Host-Pathogen Interaction in Invasive Salmonellosis: Plos Pathogens October 2012
Host-Pathogen Interaction in Invasive Salmonellosis: Plos Pathogens October 2012
Uploaded by
Alif RahmanCopyright:
Available Formats
Host-Pathogen Interaction in Invasive Salmonellosis: Plos Pathogens October 2012
Host-Pathogen Interaction in Invasive Salmonellosis: Plos Pathogens October 2012
Uploaded by
Alif RahmanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Host-Pathogen Interaction in Invasive Salmonellosis: Plos Pathogens October 2012
Host-Pathogen Interaction in Invasive Salmonellosis: Plos Pathogens October 2012
Uploaded by
Alif RahmanCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/232232512
Host–Pathogen Interaction in Invasive Salmonellosis
Article in PLoS Pathogens · October 2012
DOI: 10.1371/journal.ppat.1002933 · Source: PubMed
CITATIONS READS
147 2,307
4 authors, including:
Hanna K de Jong
Academisch Medisch Centrum Universiteit van Amsterdam
30 PUBLICATIONS 427 CITATIONS
SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Host response to melioidosis View project
All content following this page was uploaded by Hanna K de Jong on 13 April 2015.
The user has requested enhancement of the downloaded file.
Review
Host–Pathogen Interaction in Invasive Salmonellosis
Hanna K. de Jong1,2, Chris M. Parry3,4, Tom van der Poll1,2,5, W. Joost Wiersinga1,2,5*
1 Center for Infection and Immunity Amsterdam (CINIMA), Academic Medical Center, Amsterdam, the Netherlands, 2 Center for Experimental and Molecular Medicine
(CEMM), Academic Medical Center, Amsterdam, the Netherlands, 3 Mahidol-Oxford Tropical Medicine Research Unit, Faculty of Tropical Medicine, Mahidol University,
Bangkok, Thailand, 4 Centre for Tropical Medicine, Nuffield Department of Clinical Medicine, Churchill Hospital, University of Oxford, Oxford, United Kingdom,
5 Department of Medicine, Division of Infectious Diseases, Academic Medical Center, Amsterdam, the Netherlands
disease [2]. S. Typhi is an exclusively human pathogen causing a
Abstract: Salmonella enterica infections result in diverse bacteremic disease that, unlike many other Gram-negative
clinical manifestations. Typhoid fever, caused by S. bacteremias, does not typically manifest with neutrophilia or
enterica serovar Typhi (S. Typhi) and S. Paratyphi A, is a septic shock [3]. The widespread appearance of antimicrobial-
bacteremic illness but whose clinical features differ from resistant strains has limited treatment options [4,5]. Relapse and
other Gram-negative bacteremias. Non-typhoidal Salmo- chronic asymptomatic fecal carriage may complicate the illness
nella (NTS) serovars cause self-limiting diarrhea with
(Figure 1) [6,7]. Mortality usually results from intestinal perfora-
occasional secondary bacteremia. Primary NTS bacteremia
can occur in the immunocompromised host and infants in tion and peritonitis or from a severe toxic encephalopathy
sub-Saharan Africa. Recent studies on host–pathogen associated with myocarditis and hemodynamic shock [8].
interactions in Salmonellosis using genome sequencing, Infections with non-typhoidal Salmonella (NTS) serovars, such as
murine models, and patient studies have provided new S. enterica serovar Typhimurium and S. Enteriditis, also cause a
insights. The full genome sequences of numerous S. significant disease burden, with an estimated 93.8 million cases
enterica serovars have been determined. The S. Typhi worldwide and 155,000 deaths each year (see [9] for review) [10].
genome, compared to that of S. Typhimurium, harbors NTS serovars usually cause self-limiting diarrhea with secondary
many inactivated or disrupted genes. This can partly bacteremia occurring in less than 10% of patients. The host range
explain the different immune responses both serovars of non-typhoidal Salmonella serovars is broad, including poultry and
induce upon entering their host. Similar genome degra- cattle, and NTS infection is commonly due to food poisoning in
dation is also observed in the ST313 S. Typhimurium strain developed countries. NTS serovars cause high rates of bacteremia
implicated in invasive infection in sub-Saharan Africa. in the immunocompromised and, in sub-Saharan Africa, in
Virulence factors, most notably, type III secretion systems, children below 5 years old and those with HIV infection [9,11].
Vi antigen, lipopolysaccharide and other surface polysac-
Antimicrobial resistance is widespread [12].
charides, flagella, and various factors essential for the
intracellular life cycle of S. enterica have been character- The variations in the clinical features of infection with this
ized. Genes for these factors are commonly carried on intracellular pathogen relate to differences in the interaction
Salmonella Pathogenicity Islands (SPIs). Plasmids also carry between different Salmonella serovars and the host. This review
putative virulence-associated genes as well as those summarizes new and significant insights concerning the virulence
responsible for antimicrobial resistance. The interaction factors of both typhoid and non-typhoidal Salmonellae, their
of Salmonella pathogen-associated molecular patterns difference at the genome level, novel mechanisms employed by
(PAMPs) with Toll-like receptors (TLRs) and NOD-like these intruders to circumvent the host defense, and their
receptors (NLRs) leads to inflammasome formation, interactions with both host microbiome and the innate immune
activation, and recruitment of neutrophils and macro- system.
phages and the production of pro-inflammatory cyto-
kines, most notably interleukin (IL)-6, IL-1b, tumor necrosis
factor (TNF)-a, and interferon-gamma (IFN)-c. The gut
microbiome may be an important modulator of this
immune response. S. Typhimurium usually causes a local
intestinal immune response, whereas S. Typhi, by Citation: de Jong HK, Parry CM, van der Poll T, Wiersinga WJ (2012) Host–
preventing neutrophil attraction resulting from activation Pathogen Interaction in Invasive Salmonellosis. PLoS Pathog 8(10): e1002933.
of TLRs, evades the local response and causes systemic doi:10.1371/journal.ppat.1002933
infection. Potential new therapeutic strategies may lead Editor: Chetan E. Chitnis, International Centre for Genetic Engineering and
from an increased understanding of infection pathogen- Biotechnology, India
esis. Published October 4, 2012
Copyright: ß 2012 de Jong et al. This is an open-access article distributed
under the terms of the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided the
original author and source are credited.
Introduction
Funding: W.J. Wiersinga is supported by the Netherlands Organisation of
Typhoid fever is a global problem, with more than 27 million Scientific Research (VENI grant) and the Netherlands Organisation for Health
Research and Development (Clinical Fellowship grant). C.M. Parry is supported by
cases worldwide each year resulting in an estimated 217,000 the Wellcome Trust as part of the Wellcome Trust–Mahidol University–Oxford
deaths [1]. Salmonella enterica serovar Typhi (S. Typhi) and S. Tropical Medicine Research Programme. The funders had no role in study design,
Paratyphi A are the Gram-negative bacteria that cause this data collection and analysis, decision to publish, or preparation of the manuscript.
debilitating condition. It is most common among children, Competing Interests: The authors have declared that no competing interests
especially in areas of Asia and Africa that lack clean water and exist.
adequate sanitation, and is also an important travel-associated * E-mail: w.j.wiersinga@amc.uva.nl
PLOS Pathogens | www.plospathogens.org 1 October 2012 | Volume 8 | Issue 10 | e1002933
Figure 1. Dissemination of S. Typhi during systemic infection. Typhoid is usually contracted by ingestion of food or water contaminated by
fecal or urinary carriers excreting S. Typhi. The incubation period is usually 7 to 14 d. In the small intestine the bacteria adhere to the mucosa and then
invade the epithelial cells. The Peyer’s patches, which are aggregrated lymphoid nodules of the terminal ileum, play an important role in the transport
to the underlying lymphoid tissue. Specialized epithelial cells such as M cells overlying these Peyer’s patches are probably the site of internalization of
S. Typhi. Once the bacteria have penetrated the mucosal barrier, the invading organism translocates to the intestinal lymphoid follicles and the
draining mesenteric lymph nodes, and some pass on to the reticuloendothelial cells of the liver and spleen. During the bacteremic phase, the bacteria
are widely disseminated throughout the body. Secondary infection can occur with liver, spleen, bone-marrow, gallbladder, and Peyer’s patches as the
most preferred sites. The gallbladder is the main reservoir during a chronic infection with S. Typhi and invasion occurs either directly from the blood
or by retrograde spread from the bile. Of interest, the ability of Salmonella to form biofilms on gallstones is likely to be a critical factor in
establishment of chronic carriage and shedding of S. Typhi [88]. The bacteria that are excreted in the bile can then reinvade the intestinal wall by the
mechanism previously described or are excreted by feces. Typical clinical symptoms are fever, malaise, and abdominal discomfort. Clinical features
such as a tender abdomen, hepatomegaly, splenomegaly, and a relative bradycardia are common. Rose spots, the classical skin lesions associated
with typhoid fever, are relatively uncommon and occur in 5%–30% of cases. The most severe manifestations of typhoid leading to sepsis and death
are either necrosis of the Peyer’s patches resulting in gut perforation and peritonitis or a toxic encephalopathy associated with myocarditis and
haemodynamic shock [8,89].
doi:10.1371/journal.ppat.1002933.g001
The Bacteria ago [17]. The sequence-based technique of MLST (multilocus
sequence typing) provides a more accurate indication of the
Taxonomy and Genomics of Salmonella genomic relationship between different Salmonella isolates and may
The genus Salmonella is composed of two distinct species: supersede serotyping in the future [18]. Of the ,4,000 S. Typhi
Salmonella bongori and Salmonella enterica, the latter being divided into genes, more than 200 are functionally disrupted or inactive, while
six subspecies. These subspecies are classified into more than 50 most of these homologs are still fully functional in S. Typhimur-
serogroups based on the O (somatic) antigen, and divided into ium. This could in part explain the restricted host range of S.
.2,400 serovars based on the H (flagellar) antigen. Complete Typhi [16]. Although it has been suggested that the different
genome sequence from multiple Salmonella strains are available clinical outcomes of infection between typhoid and NTS serovars
[13]. For example, the S. Typhi type strain Ty2, the multidrug- may be explained by differences in genome expression leading to
resistant (MDR) isolate CT18, and the S. Typhimurium strain differences in host-pathogen recognition, one should also consider
LT2 are composed of 4.79 (Ty2), 4.86 (CT18), and 4.81 (LT2) the opposite possibility; that is, differences in host-pathogen
megabases, respectively [14–16]. The core genomes of Escherichia interaction may make certain genes dispensable, resulting in the
coli and S. enterica differ by only 10% in their DNA sequences and accumulation of pseudogenes [3,19,20].
suggest that the two species derived from a common ancestor Recent analysis of S. Typhimurium isolates from the unusually
about 100 million years ago. Comparison of different S. Typhi invasive infections seen in sub-Saharan Africa have shown
isolates show that they are highly related (clonal) and have arisen dominance of a particular MLST type, ST313, distinct from the
from a single point of origin approximately 30,000–50,000 years usual S. Typhimurium sequence type, ST19, associated in other
PLOS Pathogens | www.plospathogens.org 2 October 2012 | Volume 8 | Issue 10 | e1002933
parts of the world with diarrhea. In the D23580 invasive S. the spv genes. The spvB enzyme, which acts as an intracellular
Typhimurum isolate from Malawi, there is loss of gene function, ADP-ribosylating toxin causing host cytotoxicity, is necessary for
including genes previously implicated in the virulence of S. intra-macrophage survival but is absent in S. Typhi and S.
Typhimurium in the murine model of infection, such as sseI Paratyphi A [20,23]. Putative virulence-associated plasmid has
(encoding a type III-secreted effector protein) and ratB (encoding a only recently been identified in S. Typhi. The chimeric plasmid
secreted protein associated with intestinal persistence), and of the pR(ST98) carries genes that are involved in drug resistance and
44 novel pseudogenes or deletions in the strain relative to LT2, 26 apoptosis induction in macrophages [24,25]. Additionally, a linear
are also pseudogenes or deletions in S. Typhi or S. Paratyphi A plasmid in S. Typhi strains originating from Indonesia, called
[21]. These observations suggest that a similar process of adaption pBSSB1, carries the fljBz66 gene, which encodes a flagellin antigen
to the human host may be occurring in African S. Typhimurium as known as H:z66 [26]. Whether the presence of these particular
has been observed in S. Typhi. plasmids has an impact on the virulence of S. Typhi is not known.
The role of plasmids carrying antimicrobial resistance genes,
Virulence Factors such as cat, dhfr7, dhfr14, sul1, and blaTEM-1, in the transfer and
About 90% of the genes in S. Typhi and S. Typhimurium spread of antimicrobial resistance has been well described [20,27].
serovars are identical [16]. The 10% of genes that differ include S. Typhi is able to exchange multidrug resistance R-plasmids with
virulence factors, which determine their pathogenic potential E. coli and other enteric bacteria [28,29]. The self-transmissible
(Figure 2) [20]. The virulence factors of the Salmonella serovars are incompatibility group (Inc)HI1 plasmids almost exclusively confer
mostly encoded on the Salmonella pathogenicity islands (SPI). the phenotype of MDR S. Typhi. The presence of the MDR
Plasmids and prophages. Integrated bacteriophages, phage phenotype has been suggested to be associated with the
remnants, or plasmids are single- or double-stranded DNA development of severe or fatal disease [30,31]. The presence of
molecules that can be exchanged between bacteria by horizontal a composite genetic element encoding multiple antimicrobial
gene transfer. They give bacteria the opportunity to pass on or resistance genes on the virulence-associated plasmid in the ST313
receive selected genes that may enhance virulence or result in serovar Typhimurium isolates causing invasive disease in Africa
antimicrobial resistance [17,22]. Certain Salmonella spp. have a may provide an explanation for a linkage between drug resistance
self-transmissible virulence plasmid called pSLT, which harbors and an invasive phenotype [21]. Prophages and phage remnants
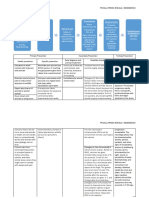
Figure 2. Virulence of S. Typhimurium and S. Typhi. S. Typhimurium and S. Typhi possess partly overlapping and a partly distinct repertoire of
virulence factors. Both serovars express the type III secretion system, lipopolysaccharide, and other surface polysaccharides, fimbrae, flagellin, and
bacterial DNA. The Vi antigen is exclusively expressed by S. Typhi and is able to circumvent the innate immune response by repressing flagellin and
LPS expression. SPI, Salmonella pathogenicity islands.
doi:10.1371/journal.ppat.1002933.g002
PLOS Pathogens | www.plospathogens.org 3 October 2012 | Volume 8 | Issue 10 | e1002933
can carry non-essential ‘‘cargo’’ genes involved in bacterial inflammatory responses [39]. However, S. Typhimurium mutants
virulence including several type III secretion system effectors, deficient in SPI-1 can disseminate and cause systemic infection
which play an important role in Salmonella virulence [20,32]. from the gastrointestinal tract by CD-18 expressing phagocytic
Type III secretion system and outer membrane cells such as dendritic cells (DCs) without disrupting the epithelial
vesicles. Salmonella enterica spp. contains two type III secretion barrier [40,41]. Therefore, this alternative pathway via CD-18
system (T3SS) gene clusters encoding a secretion apparatus that immune cells facilitates the development of a systemic infection for
functions like a molecular syringe. The T3SS secretes effector intracellular-adapted bacteria like Salmonella. T3SS2, encoded on
proteins into the target-cell cytosol, which manipulate host-cell SPI-2, plays a crucial role during the second phase of invasion,
signaling cascades. These effector proteins are suggested to have intracellular survival in macrophages [42]. Within the phagocyte,
multiple activities within host cells; for example, SopB is involved T3SS2 prevents trafficking from the phagocyte NADPH oxidase
in invasion and Akt activation, which causes fluid secretion and (nicotinamide adenine dinucleotide phosphate-oxidase) towards
Salmonella containing vacuole (SCV) formation (Figure 3a) [33–36]. the SCV, thereby preventing a phagocytic burst [43,44]. Although
The majority of genes encoding for these virulence-associated the importance of these systems for the virulence of S.
effector molecules are located on the SPIs. Other effector proteins Typhimurium is clear, limited data are available concerning the
such as SopE, SspH1, SseI, SodC-1, and SopE2 are encoded by role of T3SS in S. Typhi. Of note, the SPI-2 T3SS of S. Typhi is
phages or phage remnants [22,37,38]. not required for survival in human macrophages but may be used
Of the 21 SPIs known to date, SPI-1 and SPI-2 are the most during infection of other cell types, such as DCs or natural killer
studied. S. Typhimurium and S. Typhi genomes share 11 common cells, leading to the notion that the SPI-2 T3SS may be required to
SPIs; four are specific to S. Typhi (SPI-7, 15, 17, and 18) and only modulate the host immune system to establish long-term
one (SPI-14) for S. Typhimurium [20]. SPI-1 harbors the genes for asymptomatic infection [45].
T3SS1, which is crucial for the invasion of non-phagocytic cells Bacterial outer membrane vesicles (OMV) have been recently
such as M cells in the gut lumen and activation of pro- identified as another method used by Salmonella to transfer its
Figure 3. Salmonella and its first encounter with the host. (a) The intracellular life of Salmonella. Invasion of phagocytic and non-phagocytic
cells. Salmonella is a facultative intracellular pathogen that can be found in a variety of phagocytic and non-phagocytic cells, in which it is able to
survive and replicate. To establish this intracellular niche, the T3SS1 and -2 play a predominant role; key virulence factors are involved in accessing
and utilizing these cells [36]. After ingestion, intestinal colonization follows and Salmonella enters enterocytes and dendritic cells in the intestinal
epithelium [36]. Subsequently, Salmonella that reach the submucosa can be internalized by resident macrophages via different mechanisms: by
phagocytosis, active invasion using the T3SS1 or T3SS1-independent invasion using fimbriae or other adhesins on the bacterial surface. (1)
Salmonella-containing-vacuole. Following internalization Salmonella remains within a modified phagosome known as the Salmonella containing
vacuole (SCV) and injects a limited number of effector proteins, such as SipA, SipC, SopB/SigD, SodC-1, SopE2, and SptP into the cytoplasm. These
effectors cause rearrangements of the actin cytoskeleton and SCV morphology among other changes. (2) Replication within the SCV. Salmonella
survives and replicates within the SCV, where it is able to avoid host antimicrobial effector mechanisms. The T3SS2 is required for systemic virulence
in the mouse and survival within macrophages. (3) Transport of Salmonella to distant sites. After penetration of the M cells, the invading
microorganisms translocate to the intestinal lymphoid follicles and the draining mesenteric lymph nodes, and some pass on to the
reticuloendothelial cells of the liver and spleen. Salmonella organisms are able to survive and multiply within the mononuclear phagocytic cells
of the lymphoid follicles, liver, and spleen [36]. (b) Host–pathogen interaction in typhoid and non-typhoid Salmonella. Simplified scheme of the first
encounter between Salmonella spp. and the immune system. Specified cells such as neutrophils, macrophages, dendritic, phagocytic, and epithelial
cells recognize specific pathogen associated molecular patterns (PAMPs) and danger-associated-molecular patterns (DAMPs), thereby eliciting an
immune response. PAMPs such as LPS, Flagella, and bacterial DNA can trigger TRL4, TRL5, and TRL9, respectively. TLR-induced activation of NF-kB is
essential for the production of pro-IL-1b, pro-IL-18, which can be negatively regulated by IRAK-M [90]. The NLRs are situated in the cytosol and can
also recognize PAMPs. However, NLRP3 is triggered by a different, yet unknown, mechanism, although DAMPs are thought to play a crucial role. TLR,
toll-like receptors; LPS, lipopolysaccharide; NF-kB, regulated nuclear factor kappa-light-chain-enhancer of activated B cells; IRAK-M, IL-1R-assiociated
kinase-M; IL, Interleukin; ASC, apoptotic speck protein containing a caspase recruitment domain; NLR, NOD-like receptors (including NLRP3 and
NLRC4); MyD88, myeloid differentiation primary response gene [88].
doi:10.1371/journal.ppat.1002933.g003
PLOS Pathogens | www.plospathogens.org 4 October 2012 | Volume 8 | Issue 10 | e1002933
virulence factors into the cytoplasm of the host cell [46]. For patients with systemic infections caused by other Gram-negative
example, S. Typhi uses the OMV to enclose ClyA, a pore-forming bacteria [60,62]. Patients with typhoid fever demonstrate a
cytotoxin, and subsequently release this virulence factor extra- distinct and highly reproducible signature in the peripheral blood,
cellulary [47]. Moreover, it has also been shown that OMVs can shown by micro-arrays and transcriptional profiling, that changes
stimulate responses important for the activation of DCs, priming during treatment and convalescence, returning in the majority of
Salmonella-specific T and B cells, and possess pro-inflammatory and cases to a normal profile as measured in healthy uninfected
antigenic function, which makes them therefore attractive as controls [63]. Patients who do return to a normal profile may be
vaccine candidates [48]. genetically or temporarily incapable of developing an effective
Fimbrae and flagella. Fimbriae or pili are found on the immune response and may be more susceptible to re-infection,
bacterial surface and are thought to be mainly important for relapse, or the establishment of a carrier state [63]. In this respect
biofilm formation, colonization, and initial attachment to the host it is of importance to note that antimicrobial treatment—which
cells, although little is known about their true virulence potential can lead to depletion of the gut microbiome—is associated with
[20,36]. Each Salmonella serovar harbors a unique combination of prolonged deleterious effects on intestinal Salmonella colonization
fimbrial operons. Flagella are long helical filaments attached to resistance, which can result in increased fecal shedding and
rotary motors embedded within the membrane that enable carrier status (Box 1) [69]. In contrast to NTS, which is an
Salmonella species to travel to the epithelial barrier after ingestion. important cause of morbidity and mortality in patients with an
In vitro, flagellin causes upregulation of pro-inflammatory inherited or acquired immunodeficiency syndrome such as HIV
cytokines in tissue culture models [49]. However, in vivo data infection, IL-12R deficiency, or chronic granulomatous disease,
showed that the role of flagella in virulence can be dispensable and typhoid fever has not been associated with any primary or
model-dependent [50–52]. acquired immunodeficiency or underlying disease [9,70,71]. Such
Polysaccharides and other putative virulence factors. The a difference can potentially be ascribed to a difference in
polysaccharidic capsule Vi antigen is of key importance for S. signaling through PRRs where production of interleukin-17-
Typhi virulence, but notably absent in S. Typhimurium, S. producing T cells and their associated family cytokines (IL-17,
Paratyphi A, and most other Salmonella serovars. Its presence -21, -22, -26) play an important role in the dissemination of NTS
increases infectivity of S. Typhi and disease severity, and natural but not S. Typhi [9].
infection is usually associated with the expression of Vi antigen in
isolated S. Typhi [53]. However, Vi negative mutants are still Pattern Recognition Receptors
able to cause a typhoid-like illness in human volunteers [54]. Two Salmonella spp. expresses multiple PAMPs, most notably T3SS,
widely separated chromosomal regions, ViaA together with ViaB, flagella, fimbrae, LPS (Vi antigen), and bacterial DNA, which are
located on SPI-7, are needed for Vi synthesis [55]. Recently it has recognized by PRRs (Figure 2). Not surprisingly, TLR4 plays an
been hypothesized that the Vi capsule can prevent host-pathogen important role in invasive Salmonellosis. TLR4-deficient mice
recognition by preventing lipopolysaccharide (LPS) recognition
by pattern recognition receptors (PRRs) [56]. In this way S.
Typhi does not elicit a neutrophil influx in the small bowel but is
able to disseminate systemically and lead to a persistent bacterial Box 1. Salmonella and the Gut Microbiome
infection [3]. Other well-documented virulence factors include
In recent years it has become clear that the intestinal
ion transporters and superoxide-dismutases [36].
microbiome, consisting of more bacteria than the total
number of cells in the human body, can be seen as an
The Host Defense exteriorised organ that exerts numerous functions in the
host response against Salmonellosis. The gut hosts
PRRs, most notably the Toll-like receptors (TLR) and NOD-
,161014 bacteria from 500–1,000 different species of
like receptors (NLR), are the first component of the immune
which three bacterial divisions—the Firmicutes (Gram-
system to detect host invasion by pathogens, initiate immune positive), Bacteroides (Gram-negative), and Actinobacteria
responses, and form the crucial link between innate and adaptive (Gram-positive)—dominate. The healthy gut microbiome
immunity [57,58]. PRRs recognize conserved motifs on pathogens can protect against epithelial cell injury by producing toxic
termed ‘‘pathogen-associated-molecular-patterns’’ (PAMPs) and metabolites known to repress Salmonella virulence gene
are also able to recognize endogenous danger signals or ‘‘danger- expression, optimizes host immune systems, and mediates
associated molecular-patterns’’ (DAMPs). During invasive Salmo- pathogen clearance from the gut lumen after non-
nella infection, PAMPs and DAMPs initiate the innate immune typhoidal Salmonella diarrhea [69,91]. Of importance,
system leading to activation and recruitment of neutrophils and antimicrobial treatment depletes the gut microbiome
macrophages and the production of pro-inflammatory cytokines, and is associated with prolonged deleterious effects on
most notably Interleukin (IL)-6, IL-1b, tumor necrosis factor intestinal Salmonella colonization resistance, which can
(TNF)-a, and interferon-gamma (IFN)-c (Figure 3b) [59–65]. IFN- result in increased fecal shedding and carrier status
c plays a central role in the control of persistent infection by induction [69,92,93]. Ingeniously, S. Typhimurium is able
affecting the extent of macrophage activation [64]. IL-18 is to exploit a specific microbiome-derived nutrient, named
important for IFN-c release and early host resistance to Salmonella ethanolamine, in order to acquire a significant growth
infections [66]. advantage in the lumen of inflamed intestine over other
potential pathogens [94]. Similarly, S. Typhimurium viru-
During severe bacterial infection uncontrolled activation of the
lence factors have been found to induce host-driven
innate immune response can lead to detrimental systemic production of a new electron acceptor that allows the
inflammation, intravascular coagulation, tissue injury, and even- pathogen to use respiration to compete with fermenting
tually death [67,68]. This hyper pro-inflammatory response is only gut microbes [95]. The potential of microbiota-based
seen to a limited extent in patients with typhoid fever. Coagulation therapies for curing Salmonella-infected patients has
abnormalities do not become clinically apparent and serum levels opened a whole new area of research [69].
of TNF-a and IL-1b are low compared to the levels measured in
PLOS Pathogens | www.plospathogens.org 5 October 2012 | Volume 8 | Issue 10 | e1002933
Box 2. Mouse Models for S. Typhi Infection Box 3. Questions for Future Research
S. Typhi infects humans exclusively. The consequent lack of Genomics
animal models has hampered the study of host–pathogen
interactions in typhoid fever. To overcome this problem N Can bacterial genotype be linked to the clinical disease
phenotype in humans?
experimental murine S. Typhimurium infection has been
used extensively as a model for typhoid fever. The N Is there a true association between bacterial genotype
intestinal pathology and inflammatory response seen in and/or the presence of a multidrug resistant plasmid and
this model resembles the changes observed in patients disease severity? If there is an association, what is the
with typhoid fever [96]. Current murine models include mechanism?
both oral and systemic (intravenous or intraperitoneal)
inoculation with or without streptomycin pretreatment Host-response
[91]. Infection of susceptible mouse strains that carry a
mutation in the gene encoding for a metal transporter N Is there a difference between S. Typhi- and S. Paratyphi-
present on the SCV membrane named Nramp1 (Slc11a1), induced enteric fever in the host gene expression
such as CL57/BL6 or BALB/C mice, produces a disease that pathways?
resembles typhoid fever upon inoculation with S. Typhi- N What is the role of DAMPs during severe typhoid fever?
murium [20]. To study chronic and persistent infection Are these danger-associated molecular patterns causing
such as can be seen in S. Typhi carriers, strains of mice the damage that occurs in the gut, or are they mere
possessing the Nramp +/+ allele, which are consequently bystanders triggering the NLRP3 inflammasome?
resistant to the infection with S. Typhimurium, are used
[64]. Of note, no allelic association was identified in
N Is a change in gut flora the reason that typhoid patients
still have an altered immune profile nine months after
humans between the Nramp alleles and typhoid suscep- infection? Moreover, do these patients have an increased
tibility, and as S. Typhimurium causes a different disease in risk for re-infection with other invasive Salmonellae?
humans than S. Typhi, conclusions regarding typhoid fever
pathogenesis derived from animal experiments must be
interpreted carefully [97]. An ingenious mouse model for S. Treatment
Typhi was proposed by making use of immunodeficient
Rag22/2 yc2/2 mice engrafted with human fetal liver
N Can we exploit a better understanding of disease
pathogenesis to lead to new therapeutic approaches?
hematopoietic stem and progenitor cells creating human- Potential immunomodulating treatment strategies for
ized mice susceptible to S. Typhi [98]. Although these invasive Salmonellosis could target the pathogen
humanized mice were able to support S. Typhi replication directly (e.g., based on drugs targeting T3SS or flagella)
and persistent infection, it did not lead to an acute lethal or target key host response proteins (e.g., TLR4, NLRC4,
infection [98]. Most recently, another murine lethal S. Typhi or IL-1b) depending on the phase of the immune
model resembling characteristic features of human ty- response.
phoid fever was created by making use of humanized
nonobese diabetic-scid IL2rcnull mice, which are engrafted N Are steroids beneficial in severe typhoid fever as has
previously been suggested [100]? And if so, what is the
with human hematopoetic stem cells (hu-SRC-SCID mice).
mechanism behind these observations?
This model, which has already been proven to be useful for
detecting new virulence determinants, could also be useful
to study host–pathogen interactions and evaluate vaccine
candidates [99]. shown that S. Typhimurium induces caspase-1 and NLRC4-
dependent IL-1b release and cell death [78]. NLRC4 is able to
recognize bacterial flagellin that—as has been hypothesized by
have increased susceptibility to Salmonella infection, and stimula- different authors—can be injected accidentally into the cytoplasm
tion of TLR4 by LPS has an important role in the development of by the T3SS causing cytosolic perturbations [65,79–81]. However,
septic shock during S. Typhimurium infection [56,72–74]. during experimental infection mice deficient in NLRC4 are able to
Salmonella flagellin leads to TLR5 activation [49]. Intriguingly, clear S. Typhimurium just as efficiently as control mice, suggesting
the Vi capsule expressed in mutated S. Typhimurium prevents the involvement of other inflammasomes [78]. Indeed, Broz et al.
both in vitro and in vivo recognition of Salmonella LPS by TLR4 demonstrated that both NLRP3 and NLRC4 activate caspase-1 in
[50,56]. The presence of the Vi antigen on the cell surface leads to response to S. Typhimurium infection, and mice lacking both NLRP3
capsule formation, which ultimately prevents this recognition. A and NLRC4 genes show increased susceptibility to infection. In
crucial role is ascribed to the TviA regulatory protein, encoded on response to a bacterial trigger, NLRP3 and NLRC4 will recruit ASC
the S. Typhi–specific SPI-7 (viaB locus), which downregulates and caspase-1 into a single cytoplasmic focus, which subsequently
flagellin production and enhances Vi antigen attachment to the serves as the site for pro-IL-1b processing [82]. Recent work provides
cell surface [75]. The TviA protein therefore serves as a regulatory evidence that the recognition of bacterial flagellin by the NLRC4
switch affecting the ability of the host to recognize S. Typhi as an inflammasome in splenic dendritic cells triggers rapid release of IL-
intruder at crucial stages of the spread in humans. 18, which leads to IFN-c production by memory CD8+ T cells [65].
The inflammasomes, which are intracellular complexes consist- NLRC4-mediated release of IL-1b has also been shown to be flagellin
ing of caspase-1, NLRs (e.g., NLRP3- or NLRC4), and the dependent, while the bacterial trigger for NLRP3 remains unclear.
adaptor molecule ASC (apoptosis-associated speck-like protein However, NLRP3 is able to recognize SPI-2 T3SS mutants, which
containing a CARD), play a central role in the innate immune lack the capacity to replicate intracellularly; therefore, the receptor is
defense against S. Typhimurium [76]. Mice deficient in caspase-1 thought to play a role in the detection of persistent bacteria [83].
or the end product of inflammasome activation, namely IL-1b and Although these studies underscore the central role of the inflamma-
IL-18, have higher bacterial load and succumb earlier upon some during S. Typhimurium infection, further research is needed to
infection with S. Typhimurium [77]. In vitro experiments have define its role in typhoid fever [83].
PLOS Pathogens | www.plospathogens.org 6 October 2012 | Volume 8 | Issue 10 | e1002933
Apoptosis and Pyroptosis role of key virulence factors such as Vi antigen and T3SS (Box 2).
Apoptosis or programmed cell death is regarded as a protective Studies of genome differences between S. Typhi, S. Paratyphi A, S.
mechanism of host defense by preventing further release of pro- Typhimurium, and other Salmonella serovars have begun to explain
inflammatory cellular mediators [84]. Serovars of S. enterica are some of the variation in disease manifestations. The important yet
able to employ different mechanisms to induce macrophage cell undefined roles of DAMPs and NLR-recognition in typhoid fever
death [85,86]. Recently it has been proposed that activation of remain to be clarified, and these may be major players in the
caspase-1 can also trigger a form of pro-inflammatory cell death severe gut ulceration that is an important cause of the mortality.
called ‘‘pyroptosis’’ [87]. Caspase-1, which is triggered via the Despite these major advances, large gaps remain in our
flagellin-detection of the NRLC4-inflammasome, is able to cause understanding of the pathogenesis of the disease in humans.
clearance of S. Typhimurium independent of IL-1b or IL-18 by Unraveling of the pathogenesis of invasive Salmonellosis hopefully
pyroptotic macrophage death [76]. In infected cells, caspase-1- leads to new therapeutic treatment strategies, urgently needed in
induced lysis of macrophages can result in the release of bacteria the light of growing antimicrobial resistance. Box 3 summarizes
into the extracellular space, which will enable efficient reactive some important questions for future research on invasive Salmonella
oxygen species (ROS) mediated killing by neutrophils. During the pathogenesis research.
systemic phase of infection, S. Typhimurium is able to completely
suppress flagellin expression, which results in evasion of NLRC4
detection and subsequent pyroptosis [76]. Interestingly selected Search Strategy and Selection Criteria
Salmonella-infected caspase-1-deficient macrophages do not under-
Data for this review were identified by searches of PubMed,
go pyroptosis but display a form of delayed cell death with features
of autophagy [86]. with the search terms ‘‘Typhoid Fever’’ in combination with
‘‘epidemiology,’’ ‘‘clinical features,’’ ‘‘therapy,’’ and ‘‘origin.’’
‘‘Salmonella Typhi’’ or ‘‘Salmonella Typhimurium’’ in combina-
Conclusion
tion with ‘‘genome,’’ ‘‘virulence factors,’’ ‘‘toll-like receptors,’’
Significant progress has been made in our understanding of ‘‘NOD-like receptors,’’ and ‘‘inflammasome.’’ The references of
host–pathogen interactions in invasive Salmonellosis. Mouse identified articles were manually searched for further relevant
models using S. Typhimurium have been instrumental in papers, and we also searched our own reference databases. English
unraveling complex pathways and have shed new light on the and French papers were reviewed.
References
1. Crump JA, Mintz ED (2010) Global trends in typhoid and paratyphoid Fever. 20. Sabbagh SC, Forest CG, Lepage C, Leclerc JM, Daigle F (2010) So similar, yet
Clin Infect Dis 50: 241–246. so different: uncovering distinctive features in the genomes of Salmonella
2. Connor BA, Schwartz E (2005) Typhoid and paratyphoid fever in travellers. enterica serovars Typhimurium and Typhi. FEMS Microbiol Lett 305: 1–13.
Lancet Infect Dis 5: 623–628. 21. Kingsley RA, Msefula CL, Thomson NR, Kariuki S, Holt KE, et al. (2009)
3. Tsolis RM, Young GM, Solnick JV, Baumler AJ (2008) From bench to bedside: Epidemic multiple drug resistant Salmonella Typhimurium causing invasive disease
stealth of enteroinvasive pathogens. Nat Rev Microbiol 6: 883–892. in sub-Saharan Africa have a distinct genotype. Genome Res 19: 2279–2287.
4. Arjyal A, Basnyat B, Koirala S, Karkey A, Dongol S, et al. (2011) Gatifloxacin 22. Ehrbar K, Hardt WD (2005) Bacteriophage-encoded type III effectors in
versus chloramphenicol for uncomplicated enteric fever: an open-label, Salmonella enterica subspecies 1 serovar Typhimurium. Infect Genet Evol 5: 1–9.
randomised, controlled trial. Lancet Infect Dis 11: 445–454. 23. Lesnick ML, Reiner NE, Fierer J, Guiney DG (2001) The Salmonella spvB
5. Beeching NJ, Parry CM (2011) Outpatient treatment of patients with enteric virulence gene encodes an enzyme that ADP-ribosylates actin and destabilizes
fever. Lancet Infect Dis 11: 419–421. the cytoskeleton of eukaryotic cells. Mol Microbiol 39: 1464–1470.
6. Monack DM, Mueller A, Falkow S (2004) Persistent bacterial infections: the 24. Huang R, Wu S, Zhang X, Zhang Y (2005) Molecular analysis and
interface of the pathogen and the host immune system. Nat Rev Microbiol 2: identification of virulence gene on pR(ST98) from multi-drug resistant
747–765. Salmonella typhi. Cell Mol Immunol 2: 136–140.
7. Monack DM (2011) Salmonella persistence and transmission strategies. Curr 25. Wu S, Li Y, Xu Y, Li Q, Chu Y, et al. (2010) A Salmonella enterica serovar
Opin Microbiol 15: 100–107. Typhi plasmid induces rapid and massive apoptosis in infected macrophages.
8. Parry CM, Hien TT, Dougan G, White NJ, Farrar JJ (2002) Typhoid fever. Cell Mol Immunol 7: 271–278.
N Engl J Med 347: 1770–1782. 26. Baker S, Hardy J, Sanderson KE, Quail M, Goodhead I, et al. (2007) A novel
9. Feasey NA, Dougan G, Kingsley RA, Heyderman RS, Gordon MA (2012) linear plasmid mediates flagellar variation in Salmonella Typhi. PLoS Pathog 3:
Invasive non-typhoidal salmonella disease: an emerging and neglected tropical e59. doi:10.1371/journal.ppat.0030059
disease in Africa. Lancet 379: 2489–2499. 27. Phan MD, Kidgell C, Nair S, Holt KE, Turner AK, et al. (2009) Variation in
10. Majowicz SE, Musto J, Scallan E, Angulo FJ, Kirk M, et al. (2010) The global Salmonella enterica serovar typhi IncHI1 plasmids during the global spread of
burden of nontyphoidal Salmonella gastroenteritis. Clin Infect Dis 50: 882–889. resistant typhoid fever. Antimicrob Agents Chemother 53: 716–727.
11. Graham SM (2010) Nontyphoidal salmonellosis in Africa. Curr Opin Infect Dis 28. Phan MD, Wain J (2008) IncHI plasmids, a dynamic link between resistance and
23: 409–414. pathogenicity. J Infect Dev Ctries 2: 272–278.
12. Parry CM, Threlfall EJ (2008) Antimicrobial resistance in typhoidal and 29. Holt KE, Phan MD, Baker S, Duy PT, Nga TV, et al. (2011) Emergence of a
globally dominant IncHI1 plasmid type associated with multiple drug resistant
nontyphoidal salmonellae. Curr Opin Infect Dis 21: 531–538.
typhoid. PLoS Negl Trop Dis 5: e1245. doi:10.1371/journal.pntd.0001245
13. Baker S (2011) Genomic medicine has failed the poor. Nature 478: 287.
30. Bhutta ZA (1996) Impact of age and drug resistance on mortality in typhoid
14. Deng W, Liou SR, Plunkett G, III, Mayhew GF, Rose DJ, et al. (2003)
fever. Arch Dis Child 75: 214–217.
Comparative genomics of Salmonella enterica serovar Typhi strains Ty2 and
31. Wain J, Diep TS, Ho VA, Walsh AM, Nguyen TT, et al. (1998) Quantitation of
CT18. J Bacteriol 185: 2330–2337. bacteria in blood of typhoid fever patients and relationship between counts and
15. Parkhill J, Dougan G, James KD, Thomson NR, Pickard D, et al. (2001) clinical features, transmissibility, and antibiotic resistance. J Clin Microbiol 36:
Complete genome sequence of a multiple drug resistant Salmonella enterica 1683–1687.
serovar Typhi CT18. Nature 413: 848–852. 32. Thomson N, Baker S, Pickard D, Fookes M, Anjum M, et al. (2004) The role of
16. McClelland M, Sanderson KE, Spieth J, Clifton SW, Latreille P, et al. (2001) prophage-like elements in the diversity of Salmonella enterica serovars. J Mol
Complete genome sequence of Salmonella enterica serovar Typhimurium LT2. Biol 339: 279–300.
Nature 413: 852–856. 33. Terebiznik MR, Vieira OV, Marcus SL, Slade A, Yip CM, et al. (2002)
17. Baker S, Dougan G (2007) The genome of Salmonella enterica serovar Typhi. Elimination of host cell PtdIns(4,5)P(2) by bacterial SigD promotes membrane
Clin Infect Dis 45 Suppl 1: S29–S33. fission during invasion by Salmonella. Nat Cell Biol 4: 766–773.
18. Achtman M, Wain J, Weill FX, Nair S, Zhou Z, et al. (2012) Multilocus 34. Hernandez LD, Hueffer K, Wenk MR, Galan JE (2004) Salmonella modulates
sequence typing as a replacement for serotyping in salmonella enterica. PLoS vesicular traffic by altering phosphoinositide metabolism. Science 304: 1805–1807.
Pathog 8: e1002776. doi:10.1371/journal.ppat.1002776 35. Knodler LA, Finlay BB, Steele-Mortimer O (2005) The Salmonella effector
19. Raffatellu M, Wilson RP, Winter SE, Baumler AJ (2008) Clinical pathogenesis of protein SopB protects epithelial cells from apoptosis by sustained activation of
typhoid fever. J Infect Dev Ctries 2: 260–266. Akt. J Biol Chem 280: 9058–9064.
PLOS Pathogens | www.plospathogens.org 7 October 2012 | Volume 8 | Issue 10 | e1002933
36. Ibarra JA, Steele-Mortimer O (2009) Salmonella—the ultimate insider. 64. Monack DM, Bouley DM, Falkow S (2004) Salmonella typhimurium persists
Salmonella virulence factors that modulate intracellular survival. Cell Microbiol within macrophages in the mesenteric lymph nodes of chronically infected
11: 1579–1586. Nramp1+/+ mice and can be reactivated by IFNgamma neutralization. J Exp
37. Fang FC, DeGroote MA, Foster JW, Baumler AJ, Ochsner U, et al. (1999) Med 199: 231–241.
Virulent Salmonella typhimurium has two periplasmic Cu, Zn-superoxide 65. Kupz A, Guarda G, Gebhardt T, Sander LE, Short KR, et al. (2012) NLRC4
dismutases. Proc Natl Acad Sci U S A 96: 7502–7507. inflammasomes in dendritic cells regulate noncognate effector function by
38. Figueroa-Bossi N, Bossi L (1999) Inducible prophages contribute to Salmonella memory CD8(+) T cells. Nat Immunol 13: 162–169.
virulence in mice. Mol Microbiol 33: 167–176. 66. Mastroeni P, Clare S, Khan S, Harrison JA, Hormaeche CE, et al. (1999)
39. Galan JE (1999) Interaction of Salmonella with host cells through the centisome Interleukin 18 contributes to host resistance and gamma interferon production in
63 type III secretion system. Curr Opin Microbiol 2: 46–50. mice infected with virulent Salmonella typhimurium. Infect Immun 67: 478–
40. Vazquez-Torres A, Jones-Carson J, Baumler AJ, Falkow S, Valdivia R, et al. 483.
(1999) Extraintestinal dissemination of Salmonella by CD18-expressing 67. de Jong HK, van der Poll T, Wiersinga WJ (2010) The systemic pro-
phagocytes. Nature 401: 804–808. inflammatory response in sepsis. J Innate Immun 2: 422–430.
41. Rescigno M, Urbano M, Valzasina B, Francolini M, Rotta G, et al. (2001) 68. van der Poll T, Opal SM (2008) Host-pathogen interactions in sepsis. Lancet
Dendritic cells express tight junction proteins and penetrate gut epithelial Infect Dis 8: 32–43.
monolayers to sample bacteria. Nat Immunol 2: 361–367. 69. Endt K, Stecher B, Chaffron S, Slack E, Tchitchek N, et al. (2010) The
42. Hensel M, Shea JE, Waterman SR, Mundy R, Nikolaus T, et al. (1998) Genes microbiota mediates pathogen clearance from the gut lumen after non-typhoidal
encoding putative effector proteins of the type III secretion system of Salmonella Salmonella diarrhea. PLoS Pathog 6: e1001097. doi:10.1371/journal.-
pathogenicity island 2 are required for bacterial virulence and proliferation in ppat.1001097
macrophages. Mol Microbiol 30: 163–174. 70. Raffatellu M, Santos RL, Verhoeven DE, George MD, Wilson RP, et al. (2008)
43. Vazquez-Torres A, Xu Y, Jones-Carson J, Holden DW, Lucia SM, et al. (2000) Simian immunodeficiency virus-induced mucosal interleukin-17 deficiency
Salmonella pathogenicity island 2-dependent evasion of the phagocyte NADPH promotes Salmonella dissemination from the gut. Nat Med 14: 421–428.
oxidase. Science 287: 1655–1658. 71. Gordon MA, Kankwatira AM, Mwafulirwa G, Walsh AL, Hopkins MJ, et al.
44. Gallois A, Klein JR, Allen LA, Jones BD, Nauseef WM (2001) Salmonella (2010) Invasive non-typhoid salmonellae establish systemic intracellular infection
pathogenicity island 2-encoded type III secretion system mediates exclusion of in HIV-infected adults: an emerging disease pathogenesis. Clin Infect Dis 50:
NADPH oxidase assembly from the phagosomal membrane. J Immunol 166: 953–962.
5741–5748. 72. O’Brien AD, Rosenstreich DL, Taylor BA (1980) Control of natural resistance
45. Forest CG, Ferraro E, Sabbagh SC, Daigle F (2010) Intracellular survival of to Salmonella typhimurium and Leishmania donovani in mice by closely linked
Salmonella enterica serovar Typhi in human macrophages is independent of but distinct genetic loci. Nature 287: 440–442.
Salmonella pathogenicity island (SPI)-2. Microbiology 156: 3689–3698. 73. Weinstein DL, Lissner CR, Swanson RN, O’Brien AD (1986) Macrophage
46. Yoon H, Ansong C, Adkins JN, Heffron F (2011) Discovery of Salmonella defect and inflammatory cell recruitment dysfunction in Salmonella susceptible
virulence factors translocated via outer membrane vesicles to murine C3H/HeJ mice. Cell Immunol 102: 68–77.
macrophages. Infect Immun 79: 2182–2192. 74. Vazquez-Torres A, Vallance BA, Bergman MA, Finlay BB, Cookson BT, et al.
47. Wai SN, Lindmark B, Soderblom T, Takade A, Westermark M, et al. (2003) (2004) Toll-like receptor 4 dependence of innate and adaptive immunity to
Vesicle-mediated export and assembly of pore-forming oligomers of the Salmonella: importance of the Kupffer cell network. J Immunol 172: 6202–
enterobacterial ClyA cytotoxin. Cell 115: 25–35. 6208.
48. Alaniz RC, Deatherage BL, Lara JC, Cookson BT (2007) Membrane vesicles are 75. Winter SE, Raffatellu M, Wilson RP, Russmann H, Baumler AJ (2008) The
immunogenic facsimiles of Salmonella typhimurium that potently activate Salmonella enterica serotype Typhi regulator TviA reduces interleukin-8
dendritic cells, prime B and T cell responses, and stimulate protective immunity
production in intestinal epithelial cells by repressing flagellin secretion. Cell
in vivo. J Immunol 179: 7692–7701.
Microbiol 10: 247–261.
49. Zeng H, Carlson AQ, Guo Y, Yu Y, Collier-Hyams LS, et al. (2003) Flagellin is
76. Miao EA, Leaf IA, Treuting PM, Mao DP, Dors M, et al. (2010) Caspase-1-
the major proinflammatory determinant of enteropathogenic Salmonella.
induced pyroptosis is an innate immune effector mechanism against intracellular
J Immunol 171: 3668–3674.
bacteria. Nat Immunol 11: 1136–1142.
50. Winter SE, Thiennimitr P, Nuccio SP, Haneda T, Winter MG, et al. (2009)
77. Raupach B, Peuschel SK, Monack DM, Zychlinsky A (2006) Caspase-1-
Contribution of flagellin pattern recognition to intestinal inflammation during
mediated activation of interleukin-1beta (IL-1beta) and IL-18 contributes to
Salmonella enterica serotype typhimurium infection. Infect Immun 77: 1904–
innate immune defenses against Salmonella enterica serovar Typhimurium
1916.
infection. Infect Immun 74: 4922–4926.
51. Lockman HA, Curtiss R, 3rd (1990) Salmonella typhimurium mutants lacking
78. Lara-Tejero M, Sutterwala FS, Ogura Y, Grant EP, Bertin J, et al. (2006) Role
flagella or motility remain virulent in BALB/c mice. Infect Immun 58: 137–143.
of the caspase-1 inflammasome in Salmonella typhimurium pathogenesis. J Exp
52. Schmitt CK, Ikeda JS, Darnell SC, Watson PR, Bispham J, et al. (2001) Absence
Med 203: 1407–1412.
of all components of the flagellar export and synthesis machinery differentially
alters virulence of Salmonella enterica serovar Typhimurium in models of 79. Franchi L, Amer A, Body-Malapel M, Kanneganti TD, Ozoren N, et al. (2006)
typhoid fever, survival in macrophages, tissue culture invasiveness, and calf Cytosolic flagellin requires Ipaf for activation of caspase-1 and interleukin 1beta
enterocolitis. Infect Immun 69: 5619–5625. in salmonella-infected macrophages. Nat Immunol 7: 576–582.
53. Wain J, House D, Zafar A, Baker S, Nair S, et al. (2005) Vi antigen expression in 80. Miao EA, Alpuche-Aranda CM, Dors M, Clark AE, Bader MW, et al. (2006)
Salmonella enterica serovar Typhi clinical isolates from Pakistan. J Clin Cytoplasmic flagellin activates caspase-1 and secretion of interleukin 1beta via
Microbiol 43: 1158–1165. Ipaf. Nat Immunol 7: 569–575.
54. Zhang XL, Jeza VT, Pan Q (2008) Salmonella typhi: from a human pathogen to 81. Miao EA, Mao DP, Yudkovsky N, Bonneau R, Lorang CG, et al. (2010) Innate
a vaccine vector. Cell Mol Immunol 5: 91–97. immune detection of the type III secretion apparatus through the NLRC4
55. Kolyva S, Waxin H, Popoff MY (1992) The Vi antigen of Salmonella typhi: inflammasome. Proc Natl Acad Sci U S A 107: 3076–3080.
molecular analysis of the viaB locus. J Gen Microbiol 138: 297–304. 82. Broz P, Newton K, Lamkanfi M, Mariathasan S, Dixit VM, et al. (2010)
56. Wilson RP, Raffatellu M, Chessa D, Winter SE, Tukel C, et al. (2008) The Vi- Redundant roles for inflammasome receptors NLRP3 and NLRC4 in host
capsule prevents Toll-like receptor 4 recognition of Salmonella. Cell Microbiol defense against Salmonella. J Exp Med 207: 1745–1755.
10: 876–890. 83. Broz P, Monack DM (2011) Molecular mechanisms of inflammasome activation
57. Kawai T, Akira S (2010) The role of pattern-recognition receptors in innate during microbial infections. Immunol Rev 243: 174–190.
immunity: update on Toll-like receptors. Nat Immunol 11: 373–384. 84. Fink SL, Cookson BT (2005) Apoptosis, pyroptosis, and necrosis: mechanistic
58. Schroder K, Tschopp J (2010) The inflammasomes. Cell 140: 821–832. description of dead and dying eukaryotic cells. Infect Immun 73: 1907–1916.
59. Butler T, Ho M, Acharya G, Tiwari M, Gallati H (1993) Interleukin-6, gamma 85. Hueffer K, Galan JE (2004) Salmonella-induced macrophage death: multiple
interferon, and tumor necrosis factor receptors in typhoid fever related to mechanisms, different outcomes. Cell Microbiol 6: 1019–1025.
outcome of antimicrobial therapy. Antimicrob Agents Chemother 37: 2418– 86. Hernandez LD, Pypaert M, Flavell RA, Galan JE (2003) A Salmonella protein
2421. causes macrophage cell death by inducing autophagy. J Cell Biol 163: 1123–
60. Butler T, Bell WR, Levin J, Linh NN, Arnold K (2011) Typhoid fever. Studies of 1131.
blood coagulation, bacteremia, and endotoxemia. Arch Intern Med 138: 407– 87. Brodsky IE, Monack D (2009) NLR-mediated control of inflammasome
410. assembly in the host response against bacterial pathogens. Semin Immunol 21:
61. Keuter M, Dharmana E, Gasem MH, van dV, Djokomoeljanto R, et al. (1994) 199–207.
Patterns of proinflammatory cytokines and inhibitors during typhoid fever. 88. Crawford RW, Rosales-Reyes R, Ramirez-Aguilar Mde L, Chapa-Azuela O,
J Infect Dis 169: 1306–1311. Alpuche-Aranda C, et al. (2010) Gallstones play a significant role in Salmonella
62. Raffatellu M, Chessa D, Wilson RP, Tukel C, Akcelik M, et al. (2006) Capsule- spp. gallbladder colonization and carriage. Proc Natl Acad Sci U S A 107: 4353–
mediated immune evasion: a new hypothesis explaining aspects of typhoid fever 4358.
pathogenesis. Infect Immun 74: 19–27. 89. Everest P, Wain J, Roberts M, Rook G, Dougan G (2001) The molecular
63. Thompson LJ, Dunstan SJ, Dolecek C, Perkins T, House D, et al. (2009) mechanisms of severe typhoid fever. Trends Microbiol 9: 316–320.
Transcriptional response in the peripheral blood of patients infected with 90. Kobayashi K, Hernandez LD, Galan JE, Janeway CA, Jr., Medzhitov R, et al.
Salmonella enterica serovar Typhi. Proc Natl Acad Sci U S A 106: 22433– (2002) IRAK-M is a negative regulator of Toll-like receptor signaling. Cell 110:
22438. 191–202.
PLOS Pathogens | www.plospathogens.org 8 October 2012 | Volume 8 | Issue 10 | e1002933
91. Kaiser P, Diard M, Stecher B, Hardt WD (2012) The streptomycin mouse 96. Santos RL, Zhang S, Tsolis RM, Kingsley RA, Adams LG, et al. (2001) Animal
model for Salmonella diarrhea: functional analysis of the microbiota, the models of Salmonella infections: enteritis versus typhoid fever. Microbes Infect 3:
pathogen’s virulence factors, and the host’s mucosal immune response. Immunol 1335–1344.
Rev 245: 56–83. 97. Dunstan SJ, Ho VA, Duc CM, Lanh MN, Phuong CX, et al. (2001) Typhoid
92. Croswell A, Amir E, Teggatz P, Barman M, Salzman NH (2009) Prolonged fever and genetic polymorphisms at the natural resistance-associated macro-
impact of antibiotics on intestinal microbial ecology and susceptibility to enteric phage protein 1. J Infect Dis 183: 1156–1160.
Salmonella infection. Infect Immun 77: 2741–2753. 98. Song J, Willinger T, Rongvaux A, Eynon EE, Stevens S, et al. (2010) A mouse
93. Gopinath S, Carden S, Monack D (2012) Shedding light on Salmonella carriers. model for the human pathogen Salmonella typhi. Cell Host Microbe 8: 369–376.
Trends Microbiol 20: 320–327. 99. Libby SJ, Brehm MA, Greiner DL, Shultz LD, McClelland M, et al. (2010)
94. Thiennimitr P, Winter SE, Baumler AJ (2012) Salmonella, the host and its Humanized nonobese diabetic-scid IL2rgammanull mice are susceptible to
microbiota. Curr Opin Immunol 15: 108–114. lethal Salmonella Typhi infection. Proc Natl Acad Sci U S A 107: 15589–15594.
95. Winter SE, Thiennimitr P, Winter MG, Butler BP, Huseby DL, et al. (2010) Gut 100. Hoffman SL, Punjabi NH, Kumala S, Moechtar MA, Pulungsih SP, et al.
inflammation provides a respiratory electron acceptor for Salmonella. Nature (1984) Reduction of mortality in chloramphenicol-treated severe typhoid fever
467: 426–429. by high-dose dexamethasone. N Engl J Med 310: 82–88.
PLOS Pathogens | www.plospathogens.org 9 October 2012 | Volume 8 | Issue 10 | e1002933
View publication stats
You might also like
- Communicable and Non-Communicable DiseasesDocument46 pagesCommunicable and Non-Communicable DiseasesMohd Al Qassam100% (1)
- Host-Pathogen Interaction in Invasive Salmonellosis: ReviewDocument9 pagesHost-Pathogen Interaction in Invasive Salmonellosis: ReviewFabsscribNo ratings yet
- Cells in Dengue Virus InfectionDocument16 pagesCells in Dengue Virus Infectionthyago6No ratings yet
- Vol1 No4 3Document9 pagesVol1 No4 3Andra HijratulNo ratings yet
- Artigo InfluenzaDocument9 pagesArtigo InfluenzaMatheus GonçalvesNo ratings yet
- Immunological, Cellular and Molecular Events in Typhoid FeverDocument12 pagesImmunological, Cellular and Molecular Events in Typhoid FeverAde RifkaNo ratings yet
- Harriet Ugboko and Nandita deDocument16 pagesHarriet Ugboko and Nandita deChockalingam MeenakshisundaramNo ratings yet
- UntitledDocument15 pagesUntitledDagmawi BahiruNo ratings yet
- Nihms 940015Document50 pagesNihms 940015Maria Salome Olortegui AceroNo ratings yet
- Typhoid Fever - StatPearls - NCBI BookshelfDocument13 pagesTyphoid Fever - StatPearls - NCBI Bookshelfhasnah shintaNo ratings yet
- Microorganisms 10 02006 v2Document15 pagesMicroorganisms 10 02006 v2Novia khasanahNo ratings yet
- Intestinal Protozoan Infections in The Immunocompromised HostDocument7 pagesIntestinal Protozoan Infections in The Immunocompromised HostJenny Mundaca QuirozNo ratings yet
- Histoplasmosis AtsDocument4 pagesHistoplasmosis Atsanabella081096No ratings yet
- Toxoplasmosis - A Global ThreatDocument8 pagesToxoplasmosis - A Global ThreatDr-Sadaqat Ali RaoNo ratings yet
- University of Santo Tomas: UST-SHS Practical Research 2Document3 pagesUniversity of Santo Tomas: UST-SHS Practical Research 2MayNo ratings yet
- Typhoid ResearchDocument42 pagesTyphoid Researchhamidhasan6944No ratings yet
- IJRPR5794Document8 pagesIJRPR5794ukelabenardNo ratings yet
- Mullangi 2012Document10 pagesMullangi 2012Mariana AmbossNo ratings yet
- Salmonella, The Host and Disease: A Brief ReviewDocument8 pagesSalmonella, The Host and Disease: A Brief ReviewPedro Albán MNo ratings yet
- Infections in The Neutropenic Patient-2001Document27 pagesInfections in The Neutropenic Patient-2001Raisa_90No ratings yet
- Typhoid FeverDocument14 pagesTyphoid FeverJames Cojab SacalNo ratings yet
- Increasing Prevalence of Antimicrobial ResistanceDocument43 pagesIncreasing Prevalence of Antimicrobial ResistanceAnisa Rahma UtamiNo ratings yet
- Meningitidis Colonization and Invasive Disease: Cellular and Molecular Biology of NeisseriaDocument18 pagesMeningitidis Colonization and Invasive Disease: Cellular and Molecular Biology of NeisseriamulyadiNo ratings yet
- Analysis of Tonsil Tissues From Pts Diagnosed With Chronic Tonsillitis - Microbiological ProfileDocument15 pagesAnalysis of Tonsil Tissues From Pts Diagnosed With Chronic Tonsillitis - Microbiological Profiledr syed qasim ali jafriNo ratings yet
- (2011, Rothman AL) Immunity To Dengue Virus - A Tale of Original Antigenic Sin and Tropical Cytokine StormsDocument12 pages(2011, Rothman AL) Immunity To Dengue Virus - A Tale of Original Antigenic Sin and Tropical Cytokine StormsRebeca de PaivaNo ratings yet
- S Typhi Has Been A Major Human Pathogen For Thousands of Years, Thriving in Conditions of PoorDocument11 pagesS Typhi Has Been A Major Human Pathogen For Thousands of Years, Thriving in Conditions of PoorGio Vano NaihonamNo ratings yet
- Kumpulan Jurnal DengueDocument122 pagesKumpulan Jurnal DengueMas MantriNo ratings yet
- Bakteri S EpidermisDocument15 pagesBakteri S EpidermisSheillaizza FadhillaNo ratings yet
- Typhoid Fever Current Concepts.5Document7 pagesTyphoid Fever Current Concepts.5pawitrajayaNo ratings yet
- Microorganisms 09 02155Document15 pagesMicroorganisms 09 02155raypinky404No ratings yet
- Ciy1111 5Document6 pagesCiy1111 5inesNo ratings yet
- Pseudomonas Aeruginosa - Pathogenesis and Pathogenic MechanismsDocument24 pagesPseudomonas Aeruginosa - Pathogenesis and Pathogenic MechanismsFitryNo ratings yet
- Patogenia de La ToxoplasmosisDocument10 pagesPatogenia de La ToxoplasmosisSasha de la CruzNo ratings yet
- TB PaperDocument11 pagesTB PapergwapingMDNo ratings yet
- Enteric Fever - Diagnostic Challenges and The Importance of Early InterventionDocument14 pagesEnteric Fever - Diagnostic Challenges and The Importance of Early Interventionju.ozc.69No ratings yet
- Typhoid FeverDocument13 pagesTyphoid FeverFajar NarakusumaNo ratings yet
- NIH Public Access: Author ManuscriptDocument22 pagesNIH Public Access: Author ManuscriptuhuhsuNo ratings yet
- Typhoid Encephalopathy in Children Review Article 625Document2 pagesTyphoid Encephalopathy in Children Review Article 625Anurag UdhwaniNo ratings yet
- Salmonella From Basic Science To Clinical IssuesDocument4 pagesSalmonella From Basic Science To Clinical IssuesYusda FadillaNo ratings yet
- Typhoid Fever: Disease PrimersDocument18 pagesTyphoid Fever: Disease PrimersErick HernandezNo ratings yet
- Dengue Pathogenesis: A Disease Driven by The Host Response: Byron E.E. MartinaDocument18 pagesDengue Pathogenesis: A Disease Driven by The Host Response: Byron E.E. MartinaAn iNo ratings yet
- Tuberculosis Thesis IntroductionDocument8 pagesTuberculosis Thesis Introductionifywpqvcf100% (2)
- PatogenesisDocument28 pagesPatogenesisOka WidyaningsihNo ratings yet
- Background TyphoidDocument21 pagesBackground TyphoidNurmala Rahman LNo ratings yet
- Vervloet Et Al-2007-Brazilian Journal of Infectious DiseasesDocument8 pagesVervloet Et Al-2007-Brazilian Journal of Infectious DiseasesCynthia GalloNo ratings yet
- Typhoid Fever PDFDocument14 pagesTyphoid Fever PDFginstarNo ratings yet
- Toxoplasmosis Revisited: Sheela Mathew, MD, Infectious Diseases Department, GovernmentDocument11 pagesToxoplasmosis Revisited: Sheela Mathew, MD, Infectious Diseases Department, GovernmentMuhammad Afiq HusinNo ratings yet
- Typhoid DiseaseDocument28 pagesTyphoid DiseaseSaba Parvin Haque100% (1)
- Pathogenesis Typhoid Fever PDFDocument7 pagesPathogenesis Typhoid Fever PDFAry Nahdiyani Amalia100% (1)
- UpToDate Pneumonia Caused by I Chlamydia Pneumoniae I in AdultsDocument22 pagesUpToDate Pneumonia Caused by I Chlamydia Pneumoniae I in Adultsdr.murtaza2019No ratings yet
- Staphylococcus Epidermidis: Bio®lms: Importance and ImplicationsDocument6 pagesStaphylococcus Epidermidis: Bio®lms: Importance and ImplicationsBagus SetiawanNo ratings yet
- TUBERCULOSIS Imaging ManifestationsDocument21 pagesTUBERCULOSIS Imaging ManifestationsEdgard Eduardo Azañero EstradaNo ratings yet
- Tropicalmed 08 00487Document22 pagesTropicalmed 08 00487Angie Dominguez CampoNo ratings yet
- HHS Public Access: Strongyloidiasis: A Neglected Neglected Tropical Disease (NTD)Document20 pagesHHS Public Access: Strongyloidiasis: A Neglected Neglected Tropical Disease (NTD)Iván Castellares RojasNo ratings yet
- Mesaros 2007 1Document19 pagesMesaros 2007 1Drashua AshuaNo ratings yet
- Coidi 31 449Document6 pagesCoidi 31 449Kavyarani RathodNo ratings yet
- A Comphrensive Review On AmoebiasisDocument6 pagesA Comphrensive Review On AmoebiasisInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Introduction To Medical MicrobiologyDocument9 pagesIntroduction To Medical MicrobiologyIsba Shadai Estrada GarciaNo ratings yet
- Comprehensive Insights into Haemophilus Influenzae: From Biology to Global Health StrategiesFrom EverandComprehensive Insights into Haemophilus Influenzae: From Biology to Global Health StrategiesNo ratings yet
- Viral Vistas: Insights into Infectious Diseases: The Invisible War: Decoding the Game of Hide and Seek with PathogensFrom EverandViral Vistas: Insights into Infectious Diseases: The Invisible War: Decoding the Game of Hide and Seek with PathogensNo ratings yet
- Management of Infections in the Immunocompromised HostFrom EverandManagement of Infections in the Immunocompromised HostBrahm H. SegalNo ratings yet
- Name of Patient: E.J.P Ward/Room/Bed #: Pedia Ward/G.I./Bed 1 Age & Sex: 2 Y.o/ Female Diagnosis: Urinary Tract InfectionDocument1 pageName of Patient: E.J.P Ward/Room/Bed #: Pedia Ward/G.I./Bed 1 Age & Sex: 2 Y.o/ Female Diagnosis: Urinary Tract InfectionSALMA M. TUANONo ratings yet
- Gastritis Englis 2018Document115 pagesGastritis Englis 2018irinaNo ratings yet
- Jurnal ImunologiDocument4 pagesJurnal ImunologiElsa YuniaNo ratings yet
- The Relationship Between IgE and Allergic DiseaseDocument12 pagesThe Relationship Between IgE and Allergic DiseaseAbdusSomadNo ratings yet
- Coronavirus (COVID-19) RecordsDocument2 pagesCoronavirus (COVID-19) RecordsBADREDINENo ratings yet
- 4 C 566 A 70 Da 279 BCFDocument8 pages4 C 566 A 70 Da 279 BCFMazin AlmaziniNo ratings yet
- Table MicpDocument21 pagesTable MicpPauline Hidlao100% (1)
- c23 Microbiology Tortora TestbankDocument16 pagesc23 Microbiology Tortora Testbankwhitewave25No ratings yet
- Rabies PreventionDocument3 pagesRabies PreventionFrinkaWijaya100% (1)
- Kuliah Erupsi ObatDocument94 pagesKuliah Erupsi ObatHazbina Fauqi RamadhanNo ratings yet
- A Guide To The Management of Acute Rhinosinusitis in Primary CareDocument4 pagesA Guide To The Management of Acute Rhinosinusitis in Primary CarecubillahhNo ratings yet
- Lesson1 Non Specific DefenseDocument3 pagesLesson1 Non Specific DefenseEyad MohamedNo ratings yet
- PAEDS Infectious Diseases, Rahes, Fever SUMMARYDocument41 pagesPAEDS Infectious Diseases, Rahes, Fever SUMMARYChante LouwNo ratings yet
- 4 Merged 1516624856 PDFDocument50 pages4 Merged 1516624856 PDFVya PrabandariNo ratings yet
- Prevention of Hospital-Acquired Infections: A Practical Guide 2nd EditionDocument72 pagesPrevention of Hospital-Acquired Infections: A Practical Guide 2nd EditionHussein AhmedNo ratings yet
- Dengue-Malaria TOT For Doctors 2022 Operational Aspects (Malaria) - DR - M .GhoshDocument21 pagesDengue-Malaria TOT For Doctors 2022 Operational Aspects (Malaria) - DR - M .GhoshDk YadavNo ratings yet
- A Low Molecular Weight Fraction of Bovine Colostrum and Milk Enhances The Oxidative Burst Activity of Polymorphonuclear Leukocytes PDFDocument9 pagesA Low Molecular Weight Fraction of Bovine Colostrum and Milk Enhances The Oxidative Burst Activity of Polymorphonuclear Leukocytes PDFManuel VázquezNo ratings yet
- AEFI PPT 2Document43 pagesAEFI PPT 2HarshaWakodkar50% (2)
- Heat and Cold Application 1Document42 pagesHeat and Cold Application 1Bea Trisha ArietaNo ratings yet
- Pfizer Health Declaration Screening Form Eng June 9 2021Document1 pagePfizer Health Declaration Screening Form Eng June 9 2021Kim GomezNo ratings yet
- Engerix B Cmi AuDocument4 pagesEngerix B Cmi AuTsukishiro GomaNo ratings yet
- 02 MenangitisDocument4 pages02 MenangitisMaeen Gamal AlhadhramiNo ratings yet
- BSC H Biological ScienceDocument136 pagesBSC H Biological ScienceYash ChoudharyNo ratings yet
- 80-Article Text-153-1-10-20161118Document4 pages80-Article Text-153-1-10-20161118Rania SalwanabilaNo ratings yet
- Anm 3 241220Document721 pagesAnm 3 241220patel divyaNo ratings yet
- Pertanyaan ReferatDocument2 pagesPertanyaan ReferatBuydh BfdsfsNo ratings yet
- National Filaria Control ProgrammeDocument2 pagesNational Filaria Control ProgrammeFoysal Sirazee100% (1)
- Buletine de Analize: Dr. Nicoleta LefterDocument37 pagesBuletine de Analize: Dr. Nicoleta LefterMarilena TarcaNo ratings yet
- IPACI 2024 Second AnnouncementDocument8 pagesIPACI 2024 Second AnnouncementRaissa RiandaNo ratings yet