), anterior
Dry, scaly skin lesions that lack sensation chamber of the eye, upper airways (down to the larynx),
Asymmetric peripheral nerve involvement testes, hands and feet are involved
Skin anesthesia, skin and muscle atrophy Hypoesthetic anesthetic
Contractures, paralyses, autoamputation of “Leonine facies”
fingers and toes
GROSS:
Localized skin lesions (flat and red )
enlarge irregular shapes with indurated,
elevated, hyperpigmented margins and
depressed pale centers (central healing)
Paucibacillary (No organism)
Prominent neuronal involvement
(+) granulomas enclosing nerves nerve
destruction
T-cell immunity
Histopathology:
B. LEPROMATOUS LEPROSY
More severe form
Symmetric skin thickening and nodules
Also called Anergic Leprosy
Widespread invasioin of mycobacteria into
Schwann cells and into endoneural and Globi : large aggregates of lipid-laden histiocytes (LEPRA
perineural macrophages cells=macrophage with organisms inside) filled with
masses of organism
(-) granuloma formation : failure of TH1 response
Grenz zone
Paid Advertisement:
Peetz By: Dr. Pre
Globi (Fite Faraco) I. Dermatophytes
Capable of colonizing keratinized tissue such as
stratum corneum of epidermis, hair and nails
Stains used for demonstrating fungi:
Periodic Acid Schiff (PAS) : Red Stain
Gomori Methenamine Silver (GMS) : Black
Stain
Dermatophytosis of the scalp
Asymptomatic, often hairless patches of skin
associated with mild erythema, crust formation and
scale
Arthrospores(asexual spores) coat the outside of
hairshaft and hyphae extend to the microfollicle
Tinea Capitis
Grenz zone
Very well demarcated, often hairless patches of skin
with mild erythema, very itchy and presence of
scaling
Area that is not affected by the disease between the
dermis and epidermis(white zone)
TInea Corporis
Tuberculosis of the Skin
*REFER TO GIVEN HANDOUT*
Common superficial fungal infection of the body
surface that commonly affects persons of all ages, but
Fungal skin infections
particular in children
1. Dermatophytosis
2. Pityriasis versicolor Predisposing factors: excessive heat and humidity,
3. Chromoblastomycosis exposure to infected animals, chronic
4. Phaeohyphomycosis dermatophytosis of feet or nails
5. Sporotrichosis Seen as expanding, erythematous plaque with an
6. Mycetoma elevated scaling border
Histopathology:
DERMATOPHYTES
Parakeratosis, acanthosis, neutrophils in
a) Epidermophyton
parakeratotic crust
b) Trichophyton
Fungal hyphae seen in parakeratotic stratum
c) Microsporum
corneum
Paid Advertisement:
Peetz By: Dr. Pre
Mild dermal inflammation II. Tinea Versicolor(Ptyriasis Versicolor)
Acanthosis, parakeratosis and mixed inflammatory Malassezia furfur
infiltrate in superficial dermis Common in tropical climate
Multiple, irregular areas of hypo-and
Tinea Pedis hyperpigmentation seen primarily on the upper
Athlete’s foot” trunk
Diffuse erythema and scaling Circular, macular, scaling, and erythematous
Initially localized in the interdiginous areas
Tinea unguium: specific term which refers to
dermatophyte infection of the nail. Gross:
Discoloration, thickening and deformity of
the nail plate
Onychomycosis : general term which refers
to nail infection due to any fungus including
dermatophytes
Histopathology:
Tinea cruris
“jock itch”
Sharply demarcated erythematous patches or thin
plaques in the inguinal area extending
crescentically down the thighs
Common in men
Predisposing factors:
Heat, friction
May spread to perineal and / or perianal regions as
well as the scrotum
Common in men
Erythematous plaque extending crescentically
down the thighs
Mild acanthosis, hyperkeratosis, focal
parakeratosis, hypo-or hyperpigmentation
of basal layer
Minimal superficial perivascular infiltrate in dermis
Paid Advertisement:
Peetz By: Dr. Pre
“Spaghetti and meatballs” Fungal elements: Round, dark brown, thick-walled,
ovoid sclerotic bodies, 6-12um
“Stack of bricks” Murry-form(double check spelling)
IV. Phaeohyphomycosis
Subcutaneous or systemic infection caused by pigmented,
fungi with both yeast-like and hyphal-like forms
Bipolaris
Phialophora
Alternaria
Exophiala
Subcutaneous phaeohyphomycosis typically presents as a
solitary, discrete, asymptomatic, abscess or nodule on the
extremity
History of trauma or a splinter can sometimes be elicited
III. Chromoblastomycosis Gross:
Slowly progressive cutaneous mycosis caused by
dermatiaceous (pigmented) fungi that occur as
round, nonbudding forms in tissue sections
Saprophytic fungi
Phialophora
Fonsacaea
Exophiala
Cladosporium
Most common cause : Fonsacaea pedrosoi
Primary lesion develops as a result of traumatic
implantation of the fungus into the skin
Spread by autoinoculation of superficial lymphatic
vessels
Gross: Always appear as a nodule in the digits
Located in lower extremities as verrucous papules, Histopathology:
nodules and plaques(can be mistaken for verruca
because of wart-like appearance)
Histopathology:
Suppurative granulomatous inflammation
single large cavity with surrounding fibrous capsule,
Pseudoepitheliomatous hyperplasia with heavy cont’g PMN’s and fibrin
dermal infiltrate of epithelioid histiocytes, Organisms found within cavity and cavity edge, often
multinucleated giant cells, small abscesses, mixed within histiocytes
inflammatory infiltrate and a granulomatous
reaction
Paid Advertisement:
Peetz By: Dr. Pre
V. Sporotrichosis Pseudoepitheliomatous epidermal hyperplasia with
Caused by Sporothrix schenkii microabscess formation
Dimorphic fungus (filamentous=outside the body Central suppurative zone composed of neutrophils,
and yeast-like=inside the body) surrounded by epitheloid cells, giant cells, plasma
Ovoid bodies cells, lymphocytes
2 cutaneous forms: Asteroid bodies=“Splendore Hoeppli Material”
Lymphocutaneous :
Painless papule ulcerating nodules usually VI. Mycetoma
on a finger or hand Chronically discharging infection of skin and
Chain of asymptomatic nodules appear along subcutaneous tissue
the lymph vessel draining the area Caused by:
undergo suppuration with subsequent Actinomycetoma:
ulceration Bacteria (Nocardia, Actinomyces,
Fixed cutaneous: Streptomyces),
Solitary plaque or occasionally a group of Eumycetoma:
lesions, most commonly on an arm or the Fungi (Madurella mycetoma,
face M.guisea, P.boydii, etc.)
superficial crusting or verrucous surface Nodule abscess discharging fistula to skin
No tendency toward lymphatic spread muscles and tendons damaged eventually may
affect bone osteomyelitis
Gross: “Madura foot”
Sulfur granules or “grains” discharged from draining
sinuses
Gross:
st
1 picture: Lymphocutaneous
nd
2 picture: Fixed Cutaneous
Pathogenesis:
S. schenckii commonly contacted through exposure
to vegetal matter, often a splinter or thorn
Histopathology:
“sulfur granules” within suppuration & surrounded by
histiocytes, multinucleated giant cells and granulation
tissue
Diagnosis can be established only by finding “sulfur
granules”
to differentiate bacterial from fungal causes, special
stains are employed:
Gram stain
Lactophenol blue
Paid Advertisement:
Peetz By: Dr. Pre
Histopathology: Nodular variant:
Itching nodules, commonly on the scrotum
Acanthosis with dermal perivascular
lymphocytic and eosinophilic infiltrate
Norwegian scabies or crusted scabies
Innumerable mites present
Widespread erythema, hyperkeratosis, and
crusting but no obvious burrows
Group of mycoses Excoriation and Burrows
Observe the black “Sulfur Granules”
Parasitic infestations
Scabies
Sarcoptes scabei mite
Penetrate skin as linear burrows up to 3-cm long
Female mite burrows under the stratum corneum
deposits eggs producing burrows on the interdigital
skin, palms, wrists, periareolar skin of women and
genital skin of men
Larvae hatch in 3-5 days and mature in 10-14 days Eggs &Scybala
Burrows:
Pathognomonic lesion Histopathology:
Linear, poorly defined streaks
Vesicle may be visible near the blind end of
the burrow
Secondary excoriation and infection
Papulovesicular variant
burrows on the interdigital skin, palms,
wrists, periareolar skin of women and genital
skin of men
Spongiosis in the stratum malphigii near the
mite vesicle formation
Paid Advertisement:
Peetz By: Dr. Pre
Pediculosis
Caused by head louse, crab louse, and body louse
Pruritic
Louse or its eggs, attached to hair shafts, can usually be
seen with the unaided eye
Swabeng Recap:
Try to enumerate the causative agents, types, morphology,
histopathology and pathogenesis of each disease below
without going back. Para malaman nyo kung swabeng swabe
ang aral mo o kailangan mo ng isa pang swabeng reading.
1. VIRAL:
Verrucae
Herpes simplex infection
Varicella –Zoster
Molluscum contagiosum
2. BACTERIAL :
Impetigo
Furuncle
Carbuncle
SSSS
Erysipelas
Cellulitis
Leprosy
3. FUNGAL INFECTIONS
Dermatophytosis
Pityriasis versicolor
Chromoblastomycosis
Phaeohyphomycosis
Sporotrichosis
Mycetoma
4. ARTHROPOD INFESTATIONS
Scabies
Pediculosis
END OF TRANSCRIPTION!
Oaaaaah swabeng swabe! Come join me brothaa!!!
Paid Advertisement:
Peetz By: Dr. Pre
You might also like
- Veterinary Forensic Medicine and Forensic Sciences by Jason H. Byrd (Editor) Patricia Norris (Editor) Nancy Bradley-Siemens (Editor)Document497 pagesVeterinary Forensic Medicine and Forensic Sciences by Jason H. Byrd (Editor) Patricia Norris (Editor) Nancy Bradley-Siemens (Editor)Mae PimentelNo ratings yet
- Primary and Secondary Skin Lesions - IJDocument43 pagesPrimary and Secondary Skin Lesions - IJThanh Thảo Huỳnh ThịNo ratings yet
- Table of Differentiation of ParasitesDocument18 pagesTable of Differentiation of ParasitesManuel RendonNo ratings yet
- Erythema NodosumDocument42 pagesErythema Nodosummedpedshospitalist100% (1)
- Ncvms Approved Constitution and BylawsDocument12 pagesNcvms Approved Constitution and BylawsRoyd Joseph R. MosasoNo ratings yet
- DA Sistemik TerapiDocument11 pagesDA Sistemik TerapiariyatiNo ratings yet
- Ghid Anestezie Locala PDFDocument19 pagesGhid Anestezie Locala PDFanaNo ratings yet
- Skintox Practiceguidelines EGFR SCCDocument17 pagesSkintox Practiceguidelines EGFR SCCFelipe Scholz RamosNo ratings yet
- Dermnet NZ: Special Stains and TestsDocument4 pagesDermnet NZ: Special Stains and TestsRaja Sekaran DuraiNo ratings yet
- Tumors DR Ahmed KamelDocument98 pagesTumors DR Ahmed KamelABDALRAHMAN ABDALLAH KASEMNo ratings yet
- List of Dermatology Differential Diagnosis and Signs in DermatologyDocument54 pagesList of Dermatology Differential Diagnosis and Signs in DermatologyAhmadq76No ratings yet
- Dermatology Lectures JRRMMCDocument10 pagesDermatology Lectures JRRMMCGi Em100% (1)
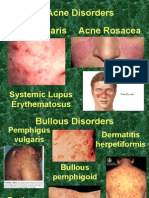
- Acne Vulgaris Acne Rosacea Acne Disorders: Systemic Lupus ErythematosusDocument19 pagesAcne Vulgaris Acne Rosacea Acne Disorders: Systemic Lupus Erythematosusapi-26938624No ratings yet
- Chapter-03 Acneiform EruptionDocument6 pagesChapter-03 Acneiform EruptionSylvia DiamondNo ratings yet
- AAD BF Paisley Tie DiagnosisDocument2 pagesAAD BF Paisley Tie Diagnosiskahkashanahmed065No ratings yet
- Derma Final 2021 (19th, 25th of May)Document91 pagesDerma Final 2021 (19th, 25th of May)Mr.FantasthiccNo ratings yet
- Derma MegatableDocument21 pagesDerma MegatableNicole ChanNo ratings yet
- Paraneoplastic DermatosesDocument57 pagesParaneoplastic DermatosesMohamed Riyaz100% (1)
- LALA Megatable DermaDocument39 pagesLALA Megatable DermaJorelle MarquezNo ratings yet
- The 3rd Year Derma Missing TableDocument6 pagesThe 3rd Year Derma Missing TableEmil GulmaticoNo ratings yet
- Phototherapy For Dermatologic ConditionsDocument18 pagesPhototherapy For Dermatologic ConditionsSeth MosebyNo ratings yet
- Dermatology Imp Images NEET PGDocument5 pagesDermatology Imp Images NEET PGSmrithi ThriloNo ratings yet
- Topical Antibiotics in DermatologyDocument19 pagesTopical Antibiotics in DermatologyJejem Marandra EmkamasNo ratings yet
- DR Pallavi - Dermatology FMGEDocument74 pagesDR Pallavi - Dermatology FMGEVickyNo ratings yet
- Melanocytic TumorsDocument254 pagesMelanocytic TumorsmixandgoNo ratings yet
- General Considerations For Topical PreparationsDocument6 pagesGeneral Considerations For Topical PreparationsOccamsRazorNo ratings yet
- Dermatology Revision 2Document49 pagesDermatology Revision 2Bahaa Shaaban100% (2)
- Eczema, Psoriasis, Cutaneous Infections, Acne, and Other Common Skin DisordersDocument6 pagesEczema, Psoriasis, Cutaneous Infections, Acne, and Other Common Skin DisordersElrey InocianNo ratings yet
- Palmoplantar KeratodermaDocument4 pagesPalmoplantar KeratodermakurutalaNo ratings yet
- HirsutismDocument86 pagesHirsutismBella AgustinNo ratings yet
- Dermatology Mcqs For PGDocument204 pagesDermatology Mcqs For PGjusta7863No ratings yet
- Derm StuffDocument7 pagesDerm StuffSudesna Roy ChowdhuryNo ratings yet
- An Approach To The Patient With ErythrodermaDocument42 pagesAn Approach To The Patient With ErythrodermaShakilNo ratings yet
- Anti Fungal DrugsDocument6 pagesAnti Fungal Drugsbilal ahmadNo ratings yet
- Tumours of Skin: DR F Bhatti Pennine VTS Sept 08Document39 pagesTumours of Skin: DR F Bhatti Pennine VTS Sept 08pfxbkNo ratings yet
- Spongiotic Dermatitis: Aka EczemaDocument8 pagesSpongiotic Dermatitis: Aka EczemafadoNo ratings yet
- Clinical Pearls DermatologíamatologyDocument4 pagesClinical Pearls DermatologíamatologyMaritza24No ratings yet
- Acne Vulgaris: Basic Dermatology CurriculumDocument58 pagesAcne Vulgaris: Basic Dermatology CurriculumJhoel Jhonatan Torres MuñozNo ratings yet
- AAD Atopic Dermatitis - Phototherapy and Systemic Agents 2014Document42 pagesAAD Atopic Dermatitis - Phototherapy and Systemic Agents 2014Yan Zhen YuanNo ratings yet
- Superficial and Deep Perivascular DermatitisDocument55 pagesSuperficial and Deep Perivascular DermatitisMarnie RoviraNo ratings yet
- Infectious DermatologyDocument206 pagesInfectious DermatologyAaron Christian Earl VillosoNo ratings yet
- Steroid Pulse Therapies in DermatologyDocument4 pagesSteroid Pulse Therapies in DermatologyWelly WijayantiNo ratings yet
- Srinadh Neonatal Skin Conditions FinalDocument110 pagesSrinadh Neonatal Skin Conditions FinalSrinadh Pragada100% (1)
- Erythema MultiformeDocument29 pagesErythema MultiformeSurabhi Sharma100% (1)
- 3) Genodermatosis - Dr. Darseem: NeurofibromatosisDocument4 pages3) Genodermatosis - Dr. Darseem: NeurofibromatosisOman ArifNo ratings yet
- What Is A RashDocument8 pagesWhat Is A RashJudi Ann MagsacayNo ratings yet
- Miliaria, Leucoplakia, PPPDocument44 pagesMiliaria, Leucoplakia, PPPcute100% (1)
- Dermatology PDFDocument23 pagesDermatology PDFjonyNo ratings yet
- 9-Patologi Skin PDFDocument34 pages9-Patologi Skin PDFririnNo ratings yet
- New Criteria For Lupus: The Author(s) 2020Document8 pagesNew Criteria For Lupus: The Author(s) 2020Kok Hui DiongNo ratings yet
- Fungal InfectionsDocument9 pagesFungal InfectionsCoral Srinivasa RamaluNo ratings yet
- Introduction To Dermatology Assessment of A Dermatologic PatientDocument86 pagesIntroduction To Dermatology Assessment of A Dermatologic PatientAtif100% (1)
- Vesiculobullous Disorders in Children2Document5 pagesVesiculobullous Disorders in Children2Luciana FernandesNo ratings yet
- Dermatology Revision E6.5 @theboggusdocDocument36 pagesDermatology Revision E6.5 @theboggusdockhushi koliNo ratings yet
- Clinico-Epidemiological Study of Dermatophytosis in Teaching Hospital of North KarnatakaDocument4 pagesClinico-Epidemiological Study of Dermatophytosis in Teaching Hospital of North KarnatakaAldo NovaNo ratings yet
- PsoriasisDocument27 pagesPsoriasisMishaNo ratings yet
- Sqweqwesf Erwrewfsdfs Adasd Dhe: Dermnet NZDocument19 pagesSqweqwesf Erwrewfsdfs Adasd Dhe: Dermnet NZkdwazirNo ratings yet
- Dermatology and Venerology Notes 4Document111 pagesDermatology and Venerology Notes 4SpyrosNo ratings yet
- Gyne - Case 15 Benign Lesions of The Vulva & VaginaDocument2 pagesGyne - Case 15 Benign Lesions of The Vulva & Vaginacbac1990No ratings yet
- Leishmaniasis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandLeishmaniasis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Clinical Cases in Pigmentary DisordersFrom EverandClinical Cases in Pigmentary DisordersTorello LottiNo ratings yet
- SLE SketchyDocument2 pagesSLE SketchyLanaAmerieNo ratings yet
- Ah PDFDocument134 pagesAh PDFLanaAmerieNo ratings yet
- Truelearn Stuff PDFDocument16 pagesTruelearn Stuff PDFLanaAmerieNo ratings yet
- Cluster of Lesions, PapularDocument3 pagesCluster of Lesions, PapularLanaAmerieNo ratings yet
- Congenital Anomalies of Kidney and Lowe Urinary TractDocument2 pagesCongenital Anomalies of Kidney and Lowe Urinary TractLanaAmerieNo ratings yet
- Table 1: Infective Endocarditis Non Infective Myocarditis Myocardidits PericarditisDocument3 pagesTable 1: Infective Endocarditis Non Infective Myocarditis Myocardidits PericarditisLanaAmerieNo ratings yet
- "Mapping The Nephron" Cellular Templates: Gina Bartoni Lana Daniel ShinDocument11 pages"Mapping The Nephron" Cellular Templates: Gina Bartoni Lana Daniel ShinLanaAmerieNo ratings yet
- Macules Macules and Papules Papules VesiclesDocument6 pagesMacules Macules and Papules Papules VesiclesLanaAmerieNo ratings yet
- RNL DruDocument1 pageRNL DruLanaAmerieNo ratings yet
- OPP - Lab - Counterstrain - Ribs, Anterior, PosteriorDocument1 pageOPP - Lab - Counterstrain - Ribs, Anterior, PosteriorLanaAmerieNo ratings yet
- Integumentary Lec 1: Overview of The Integument: A-Integumentary (Skin) SystemDocument6 pagesIntegumentary Lec 1: Overview of The Integument: A-Integumentary (Skin) SystemLanaAmerieNo ratings yet
- Urinery IncontinsetenceDocument1 pageUrinery IncontinsetenceLanaAmerieNo ratings yet
- AvianInsightVol1 05Document2 pagesAvianInsightVol1 05Bryan NicollNo ratings yet
- What Is The Flu? How Is The Flu Spread?Document2 pagesWhat Is The Flu? How Is The Flu Spread?porfirio ruizNo ratings yet
- Aprendo en Casa Semana 2Document7 pagesAprendo en Casa Semana 2Yesi GNo ratings yet
- Pns Code of Good Animal Husbandry Practices For Chicken - Broilers and LayersDocument10 pagesPns Code of Good Animal Husbandry Practices For Chicken - Broilers and LayersOliver TalipNo ratings yet
- Directory of Avma Listed Veterinary Colleges of The World: NangarharDocument23 pagesDirectory of Avma Listed Veterinary Colleges of The World: NangarharMuneebNo ratings yet
- Biologi Bordetella PertussisDocument7 pagesBiologi Bordetella PertussisSetyadinda Putri MalindaNo ratings yet
- Avion FluDocument1 pageAvion FluImaan RiazNo ratings yet
- The Rise of Veterinary ForensicsDocument40 pagesThe Rise of Veterinary ForensicsMateoNo ratings yet
- English Task "Factual Report" About Coronaviruses: / By: M.Aijul Furqan Xiipa2Document3 pagesEnglish Task "Factual Report" About Coronaviruses: / By: M.Aijul Furqan Xiipa2Aijul FurqanNo ratings yet
- Febrele HemoragiceDocument23 pagesFebrele HemoragicegvfhgNo ratings yet
- Research Assessment 10Document2 pagesResearch Assessment 10api-523475875No ratings yet
- Animal Movements WorkbookDocument20 pagesAnimal Movements WorkbookAdam AdhaNo ratings yet
- Daftar Pustaka PertusisDocument1 pageDaftar Pustaka PertusisErica PuteriNo ratings yet
- Introduction To ImmunologyDocument9 pagesIntroduction To ImmunologyDr-Rmz RabadiNo ratings yet
- ToxoplasmosisDocument27 pagesToxoplasmosisKnjigeNo ratings yet
- PNS - Bafs 267.2022 - PNS Swine - Good Animal Husbandry Practices (GAHP)Document25 pagesPNS - Bafs 267.2022 - PNS Swine - Good Animal Husbandry Practices (GAHP)Johana Pinagayao AngkadNo ratings yet
- Canine DiseasesDocument5 pagesCanine Diseasessambhaji1976No ratings yet
- Acute Respiratory InfectionsDocument22 pagesAcute Respiratory InfectionsKumara GuruNo ratings yet
- Control of Drugs and Cosmetics Regulations 1984 (Amendment 2009)Document16 pagesControl of Drugs and Cosmetics Regulations 1984 (Amendment 2009)NasuhaNo ratings yet
- CV - DR Rahul UpdatedDocument3 pagesCV - DR Rahul UpdatedDrRahul PaulNo ratings yet
- MumpsDocument1 pageMumpsFikri PutroNo ratings yet
- @heto Pala Ung Unang Comment Ni Sir Sa Inot Kong Consultation Na Yaon Dyan Sa Baba Kang Comment Ni Sir,,, Hahah, Thank You AiraDocument6 pages@heto Pala Ung Unang Comment Ni Sir Sa Inot Kong Consultation Na Yaon Dyan Sa Baba Kang Comment Ni Sir,,, Hahah, Thank You Airabaoshi3382No ratings yet
- Herpes Simplex SymptomsDocument3 pagesHerpes Simplex SymptomsInes JianaNo ratings yet
- Resume Holly Standeford For KisdDocument3 pagesResume Holly Standeford For Kisdapi-340637026No ratings yet
- Gape WormDocument4 pagesGape WormNjoku IykeNo ratings yet
- WSJ - Printing Declawing Cats Provokes A Billion-Dollar DebateDocument4 pagesWSJ - Printing Declawing Cats Provokes A Billion-Dollar DebateTesy MctestersonNo ratings yet
- K - 12 Grade: California Immunization Requirements ForDocument2 pagesK - 12 Grade: California Immunization Requirements Forjulian14No ratings yet
- tmp8237 TMPDocument10 pagestmp8237 TMPFrontiersNo ratings yet