PLM Abdomen
PLM Abdomen
Uploaded by
Claudine Victoria TaracatacCopyright:
Available Formats
PLM Abdomen
PLM Abdomen
Uploaded by
Claudine Victoria TaracatacOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
PLM Abdomen
PLM Abdomen
Uploaded by
Claudine Victoria TaracatacCopyright:
Available Formats
3.
04
November 24, 2015
ABDOMINAL PORTION OF THE ESOPHAGUS, STOMACH, DUODENUM
& ACCESSORY DIGESTIVE GLANDS
#NaPAASCU
TOPIC OUTLINE
I. Esophagus
a. Abdominal Esophagus
b.
c.
Esophageal Hiatus
Relations
d. Termination
e. Blood Supply, Venous and Lymphatic Drainage
II. Stomach
a. Parts of the Stomach
b. Relations
c. Stomach bed
d. Blood Supply, Venous and Lymphatic Drainage
e. Innervation
f. Omenta
g. Gastric Ulcer
III. Small Intestine
a. Duodenum
b. Divisions of the Duodenum
c. Blood Supply, Venous, and Lymphatic Drainage
Accessory Glands of the Gastrointestinal Tract
IV. Liver
a. Function
Figure 1. Abdominal Aspect of the Diaphragm
b.
c.
Relations
Surfaces
iii esophagealaperture entersthruabdomen i of
A. Abdominal Esophagus midline
i. Porta Hepatis
d. Peritoneal Ligament
1-2.5cm in length; slightly broader at cardiac orifice than at
diaphragmatic aperture.
e. Divisions
i. Anatomical
Lies to the left of the midline; enters abdomen through esophageal
aperture at T11 vertebra (According to Gray’s Anatomy .
ii. Functional Anterior is longer than posterior wall due to obliquity of the crura.
f.
g.
Blood Supply, Venous, and Lymphatic Drainage
Innervations
7 Surface covered by thin layer of connective tissue and visceral
peritoneum that contain anterior and posterior vagus nerves and
h. Portal System
i. Areas of Porto-caval Anastomoses
esophageal branches of the left gastric vessels.
V. Biliary Apparatus so Tethered to the margins of muscular esophageal hiatus in the
diaphragm by the phrenoesophageal ligament.
a. Components
i. Hepatic Ducts
o (1) Helps anchor esophagus to crural muscle fibers of
diaphgram; (2) Acts to limit upward and downward mobility of
ii. Bile Duct
iii. Gall Bladder
esophagus within the hiatus.
iv. Cystic Duct Tao anterosuperiorto E L ofaortichiatus
B. Esophageal Hiatus
b. Bile Flow
VI. Pancreas Located at T10; anterosuperior to, and to the left, of aortic hiatus.
a.
b.
Main Parts
Relations
Transmits: esophagus, vagal trunks, gastric nerves, esophageal
branches of the left gastric vessels, and some lymphatic vessels.
c. Ducts Has slight oblique long axis, bounded by muscle fibers that originate
d. Blood Supply, Venous and Lymphatic Drainage from medial part of right crus, forming a ‘chimney’, that
e. Nerve Supply accommodates the terminal part of the esophagus.
VII. Spleen
a. Relations C. Relations of the Abdominal Portion of the Esophagus
b. Peritoneal Ligament Anterior: Left lobe of the liver (posterior surface)
c. Blood Supply, Venous and Lymphatic Drainage
d. Nerve Supply
Posterior:oooLeft crus, left inferior phrenic vessels,
ooo ooo left greater and
lesser sphlanchnic nerves
deeply placedlying behind i lobe of theliver
joins PHARYNX STOMACH abt 10in
ESOPHAGUS I
continuousw ww.iacorieioeor isiom.cn
Anterior and Posterior: Left and Right vagi, respectively
A muscular, collapsible, tubular structure that joins that pharynx to
Tn gastro esophageal
D. Termination of the Esophagus junctiongastriccardiacorifice
the stomach about 10 in. (25cm). Ends at the gastro-esophageal junction/ gastric cardiac orifice,
Greater part lies within the thorax. Enters abdomen through an
Iopening in the1 right crus of the diaphragm.
at T11 vertebra, where it is continuous with cardiac orifice of
stomach.
Pierces diaphragm to the left of the midline and after 0.5 in (1.25 No anatomic sphincter exists at lower end of the esophagus.
physiologic sphincter. Tantra
cm) it enters the stomach on its right side.
Deeply placed, lying behind the left lobe of the liver.
Circular layer of smooth muscle in this region serves as the
gleft Closure of sphincter is under vagal control and can be augmented by
2 vagalcontrol
rainie
ggastrioxeinctributaryportaivein
astric artery closure
hormone ofsphincter
gastrin and reduced in response to secretin,
iigastric
nodes cholecystokinin, and glucagon.aoomenteoisygastrin
reauceainresponse
isecretin
1 of 11 ABDOMINAL PORTION OF THE ESOPHAGUS, STOMACH, DUODENUM & ACCESSORY GLANDS
[Bayas, Capalaran, Cruz, Garcia, Hitosis, Mayo, Olano, Sangca, Sarcia] 2cholecystokinin
3glucagon
3.04 ABDOMINAL PORTION OF THE ESOPHAGUS, STOMACH,
DUODENUM & ACCESSORY GLANDS
4. Rugae - Longitudinal folds of the stomach which flatten when the
stomach is distended
5. Visceral peritoneum - Completely surrounds the stomach
which leaves the lesser curvature at the lesser omentum and the
greater curvature as the gastrosplenic omentum and greater
omentum. The greater sac gives rise to the greater omentum.
ooo
Figure 2. Arteries that supply the stomach.
Note that all arteries are derived from branches of the celiac artery.
ESOPHAGUS
E. Blood Supply, Venous and Lymphatic Drainage
Blood Supply: Esophageal branches of the left gastric artery.
Venous Drainage: Left gastric vein, tributary of portal vein.
Lymph Drainage: Left gastric nodes
o Left gastric, left and right paracardial nodes, and from there to
oWEE
celiacESOPHAGEAL car
nodes. (According to Gray’s Anatomy
In lower esophageal cancer, lymph drains cranially to
mediastinal nodes. a
oo Left gastric nodes are also the lymphatic c drainage of the
stomach. Hence, cancer of the stomach may easily spread to
045 esophagus.0
o 7 YYfa9 nPYmpn
Incidencer of metastases to lymph nodes inchannels
carcinoma of the
esophagus ranges between 45% to 70%. Its anatomy and may
5
I sFm
physiology is important as to when and where to look for nodal
auoa.nm
o
spread.
Under this condition, lymph channels may be altered and thus aS sn.roeeniatoneai
metastatic spread may not follow the same pathways as lymph
s
flow under normal circumstances.
t.mnieasaaonon
Figure 3. Stomach
From 2017 Gross Anatomy Trans:
STOMACH
Which GIT organs are fixed in position?
The second to fourth parts of duodenum, as well as the
A. External and Internal Features ascending and descending colon, are retroperitoneal which
External features: make them fixed. The tranverse colon and sigmoid colon,
1. Fundus - Dome-shaped and project upward and bet.eyophagusandfunaus
to the left of the despite being intraperitoneal, is fixed due to the transverse
cardiac orifice. It is usually full of gas. There is a cardiac notch and sigmoid mesocolon, respectively. The remaining
intraperitoneal organs are mobile. The stomach is relatively fixed
between the esophagus and the fundus.
2. Body - Extends from the level of the cardiac orifice to the level of at both ends but is very mobile in between.
gaggifsterifftertatisfortate MACH
B. Relations
3.
incisura angularis.
Incisura angularis - Ang la n ch or angularis,” it is the notch Anteriorly: anterior abdominal wall, left costal margin, left pleura
in the lower part of the lesser curvature. and lung, diaphragm, left lobe of liver.
4.
iTEETaTTsT T
Pyloric antrum - Extends from the incisura angularis to the
_g
Posteriorly: lesser sac, diaphragm, spleen, left suprarenal gland,
5. saggy
pylorus.
Pylorus - Tubular part of the stomach which contains the pyloric
upper part of left kidney, splenic artery, pancreas, transverse
mesocolon, transverse colon.
sphincter; [Lies on the transpyloric plane, its position can be
recognized by a slight constriction on the surface of the stomach] structuresformingposterior
C. Stomach Bed
wall ofouews
altsorq.gg
6. Lesser curvature - Forms rag the right border of the stomach and
extends from the cardiac orifice to the pylorus. It is suspended Refers to structures upon which stomach rests in supine position
ga o Pancreas
7.
from the liver by the lesser omentum.
Greater curvature - Extends from the left of the cardiac orifice, o Spleen
3
Eateartainifthiffterton
over the dome of the fundus and along the left border of the o Left kidney
stomach to the pylorus o
o
Left suprarenal gland
Transverse colon and its mesocolon
putts
o Diaphragm
Internal features: Also refers to the structures forming the posterior wall of the
1. Pyloric sphincter - Anatomic and physiologic sphincter of
pylorus, it is the thick muscular wall of the pylorus.
omental bursa(lesser sac).
Foramen of Winslow–found behind the lesser omentum.
2. Pyloric Canal - Cavity of the pylorus It is found near the hepatoduodenal ligament.
3. Cardiac orifice - Where the esophagus enters the stomach
2 of 11 ABDOMINAL PORTION OF THE ESOPHAGUS, STOMACH, DUODENUM & ACCESSORY GLANDS
[THE WITTY TRANS GRP ]
3.04 ABDOMINAL PORTION OF THE ESOPHAGUS, STOMACH,
DUODENUM & ACCESSORY GLANDS
Left gastroepiploic artery from splenic artery) – Supplies the
upper part of greater curvature.
Right gastroepiploic artery (from gastroduodenal artery, a
branch of the hepatic artery) - Supplies the lower part of
greater curvature.
STOMACH
Venous Drainage portalcirculation
The veins drain into the portal circulation.
The left and right gastric veins drain directly to the portal vein.
The short gastric vein and left gastroepiploic vein drains e to the
splenic vein.
a
The right gastroepiploic vein drains to the superior mesenteric
vein.
EEE897889no
STOMACH snort node
gastric
Lymphatic Drainage
Lymph vessels follow the arteries into the left and right gastric
nodes, left and right gastroepiploic nodes, and short gastric nodes.
All lymph from the stomach eventually passes to the celiac nodes
located around the root of celiac artery on the posterior abdominal
wall.
paintransmittingnerve
E. Innervation of the Stomach
fibers
Sympathetic innervations from the celiac plexus.
The sympathetic innervation carries proportion of pain-
transmitting nerve fibers.
Parasympathetic innervations from the right and left vagus nerves.
o Serves secretomotor functions to the gastric glands, and
motor functions to the muscular wall of the stomach.
o In ulcer, vagotomy is done to depress the secretomotor
activity of the stomach. However, vagotomy leads to
gastroparesis ( stomach motility .
left
The anterior vagal trunk (formedvin agus
the thorax mainly from the
left vagus) enters the abdomen on the anterior surface of the
esophagus.
o Single or multiple trunks give off branches that supply the
Figure 4. Stomach Bed anterior surface of the stomach.
D. Blood Supply, Venous and Lymphatic Drainage STOMACH o A large hepatic branch passes up to the liver, and from
this, pyloric branch passes down to the pylorus.
right vagus
The posterior vagal trunk (formed in the thorax mainly from the
right vagus) enters the abdomen on the posterior surface of the
esophagus.
Divides into branches that supply mainly the posterior surface
o
of the stomach.
o A large branch passes to the celiac and superior
mesenteric plexuses, and is distributed to the intestine as
far as the splenic flexure and to the pancreas.
The pyloric sphincter receives motor fibers from the
sympathetic system, and inhibitory fibers from the vagi.
motorsympathetic
inhibitoryvagi
F. Omenta
Visceral peritoneum that completely surrounds the stomach.
o
o co
Leaves the lesser curvature to become the lesser omentum.
Leaves the greater curvature to become the greater
omentum.
colon
cgreatercurvaturetransverse
I Greater Omentum stomach another
a viscus
2-layered folds that connect the stomach to another viscus.
Connects the greater curvature of the stomach to the transverse
colon; It hangs down like an apron in front of the coils of the small
intestine and is folded back on itself to be attached to the transverse
colon
Figure 5. Blood supply and venous drainage of the stomach.
It controls the spread of infection (such as how it protects the
peritoneum incases ofruptured appendicitis)
Blood Supply
Left gastric artery (from celiac artery) - Supplies the lower
i gastricartery I 3rd of
LesserSuspends
Omentum
esophagus
third of the esophagus and upper
inrightof
right part of the stomach.
stomach
Right gastric artery (from hepatic
22
artery) - Supplies the lower right
the lesser curvature of the stomach from the fissure
of ligamentum venosum and the porta hepatis on the undersurface
part of the stomach.
r gastric artery drightpartof stomach
Short gastric arteries (from splenic artery) - Supply the fundus.
of the liver.
Extends to part of the duodenumand part of the liver.
snortgastric fundus
3 of 11artery
ABDOMINAL PORTION OF THE ESOPHAGUS, STOMACH, DUODENUM & ACCESSORY GLANDS
L gastroepiploicartery T great curvature
[THE WITTY TRANS GRP ]
R gastroepipcoicartery 1greatercurvature
3.04 ABDOMINAL PORTION OF THE ESOPHAGUS, STOMACH,
DUODENUM & ACCESSORY GLANDS
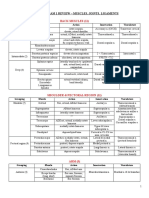
II. Second Part of the DuodenumL2 i3
G. Gastric Ulcer
Dr. Wong (Lifted from 2017 trans):What organs/artery will be Runs vertically downward in from of the hilum of right kidney on
the right side of 2 and 3 lumbar vertebra.
nd rd
affected by a gastric ulcer that penetrates the posterior wall? About halfway down its medial border, bile duct and main
pancreatic duct pierce the duodenal wall. They unite to form the
Gastric ulcers occur in the alkaline-producing mucosa of the ampulla that opens on the summit of the major duodenal papilla.
stomach (usually close to the lesser curvature)
An ulcer situated on the posterior wall of the stomach may
The accessory pancreatic duct, if present, opens into the duodenum
a little higher up on the minor duodenal papilla.
perforate into the lesser sac or become adherent to the
pancreas(producing pain referred to the back). Relations
The splenic artery runs along the upper border of the pancreas, Fundus of gallbladder, right lobe of liver, transverse
and erosion of this artery may produce fatal hemorrhage. Anterior colon, coils of small intestine
Vagotomy–performed to reduce the production of acid in cases of
chronic or recurring gastric ulcers. rare
Posterior Hilum of right kidney, right ureter
Truncal vagotomy– Surgical section of the vagal trunks; rarely Superiorly Ascending colon, right colic flexure, right lobe of liver
o
performed because the innervaton of the other gastric Inferiorly Head of the pancreas, bile duct, main pancreatic duct
structures are also sacrificed (i.e., can produce gastroparesis).
o Selective vagotomy- The stomach is denervated but the vagal
branches to the pylorus, liver, biliary ducts, intestines, and
celiac plexus are preserved (i.e., less gastroparesis).
It is better to give medication to ulcer patients at night,
because parasympathetic activity is very high at night (rest
and digest –Parasympathetic.
pylorus stomach iiwc.cajunction
SMALL INTESTINE
Longest part of the alimentary canal; extends from pylorus of
stomach to the ileocecal junction.
Greater part of digestion and food absorption takes place here.
Divided to three parts: duodenum, jejunum, ileum
c.sn
e89ugneumjejenum
ileum Figure 7. Anterior Relations of Duodenum
III. Third Part of the Duodenum
subcostalplane
Runs horizontally to the left on the subcostal plane, passing in front
of the vertebral column and following the lower margin of the head
of the pancreas.
Figure 6. Four Parts of the Duodenum.
A. DuodenumE.E.IE mm.minasnonsegment
IT
9ooimemmw Relations
Root of the mesentery of the small intestine, superior
C-shaped tube, about 10 in (25 cm), which joins stomach to jejunum. Anterior mesenteric vessels, coils of jejunum
It receives openings of bile and pancreatic ducts.
It curves around the head of the pancreas. Posterior
Right ureter, right psoas muscle,
inferior vena cava, aorta
Its first inch resembles the stomach in that it is covered on its
anterior and posterior surfaces with peritoneum. Superiorly Head of the pancreas
Has lesser omentum attached to its upper border and greater Inferiorly Coils of jejunum
omentum attached to its lower border; lesser sac (omental bursa)
lies behind this short segment.
The remainder of the duodenum is retroperitoneal, being partially
covered by peritoneum.It is situated in the epigastric and umbilical
regions. And is divided into four parts:
B. Divisions of the Duodenum
L1 I. First Part of the Duodenumpylorus s duodenalflexion
Most mobile; 5cm long; Begins at the pylorus and ends at the
aenaicap
superior deuodenal flexure; runs upward and backward on the
transpyloric plane at level of L1 vertebra.
Frequently referred to as the duodenal ‘cap’.
Relations
Anterior Quadrate of liver and Gallbladder
Lesser sac (first inch only), gastroduodenal artery,
Posterior
common bile duct, portal veins, inferior vena cava
Superiorly Entrance to lesser sac (epiploic foramen)
Inferiorly Head of the pancreas Figure 8. Posterior Relations of Duodenum
4 of 11 ABDOMINAL PORTION OF THE ESOPHAGUS, STOMACH, DUODENUM & ACCESSORY GLANDS
[THE WITTY TRANS GRP ]
3.04 ABDOMINAL PORTION OF THE ESOPHAGUS, STOMACH,
DUODENUM & ACCESSORY GLANDS
IV. Fourth Part of the DuodenumDoodenojyunal
flex un
Runs upward and to the left to the duodenojejunal flexure.
Posteriorly:
o Diaphragm
Flexure is held in position by a peritoneal fold, ligament of Right kidney
o o
Relations
µ
Treitz, which is attached to the right crus of the diaphragm. o
o
o
Hepatic flexure of the colon
Duodenum
Gallbladder
Anterior Beginning of the root of mesentery, coils of jejunum o Inferior vena cava
Esophagus
Posterior
Left margin of aorta,
o
o Fundus of the stomach
medial boarder of the left psoas muscle aitaoneato
p
aim minwantedgamment
B. Surfaces of the Liver
B. Blood Supply, Venous and Lymphatic Drainage Superior surface (Diaphragmatic surface)
Blood Supply: DUODENUM o Attached to diaphragm and anterior abdominal wall by the
o Upper half: Superior pancreaticoduodenal artery, a branch of triangular or falciform fold of peritoneum (falciform
the gastroduodenal artery. ligament)
o Lower half: Inferior pancreaticoduodenal artery, a branch of o In the free margin of the falciform ligament is a rounded cord,
the superior mesenteric artery. the ligamentum teres.
Venous Drainage:
o Superior pancreaticoduodenal vein drains into the portal vein
Inferior surface (Visceral surface)
o Uneven, concave, directed downwards, backwards, to the left
eat
o Inferior pancreaticoduodenal vein joins the superior o Is in relation with the stomach, duodenum, and right colic
mesenteric vein.
Lymphatic Drainage: o
flexure, right kidney, and suprarenal gland.
Marked with deep impressions (e.g., gastric, esoph, renal, colic)
o Lymph vessels follow arteries and rain upward via
O
pancreaticoduodenal nodes to the gastroduodenal nodes and
o Covered with visceral peritoneum except in the fossa of the
gallbladder and at the porta hepatis
then to the celiac nodes
a
Posterior surface caudate quadratelobes
o
0
Then downward via panreacticoduodenal nodes to the superior
mesenteric nodes around the origin of the superior mesenteric
o
o
Rounded, broad behind right lobe, but sharp/narrow on left.
Contains the caudate and quadrate lobes.
artery.
date
I. Porta Hepatisfoundposterone sur quadratelobe
Transverse fissure of the liver or hilum of the liver
o Found on the posteroinferior surface; between the caudate and
quadrate lobes.
o It is short but deep fissure extending transversely across the
under surface of the left portion of right lobe of liver, nearer to
its posterior surface than its anterior border.
o Joins nearly at right angles with the left sagittal fossa, and
separates the quadrate lobe in front from the caudate lobe and
process behind.
o Transmits:
Right and left hepatic duct [common hepatic duct accdg.
to Dr. Wong]
Right and left branches of hepatic artery [hepatic artery
proper accdg. to Dr. Wong]
3 Hepatic portal vein
Sympathetic and parasympathetic nerve fibers (hepatic
4 nerve plexus)
Figure 9. Arterial Supply of the Duodenum
BsHepatic
xD portal
Hepatic artery
vein g Lymphatic vessels
vein
LIVER
as
Largest visceral organ and the largest gland in the body.
Occupies the upper part of the abdominal cavity just below the
diaphragm.
The greater part of t.he liver is situated under cover of the right
costal margin
Right hemidiaphragm separatesliver it from the pleura, lungs,
am
pericardium, and heart.
Extends to the left to reach the left hemidiaphragm.
Has a bare area on the diaphragmatic surface, which is limited by
layers of the coronary ligament, but is devoid of peritoneum.
A. Relations of the Liver
Anteriorly:
o Diaphragm
Right and left costal margins
o
o Right and left pleura
Figure 10. Structures entering and leaving the Porta Hepatis
o Lower margins of both lungs
o Xiphoid process
o Anterior abdominal wall in the subcostal angle
C. Peritoneal Ligaments
Falciform Ligament
5 of 11 ABDOMINAL PORTION OF THE ESOPHAGUS, STOMACH, DUODENUM & ACCESSORY GLANDS
[THE WITTY TRANS GRP ]
3.04 ABDOMINAL PORTION OF THE ESOPHAGUS, STOMACH,
DUODENUM & ACCESSORY GLANDS
FalciformLIGAMENT
o Attaches liver to diaphragm and anterior abdominal wall
o 2-layered fold of peritoneum
o Ascends from umbilicus to liver; has sickle shaped free margin
that contains ligamentum teres (remains of umbilical vein)
Ligamentum Teres Hepatis (Round Ligament)
Remains of the left umbilical vein
o
o Lies in the free margin of the falciform ligament and ascends
from the umbilicus to the inferior (visceral)surface of the liver,
lying in the fissure that forms the left boundary of the quadrate
lobe of the liver,
o Passes into a fissure on the visceral surface and joins left
branch of portal vein in porta hepatis
Coronary Ligament
o Demarcates the margins of the bare area of the diaphragmatic
surface
o
o
R part: gives rise to R triangular ligament
L part: gives rise to L triangular ligament
Ligamentum Venosum
o Fibrous band
o Remains of ductus venosus
o Lies in the fissure on the inferior surface of the liver, forming
the left boundary of the caudate lobe of the liver
o Attached to left branch of portal vein & ascends in a fissure on
visceral surface to be attached above to inferior vena cava
Figure 11. Peritoneal ligaments
o May be continuous with the round ligament
Lesser Omentum (Hepatogastric Ligament) I. Anatomical Division
o Arises from the edges of porta hepatis & fissure for The liver may be divided into a large right lobe and a small left
ligamentum venosum
o Passes down the lesser curvature of stomach
lobe by the attachment of the peritoneum of the falciform
ligament.
Hepatoductal Ligament
o Attaches 1st part of duodenum to the liver
The right lobe is further divided into a quadrate lobe and a
caudate lobe by the presence of the following:
o Contains: o Gallbladder
9oaarateios
Portal vein
Hepatic artery
o Fissure for the ligamentum teres r.com
Bile duct
o Inferior vena cava aaaa
o Fissure for the ligamentum venosum
The quadrate and caudate lobes are a functional part of the left lobe
D. Divisions of the Liver
of the liver.
Important for surgeons performing lobectomies. Each segment has
its own vascular inflow, outflow, and biliary drainage. II. Functional Division
Right and left branches of the hepatic artery and portal vein, and the IVC to Gallbladder
right and left hepatic ducts are distributed to the right lobe and the In this division, the Caudate and Quadrate become part of Left lobe,
left lobe plus caudate and quadrate lobes, respectively. with the caudate division that separates the 2
o
h i_
Right lobe: right and left branches of the hepatic artery and
portal vein.
Each segment is further divided into superior and inferior areas
with caudate lobe divided into left and right part.
o
ire
Left lobe (plus caudate and quadrate lobes); right and left
hepatic ducts. Primary segments 10 segments
Lateral superior
Lateral
Lateral inferior
Medial superior
Medial
Medial inferior
Posterior superior
Posterior
Posterior inferior
Anterior superior
Anterior
Anterior inferior
Caudate superior
Caudate
Caudate inferior
6 of 11 ABDOMINAL PORTION OF THE ESOPHAGUS, STOMACH, DUODENUM & ACCESSORY GLANDS
[THE WITTY TRANS GRP ]
3.04 ABDOMINAL PORTION OF THE ESOPHAGUS, STOMACH,
DUODENUM & ACCESSORY GLANDS
The portal systemic anastomosis or porto-caval anastomosis that
occurs between veins of portal circulation and those of systemic
circulation
aka Portal-Systemic Anastomoses 1
I. Areas of Porto-Caval Anastomoses portal
systemicanastomosis
Specific type of anastomoses that occurs between the veins of portal
circulation and those of systemic circulation.
Significance:
o Under normal conditions, portal venous system blood
traverses liver and drains into inferior vena cava of systemic
venous circulation by way of the hepatic veins (direct route).
o However, small communication exists between the portal and
systemic systems, and becomes significant when the direct
route becomes blocked.
1. Lower third of the esophagus: esophageal branches of left gastric
vein (portal tributary) anastomose with esophageal veins draining
the middle third of esophagus into azygos veins (systemic tributary)
2. Halfway down the anal canal: superior rectal veins (portal
tributary) draining the upper half of the anal canal anastomose with
middle and inferior rectal veins (systemic tributaries), which are
tributaries of internal iliac and internal pudendal veins, respectively.
3. Paraumbilical veins – connect the left branch of the portal vein
Figure 12. Divisions of the liver with the superficial veins of the anterior abdominal wall (systemic
tributaries); the veins travel in the falciform ligament and
E. Blood Supply, Venous and Lymphatic Drainage of the Liver accompany the ligamentum teres.
Blood Supply 4. Veins of the ascending colon, descending colon, duodenum,
o Hepatic artery pancreas and liver (portal tributaries) anastomose with the
Branch of celiac artery renal, lumbar, and phrenic veins (systemic tributaries).
Divides into the right and left terminal branches that
enter the porta hepatis BILIARY APPARATUS
Venous Drainage Bile is secreted by liver cells at a constant rate of about 40 mL/ hr.
o Portal Vein When digestion is not taking place, the bile is stored and
Divides into the right and left terminal branches that concentrated in the gallbladder; later it is delivered to the
enter the porta hepatis behind the arteries duodenum to help in digestion.
o Hepatic veins
Emerge from the posterior surface of the liver
Drain into the inferior vena cava
Hepatic artery [30%] (oxygenated blood) or portal vein [70%]
(deoxygenated blood) -> liver sinusoids -> central vein each liver
lobule -> right and left hepatic veins -> posterior surface of the liver ->
inferior vena cava
The hepatic artery brings oxygenated blood to the liver and portal
vein brings venous blood rich in products of digestion which have been
absorbed in the GI tract.
When there is blockage in the portal vein, the portocaval anastomoses
serves as the passage.
Lymphatic Drainage
o Liver produces 1/3 to 1/2 of all body lymph
o Lymph vessels leave the liver and enter the lymph nodes in the
porta hepatis.
o The efferent vessels pass to the celiac nodes.
o A few vessels pass from the bare area of the liver through the
diaphragm to the posterior mediastinal lymph nodes.
Figure 13. Biliary Apparatus
F. Innervations
Innervations
A. Component Organs
o Sympathetic and parasympathetic nerves from celiac plexus
o Anterior vagal trunk rise to a large hepatic branch The bile ducts of the liver consist of:
o the right and left hepatic ducts,
G. Portal System o the common hepatic duct,
Is a system consisting of 2 capillary beds o the bile duct,
o Portal Venous System – when capillary beds pools into o the gallbladder,
another capillary bed through the heart o and the cystic duct.
Both capillary beds and blood vessels that connect them are
considered part portal system I. Hepatic Ducts
Examples are the hepatic portal system and the porto-caval The right and left hepatic ducts emerge from the right and left
anastomosis lobes of the liver in the porta hepatis (see Fig. 14).
7 of 11 ABDOMINAL PORTION OF THE ESOPHAGUS, STOMACH, DUODENUM & ACCESSORY GLANDS
[THE WITTY TRANS GRP ]
3.04 ABDOMINAL PORTION OF THE ESOPHAGUS, STOMACH,
DUODENUM & ACCESSORY GLANDS
After a short course, the hepatic duct unites to form the common Ampulla opens into the lumen of duodenum by small papilla
hepatic duct (see figure 15). (major duodenal papilla)
The common hepatic duct is about 1.5 in. (4 cm) long and descends
within the free margin of the lesser omentum. It is joined on the Terminal part of both ducts and the ampulla are surrounded by
right side by the cystic duct from the gallbladder to form the bile circular muscle (Sphincter of hepatopancreatic ampulla or
duct. Sphincter of Odi)
Occasionally, the bile and pancreatic ducts open separately into
the duodenum (see fig 16)
Figure 16. Three common variations of the bile and main
pancreatic ducts.
Figure 14. Right and Left haptis emerging from Porta hepatis
Figure 17. Bile duct lies in front of the right margin of portal
vein.
Figure 15. Common Hepatic Duct
I. Bile Duct
7 Common BileDuct
Also called as common bile duct.
About 3 inches or 8 cm long.
The common bile duct opens on the posteromedial (2nd) part of the
duodenum. It sometimes fuses with the pancreatic duct, forming a
common channel called the Ampulla of Vater.
Course:
(1st part) It lies in the right free margin of lesser omentum, in
front of the opening of the lesser sac (foramen of Winslow).
Lies in front of the right margin of the portal vein, on the right
side of hepatic artery (see fig 17).
Figure 18. Bile duct behind the first part of the duodenum.
(2nd part)It is situated behind the first part of duodenum (see
fig 18) to the right of gastroduodenal artery(see fig 19).
(3rd part)It lies in a groove on the posterior surface of the head
of pancreas, comes in contact with the main pancreatic duct
(Duct of Wirsung)(see fig 19)
CBD ends by piercing the medial wall of the 2nd part of the
duodenum almost halfway its length (joined by the main
pancreatic duct)
Both ducts open in a small ampulla in the duodenal wall
(Ampulla of Vater or hepatopancreatic ampulla)
Figure 19. Bile duct to the right of gastroduodenal artery.
8 of 11 ABDOMINAL PORTION OF THE ESOPHAGUS, STOMACH, DUODENUM & ACCESSORY GLANDS
[THE WITTY TRANS GRP ]
3.04 ABDOMINAL PORTION OF THE ESOPHAGUS, STOMACH,
DUODENUM & ACCESSORY GLANDS
The peritoneum completely surrounds the fundus and the
gallbladderand binds the body and neck to the visceral
surface.
Relations
Anterior Anterior Abdominal Wall, Inferior Surface of Liver
Posterior Transverse Colon, 1st and 2nd part of Duodenum
III. Cystic Duct
About 1.5 in. (3.8 cm) long and connects the neck of the gallbladder
to the common hepatic duct to form the bile duct. See figure 3.
It usually is somewhat S-shaped and descends for a variable
distance in the right free margin of the lesser omentum.
Mucous membrane is raise to form a spiral fold (“spiral valve” that
Figure 20. Bile duct comes into contact with the main pancreatic duct.
is continuous with a similar fold in the neck of the gall bladder. The
function of spiral valve is to keep the lumen constantly open.
B. Bile Flow
Hepatocytes Bile canaliculi interlobular biliary duct
collecting bile ducts which merge to form the right and left hepatic
ducts common hepatic duct cystic duct (to be stored in the gall
bladder) cystic duct (for excretion) common bile duct
duodenum excretion and enterohepatic circulation
Gallbladder cystic duct CBD duodenum
Figure 21. Bile duct ends in the duodenum halfway down its length. PANCREAS
It is both an exocrine and endocrine gland.
II. Gallbladder - exocrine: through ducts
It is a pear-shaped sac lying on the undersurface of the liver. - endocrine: directly through the blood
It has a capacity of 30 to 50 mL and stores bile, which it It is an elongated structure that lies in the epigastrium and the left
concentrates by absorbing water. upper quadrant.It is soft and lobulated and situated on the posterior
Function: abdominal wall behind the peritoneum (retropenial), behind the
o Stores bile which it concentrates by absorbing water. stomach, encircled by duodenum.
o Concentrates bile, excretes cholesterol and secretes mucus It crosses the transpyloric plane.
o Contracts in response to cholecystokinin, which is produced
by mucous membrane of duodenum on the arrival of fatty
food from the stomach
Figure 22. Location of Gallbladder
Blood Supply Cystic artery (branch of right hepatic artery)
Figure 23. Panreas
Venous drainage Cystic vein drains into portal vein
Function:
Lymph drainage Drains into cystic lymph node, situated near o Exocrine: (major part) produces secretion with enzymes
the neck of gallbladder capable of hydrolyzing proteins, fats and carbohydrates
Nerve Supply Sympathetic and parasympathetic vagal fibers o Endocrine: (islet of Langerhans) produces the hormones
from celiac trunk insulin and glucagon which play a role in carbohydrate metabolism
Divided into: A. Main Parts
o Fundus- rounded and projects below the inferior margin of
1. Head
the liver, where it comes in contact with the anterior
o Disc-shaped; located within the concavity of the duodenum
abdominal wall at the level of the tip of the 9th costal
o Right of midline, anterior and to right side of vertebral column
cartilage. o Uncinate process - a part that extends to the left, behind the
o Body- lies in contact with the visceral surface of the liver superior mesenteric vessels
and is directed upward, backward, and to the left. o Surfaces:
o Neck- becomes continuous with the cystic duct, which turns Anterior: Covered in peritoneum, related to origin of
into the lesser omentum to join the hepatic duct, to form the transverse colon
bile duct. See figure 19. Posterior: Related to inferior vena cava, right renal vein,
right crus, and usually the origin of right gonadal vein
9 of 11 ABDOMINAL PORTION OF THE ESOPHAGUS, STOMACH, DUODENUM & ACCESSORY GLANDS
[THE WITTY TRANS GRP ]
3.04 ABDOMINAL PORTION OF THE ESOPHAGUS, STOMACH,
DUODENUM & ACCESSORY GLANDS
2. Neck D. Blood Supply, Venous and Lymphatic Drainage
o Constricted portion of Pancreas Blood Supply:
o Most anterior portion of the gland; connects head to body o Splenic artery
o Lies in front of beginning of the portal vein and the origin of o Superior and inferior pancreaticoduodenal arteries
the superior mesenteric artery from the aorta Venous Drainage:
3. Body o Splenic Vein to the portal system
o Runs upward and to the left across the midline Lymphatic Drainage:
o Triangular in cross section; Becoming progressively thinner o Lymph nodes situated along the arteries that supply gland.
and less broad towards the tail. o The efferent vessels ultimately drain into the celiac and
4. Tail superior mesenteric lymph nodes
o Passes forward in the splenicorenal ligament
o Comes in contact with the hilum of the spleen
E. Nerve Supply
o Posteriorly related to the splenic branches of the splenic artery
and the splenic vein and its tributaries Sympathetic and parasympathetic (vagal) nerve fibers
B. Relations of the Parts SPLEEN
910,11rib
Anteriorly: (R to L): [TALS] It is reddish, the largest single mass of lymphoid tissue in the body.
Transverse colon It is oval shaped and has a notched anterior border.
Attachment of the transverse mesocolon It lies beneath left half of diaphragm close to 9th, 10th, and 11th rib
Lesser sac The long axis lies along the shaft of the 10th rib
Stomach Its lower pole extends forward only as far as the midaxillary line and
cannot be palpated on clinical examination
Posteriorly: (R to L): It is surrounded by peritoneum, which passes from it at the hilum as
Bile duct the gastrosplenic omentum (ligament) to the greater curvature of
Portal and splenic veins the stomach (carrying the short gastric and left gastroepiploic
Inferior vena cava vessels).
Aorta Functions:
Origin of the superior mesenteric artery o Removal of red blood cells - to remove any old red blood cells
Left psoas muscle o Part of immune response
Left suprarenal gland o Reservoir for blood
Left kidney o Erythropoiesis - fetus (9 to 28 week old)
Hilum of the spleen
C. Ducts
Main duct of the pancreas (Duct of Wirsung)
o begins in the tail and runs the length of the gland, receiving
numerous tributaries on the way
o opens into the 2nd part of the duodenum at about its middle
with the bile duct on the major duodenal papilla
o sometimes, the main duct drains separately into the duodenum
Accessory duct of the pancreas (Duct of Santorini)
o when present, drains the upper part of the head
o opens into the duodenum a short distance above the main duct
of the minor duodenal papilla
o frequently communicates with the main duct
Figure 25. Location of Spleen
A. Relations
Anteriorly:
Stomach
Tail of the pancreas
Left colic flexure
Left kidney (medial border)
** Hepatic Flexure – Right Colic Flexure
** Splenic Flexure – Left Colic Flexure
Posteriorly:
Diaphragm
Left pleura
Left lung
9th , 10th , 11th ribs
B. Peritoneal Ligaments
Figure 24. Panreatic Ducts
Two-layered folds of peritoneum that connects solid viscera to the
abdominal walls
10 of 11 ABDOMINAL PORTION OF THE ESOPHAGUS, STOMACH, DUODENUM & ACCESSORY GLANDS
[THE WITTY TRANS GRP ]
3.04 ABDOMINAL PORTION OF THE ESOPHAGUS, STOMACH,
DUODENUM & ACCESSORY GLANDS
a. Gastrosplenic omentum (ligament) TRANSER S MESSAGE
o contains the short gastric and left gastroepiploic branches of the
splenic artery; Attached to the greater curvature
o Two layers:
- Posterior layer: continuous with the peritoneum at the
splenic hilum and over the posterior aspect of the stomach.
- Anterior layer: formed from the peritoneum that is reflected
off the gastric impression and reaches the greater curvature
of the stomach anteriorly.
b. Splenicorenal ligament
o carries the splenic vessels and the tail of the pancreas
o attached to the left kidney
Figure 26. Peritoneal Ligaments
C. Blood Supply, Venous and Lymphatic Drainage GO 1D MR. & MS. MED!!
Blood Supply: Large splenic artery (largest branch of the celiac Go, break a Tibia, ika nga ni Yeeen!
artery) runs along the upper border of the pancreas and divides into
six branches which enter the spleen at the hilum.
Venous Drainage: Drained through the splenic vein which leaves
the hilum and runs behind the tail and body of the pancreas, where
it joins the superior mesenteric vein to the portal vein.
Lymphatic Drainage: Emerge from the hilum and pass through a
few lymph nodes along the course of the splenic artery and then
drain to the celiac nodes
D. Nerve Supply
Derived from the celiac plexus
Accompany the splenic artery
REFERENCES
Chung, K.W., & Chung, H.M. (2012). Board Review Series: Gross
Anatomy 7th edition. Wolters Kluwer Health/ Lippincott, Williams
and Wilkins.
Gray, H. (2005). Gray's Anatomy: The Anatomical Basis of Clinical
Practice. (40th ed.). Edinburgh: Elsevier Churchill Livingstone.
Snell, R.S. (2011). Clinical Anatomy by Regions. Wolters Kluwer
Health/ Lippincott, Williams and Wilkins
PLM CM Batch 2017 1B & 1D TRANS
11 of 11 ABDOMINAL PORTION OF THE ESOPHAGUS, STOMACH, DUODENUM & ACCESSORY GLANDS
[THE WITTY TRANS GRP ]
You might also like
- Renal Physiology NotesDocument6 pagesRenal Physiology Notescipa920% (1)
- Bipolar Disorder Mixed Episode Case StudyDocument14 pagesBipolar Disorder Mixed Episode Case Studyapi-658874568No ratings yet
- Abdomen Practice Exam - 1Document11 pagesAbdomen Practice Exam - 1Obinna Adolalom100% (1)
- Chapter 33, 36 - GuytonDocument8 pagesChapter 33, 36 - GuytonRoderick Palattao100% (3)
- Brachial PlexusDocument98 pagesBrachial PlexussandeepNo ratings yet
- Slides 01 UpperLimbAnatomy PickeringDocument33 pagesSlides 01 UpperLimbAnatomy Pickeringsparta oscar100% (1)
- Chapter 12: Heart: Functions of The HeartDocument12 pagesChapter 12: Heart: Functions of The Heartchristian anchetaNo ratings yet
- Anatomy and Physiology Lecture NotesDocument6 pagesAnatomy and Physiology Lecture NotesBlackcat KememeyNo ratings yet
- 2.bones of The Lower Limbs PDFDocument14 pages2.bones of The Lower Limbs PDFYahya Alkamali100% (1)
- Snell's Clinical Anatomy 1 - IntroductionDocument3 pagesSnell's Clinical Anatomy 1 - IntroductionAnna Dominique Jimenez50% (8)
- Blue Boxes For Head and NeckDocument11 pagesBlue Boxes For Head and NeckhajajyNo ratings yet
- Bones of Upper and Lower Limbs - RevisionDocument15 pagesBones of Upper and Lower Limbs - RevisionChess Nuts100% (1)
- St. Luke's College of Medicine - William H. Quasha Memorial: PhysiologyDocument3 pagesSt. Luke's College of Medicine - William H. Quasha Memorial: PhysiologyMavic Villanueva100% (1)
- Mnemonics Anatomy 1st SemDocument4 pagesMnemonics Anatomy 1st SemNastassja Callmedoctor Douse67% (3)
- ABS-Anatomy of The ThoraxDocument52 pagesABS-Anatomy of The ThoraxAtti Tamas100% (2)
- Special SensesDocument6 pagesSpecial SensesmasorNo ratings yet
- Anatomy of The AbdomenDocument107 pagesAnatomy of The AbdomenmichaelhossianNo ratings yet
- Anatomy Mnemonics PDFDocument31 pagesAnatomy Mnemonics PDFNonoy JoyaNo ratings yet
- MnemonicsDocument34 pagesMnemonicsAleena Stephen100% (2)
- St. Luke's College of Medicine - William H. Quasha Memorial: AnatomyDocument4 pagesSt. Luke's College of Medicine - William H. Quasha Memorial: AnatomyMavic VillanuevaNo ratings yet
- Abdominal Wall Edited WordDocument13 pagesAbdominal Wall Edited WordKennie RamirezNo ratings yet
- Gross Anatomy Learning Objectives - LimbsDocument8 pagesGross Anatomy Learning Objectives - Limbskep1313No ratings yet
- MTHISTO100 Lesson 2 Excretory SystemDocument9 pagesMTHISTO100 Lesson 2 Excretory SystemJaeri HuangNo ratings yet
- Pectoral Region QuestionsDocument14 pagesPectoral Region QuestionssizweNo ratings yet
- Regional Anatomy Question - FinalDocument8 pagesRegional Anatomy Question - FinalManju ShreeNo ratings yet
- Exam A-3Document11 pagesExam A-3yapues87No ratings yet
- Anatomical TermsDocument38 pagesAnatomical Termsrajni singhNo ratings yet
- Anatomy - NotesDocument149 pagesAnatomy - Noteshusayn12No ratings yet
- Anatomy Thorax-1Document25 pagesAnatomy Thorax-1zeeshanNo ratings yet
- Limbs 1b - Overview of Anatomy of Upper and Lower LimbsDocument5 pagesLimbs 1b - Overview of Anatomy of Upper and Lower LimbsTarmizi Md NorNo ratings yet
- Anatomy, Lecture 6, Pericardium and The Heart (Slides)Document22 pagesAnatomy, Lecture 6, Pericardium and The Heart (Slides)Ali Al-Qudsi100% (1)
- 15 CerebrumDocument32 pages15 CerebrumMédecin Adrian TGNo ratings yet
- Guyton Hall PHYSIOLOGY Chapter 1 PDFDocument3 pagesGuyton Hall PHYSIOLOGY Chapter 1 PDFOsman NazirNo ratings yet
- Anatomy Exam Review Muscles Innervations VasculatureDocument27 pagesAnatomy Exam Review Muscles Innervations Vasculaturegdubs215No ratings yet
- Anatomy LE2 Samplex 2017BDocument7 pagesAnatomy LE2 Samplex 2017BHanako Sasaki Aranilla100% (1)
- Upper Limbs NOTES - BRS Anatomy, Table of Muscles and BRS Questions With Answers ExplainedDocument14 pagesUpper Limbs NOTES - BRS Anatomy, Table of Muscles and BRS Questions With Answers ExplainedJustyna PoznanskaNo ratings yet
- Femoral TriangleDocument4 pagesFemoral TriangleHassan MohamedNo ratings yet
- St. Luke's College of Medicine - William H. Quasha Memorial: PhysiologyDocument6 pagesSt. Luke's College of Medicine - William H. Quasha Memorial: PhysiologyMavic Villanueva100% (1)
- 2.02 Gross Anatomy Trans - HeartDocument15 pages2.02 Gross Anatomy Trans - HeartElma Gonzales100% (1)
- Physiology: Guevara, Henaku-Larbi, Inciong, JutizDocument3 pagesPhysiology: Guevara, Henaku-Larbi, Inciong, JutizMavic VillanuevaNo ratings yet
- Muscle HistologyDocument50 pagesMuscle HistologyKhalid H MuseNo ratings yet
- Gross Anatomy CheatsheetDocument302 pagesGross Anatomy CheatsheetNobody2015100% (1)
- Subclavius Pectoralis Minor: Axial Skeleton To Shoulder Girdles (Ventral Side)Document6 pagesSubclavius Pectoralis Minor: Axial Skeleton To Shoulder Girdles (Ventral Side)馮素琴No ratings yet
- Circumflex Scapular: Dorsum of Thoracodorsal: Latissmus DorsiDocument4 pagesCircumflex Scapular: Dorsum of Thoracodorsal: Latissmus Dorsispeedy.catNo ratings yet
- By Prof. Saeed Abuel MakaremDocument25 pagesBy Prof. Saeed Abuel MakaremmahardikaNo ratings yet
- Anatomy Final ReviewDocument35 pagesAnatomy Final ReviewMarie100% (1)
- Upper LimbDocument22 pagesUpper LimbPing YangNo ratings yet
- Anatomy - Abdomen and PelvisDocument46 pagesAnatomy - Abdomen and PelvisDr.G.Bhanu PrakashNo ratings yet
- Lower Limb ReviewDocument24 pagesLower Limb ReviewRyan Silber100% (1)
- Lower LimbDocument6 pagesLower LimbYusri Arif100% (2)
- ABDOMEN & PELVIS NotesDocument12 pagesABDOMEN & PELVIS NotesNavaal AnjumNo ratings yet
- Human Anatomy Lecture Notes Update 2017Document58 pagesHuman Anatomy Lecture Notes Update 2017RAGHVENDRANo ratings yet
- Appendicular Worksheet With Answers ch.11Document7 pagesAppendicular Worksheet With Answers ch.11Alejandra ReynaNo ratings yet
- Anatomy Q-Bank: Thorax: December 2014Document57 pagesAnatomy Q-Bank: Thorax: December 2014Amisha YadavNo ratings yet
- (PHYSIO) 1.05 Autonomic Nervous System (EGBartolome)Document7 pages(PHYSIO) 1.05 Autonomic Nervous System (EGBartolome)Izza Mari DeLeon Laurio100% (2)
- Introduction To General AnatomyDocument7 pagesIntroduction To General AnatomyPia Abila100% (1)
- Anatomy TotalDocument19 pagesAnatomy TotalSnehanshNo ratings yet
- ANA Lab 4.01 Dissection of Abdominal Wall and Abdominal VisceraeDocument65 pagesANA Lab 4.01 Dissection of Abdominal Wall and Abdominal Visceraepattydump11No ratings yet
- (ANA) 4.01 Abdomen in General - Dr. ElevazoDocument22 pages(ANA) 4.01 Abdomen in General - Dr. ElevazopasambalyrradjohndarNo ratings yet
- Digestive SystemDocument7 pagesDigestive SystemKirsten CruzadoNo ratings yet
- Sustainable Energy Technologies and AssessmentsDocument14 pagesSustainable Energy Technologies and AssessmentsDaniel Yoshito IkejiriNo ratings yet
- Deploying A Portlet To Sun Java Portal Server: April 2006 (Revision Number: V2.1-1)Document10 pagesDeploying A Portlet To Sun Java Portal Server: April 2006 (Revision Number: V2.1-1)nyellutlaNo ratings yet
- Core 8Document13 pagesCore 8eleno m. estoqueNo ratings yet
- Power TransformerDocument78 pagesPower TransformerBhaanuj Anand100% (1)
- Narrative Podcasting Training ReportDocument8 pagesNarrative Podcasting Training ReportAna Maria CiobanuNo ratings yet
- Guide Acb UserDocument91 pagesGuide Acb UserCristianEnacheNo ratings yet
- TVL Bread & Pastry Production-Q1-M5Document15 pagesTVL Bread & Pastry Production-Q1-M5John Paul AnapiNo ratings yet
- Asme RimapDocument10 pagesAsme RimapDia Putranto HarmayNo ratings yet
- Convert TDMSDocument7 pagesConvert TDMSBhanupriya JainNo ratings yet
- 1354 Athlete Cardiac Arrests, Serious Issues, 922 of Them Dead, Since COVID Injection - Real ScienceDocument205 pages1354 Athlete Cardiac Arrests, Serious Issues, 922 of Them Dead, Since COVID Injection - Real ScienceHansley Templeton CookNo ratings yet
- Seminar Report: Hyperloop TrainDocument13 pagesSeminar Report: Hyperloop TrainKishan AvmNo ratings yet
- Cis HandoutDocument3 pagesCis HandoutMay-May BellecaNo ratings yet
- Aspects of Modern PoetryDocument6 pagesAspects of Modern Poetrymumin jamalNo ratings yet
- Acl 2015 HandbookDocument225 pagesAcl 2015 HandbookShu-Kai HsiehNo ratings yet
- T Eco H P II: HE Istogram ARTDocument8 pagesT Eco H P II: HE Istogram ARTKovacs ImreNo ratings yet
- Permutation and Combination: Name - Tuhin Nayak Class - XI A' Roll No. - 29Document8 pagesPermutation and Combination: Name - Tuhin Nayak Class - XI A' Roll No. - 29Tuhin NayakNo ratings yet
- Paper Sticking To PlateDocument2 pagesPaper Sticking To PlateRocio RodriguezNo ratings yet
- EM g7 Maths 2021 WP 3rdDocument10 pagesEM g7 Maths 2021 WP 3rdNikila WeerasingheNo ratings yet
- Logical Reasoning TestsDocument7 pagesLogical Reasoning Testsls-checkinNo ratings yet
- Ngsmips BrochureDocument21 pagesNgsmips BrochureSaroja RajuNo ratings yet
- Selection and Training of Sales ForceDocument23 pagesSelection and Training of Sales ForceSelena Torres67% (3)
- Dbms 2021Document74 pagesDbms 2021andiNo ratings yet
- Civil Service Commission Professional or Sub DwawdawdawdreviewerDocument99 pagesCivil Service Commission Professional or Sub DwawdawdawdreviewerHarey PatarNo ratings yet
- Audiovisual TouringBrochure SLAMLexDocument44 pagesAudiovisual TouringBrochure SLAMLexantonioNo ratings yet
- Inspiration-To-Go Ebooks For You: The Magic StoryDocument15 pagesInspiration-To-Go Ebooks For You: The Magic StoryraostoreNo ratings yet
- Designation: D6496/D6496M - 20: Date: To: Tech Contact: Work Item #: Ballot ActionDocument2 pagesDesignation: D6496/D6496M - 20: Date: To: Tech Contact: Work Item #: Ballot ActionEdward Carhuanina LescanoNo ratings yet
- 2014 Mrcs Osce RECALLDocument85 pages2014 Mrcs Osce RECALLIdo EgaziNo ratings yet
- Francois Lelord - Cum Sa Te Iubesti Pe TineDocument28 pagesFrancois Lelord - Cum Sa Te Iubesti Pe TineSasu NicoletaNo ratings yet
- Thesis Chapter 2 Review of Related Literature and StudiesDocument4 pagesThesis Chapter 2 Review of Related Literature and Studieslizaschmidnaperville100% (2)