Upper Limb 0809 PDF
Upper Limb 0809 PDF
Uploaded by
asdaCopyright:
Available Formats
Upper Limb 0809 PDF
Upper Limb 0809 PDF
Uploaded by
asdaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Upper Limb 0809 PDF
Upper Limb 0809 PDF
Uploaded by
asdaCopyright:
Available Formats
Upper limb
Muscles, fascia, joints &
regions
2008/2009
Haytham Bayadsi
Haytham Bayadsi 2008/2009
Upper Limb
Muscles
Haytham Bayadsi 2008/2009
Haytham Bayadsi 2008/2009
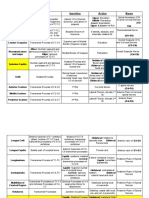
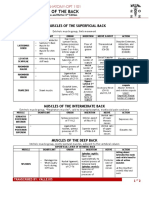
Muscle Origin Insertion Innervation
Anterior
Axioappendicular
Pectoralis Major
- Clavicular part: - Medial 1/2 of Crest of the Pectoral
- Sternocostal Anterior Surface of Greater tubercle Nerves (Lat.
part: clavicle. and Med.)
- Abdominal - Sternum (Ant. (C5-T1)
part: Surface) & cartilages
of 1-6th ribs.
- Rectus sheath (Ext.
oblique aponeurosis).
Coracoid Med. Pectoral
Pectoralis Minor 3rd-5th ribs
process nerve (C7-T1)
Junction of 1st rib and Subclavius Subclavian n.
Subclavius cartilage groove of (C5-C6)
clavicle
Ant. Surface of
External surfaces of Long Thoracic
Serratus Anterior medial border of
1st-8th ribs (slips) n. (C5-C7)
scapula
Posterior
Axioappendicular
Trapezius
- Descending - Superior Nuchal line, - Lateral 1/3 of Accessory n.
part: external occipital clavicle. (CN XI) &
protuberance and trapezius
Nuchal ligament. branch from
- Transverse - Spinous processes of - Acromion. cervical plexus
part: C7-T3 vertebrae. (C3-C4)
- Ascending part: - Spinous processes of - Spine of
T4-T12 vertebrae. Scapula.
Spinous processes of
T6-T12 vertebrae,
Thoracolumbar fascia,
Posterior 1/3 of Iliac Crest of the Thoracodorsal
Latissimus Dorsi
crest and from 9th-12th Lesser tubercle. n. (C6-C8)
ribs.
Inconstant: inferior
angle of scapula.
Posterior tubercles of
Superior angle
Levator scapulae transverse processes of Dorsal
of scapula
C1-C4 vertebrae. Scapular n.
Spinous process of T1- Medial border of (C4-C5)
Rhomboid Major
T5 vertebrae. scapula (inf.)
Haytham Bayadsi 2008/2009
Spinous processes of Medial border of
Rhomboid Minor
C6-C7 vertebrae. scapula (sup.)
Muscle Origin Insertion Innervation
Scapulohumeral
Deltoid
- Clavicular part: - Lateral 1/3 of Deltoid Axillary n.
- Acromial part: clavicle. Tuberosity. (C4-C6)
- Spinal part:
- Acromion.
- Spine of scapula.
Supraspinous fascia Superior facet of
Supraspinatus and fossa of scapula. Greater
Tubercle. Suprascapular
Infraspinatus fossa of Middle facet of n. (C4-C6)
Infraspinatus scapula. Greater
Tubercle.
Middle part of Lateral Inferior facet of Axillary n.
Teres Minor border of scapula. Greater (C4-C6)
Tubercle.
Lower
Lateral border of Subscapular n.
Crest of Lesser
Teres Major scapula near inferior (C5-C6) OR
Tubercle.
angle. Thoracodorsal
n. (C6-C7)
Lower &
Upper
Subscapularis Subscapular fossa. Lesser Tubercle
Subscapular n.
(C5-C7)
Shoulder girdle muscle groups:
A) Anterior Axioappendicular.
B) Posterior Axioappendicular: 1) Superficial: Trapezius & Latissimus Dorsi.
2) Deep: Levator scapulae and rhomboids.
C) Scapulohumeral.
A+B = Extrinsic Shoulder C = Intrinsic Shoulder
Rotator Cuff Muscles (SITS): Form musculotendinous rotator cuff around
glenohumarl joint. Tendons blend and reinforce the fibrous layer of the joint capsule
(labrum) and maximize stability of the joint.
- Supraspinatus
- Infraspinatus
- Teres Minor
- Subscapularis
Haytham Bayadsi 2008/2009
Coracobrachialis muscle is an upper arm muscle but it can be also considered as a
shoulder girdle muscle that originates from Coracoid process of scapula and inserts on
the medial surface of the humerus (lower 2/3).
Haytham Bayadsi 2008/2009
Muscle Origin Insertion Innervation
Arm
Ventral Group
Ulnar Tuberosity
Distal 1/2 of Anterior
Brachialis and Coronoid
surface of Humerus
process.
Short Head: Coracoid Tuberosity of
Process. Radius + Fascia Musculo-
Biceps Brachii of forearm via cutaneous n.
Long Head: bicipital (C5-C7)
Supraglenoid Tubercle. aponeurosis.
Medial 1/3 of
Coracobrachialis Coracoid process medial surface of
humerus
Arm
Dorsal Group
Long Head:
Infraglenoid Tubercle.
Lateral Head:
Posterior surface of Olecranon of
Humerus, Superior to Ulna and
Triceps Brachii Radial groove Posterior wall of
Radial n. (C6-
Medial Head: joint capsule.
C8)
Posterior surface of
Humerus, Inferior to
Radial groove
Superior 1/4 of
Dorsal surface of Lateral
Anconeus dorsal side of
Epicondyle.
ulna.
Forearm, Ventral
Superficial
Humeral Head:
medial epicondyle of
Pronator
humerus (CFO)
Pronator Teres Tuberosity of
Ulnar Head:
Radius
Coronoid process of
ulna.
Flexor Carpi Medial Epicondyle of Base of 2nd
Radialis humerus (CFO) metacarpal
Median n. (C7-
Medail Epicondyle of Palmar
Palmaris Longus T1)
humerus (CFO) Aponeurosis
Flexor Digitorum Humeral Head:
Superficialis medial epicondyle of
humerus (CFO) Shafts of middle
Ulnar Head: phalanges of 2nd-
Coronoid process. 5th fingers.
Radial Head:
Superior 1/2 of Radius.
Haytham Bayadsi 2008/2009
Humeral Head:
Pisiform bone and
medial epicondyle of
via pisohamate
humerus (CFO)
Flexor Carpi ligament to the Ulnar n. (C7-
Ulnar Head:
Ulnaris Hook of Hamate T1)
Olecranon & Upper 2/3 th
and 5
of posterior margin of
metacarpal.
ulna.
Forearm, Ventral
Deep
Ulnar side:
Ulnar n. (C7-
Proximal 2/3 of palmar Bases of Distal
Flexor Digitorum T1)
surface of ulna & Phalanges of 2nd-
Porfundus Radial side:
interossious membrane. 5th fingers
Median n. (C7-
T1)
Anterior surface of Base of Distal
Flexor Pollicis
Radius and interossious phalanx of
Longus
membrane. Thumb. Median n. (C7-
Distal 1/4 of T1)
Distal 1/4 of anterior
Pronator Quadratus anterior surface of
surface of Ulna
Radius
Forearm, Dorsal
Superficial
Lateral surface of
Lateral supracondylar
Brachioradialis styloid process of
crest of humerus
Radius
Extensor Carpi Base of 2nd
Lateral supracondylar
Radialis Longus metacarpal
crest of humerus
(ECRL) (Dorsal aspect)
Extensor Carpi Base of 3rd
Radialis Brevis metacarpal
(ECRB) (Dorsal aspect) Radial n. (C5-
Lateral epicondyle of Extensor C8)
Extensor Digitorum humerus (CEO= Expansions of
common extensor origin) 2nd-4th fingers
Extensor
Extensor Digiti
Expansion of 5th
Minimi (EDM)
finger
Lateral epicondyle of Base of 5th
Extensor Carpi
humerus & posterior metacarpal
Ulnaris (ECU)
border of Ulna (Dorsal aspect)
Forearm, Dorsal
Deep
Lateral epicondyle of
Upper 1/3 of
Supinator humerus & Supinator
Radius
crest Radial n. (C5-
Posterior surface of C8)
Abductor Pollicis Base of 1st
Ulna, Radius and
Longus (APL) metacarpal
interossious membrane
Haytham Bayadsi 2008/2009
Extensor Pollicis Dorsal surface of Ulna & Base of 1st Distal
Longus (EPL) interossious membrane phalanx
Middle 1/3 of Ulna,
Extensor Pollicis Radius and interossious Base of 1st
Radial n. (C5-
Brevis (EPB) membrane (Dorsal Proximal phalanx.
C8)
aspect).
Posterior surface of Extensor
Extensor Indicis
distal 1/3 of ulna and expansion of 2nd
(EI)
interossious membrane finger.
Hand, Thenar
Abductor Pollicis Scaphoid tubercle & Base of proximal Median n. (C8-
Brevis Flexor retinaculum Phalanx of thumb T1)
Superficial
Superficial head: head: Median
Metacarpo-
Flexor retinaculum n. (C8-T1)
Flexor Pollicis phalangeal joint
Brevis of thumb (Radial
Deep head: Tubercle Deep Head:
sesamoid bone)
of Trapezium Ulnar n. (C8-
T1)
Tubercle of Trapezium Radial side of 1st Median n. (C8-
Opponens Pollicis
& Flexor retinaculum metacarpal T1)
Oblique head: bases
of 2nd & 3rd metacarpals Metacarpo-
and adjacent carpals phalangeal joint Ulnar n. (C8-
Adductor Pollicis
of thumb (Ulnar T1)
Transverse head: sesamoid bone)
shaft of 3rd metacarpal
Hand,
Hypothenar
Ulnar surface of
Abductor Digiti Pisiform & Pisohamate base of proximal
Minimi ligament phalanx of 5th
finger
Palmar surface of Ulnar n. (C8-
Flexor Digiti base of proximal T1)
Minimi Brevis Hook Hamate & Flexor phalanx of 5th
retinaculum finger
Opponens Digiti Ulnar margin of
Minimi 5th metacarpal
Hand,
Mesothenar
1st & 2nd : Radial 2
1st & 2nd:
tendons of Flexor
Median n. (C8-
Digitorum Porfundus
Extensor T1)
(Unipennate)
Lumbricals (4) expansions or
hoods 3rd & 4th:
3rd & 4th : Ulnar 3
Ulnar n. (C8-
tendons of FDP
T1)
(Bipennate)
Haytham Bayadsi 2008/2009
Bases of Proximal
Dorsal Interossei Adjacent sides of 2 Phalanges &
(4) metacarpals (Bipennate) extensor hoods of
2nd – 4th fingers.
Ulnar n. (C8-
Bases of Proximal
T1)
Palmar surfaces of 2nd, Phalanges &
Palmar Interossei
4th and 5th metacarpals extensor hoods of
(3)
(Unipennate) 2nd, 4th and 5th
fingers.
Intermuscular Speta: separate the ventral (Flexor) and dorsal (Extensor) groups of
muscles in the arm and forearm into compartments. (In the forearm also the
Interossious membrane between Radius and Ulna)
Medial and Lateral Bicipital grooves are grooves separating the Biceps Brachii
muscle from the Brachialis muscle on both sides of the arm. In the medial bicipital
groove we can find many formations such Blood vessels and nerves for the upper
limb. In the lateral bicipital groove we can find the cephalic vein running up to the
Deltopectoral groove/sulcus.
At the level of the medial bicipital groove, we can find the Basilic Hiatus, in which
the Basilic vein pierces the brachial fascia and becomes Sub-fascial position to join
the Brachial or Axillary veins.
Coracobrachialis muscle is pierced by the Musculocutaneous n.
Supinator muscle is pierced by the Radial n. (deep branch).
Median n. in the forearm first runs between the 2 heads of Pronator Teres muscle
and then runs inside the fascia of the Flexor Digitorum Superficialis in an Epifascial
position.
Haytham Bayadsi 2008/2009
Upper Limb
Joints
Haytham Bayadsi 2008/2009
Upper Limb Joints
In the Upper limb we must distinguish between:
- Pectoral (shoulder) Girdle (made by the scapulae x2 and the clavicles x2)
(incomplete bony ring).
- Free Upper limb (Humerus, Radius, Ulna, Carpals, Metacarpals and
Phalanges).
The pectoral girdle joints are the Sternoclavicular and Acromioclavicular. The
glenohumeral joint is between the upper free limb and the pectoral girdle.
The three joints function together to produce maximum range and flexibility of upper
limb and shoulder movements, usually all moves simultaneously, any lesion or defect
in one of these joints will impede and restrict the other 2.
Mobility of the scapula is essential for the movement of the upper limb, the clavicles
form the strut that holds the scapula, and the glenohumarl joint is away far from thorax
so it can move freely.
The clavicle establishes the radius at which the shoulder (half of pectoral girdle – 1
clavicle and 1 scapula – and glenohumarl joint) rotates at the sternoclavicular joint.
The remaining movement at the acromioclavicular joint is for positioning the glenoid
cavity that is necessary for arm movements.
1) Sternoclavicular joint:
- Ball & socket (spheroidal) by definition but functionally its limited.
3 axes joint that produces rotation and Circumduction.
- Articulation between the sternal end of the clavicle with the manubrium of
sternum at 1st costal cartilage.
- The joint contains an articular disk (serves as shock absorber of forces
transmitted through clavicle from upper limb).
- Articular surfaces covered with fibrocartilage, joint capsule surrounds the joint,
attached to the margins. Synovial membrane lines the fibrous layer of capsule.
- Ligaments: Establishes the strength of the SC joint
Anterior + Posterior sternoclavicular ligaments.
Interclavicular ligaments.
Costoclavicular ligaments- (Limits the elevation of pectoral girdle).
- Movements of the joint:
Elevation / Depression (along saggital axis) (~60º)
Forward and backward rotation of clavicle (along transverse axis)
Protraction / Retraction (along vertical axis) (~30º)
Circumduction (produced from both movements above)
- Blood supply: internal thoracic artery, suprascapular artery.
- Nerve supple: supraclavicular n. branch.
Haytham Bayadsi 2008/2009
2) Acromioclavicular joint:
- Plane type of joint that functions as a very limited Ball & socket (spheroidal).
3 axes of movement, Mobility at the AC joint allows the scapula to move in
three dimensions so that it follows the contours of the ribcage. After all, the
scapula must move on the ribcage, and the ribcage is not flat!
- Articulation between the Acromial end of the clavicle and the Acromion of
scapula.
- The joint contains an incomplete articular disk.
- Articular surfaces covered with fibrocartilage, joint capsule is relatively loose,
attached to the margins of articular surfaces. Synovial membrane lines the
fibrous layer.
- Ligaments: Acromioclavicular ligament: strengthens superiorly.
Coracoclavicular ligament: strong pair of bands:
- Vertical Conoid ligament (triangle shaped).
- Horizontal Trapezoid ligament.
Also provides passive suspension of scapula and free limb from
clavicle and prevents dislocation.
Coracoacromial ligament (belongs also to glenohumarl joint).
Haytham Bayadsi 2008/2009
- Movements of the joint: The scapula moves around each of the three acromioclavicular
axes:
The scapula Protracts & Retracts (Wings) around a vertical axis
The scapula can be Elevated & Depressed in a Frontal plane
The scapula tips around a transverse axis.
The scapula rotates upward or downward around saggital axis through the
joint's capsule.
- Blood Supply: Suprascapular and thoracoacromial arteries.
- Nerve Supply: Supraclavicular and Axillary nerves.
Haytham Bayadsi 2008/2009
3) Glenohumeral Joint (Shoulder joint):
- Ball & socket type of joint (shperoidal). 3 axes of movement. Free moving.
- The large round humeral head articulates with the shallow glenoid cavity of scapula. (3:1
ratio in size)
- Fibrocartilage glenoid labrum (lip): around the margins of glenoid cavity, deepens and
enlarges the shallow cavity. Hylaine cartilage covers the articular surfaces.
- The joint capsule attaches around the neck of scapula and around the anatomical neck of
Humerus. Has a synovial membrane lining it and contains 2 apertures:
Opening between the tubercles of humerus for the tendon of long head of
biceps brachii that passes through the fibrous layer of the joint capsule when
originating from the supraglenoid tubercle.
anterior opening, under coracoid process that communicates with the
subscapular bursa.
The join cavity contians the Axillary recess inferiorly, which is importand to
allow the elevation of the upper limb without stretching the joint capsule
The joint is reinforced superiorly by the Coracoacromial arch and on the sides by the
glenohumaral ligaments, plus, the Rotator cuff muscles SITS play an important role in
strengthening the joint superiorly and holding the head of humerus into postion. So the
weakest point in the joint is inferiourly, a location where the dislocation of the head of
humerus occurs the most.
- Ligaments: Coracohumeral ligament: strengthens superiorly.
Glenohumeral ligaments: 3 fibrous bands, strengthens the caspule
anteriorly.
Transverse humeral ligament: hold the tendon of long head of biceps
inside the intertubercular sulcus.
Coracoacromial ligament: forms the coracoacromial arch together
with the acromion and coracoid process.
Extremly strong extrinsic protective arch above the head of humerus,
preventing superior dislocation (like when standing on a desk with your
arms pushing it).
- Bursae: Subscapular bursa:
between the tendon of subscapularis muscle and the neck of scapula.
Communicates with joint cavity anteriorly.
Subacromial bursa (subdeltoid):
between the acromion, coracoacromial ligament and deltoid superiorly
and the supraspinatus tendon and joint caspule inferiorly. Facilates the
movement of the supraspinatus tendon under the coracoacromial arch, and
the Deltoid movement over the greater tubercle.
- Movements: free moving joint, 3 axes:
Anteversion / Retroversion (Anteflexion / Retroflextion) along transverse axis.
Abduction / Adduction along saggital axis.
Outward (lateral) / Intward (medial) Rotation along vertical axis.
The combination of these 3 types of movements produces circumduction.
Haytham Bayadsi 2008/2009
Note: The abduction is limited anteriouly untill 90º and lateraly untill 75º due the
greater and lesser tubercles touching the Coracoacromial arch. Beyond that, we will
need the scapula to move with the humerus to produce Elevation of the arm.
- Blood supply: Anterior and Posterior circumflex humeral arteries.
- Nerve supple: Suprascapular, Axillary and lateral pectoral nerves.
Muscle Effects on the Shoulder joint and Pectoral girdle
Effect on the Arm (Shoulder Joint)
Antiflexion Retroflexion Abduction Adduction Inward Rot. Outward Rot.
To Horizontal plane Max. 40º Max. 90º Max. 70º Max. 60º
Pectoralis Maj. Deltoid Pectoralis Maj.
Lattisimus Dorsi Subscapularis Infraspinatus
Calvicular part Acromial part Sternocostal pt.
Deltoid Deltoid
Suprapinatus Lattisimus Dorsi Teres Major Teres Minor
Calvicular part Spinal part
Biceps Brachii Deltoid
Biceps Brachii Teres Major Teres Major Pectoralis Maj.
Long Head Spinal part
Triceps Brachii Trapzeius
Coracobrachialis Coracobrachialis Lattisimus Dorsi
Long Head Descending part
Deltoid
Pectoralis minor Trapezius (Indirect) Pectoralis minor
Clavicular part
Elevation of Arm
Up to 160º - 180º
Serratus Anterior
Trapezius
Descending part
The clavicular and Spinal parts of the Deltoid promote Adduction untill the horizontal plane and
above that they provide abdution insted.
Effect on Pectoral girdle and Scapula movements (sternoclavicular and
acromioclavicular joints)
Protraction Retraction Elevation Depression Upward Rot. Downward Rot.
Serratus Anterior Trapezius Trapezius Trapezius Trapezius Lattisimus Dorsi
Transverse part Descendig part Ascending part Descending part
Pectoralis Maj. Rhomboids Levator Scapulae Pectoralis minor Trapezius Rhomboids
Ascending part
Pectoralis Minor Lattisimus Dorsi Sternocliedomastoid Lattisimus Dorsi Serratus Anterior Pectoralis Major
Inferior part Abdominal part
Rhomboids Pectoralis Maj. Pectoralis Minor
Abdominal part
Serratus Anterior
Inferior part Gravity
Gravity
- Elevation: Muscles elevating the Acromial end of clavicle and scapula: (max. 40º)
- Depression: Muscles depressing the Acromial end of clavicle and scapula: (max. 10º)
- Protraction: Muscles moving the Acromial end of the clavicle forwards and the scapula ventro-
laterally: (25-30º)
- Retraction: Muscles moving the Acromial end of the clavicle backward and the scapula dorso-
medially: (20-25º)
- The winging and tipping of scapula is a modified moves from the basic moves of
scapula (protraction/retraction, elevation/depression and rotation)
Haytham Bayadsi 2008/2009
Haytham Bayadsi 2008/2009
4) The Elbow joint:
- Hinge type of joint, 1 axis of movement through the condyles of humerus.
* The humeroradial articulation is ball & socket, but restricted functionally into hinge by
the collateral ligaments.
- The spool shaped Trochlea and Spheroidal Capitulum of the humerus articulate with the
trochlear notch of the Ulna and the Superior articular surface of Radius respectively,
making the Humeroulnar and Humeroradial joints that compose the Elbow joint.
- The articular surfaces are covered with Hyaline cartilage. The fibrous joint capsule is
attached to the humerus at the margins of lateral and medial ends of the Capitulum and
trochlea and proximal to the Coronoid process anteriorly, and posteriorly it reaches above
the Olecranon fossa. Synovial membrane lines it from the inside. The capsule is weak
anteriorly and posteriorly but strengthened laterally by the collateral ligaments.
- In the supination position, there is a carrying angle between the Radius and humerus
laterally which is about 170º, more pronounced in women.
- Angle of excursion: angle measured between the upper arm and forearm at maximal
extension. Females: 180° males: 175°. (At maximal flexion: 35°).
- Ligaments: Lateral Radial Collateral ligament:
Fan like, blends with the annular ligament.
Medial Ulnar Collateral ligament:
Consists of 3 bands: * Anterior cord like band, * Posterior fan like
band, and the * Oblique band which deepens the socket for the trochlea
of humerus.
Annular ligament of the Radius: encircles and holds the head of radius
in the radial notch of Ulna, forming proximal Radioulnar joint.
- Bursae: Intratendinous Olecranon bursa: in the tendon of triceps Brachii.
Subtendinous Olecranon bursa: between Olecranon and the triceps
tendon.
Subcutaneous Olecranon bursa: in the subcutaneous connective tissue,
above Olecranon.
Bicipitoradial bursa: between Biceps Brachii tendon and radial
tuberosity.
- Movements: 1 axis (transverse)
Flexion / Extension
- Blood supply: the anastomosis between radial, Ulnar and brachial arteries around the
elbow.
- Nerve supply: Musculocutaneous, radial and ulnar nerves.
Flexion: Biceps Brachii Brachialis Brachioradialis Pronator Teres
Extension: Triceps Brachii Anconeus
Haytham Bayadsi 2008/2009
5) Proximal Radioulnar Joint:
- Pivot type of joint. 1 rotatory axis.
- The articular circumference of the head of the Radius articulates with the Radial notch of
the Ulna. The head of radius is held in position by the annular ligament of the head of
Radius.
This joint allows the movement of the Head of Radius on the Ulna.
- The fibrous capsule is continuous with elbow joint. The Synovial membrane continues
distally as a sacciform recess under the annular ligament. (so the head of Radius wont
tear or damage the membrane while rotating)
- Ligaments: Annular ligament of Head of Radius.
- Movements: 1 axis, (Oblique line, from the center of the head of Radius until the styloid
process of Ulna).
Supination / Pronation
- Blood supply: Periarticular arterial anastomosis of the elbow joint.
- Nerve supply: Musculocutaneous, Median, and Radial nerves.
Haytham Bayadsi 2008/2009
6) Distal Radioulnar Joint:
- Pivot type of joint. 1 rotatory axis.
- Rounded head of Ulna articulates with the ulnar notch on the Radius.
The joint allows the movement of the Head of Ulna on the Radius.
- The joint has a fibrocartilaginous articular disk (triangular ligament), that binds the ulna
and the radius at the distal end.
- The joint cavity is L-Shaped, the joint capsule is deficient superiorly, and the Synovial
membrane extends as a sacciform recess of the distal RU joint.
- Ligaments: Anterior and Posterior Radioulnar ligaments.
- Movements: 1 axis, (Oblique line, from the center of the head of Radius until the styloid
process of Ulna).
Supination / Pronation
- Blood supply: anterior and posterior interossious arteries.
- Nerve supply: anterior and posterior interossious nerves.
Supination: Supinator Biceps Brachii EPL ECRL
Pronation: Pronator Teres Pronator Quadratus FCR
* Brachioradialis muscle: brings arm into mid-position (like the army Salute)
EPL: Extensor Pollicis longus
ECRL: Extensor Carpi Radialis longus
FCR: Flexor Carpi Radialis
Haytham Bayadsi 2008/2009
7) The Wrist (Radiocarpal) Joint:
- Ellipsoid or Condyloid type of Joint. 2 axes of movements.
- Articulation between the carpal articular facet of the Radius + the articular disk and the
proximal row of the carpal bones except the Pisiform bone.
* The triquetrum bone participates and contacts the articular disk only in ulnar abduction
and loses contact in radial abduction!
** Ulna doesn’t participate in the joint!!!
- The fibrous capsule attaches to the distal ends of radius and ulna and proximal row of
carpals except Pisiform. Synovial membrane lines the internal surface of the fibrous layer
with many Synovial folds.
- Ligaments: Palmar and Dorsal Radiocarpal ligaments:
From the radius to the 2 carpal rows. Strong and makes the following of
hand to forearm possible during Supination / Pronation.
Ulnar Collateral ligament: strengthens medially.
Radial Collateral ligament: strengthens laterally.
- Movements: 2 axis joint:
Palmarflexion / Dorsiflexion (Transverse Axis through Lunate and Capitate)
Adduction (Ulnar Abduction) / Abduction (Radial Abduction) the axis is (Dorso-
palmar through the head of Capitate)
Combined motions produce rotation.
- Blood Supply: Dorsal and Palmar carpal arches.
- Nerve Supply: Median, Radial and Ulnar nerves (interossious branches).
Adduction Abduction Palmarflexion Dorsiflexion
(35-40º) (25-30º) (60-90º) (40-90º)
Extensor Carpi Ulnaris Extensor Carpi Radialis longus Flexor Carpi Radialis Extensor Carpi Radialis longus
Flexor Carpi Ulnaris Extensor Carpi Radialis Brevis Flexor Carpi Ulnaris Extensor Carpi Radialis Brevis
Abductor Pollicis longus Abductor Pollicis longus Extensor Carpi Ulnaris
Flexor Carpi Radialis Flexor of the digits Extensors of the digits
Deep and superficial (assistance)
* * Dorsiflexion is aided by midcarpal joint
Haytham Bayadsi 2008/2009
Haytham Bayadsi 2008/2009
8) Intercarpal Joints:
- Plane type of joints, connecting the carpal bones with each other.
- 3 types: 1) Joints between carpal bones of proximal row.
2) Joints between carpal bones of distal row.
3) Midcarpal joint, S-shaped between proximal and distal rows.
4) Pisotriquetral joint, between Pisiform and palmar surface of triquetrum.
- Joint capsule (Fibrous and Synovial layers) is common and continuous formed by the
Intercarpal joints and the carpometacarpal joints except the 1st carpometacarpal joint of
thumb (This continuity is very significant in spread of infections and in arthroscopy).
- Ligaments: Dorsal / Palmar Intercarpal ligaments.
Interossious Intercarpal ligaments.
Pisohamate ligament.
Radiate carpal ligament.
- Movements:
Gliding movements between the carpal bones, which occur together with the
movements of the Radiocarpal (wrist) joint and augment them and increase the
overall range of mobility and flexibility
Palmarflexion / Dorsiflexion at the Midcarpal joint, aiding the wrist joint and
initiating it moves. Some investigators say that the Dorsiflexion and radial
abduction occur in this joint only. Proximal row is more flexible than the distal one.
- Blood supply: Dorsal and palmar carpal arches.
- Nerve supply: Dorsal / deep branches of ulnar nerve.
Haytham Bayadsi 2008/2009
9) Carpometacarpal (CMC) and Intermetacarpal (IM) Joints:
- Plane type of joints, except for the 1st CMC joint of the thumb, which is Saddle joint.
- The distal surfaces of the carpals of the distal row articulate with the carpal surfaces of
the bases of the metacarpals at the CMC joints. The CMC joint of the thumb is between
the Trapezium and the base of the 1st metacarpal bone. Adjacent metacarpals articulate
with each other at the IM joints at the Ulnar and radial sides of their bases.
- The medial 4 CMC joints and the IM joints have a common joint cavity and capsule. The
1st CMC joint of the thumb has a separate loose joint capsule (Fibrous and Synovial
layers) that facilitates the free movements of the joint.
- Ligaments: Palmar / Dorsal CMC ligaments.
Pisometacarpal ligament.
Palmar / Dorsal IM ligaments.
Interossious IM ligaments.
- Movements: Almost no movements occur at CMC joints (slight at the 5th).
In a tight grasp of the hand, 2/3 of the movement occur at the
CMC joint of the thumb and 1/3 of the movement occur at the
CMC joint of the 4th and 5th CMC joints.
The 1st CMC joint of the thumb is a 2 axes joint allowing:
- Abduction / Adduction of the thumb. (Dorso-palmar axis)
- Opposition / Reposition of the thumb (only in humans and human
shaped monkeys) (vertical axis in the anatomical position)
- Combined movements of the above producing Circumduction.
** Please note that the Flexion / Extension movements of the thumb do
exist, but they do not occur at the CMC joint of the thumb, instead they
occur at the Metacarpo-phalangeal and Interphalangeal joints of the
thumb. (Don’t mix them with the opposition/reposition!).
- Blood supply: Dorsal/palmar carpal arches, deep palmar arch and MC arteries.
- Nerve supply: Interossious branch of Median and Radial nerves, and branches of Ulnar
nerve (deep, dorsal).
Adduction of thumb Abduction of thumb Opposition of thumb Reposition of thumb
35-40º
Adductor Pollicis Abductor Pollicis longus Opponents Pollicis Abductor Pollicis longus
Extensor Pollicis longus Abductor Pollicis Brevis Adductor Pollicis Extensor Pollicis longus
1st Dorsal interossious Opponens Pollicis Flexor Pollicis Longus Extensor Pollicis Brevis
Flexor Pollicis Brevis Flexor Pollicis Brevis
Superficial Head
Haytham Bayadsi 2008/2009
10) Metacarpophalangeal (MP) joints:
- Spheroidal (Ball & Socket) shaped joints but restricted into 2 axes (ellipsoid
functionally).
- Heads of metacarpals articulate with bases of proximal phalanges.
- Joint capsule attaches to the margins of articulation (Fibrous and Synovial layers).
- Ligaments: Collateral ligaments (Medial & Lateral), has 2 parts:
- Dense Cord-like: passes from heads of MC to base of Phalanges,
prevents spreading of fingers during flexion.
- Thin Fan-like: passes anteriorly to attach to palmar plates.
Palmar ligaments or Plates: dense fibrous plates form the palmar
aspect of the joint. Provide smooth longitudinal groove that allows the
long flexor tendons to glide in and remain centrally placed as they cross
the joint cavity.
Superficial and Deep transverse metacarpal ligaments: hold the
metacarpals together at the distal ends, limits the moves of the CMC and
IM, and MP joints and prevents excessive spreading of fingers.
Extensor hood: attaches anteriorly to the sides of the palmar plates of
MP joints.
- Movements: Flexion / Extension (Transverse axis)
Abduction / Adduction (in relation to the middle finger, away from it
is abduction, towards it is adduction).
Combined movements of the above to produce Circumduction
* 1st MP joint of thumb has only Flexion / Extension.
11) Interphalangeal (IP) joints:
- Hinge type of joints. 1 axis of movement.
- Heads of phalanges articulates with the bases of the more distally located phalanges.
- Joint capsule attaches to the margins of articulation (Fibrous and Synovial layers).
- Ligaments: Collateral ligaments (Medial & Lateral), has 2 parts:
- Dense Cord-like: passes from heads of phalanges to base of
the more distal Phalanges.
- Thin Fan-like: passes anteriorly to attach to palmar plates.
Palmar ligaments or Plates: dense fibrous plates form the palmar
aspect of the joint. Provide smooth longitudinal groove that allows the
long flexor tendons to glide in and remain centrally placed as they cross
the joint cavity.
- Movements: 1 axis (Transverse) joint:
Flexion / Extension
- Blood supply of MP and IP joints: Deep digital arteries.
- Nerve supply of MP and IP joints: Digital nerves (from ulnar and median nerves).
Haytham Bayadsi 2008/2009
The movements of the thumb
At the 1st CMC joint of the thumb:
Adduction of thumb Abduction of thumb Opposition of thumb Reposition of thumb
35-40º
Adductor Pollicis Abductor Pollicis longus Opponents Pollicis Abductor Pollicis longus
Extensor Pollicis longus Abductor Pollicis Brevis Adductor Pollicis Extensor Pollicis longus
1st Dorsal interossious Opponens Pollicis Flexor Pollicis Longus Extensor Pollicis Brevis
Flexor Pollicis Brevis Flexor Pollicis Brevis
Superficial Head
At MP and IP joints of the thumb:
MP joint of thumb IP joint of thumb
Flexion Flexor Pollicis longus Flexor Pollicis longus
Max. 70º at MP joint Flexor Pollicis Brevis
Max. 40º at IP joint
Extension Extensor Pollicis longus Extensor Pollicis longus
Extensor Pollicis Brevis
The movements of the proximal phalanges of the 2nd to 5th fingers (MP joints)
Flexion Extension Abduction Adduction
90° (Hyperextension) 20° Max. 40°
Flexor Digitorum Superficialis Extensor Digitorum Dorsal Interossious Palmar interossious
Flexor Digitorum Porfundus Extensor Indicis Abductor Digiti Minimi Extensor Indicis
Lumbricals Extensor Digiti Minimi Extensor Digiti Minimi
Flexor Digiti Minimi
The movements of the middle and distal phalanges of the 2nd to 5th fingers (IP
joints)
Proximal IP joint Distal IP joint
Flexion Flexor Digitorum Superficialis Flexor Digitorum Porfundus
Max. 110º at proximal IP joint Flexor Digitorum Porfundus
Max. 90º at distal IP joint
Extensor Digitorum Extensor Digitorum
Extension Extensor Indicis Extensor Indicis
5º at distal IP joint Extensor Digiti Minimi Extensor Digiti Minimi
Lumbricals Lumbricals
Haytham Bayadsi 2008/2009
Haytham Bayadsi 2008/2009
This page is taken from Dr. M. Kálmán's lecture, EM, Oct. 10, 2006-10:
Motto 1: The bones are inserted between the muscles, not the muscles are hinged up on
the bones
Some muscles form chains interrupted by bones, e.g.
Serratus anterior – rhomboids;
Trapezius – deltoid;
Motto 2: The muscles have formed for three-dimensional biological movements, only
their descriptions occur according to the coordinate system of Descartes.
See below the actions of the biceps and the Latissimus Dorsi.
Motto 3: Not an individual muscle but the whole musculature moves.
See lumbalgic attack in upper limb abduction.
Why are there several muscles for the same movement?
Different phases of the same movement: Supraspinatus – deltoid.
Stabilizing and adapting the insertion (chain-action): trapezius – deltoid.
Compensation of unnecessary effects: two heads of biceps;
Thoracoscapular muscles
Controlling the movement: Scapulohumeral - deltoid
Different biological situations: biceps – Brachialis;
Trapezius – Serratus anterior.
Different points of reference: Teres major (to the scapula) – Latissimus Dorsi (to the ribs).
Why are there several effects of one muscle?
There is always only one movements but in three dimension.
Several muscles bridge over two joints (but of common action: shoulder and elbow).
Different parts have different movements: see deltoid, trapezius.
Depending on the position: flexion or rotation by the deltoid.
Depending on the synergists: Latissimus with Pectoralis maj., versus with rhomboids.
Depending on the point fixed: see accessory respiratory movements.
The movements are components of the same action:
Biceps: shoulder flexion, elbow flexion, hand supination ------------- pick and eat it.
Latissimus: shoulder retroflexion, adduction, inward rotation ------- ass-scratching.
Note: there is no „perfect” table on the muscle movements, because:
-The opinions are speculative (i.e. from the anatomical positions) rather than supported by
electromyography.
- The movements change with the position of the limbs.
-There is no general agreement, which minimal movements are not to taken into
consideration.
The most important movements, however, are identically described everywhere.
Haytham Bayadsi 2008/2009
Upper Limb
Fascia
Haytham Bayadsi 2008/2009
Fascia of the Upper Limb:
The Deltoid muscle is covered by the deltoid fascia, which continues inferiorly with the
pectoral fascia and the dense Infraspinatus fascia posteriorly. The Pectoralis major is covered
by the Pectoral fascia.
The Claviopectoral fascia stretches from the clavicle, Coracoid process and extends
downward enclosing the Subclavius muscle then the Pectoralis minor (between them its called
costocoracoid membrane or ligament) and inferiorly it becomes continuous with the Axillary
fascia as the Suspensory Ligament of the Axilla, which supports the Axillary fascia and pulls it
with the skin upward, forming the Axillary fossa. The Claviopectoral fascia divides the
Deltopectoral triangle into 2 compartments: Superficial & Deep.
The Superficial Pectoral fascia covers the Pectoralis major muscle, which continues to the
Axillary region to become the Superficial Axillary fascia (base-floor of Axillary fossa with
skin). The Deep pectoral fascia covers the Pectoralis major muscle form the inside.
Note: please check the Netter atlas, Plate 428 for this fascia and drawing
The Brachial fascia is a continuation of the deltoid, pectoral, Infraspinatus & Axillary fascias
and attaches inferiorly to the humeral epicondyles & Olecranon of ulna and extends
downwards as the fascia of forearm.
The fascia sends 2 speta that attach along the medial & lateral sides of humeral shafts and
supracondylar ridges, the Medial & Lateral Intermuscular Speta respectively. These 2 septa
divide the arm into anterior flexor & posterior extensor muscular compartments
The fascia is pierced in the middle of the arm and medially by the Basilic vein, reaching
the one of the brachial veins via the Basilic Hiatus
The Medial and Lateral Bicipital grooves are grooves separating the Biceps Brachii muscle
from the Brachialis muscle on both sides of the arm.
In the cubital region it's known as the cubital fascia, separating the superficial structures
from the deep structures in the cubital fossa.
The Antebrachial fascia is the continuation of the brachial fascia in the forearm. In the
forearm we don’t have Intermuscular septa separating the different extensors from the
flexors. But we can say that the border between the extensor and the flexor compartment
laterally is the Brachioradialis muscle, and medially is the Flexor Digitorum Profundus.
Note: Check this in the Netter atlas, Plate 449, the 2nd cross section (middle one)
Distally, the Antebrachial fascia has 2 layers: Superficial & Deep:
* The superficial layer is the normal Antebrachial fascia covering the forearm
muscles
* The deep layer of the Antebrachial fascia forms the Palmar or Volar carpal
ligament ventrally, and the Extensor Retinaculum Dorsally.
The Palmar fascia covers the Thenar & Hypothenar compartments in the palm, but the central
Mesothenar compartment is covered by the Palmar Aponeurosis.
Haytham Bayadsi 2008/2009
The palm of the hand is subdivided by the Medial, Intermediate & Lateral Palmar Septa
(extensions of the Palmar Aponeurosis) into 3 regions: Thenar Eminence, the Mesothenar or
Central compartment and the Hypothenar Eminence.
The Palmar fascia extends dorsally as the Dorsalis Palmaris fascia covering the Dorsum of the
hand.
Haytham Bayadsi 2008/2009
Haytham Bayadsi 2008/2009
Upper Limb
Regions &
Special
Formations
Haytham Bayadsi 2008/2009
Regional Anatomy of the Upper Limb and Special structures:
1) Infraclavicular Region:
Skin Innervation: Medial & Intermediate Supraclavicular nerves from cervical plexus
This region includes the Deltopectoral (Calviopectoral) Triangle, which is the proximal
divergence of the narrow Deltopectoral Groove, and its borders are:
Superior: Clavicle
Lateral: Deltoid muscle
Medial: Pectoralis Major
The Deltoid muscle is covered by the Deltoid fascia, and the Pectoralis major is covered by
the Pectoral fascia, after the removal of the fascia and reflecting the Clavicular part of the
Pectoralis major muscle we can expose the Deltopectoral triangle more clearly and see its
contents.
The Claviopectoral fascia stretches from the clavicle, Coracoid process and extends
downward enclosing the Subclavius muscle then the Pectoralis minor (between them its called
costocoracoid membrane or ligament) and inferiorly it becomes continuous with the Axillary
fascia as the Suspensory Ligament of the Axilla, which supports the Axillary fascia and pulls it
with the skin upward, forming the Axillary fossa. The Claviopectoral fascia divides the
Deltopectoral triangle into 2 compartments: Superficial & Deep.
In the Superficial Layer the Cephalic vein reaches the Deltopectoral triangle from the
groove, accompanied by the Deltoid branch of the Thoraco-acromial artery trunk and
penetrates the Calviopectoral fascia to end up in the Axillary vein. The thoraco-acromial
trunk (with its branches: Clavicular, Acromial, Pectoral & Deltoid) and the Pectoral nerves
can be found in the superficial layer as well next the cephalic vein.
In the Deep Layer (under the Calviopectoral fascia) we can find the main vessels and nerves
that supply the upper limb. From medial to lateral we can find:
Axillary vein
Axillary artery
3 nerve cords of Brachial plexus. (Lateral, Posterior & Medial)
Upper border of Pectoralis Minor attaching to Coracoid process (The Axillary
vessels & brachial plexus nerves go under it)
Suprascapular a/v/n (deep lateral part)
**Note:
The Pectoral Region can be included with the Infraclavicular region in some sources,
although it's not really a part of the upper limb, but it contains Thoracoappendicular muscles
that inserts on the upper limb. So just in any case we shall discuss it:
Haytham Bayadsi 2008/2009
2) The Pectoral Region:
Borders: Superior: Clavicle
Lateral: Deltopectoral Sulcus (groove)
Inferior: Inferior margin of Pectoralis Major
Medial: lateral border of Sternum
Skin Innervation:
Supraclavicular nerves (Medial & Intermediate)
Anterior Cutaneous branches of the Intercostal nerves 1-6
After the removal of the skin we find the Superficial Pectoral fascia covering the Pectoralis
major muscle, which continues to the Axillary region to become the Superficial Axillary
fascia (base-floor of Axillary fossa with skin). The Deep pectoral fascia covers the Pectoralis
major muscle form the inside.
After the removal of the Pectoralis major muscle and it's fascia we find the Pectoralis Minor
fascia (embedded in the Claviopectoral fascia). The Pectoralis minor muscles lies over the
Axillary vessels and brachial plexus cords & it must be removed to dissect them. This muscle
divides the Axillary artery into 3 parts, and in each part we have 2 different branches of the
Axillary artery:
Proximal to the muscle, 1st part: 1. Superior Thoracic artery
2. Thoraco-acromial artery / Trunk
Under the muscle, 2nd part: 3. Lateral Thoracic Artery
4. Subscapular Artery
Distal to the muscle, 3rd part: 5. Anterior Circumflex Humeral artery
6. Posterior Circumflex Humeral artery
The Superior Thoracic artery originates near the first rib and supplies the superior chest
muscles, the Thoraco-acromial originates as a trunk that pierces the costocoracoid
membrane with 4 branches: Clavicular, Acromial, Pectoral & Deltoid. The Lateral thoracic
artery runs on the lateral side of the chest on the Serratus anterior muscle with the Long
thoracic nerve. The Subscapular artery is the biggest branch and divides into 2 important
branches:
1. Circumflex scapular artery: which goes through the medial triangular space to the
dorsal scapular region around the lateral border of scapula to anastomose with the
Suprascapular artery (branch of the thyrocervical trunk of Subclavian artery) & the Dorsal
Scapular artery (branch of transverse cervical artery, found on the medial margin of
scapula) under the Infraspinatus muscle on the Infraspinatus fossa of the scapula.
Clinically, this is a very important anastomosis, in case of damage or obstruction of the
Axillary artery, the blood can still reach the upper limb via this anastomosis
2. Thoracodorsal artery: runs together with the Thoracodorsal nerve to supply the
Latissimus Dorsi muscle
The Anterior & Posterior Circumflex Humeral arteries anastomose also with each other
around the surgical neck of humerus. The posterior circumflex humeral artery goes behind the
neck of humerus via the Quadrangular Space together with the Axillary nerve & also
anastomosis inferiorly via the descending branch with the Profunda Brachii branch of the
brachial artery & superiorly with the Acromial artery via the ascending branch.
Haytham Bayadsi 2008/2009
3) The Axillary Region:
Or also known as the Axilla, a Pyramidal space under the glenohumarl joint, with and apex,
open base (covered by concave skin) & 4 solid walls found on the junction between the arm &
the thorax.
It can be considered as a distribution center for the neurovascular structures passing through it.
Borders of the Axilla:
Apex: Cervicoaxillary Canal, passage between neck & Axilla, formed between the
1st rib, clavicle and superior border of scapula.
Base: open, formed by the concave skin, subcutaneous tissue and Axillary (deep)
fascia extending from the arm to the thoracic wall at the level of 4th rib, forming the
Axillary fossa (armpit) which is bordered anteriorly by the Anterior Axillary fold, and
posteriorly by the Posterior Axillary fold
Anterior Wall: formed by the Pectoralis Major & Minor muscles, together with
the pectoral & Calviopectoral fascia associated with them.
The Anterior Axillary fold is the lowest part of the anterior wall that can be grabbed
by the fingers, and it's formed by the Pectoralis major muscle only
Posterior Wall: formed by the Scapula & Subscapularis muscles lying on it
superiorly and the Teres Major & Latissimus Dorsi muscles inferiorly. The posterior
Axillary fold in the lowest part formed by the muscles only and can be grabbed by the
fingers
Medial Wall: formed by the thoracic wall (1st – 4th ribs and Intercostal muscles)
and the overlying Serratus anterior muscle
Lateral Wall: formed by the Intertubercular groove of the Humerus with the
Long tendon of Biceps Brachii running in it.
Connections of the Axilla:
Cervicoaxillary canal superiorly to the root of neck (or from)
Calviopectoral triangle (and fascia) anteriorly to the pectoral region
Inferolaterally to the Upper limb
Quadrangular space posteriorly to the scapular region
Inferomedially along thoracic wall to the Serratus anterior & Latissimus Dorsi
muscles
Contents of the Axilla:
Axillary blood vessels (artery, vein) and their branches
Lymphatic vessels & Axillary lymph nodes
Brachial Plexus Cords with branches: Pectoral nerves, Subscapular nerve & Long
Thoracic nerve
Tendon of Coracobrachialis muscle
Short Head of Biceps Brachii
* Skin Innervation: Intercostobrachial anastomosis between the 2nd Intercostal nerve and the
medial brachial cutaneous nerve, very important to anesthetize it in breast surgeries
Haytham Bayadsi 2008/2009
4) The Deltoid Region:
Borders: Anteriorly: Deltopectoral Groove
Posteriorly: Posterior margin of the Deltoid & posteriorly, origin of the
deltoid muscles
Skin innervation:
Lateral Supraclavicular nerves
Superior Lateral Brachial Cutaneous nerve (from Axillary nerve)
The Deltoid muscle is covered by the deltoid fascia, which continues inferiorly with the
pectoral fascia and the dense Infraspinatus fascia posteriorly.
If we remove the Spinal part of the Deltoid muscle and reflect it upwards, we can see 3 spaces
formed by the Teres major, Teres minor, Long Head of Triceps muscle and the Humerus.
Haytham Bayadsi 2008/2009
1) Quadrangular Space:
Borders: - Superiorly: Teres Minor
- Inferiorly: Teres Major
- Medially: Long Head of Triceps Brachii
- Laterally: Surgical Neck of Humerus
Contents: - Axillary nerve
- Posterior circumflex humeral artery
2) Medial Triangular Space:
Borders: - Superiorly: Teres Minor
- Inferiorly: Teres Major
- Laterally: Long Head of Triceps Brachii
Contents: - Circumflex Scapular artery (branch of Subscapular artery)
3) Lateral Triangular Space:
Borders: - Superiorly: Teres Major
- Medially: Long Head of Triceps Brachii
- Laterally: shaft of Humerus & Lateral head of Triceps Brachii
Contents: - Radial nerve
- Deep branch of brachial artery (Profunda Brachii artery)
** Note:
The Quadrangular & Medial Triangular spaces are often referred to as Lateral & Medial
Axillary spaces or Hiatuses.
Haytham Bayadsi 2008/2009
5) Dorsal Scapular Region:
Borders: Superior: along the side of the Acromion to the 7th cervical vertebra
Medial: the midline of the body.
Inferior: along the side of the inferior angle of the scapula
(Transverse line)
Lateral: a longitudinal line from the Acromion
Skin innervation:
Dorsal Rami of Spinal Nerves
Just a quick revision of the Ligaments of the Scapula for this region:
o The Coracoacromial Ligament: This ligament is a strong triangular band, extending
between the Coracoid process and the Acromion. This ligament, together with the Coracoid
process and the Acromion, forms a vault for the protection of the head of the humerus
(Coracoacromial arch). It is in relation, above, with the clavicle and under surface of the
Deltoid; below, with the tendon of the Supraspinatus, a bursa being interposed. Its lateral
border is continuous with a dense lamina that passes beneath the Deltoid upon the tendons
of the Supraspinatus and Infraspinatus.
o The Superior Transverse Scapular Ligament: This ligament converts the scapular notch
into a foramen. It is a thin and flat fasciculus, narrower at the middle than at the
extremities, attached by one end to the base of the Coracoid process, and by the other to the
medial end of the scapular notch. The Suprascapular nerve runs through the foramen; the
transverse scapular vessels cross over the ligament. The ligament is sometimes ossified.
The Suprascapular artery passes above it
o The Inferior Transverse Ligament: This ligament is a weak membranous band, situated
behind the neck of the scapula and stretching from the lateral border of the spine to the
margin of the glenoid cavity. It forms an arch under which the transverse scapular vessels
and Suprascapular nerve enter the Infraspinatus fossa.
Removing the skin reveals a fascia covering the trapezius muscle. Below the trapezius, the
Latissimus Dorsi muscle is found at the inferior part of the region as well as the Teres major
muscle (these 2 muscles have a common embryonic origin hence have the same functions).
Beneath the trapezius muscle, there are other muscles too, namely the Supraspinatus (above
spine of scapula), the Infraspinatus (below the spine of scapula), and the Teres minor.
At the lateral border of the region, you can see the long head of the triceps (Separating the
medial triangular and quadrangular spaces from each other)
The main structure of the region is the Suprascapular artery which comes from the Subclavian
artery, and passes through the region above the superior transverse scapular ligament. The
Suprascapular nerve comes together with the artery passing through the superior scapular
foramen (below the superior transverse ligament). These two structures innervate the
Supraspinatus and Infraspinatus muscles. Both structures, after passing through the superior
scapular foramen, pass through the inferior scapular foramen to the Infraspinatus fossa under
the inferior transverse scapular ligament.
At the neck of the scapula, there is an anastomosis between the Suprascapular artery and the
circumflex scapular artery. So finally, this is an anastomosis between the Axillary artery and
Haytham Bayadsi 2008/2009
the Subclavian artery because the circumflex scapular artery comes from the Axillary
(Subscapular) and the Suprascapular from the Subclavian.
In the superior part of the region, you can see the Levator scapulae muscle coming from the
Nuchal region, the Dorsal scapular nerve innervates the Levator scapulae, and comes together
with the Dorsal scapular artery. On the medial side of the scapula we can see the 2 Rhomboids
attaching to the medial margin of the scapula.
**Note: on the Subscapular surface of the scapula, we can see the Subscapularis muscle
covering the fossa, together with the Serratus anterior muscle inserting on the medial margin of
the scapula. The Thoracodorsal Nerve & Artery (branch of Subscapular artery) can be seen on
the Subscapularis muscle descending down for the Latissimus Dorsi muscle, which might have
an inconstant origin at the inferior angle of the scapula. The Subscapular nerve can be seen also
supplying the Subscapularis muscle.
Haytham Bayadsi 2008/2009
6) Anterior Brachial (Arm) Region:
Borders: Superior: Inferior Border of Pectoralis Major & Deltoid muscles
Inferior: 3 fingers above the cubital sulcus
Medial: Medial margin of humerus
Lateral: Lateral margin of humerus
Skin innervation:
Medial Brachial cutaneous nerve (medial cord of brachial plexus)
Superior Lateral Brachial cutaneous nerve (from Axillary nerve)
Inferior Lateral Brachial cutaneous nerve (from Radial nerve)
Subcutaneous Structures:
After removing the skin, we can find 2 superficial veins in the subcutaneous tissue (and of
course the cutaneous nerves).
* On the Lateral side we can find the Cephalic vein running up to reach the Deltopectoral
groove to reach the Deltopectoral triangle and end up in the Subclavian or Axillary veins.
* On the Infero-medial side we can find the Basilic vein running together with the medial
cutaneous Brachial & Antebrachial nerves. The Basilic vein pierces the brachial fascia at the
Basilic Hiatus (at the middle of arm) to end up in 1 of the Brachial veins.
** The Brachial fascia is a continuation of the deltoid, pectoral, Infraspinatus & Axillary
fascias and attaches inferiorly to the humeral epicondyles & Olecranon of ulna and extends
downwards as the fascia of forearm.
The fascia sends 2 speta that attach along the medial & lateral sides of humeral shafts and
supracondylar ridges, the Medial & Lateral Intermuscular Speta respectively. These 2 septa
divide the arm into anterior flexor & posterior extensor muscular compartments
Subfascial Structures:
After removing the fascia, we can find the Biceps Brachii muscle with the lateral long head and
medial short head. If we remove this muscle we can find the Coracobrachialis muscle in the
superior medial 1/2 of this region, and the Brachialis muscles in the lower 1/2. the
Coracobrachialis muscle can be easily distinguished since its pierced dorsally by the
Musculocutaneous nerve (from brachial plexus) which continues to run on the
Coracobrachialis and Brachialis muscles and the under the Biceps Brachii (between the 3
muscles) to end up laterally as a Lateral Antebrachial Cutaneous nerve, that merges laterally in
the cubital fossa from under the biceps muscles to run with the cephalic vein and supply
sensory innervation for the lateral side of the forearm. The Musculocutaneous nerve
innervates the 3 muscles of the arm.
The Medial and Lateral Bicipital grooves are grooves separating the Biceps Brachii muscle
from the Brachialis muscle on both sides of the arm.
In the medial bicipital groove we can find many formations such as:
Median nerve
Medial Brachial & Antebrachial cutaneous nerves
Brachial Artery accompanied by 2 brachial veins (1 of them is enlarged because it
receives the Basilic vein)
Ulnar nerve with the Superior collateral ulnar artery (Branch of Brachial), they
don’t reach the end of the region, because they pierce the medial Intermuscular
Haytham Bayadsi 2008/2009
septum at the lower 2/3 of the arm to go to the groove for ulnar nerve under the
medial humeral epicondyle
** Very important! The Radial nerve is not part of the medial bicipital groove,
instead it goes immediately at the superior part of the brachial region behind the
humerus through the lateral triangular space together with the deep brachial artery
(Profunda Brachii, branch of the brachial artery) to run together in the groove for
radial nerve on the posterior aspect of the humerus.
The Median nerve crosses the brachial artery at the middle of arm, and comes to lie as the
most medial structure in the distal 1/2 of the arm and cubital fossa.
The Brachial artery gives also another branch in lower part of this region near just before the
cubital region (besides the Deep Brachial & the Superior Ulnar collateral) which is the
Inferior Ulnar Collateral artery (Anterior & posterior).
In the lateral bicipital groove we can find the cephalic vein running up to the Deltopectoral
groove/sulcus.
Haytham Bayadsi 2008/2009
7) Posterior Brachial (Arm) Region:
Borders: Superior: Inferior Border Deltoid
Inferior: 3 fingers above the Olecranon
Medial: Medial margin of humerus
Lateral: Lateral margin of humerus
Skin innervation:
Posterior Brachial cutaneous nerve (from Radial nerve)
Medial Brachial Cutaneous nerve (Brachial plexus)
Inferior Lateral Brachial cutaneous nerve (from Radial nerve)
After the removal of the skin and the brachial fascia, we can find the Triceps Brachii muscle
which the main structure of this region with its 3 heads.
If we cut the lateral head in the obliquely in the middle, and we reflect it, we can find the
Radial nerve running together with the deep brachial artery in the groove for radial nerve
between the medial & lateral head of the triceps muscle, innervating and supplying the muscle.
The Brachial artery gives 2 branches here called the Middle Collateral Artery & Radial
Collateral artery.
The Radial nerve gives a sensory branch that emerges under the lateral head of triceps at the
lower portion of this region to reach the posterior surface of the forearm; this branch is the
Posterior Antebrachial Cutaneous nerve.
At the lower 2/3 of the region, after it gives the sensory branch, the Radial nerve pierces the
lateral Intermuscular septum together with the radial collateral artery to pass anteriorly to the
lateral epicondyle of humerus, under the Brachioradialis and on the Supinator muscle.
Haytham Bayadsi 2008/2009
8) Anterior Cubital Region:
Borders: Superior: 2 fingers above the cubital sulcus (fold)
Inferior: 2 fingers under the cubital sulcus
Medial: Medial epicondyle of humerus
Lateral: Lateral epicondyle of humerus
Skin innervation:
Lateral Antebrachial Cutaneous nerve (of Musculocutaneous)
Medial Antebrachial Cutaneous nerve (of Brachial plexus)
Subcutaneous Structures:
- Medially: The Basilic vein runs with the Medial Antebrachial cutaneous nerve
- Laterally: The Cephalic vein runs with the Lateral Antebrachial cutaneous nerve
Between the 2 veins there is an important anastomosis in this region called the Median Cubital
vein. It's an M or N shaped anastomosis. Clinically it's important since blood samples are taken
from vein or intravenous injections are given.
Haytham Bayadsi 2008/2009
Subfascial structures:
Under the anastomosis & the fascia we can find the V-shaped (Triangular) Cubital fossa.
Borders: Roof: Antebrachial fascia (forearm), Bicipital Aponeurosis (Radiating into the
Antebrachial fascia & the venous anastomosis
Floor (base): Brachialis muscle, and the Supinator laterally
Medial: Pronator Teres muscles & the flexors of the forearm
Lateral: Brachioradialis muscle & the extensors of the forearm
Superior: Imaginary line connecting the 2 epicondyles of Humerus
Contents: from medial to lateral:
Median nerve (most medial)
Brachial artery (in the middle)
Tendon of Biceps Brachii inserting of the radial tuberosity (most lateral)
Some lymph nodes (in between)
** In the cubital fossa, the brachial artery divides into 2 main branches:
Ulnar Artery (giving the Anterior/Posterior Ulnar recurrent arteries, anastomosing with the
Inferior/Posterior Ulnar collateral arteries respectively)
Radial Artery (giving the Radial recurrent artery later anastomosing with the radial
collateral artery)
Laterally in this region, the Radial nerve can be found between the tendon of Biceps Brachii
muscle and the Brachioradialis muscle, lying on the Brachialis muscle. Its not part of the
cubital fossa, but part of the cubital region!
In this region the origin of the flexors of the forearm (medial epicondyle) and the origin of
some of the extensors of the forearm (lateral epicondyle) can be seen also
Haytham Bayadsi 2008/2009
Haytham Bayadsi 2008/2009
9) Posterior Cubital Region:
Borders: Superior: 3 fingers above the Olecranon of Ulna
Inferior: 3 fingers under the Olecranon of Ulna
Medial: Medial epicondyle of humerus
Lateral: Lateral epicondyle of humerus
Skin innervation:
Posterior Brachial cutaneous nerve (of Radial)
Medial & Lateral Brachial & Antebrachial cutaneous nerves
Under the fascia we can find the muscles of extensors & flexors of the forearm arising from the
lateral & medial humeral epicondyles respectively. We can see also the insertion of the tendon
of triceps muscle on the Olecranon of ulna and the Anconeus muscle originating from the back
of the lateral epicondyle and inserting on the Olecranon and posterior surface of ulna.
On the medial side, the Ulnar nerve can be found in the Groove for Ulnar nerve on the medial
epicondyle of humerus accompanied by the Superior Ulnar Collateral artery. (After they both
pierce the medial Intermuscular septum)
Around the Elbow, we can summarize the Arterial Reti formation of the elbow, or the
Periarticular arterial anastomosis of the elbow, which supplies the elbow joint and the
muscles of that region, and very important in case of occlusion of the brachial artery or one of
its branches to assure the proper blood supple to the rest of forearm and hand:
1) Superior Ulnar Collateral artery (from brachial)
2) Inferior Ulnar Collateral artery (from brachial)
3) Radial Collateral artery (from deep brachial)
4) Middle Collateral artery (from deep brachial)
5) Radial Recurrent artery (from radial)
6) Anterior/Posterior Ulnar recurrent arteries (from ulnar)
7) Recurrent Interossious artery (from common interossious, which is from ulnar)
10) Anterior Antebrachial (forearm) Region:
Borders: Superior: 3 fingers below the cubital sulcus
Inferior: a line between the styloid processes of Ulna & Radius, or 2 fingers
above the carpal eminences
Skin innervation:
Medial & Lateral Antebrachial cutaneous nerves
Subcutaneous Structures:
In the subcutaneous fatty tissue after skin removal, we can find the cephalic vein radially
running with the lateral Antebrachial cutaneous nerve. The Brachioradialis muscle is found
on the radial border of this region.
Haytham Bayadsi 2008/2009
The Basilic vein passes on the Ulnar side of the anterior forearm region together with the
medial Antebrachial cutaneous nerve.
In the distal part of the forearm, the Palmar Branch of Ulnar nerve pierces the fascia to lie
subcutaneously. More radially, the Palmar Branch of Median nerve pierces the fascia to lie
subcutaneously as well.
Subfascial Structures:
After the removal of the fascia (which is very condensed and attached strongly to the muscles
on the Ulnar side) we can see the group of superficial anterior Antebrachial muscles with some
arteries & nerves between them & their tendons.
Starting from the Ulnar side we can see the Flexor Carpi Ulnaris (FCU) muscle covering the
Ulnar nerve & artery at the superior 2/3 of this region. After it goes in the groove for Ulnar
nerve, the Ulnar nerve comes to lie on the Ulnar side of the Flexor Digitorum Profundus (FDP)
(& innervates this side of the muscle together with FCU). The Ulnar artery branches of the
brachial artery & goes under the Pronator Teres, Median nerve & Common Flexor Origin to
reach the Ulnar nerve and run together with it under the FCU (guiding their course) and above
the Ulnar side of FDP, and when they reach the wrist, they lie radially to the tendon of FCU.
After the FCU, we can find the Flexor Digitorum Superficial muscle, then Palmaris Longus
muscle (if present) then the Flexor Carpi Radialis muscle then the Pronator Teres muscle
proximally. After the cubital fossa, the Median nerve passes between the 2 heads of Pronator
Teres, and comes to lie between the Flexor Digitorum Profundus & Superficialis embedded in
the fascia of the Flexor Digitorum Superficialis in an Epi-fascial position (so first dissect the
median nerve by lifting the muscle, then you can cut the muscle safely). The median nerve
innervates all the flexor muscles of the forearm except the FCU & the ulnar side of the FDP!
After the Pronator Teres muscle, we can find the Brachioradialis Muscle. Under the
Brachioradialis muscle Proximally we can find the Supinator Muscle being pierced by the
Deep Branch of the Radial nerve (goes behind & gives the Posterior interossious nerve,
which innervates all extensors of the forearm), and the Superficial Branch of the Radial nerve
continuing to run distally together with the Radial artery under the Brachioradialis. More
Distally the Superficial branch of radial nerve goes to the dorsum of the hand, and the Radial
artery comes to lie between the tendons of Brachioradialis & FCR.
The deepest structures in the forearm are the Flexor Pollicis Longus lying radially on the radius
and interossious membrane, the Pronator Quadratus (quadrangular muscle) lying distally on the
2 bones between the Radial margin of radius & the Ulnar margin of ulna. The Anterior
Interossious artery (branch of the common interossious of Ulnar) and the anterior interossious
nerve (branch of median) can be seen also running deeply on the interossious membrane.
So we can summarize the muscles from Radial side to ulnar side superficially:
Brachioradialis, Pronator Teres, Flexor Carpi Radialis, Palmaris Longus, Flexor Digitorum
Superficialis and Flexor Carpi Ulnaris
The deep muscles are Supinator (can be considered part of cubital fossa), Flexor Pollicis
Longus, Flexor Digitorum Profundus and Pronator Quadratus.
Haytham Bayadsi 2008/2009
The vessels & nerves can be arranged into 3 neuromuscular bundles or routes:
1. Radial vascular bundle: Radial artery & accompanying veins. Found distally
between Brachioradialis and FCR muscles/tendons. It is accompanied proximally by
the Superficial branch of Radial nerve.
2. Middle neurovascular bundle: between the superficial & deep flexors. Consists of
the Median nerve running between the FDS & FDP muscles. And deeply of the
anterior interossious artery & nerve between the deep flexors & interossious
membrane.
3. Ulnar neurovascular bundle: in the distal 2/3 of the forearm. Between the FDS and
FCU muscles. Consists of Ulnar artery (with accompanying veins) & Ulnar nerve.
11) Posterior Antebrachial (Forearm) Region:
Borders: Superior: 3 fingers below the Olecranon
Inferior: a line between the styloid processes of Ulna & Radius
Skin innervation:
Posterior Antebrachial Cutaneous nerve (of Radial)
Posterior Branches of Medial/Lateral Antebrachial cutaneous nerves
After skin removal, we can find the Posterior Antebrachial fascia. Removing this fascia will
expose the extensor muscles of the forearm arranged in 2 layers: Superficial & Deep.
Superficial Layer of muscles (from radial to ulnar): Brachioradialis, Extensor Carpi Radialis
Longus & Brevis, Extensor Digitorum, Extensor Digiti Minimi and Extensor Carpi Ulnaris
After the removal of the superficial muscles, we can see:
The Posterior interossious artery (from common interossious) and the Deep Branch of
Radial nerve can be seen piercing the Supinator Muscle and forming the Supinator canal and
come to lie on the deep muscles of the forearm.
Deep layer of muscles (from radial to ulnar): Supinator, Abductor Pollicis Longus, Extensor
Pollicis Brevis & Longus and Extensor Indicis
** Distally in this region, before the wrist, we can see 2 tendons crossing from the ulnar side to
the radial over 2 other tendons. The first 2 tendons are the tendons of Abductor Pollicis Longus
muscle & Extensor Pollicis Brevis that cross the Tendons of the Extensor Carpi Radialis
Longus & Brevis. (That’s how they come to lie in the 1st extensor compartment although they
originate more ulnary)
Haytham Bayadsi 2008/2009
12) Volar (Palmar) Carpal (Wrist) Region:
Borders: Superior: level of styloid processes
Inferior: level of the Pisiform bone, 2 fingers above the carpal eminence
Skin innervation:
End branches of Lateral/Medial Antebrachial Cutaneous nerves
In the subcutaneous tissue we can find the Cephalic & Basilic veins running on the edges of
this region with the Palmar branches of ulnar & median nerves that pierces the Antebrachial
fascia to reach the palm.
Under the subcutaneous tissue and its structures we can find the Antebrachial fascia proximally
and the Palmar aponeurosis origining from the tendon of Palmaris longus muscle and attached
to the Palmar or Volar carpal ligament (which is the thickening of the deep layer of the
Antebrachial fascia)
Haytham Bayadsi 2008/2009
If we remove the proximal part covered by the Antebrachial fascia we can expose a series of
tendons, nerves & arteries organized in this manner from Radial to Ulnar side:
1) Superficial branch of Radial nerve
2) Brachioradialis muscle inserting on styloid process (sometimes also EPB & APL)
3) Radial artery accompanied by 2 radial veins and it's superficial palmar branch
originating
4) Flexor Carpi Radialis
5) Median nerve
6) Palmaris longus (covering the median nerve if present)
7) Flexor Digitorum Superficialis (4 tendons)
8) Ulnar artery
9) Ulnar nerve
10) Flexor Carpi Ulnaris
Distally, if we remove the Palmar carpal ligament & Palmaris longus tendon attached to it
we can see the Ulnar Nerve & Artery on the ulnar side lying in a special canal called Guyon
Canal above the Transverse Carpal ligament or Flexor retinaculum. On the radial side we
can see a small branch of the radial artery called the Superficial Palmar branch, that goes to
join the Superficial palmar arch and closes it.
The flexor retinaculum or the Transverse carpal ligament lies under the Ulnar artery & nerve
and the superficial palmar branch of radial artery. It extends from the lateral carpal eminence
(tubercles of Scaphoid & Trapezium) to the medial carpal eminence (Pisiform & Hook of
Hamate) and it forms the Roof of the so called Carpal Tunnel or Canal:
Borders: Roof: Transverse Carpal ligament or flexor retinaculum
Floor: Capitate and trapezoid
Lateral border: Lateral carpal eminence & Trapezium
Medial border: Medial carpal eminence & Hamate
Structures that pass through the carpal tunnel:
Median nerve
Flexor Pollicis longus muscle in one tendinous sheath
Flexor Digitorum Superficialis & Profundus tendons in a common tendinous
sheath
** Important note: the Flexor Carpi Radialis doesn't exactly pass into the canal,
more precisely its passes through a duplication of the transverse carpal ligament, or
basically through it.
The flexor retinaculum or the transverse carpal ligament has other functions rather than
forming the roof of the carpal tunnel and keeping the tendons inside, it also functions as
insertion & origin of some Hypothenar, Thenar and Palmaris muscles.
Haytham Bayadsi 2008/2009
Haytham Bayadsi 2008/2009
12) Dorsal Carpal (Wrist) region:
After the removal of the skin, we can find the subcutaneous superficial structures lying above
the Extensor retinaculum. These structures are the Cephalic vein & the Superficial branch of
Radial nerve on the Radial side and the Basilic vein & the Dorsal Branch of Ulnar nerve on the
ulnar side. In the middle we can find the termination of the Posterior Antebrachial cutaneous
nerve
Under these structures we can find the Extensor Retinaculum, which is a continuation of the
Deep layer of the Antebrachial fascia (Palmar Carpal ligament) dorsally. (Not the
continuation of the flexor retinaculum). It’s a ribbon like band stretching obliquely across the
back of the wrist, attaching deeply to ridges on the dorsal aspect of the radius, triquetrum, and
Pisiform bones, and binding down the extensor tendons of the fingers and thumb, Giving
fibrous septa that creates 6 compartments, which are (from radial to ulnar side):
1st compartment: Abductor Pollicis Longus + Extensor Pollicis Brevis
2nd compartment: Extensor Carpi Radialis Brevis + Extensor Carpi Radialis
Longus
3rd compartment: Extensor Pollicis Longus
4th compartment: Extensor Digitorum + Extensor Indicis
5th compartment: Extensor Digiti Minimi
6th compartment: Extensor Carpi Ulnaris
A special formation or structure is formed between the first 3 compartments and the tendons
passing through them, this is the triangular Foveola Radialis or the Anatomical Snuff Box:
Located between: Extensor Pollicis longus tendon (3rd compartment) (Lateral border)
Abductor Pollicis Longus + Extensor Pollicis Brevis tendons (1st
compartment) (Medial border)
Extensor Retinaculum (Proximally)
Trapezium and Scaphoid bones forming its floor
Contents: ** Superficial (Above the fascia) Superficial Branch of Radial nerve
Cephalic Vein
** Deep (Under the fascia) Radial Artery
Tendons of Extensor Carpi Radialis Longus & Brevis
Under the tendons of Abductor Pollicis Longus & Extensor Pollicis Brevis, the Radial artery
gives its Dorsal Carpal Arterial Arch branch that passes to the back to join the Dorsal carpal
network and gives Dorsal Metacarpal arteries that anastomose with the common Palmar
Digital arteries between the distal ends of the metatarsals.
Haytham Bayadsi 2008/2009
Haytham Bayadsi 2008/2009
13) Palmar (Volar) Region:
Borders: Superior: Radial and Ulnar carpal eminences
Inferior: Roots of fingers
Lateral: Lateral border of the palm
Medial: a line from the Pisiform bone to the 5th finger or medial border of the
palm
Skin innervation:
The Radial 7 Finger-sides & palm by the Median nerve
The Ulnar 3 Finger-sides & palm by the Ulnar nerve
The palm of the hand is subdivided by the Medial, Intermediate & Lateral Palmar Septa
(extensions of the Palmar Aponeurosis) into 3 regions: Thenar Eminence, the Mesothenar or
Central compartment and the Hypothenar Eminence.
After the removal of the skin, we can see that the fascia covers the Thenar & Hypothenar
compartments, but the central Mesothenar compartment is covered by the Palmar Aponeurosis
(continuation of Palmaris longus muscle) with the Palmar branches of Median (in the middle)
and Ulnar (on the Hypothenar eminence) nerves (sensory innervation of fingers & palm).
The palmar aponeurosis has longitudinal & transverse fascicles. It can radiate on the
Hypothenar eminence sometimes as the Palmaris Brevis muscle. At the distal end of the
palmar aponeurosis the Common palmar digital arteries & nerves emerge and become
subcutaneous and they divide into Proper Digital arteries & nerves that extend to the distal
phalanges of the digits.
After the removal of the palmar aponeurosis, we can immediately see the Superficial Palmar
arterial arch. This arch is formed by the Ulnar artery (after passing through the Guyon canal)
and closed from the radial side by the Superficial Palmar branch of the radial artery (Passing
under the Abductor Pollicis Brevis muscle). The Superficial palmar arch gives off the common
palmar digital arteries which run at first superficial toe the tendons of the long flexors and at
the root of the digits between them.
The Median nerve and its branches can be also seen after the removal of the palmar
aponeurosis. It has common & proper palmar digital branches for the 7 radial finger-sides, and
has recurrent branches for some of the Thenar muscles (Abductor Pollicis Brevis, Opponens
Pollicis and Superficial Head of Flexor Pollicis Brevis) and the 1st & 2nd Lumbricals.
The Median nerve & its branches and the Superficial Palmar arch lie over the tendons of the
Flexor Digitorum Superficialis muscle. Between these tendons we can see the Lumbricals
arising from the tendons of the Flexor Digitorum Profundus, which lie under the superficial
ones.
After the removal of the tendons of the flexors of the digits and the Lumbricals, we can see the
Adductor Pollicis muscle, and proximal to it we can see the Deep Palmar arterial arch. This
arterial arch is formed by the Radial artery and closed by the Deep Palmar branch of Ulnar
artery.
The radial artery in the wrist region will turn around the base of the 1st metacarpal under the
tendons of the Abductor Pollicis longus & Extensor Pollicis Brevis to the dorsum of the hand
through the radial Foveola, and then it pierces the 1st dorsal interossious muscle and forms the
Haytham Bayadsi 2008/2009
Deep Palmar arch. The Deep palmar arch gives the Princips Pollicis Artery, which has 3
branches: 1 for the 2nd finger (Radialis Indicis artery) and 2 for the thumb.
The deep palmar arterial arch lies on the Palmar interossious muscles (3) and gives also the
Palmar metacarpal arteries that anastomose distally with the common palmar digital arteries
from the superficial arch and then separate the root of fingers as the proper palmar digital
arteries.
The Ulnar nerve has a deep branch that after the Guyon canal, it separates and penetrates
deeply between the Abductor Digiti Minimi & Flexor Digiti Minimi Brevis. This deep branch
supplies ALL Hypothenar muscles, the Adductor Pollicis muscle, the Deep Head of Flexor
Pollicis Brevis muscle, both palmar & dorsal Interossei muscles and the 3rd & 4th Lumbricals.
The superficial palmar ulnar branch has common & proper palmar digital branches for the 3
ulnar finger-sides.
In the Thenar eminences, the most superficial & radial muscle is the Abductor Pollicis Brevis,
then the Flexor Pollicis Brevis muscle with the 2 heads, then Opponens Pollicis, and the most
deep one is the Adductor Pollicis muscle.
In the Hypothenar eminence, the same pattern, the most superficial & ulnar muscle is the
Abductor Digiti Minimi, then the Flexor Digiti Minimi, then the Opponens Digiti Minimi
muscle
On the palmar surface of the fingers we can find the tendons of Flexor Digitorum Superficialis
inserting on the base of the middle phalanx and expanding towards the margins of the fingers
creating a hiatus or a chiasm through which the tendons of the Flexor Digitorum Profundus
can pass and reach the distal phalanges. On the dorsal surface of the fingers we should see the
extensor tendons reaching the distal phalanx with the extensor hood and expansions on
radiation on the side with the Lumbricals inserting on them.
The proper digital arteries & nerves run on both sides of 1 finger between the tendons of the
flexor Digitorum superficial & Profundus.
One finger is supplied by two digital palmar nerves and the medical significance of this is
Ober's anesthesia: if you operate on the fingers, you should anesthetize both sides of the
finger.
Tendon sheath: an outer, fibrous layer and an inner, Synovial layer. The inner layer has a
double layer which is called vincula tendineum or mesotendineum. This is very important
because blood vessels come through this sheath to supply the tendons. So, you must not lift the
tendons during an operation because you will destroy the arteries and the finger will be
necrotized.
Inflammation of the tendon sheath is called Phlegmon (an obsolete term for inflammation
of subcutaneous connective tissue this phlegmon can spread onto the 1st finger through this
tendon sheath -- in this sheath, we don't have tendons of the 2nd, 3rd, and 4th fingers): from 5th to
1st and opposite.
Tendons of the 2nd, 3rd, and 4th do not have tendon sheaths at the palmar region. Their tendon
sheaths begin after the metacarpals.
Paralysis of the ulnar nerve: Metacarpo-phalangeal joints are extended and interphalangeal
joints are a little flexed-- Clawhand.
Haytham Bayadsi 2008/2009
Haytham Bayadsi 2008/2009
14) Dorsalis Manus (Hand) Region:
Skin innervation:
The Radial 5 Finger-sides & dorsum of hand by the Ulnar nerve (except the distal
phalanges of the ulnar 1/2 of the 2nd finger and the radial 1/2 of the 3rd finger, they
are supplied by the Median nerve)
The Ulnar 5 Finger-sides & dorsum of the hand by the radial nerve (except the
distal phalanges of them are supplied by the median nerve.
After the removal of the skin in this region, we can find the Dorsal Venous Network or Rete
Venosum Dorsalis Manus of the hand. From this venous network the 2 superficial veins of the
upper limb arise: the Cephalic & the Basilic veins.
The superficial branches of radial nerve, and the Dorsal branch of Ulnar nerve together with
their branches supplying the fingers (via the dorsal digital branches) can be found along the
venous network.
Below the venous Plexus, the fascia covering the Extensor tendons and some short muscles.
The tendons are ED, APL, EPB and EPL.
Beneath the tendons, the dorsal interossious muscles (4) can be found and the dorsal
metacarpal arteries from the Dorsal Carpal arch (branch of Radial) can be found, they will
give rise to the Dorsal Digital arteries. We can find intratendinous connections between the
tendons also.
Haytham Bayadsi 2008/2009
Haytham Bayadsi 2008/2009
You might also like
- Muscle Origins, Insertions, Actions, and InterventionsDocument15 pagesMuscle Origins, Insertions, Actions, and InterventionsJoseph Kachelman100% (3)
- Singh's OsceDocument466 pagesSingh's OsceShuaib AhmedNo ratings yet
- Brachial Plexus Palsy: A Therapy Guide For Your BabyDocument8 pagesBrachial Plexus Palsy: A Therapy Guide For Your BabyNovy Dita100% (1)
- Muscle Origin Insertion Nerve Action Comment ShoulderDocument10 pagesMuscle Origin Insertion Nerve Action Comment ShoulderAdam IrsyaddyraNo ratings yet
- Scapula - 18 Muscle AttachmentsDocument2 pagesScapula - 18 Muscle Attachmentsdarbyje88% (8)
- OSTEOARTHRITISDocument42 pagesOSTEOARTHRITISDaisy R. Lim100% (4)
- (Eric - Frankling) - Breathing For Peak Performance Functional Exercises For Dance, Yoga, and Pilates PDFDocument73 pages(Eric - Frankling) - Breathing For Peak Performance Functional Exercises For Dance, Yoga, and Pilates PDFLuis Lanca100% (2)
- Gorgeous Glutes SpreadsheetDocument31 pagesGorgeous Glutes SpreadsheetVeronica ZambranoNo ratings yet
- Clavicular Head:: RD THDocument3 pagesClavicular Head:: RD THSam PadreNo ratings yet
- Anatomy of Shoulder Joint ComplexDocument30 pagesAnatomy of Shoulder Joint ComplexDr. JDPNo ratings yet
- Anatomy Notes MusclesDocument24 pagesAnatomy Notes Musclesjonmusco100% (1)
- Muscles of Shoulder and ArmDocument3 pagesMuscles of Shoulder and ArmAhadNo ratings yet
- Table of Back Muscles RWDocument3 pagesTable of Back Muscles RWFrank Zhang100% (1)
- MSKDocument7 pagesMSKKY KimberlyNo ratings yet
- Unit4 DM - Vb.inddDocument31 pagesUnit4 DM - Vb.inddAlexNo ratings yet
- Muscle Origin Insertion Innervation Actions: ShoulderDocument5 pagesMuscle Origin Insertion Innervation Actions: ShoulderSíofra MurphyNo ratings yet
- Upper Limb AnatomyDocument15 pagesUpper Limb AnatomyAjennyKinoNo ratings yet
- Back Muscle ChartDocument3 pagesBack Muscle ChartTony Montana100% (1)
- 2nd Order (Unit I) - ADocument3 pages2nd Order (Unit I) - Auberjunk426801No ratings yet
- Thoracic Wall To Upper Limb: Muscle Origin Insertion Action Nerve SupplyDocument13 pagesThoracic Wall To Upper Limb: Muscle Origin Insertion Action Nerve SupplyShandria AlbertoNo ratings yet
- Upper Extermity: A. SkeletalDocument24 pagesUpper Extermity: A. SkeletalDinda BiolawatikaNo ratings yet
- UE Muscles OINADocument3 pagesUE Muscles OINAUshuaia Chely FilomenoNo ratings yet
- Upper Limb MusclesDocument16 pagesUpper Limb MusclesmehekNo ratings yet
- Upper-LIMB-Muscles Upper-LIMB - MusclesDocument8 pagesUpper-LIMB-Muscles Upper-LIMB - MusclesAnne SerneoNo ratings yet
- Muscles of The ScapulaDocument6 pagesMuscles of The ScapulaAndika Anjani AgustinNo ratings yet
- Anatomy Tables SarahDocument4 pagesAnatomy Tables Sarahanasadel1234.1No ratings yet
- Muscles AnatomyDocument14 pagesMuscles AnatomyJiya JithinNo ratings yet
- 09:16 - Back & Spinal Cord PDFDocument24 pages09:16 - Back & Spinal Cord PDFVidya BalaNo ratings yet
- Muscles of The Human BodyDocument150 pagesMuscles of The Human BodyJoseph EpsteinNo ratings yet
- 2nd Order (Unit 1 - B)Document5 pages2nd Order (Unit 1 - B)uberjunk426801No ratings yet
- Bootcamp Muscle TablesDocument48 pagesBootcamp Muscle TablesvesteriawylnisNo ratings yet
- Upper Extremity - Muscle Summary ChartDocument9 pagesUpper Extremity - Muscle Summary ChartpoggerNo ratings yet
- Muscles of The BackDocument2 pagesMuscles of The BackavrilaNo ratings yet
- Muscle Origin Insertion Innervation Action: (Branch of The Brachial Plexus)Document58 pagesMuscle Origin Insertion Innervation Action: (Branch of The Brachial Plexus)sdfs sdfdNo ratings yet
- Bones AssignmentDocument5 pagesBones Assignmentmunirwisal4No ratings yet
- Suboccipital and Scapular Region 1125Document50 pagesSuboccipital and Scapular Region 1125qns8mhb7wyNo ratings yet
- 01 Muscle Tables Upper LimbDocument7 pages01 Muscle Tables Upper LimbhawkreadNo ratings yet
- Muscle OIAN - HandDocument3 pagesMuscle OIAN - Handanais MitchellNo ratings yet
- Tabel Gerakan Sendi Di Neck Trunk Upper Amp Lower Extremity PDF FreeDocument30 pagesTabel Gerakan Sendi Di Neck Trunk Upper Amp Lower Extremity PDF FreeIchlasul AkmalNo ratings yet
- UPPER LIMB Muscle Origins, Insertions, Innervations, Blood Supplies and ActionsDocument6 pagesUPPER LIMB Muscle Origins, Insertions, Innervations, Blood Supplies and ActionsMohiuddin AhmedNo ratings yet
- Muscles of The Superficial BackDocument3 pagesMuscles of The Superficial BackMargaux Chang NuñezNo ratings yet
- HUBS1105 Anterior NeckDocument4 pagesHUBS1105 Anterior NeckChloe HeuchanNo ratings yet
- Muslce Chart GA1Document10 pagesMuslce Chart GA1kaycorkumNo ratings yet
- Unit 2 Skeletal Muscles Part 2Document3 pagesUnit 2 Skeletal Muscles Part 2Sharva BhasinNo ratings yet
- Neck Fascia and BonesDocument16 pagesNeck Fascia and BonesRAQUELLE PADERNANo ratings yet
- Tabel Gerakan Sendi Di Neck & Trunk, Upper Extremity Dan Lower ExtremityDocument31 pagesTabel Gerakan Sendi Di Neck & Trunk, Upper Extremity Dan Lower Extremityfira fadhillah salyNo ratings yet
- 1D-19 GRSANA Reviewer 1.04 - Muscles of The Shoulder RegionDocument16 pages1D-19 GRSANA Reviewer 1.04 - Muscles of The Shoulder RegionShaira Aquino VerzosaNo ratings yet
- W11 - Upper Limb - 2024 - CKK - UploadDocument39 pagesW11 - Upper Limb - 2024 - CKK - Upload陳文迪No ratings yet
- Clavicular Part: Flexes and Acromial Part: AbductsDocument1 pageClavicular Part: Flexes and Acromial Part: AbductsMihaelaNo ratings yet
- Superficial Back Proximal Insertion Distal Insertion Innervation Blood Supply Function Latissimus DorsiDocument23 pagesSuperficial Back Proximal Insertion Distal Insertion Innervation Blood Supply Function Latissimus Dorsimeyouhere100% (1)
- MRI of The ShoulderDocument32 pagesMRI of The Shoulderrandy22002No ratings yet
- All Bat NotesDocument1,048 pagesAll Bat NotesAfk SystemNo ratings yet
- MoinaDocument12 pagesMoinacj.tenederoNo ratings yet
- Myology of The Thorax PDFDocument4 pagesMyology of The Thorax PDFlina taziNo ratings yet
- Muscle Origin/Insertion/Action/Innervation Chart Muscles of Upper Extremity Muscle Name Origin Insertion Action InnervationDocument11 pagesMuscle Origin/Insertion/Action/Innervation Chart Muscles of Upper Extremity Muscle Name Origin Insertion Action InnervationNurul Afiqah Fattin AmatNo ratings yet
- Scapular RegionDocument23 pagesScapular Regioncodymike24434No ratings yet
- Elbow Complex (Kinesiology)Document2 pagesElbow Complex (Kinesiology)Kimmybee Garcia50% (2)
- MSK Upper LimbDocument24 pagesMSK Upper LimbAhmed QrariaNo ratings yet
- UE Review (Color!)Document2 pagesUE Review (Color!)Research4OTNo ratings yet
- Root of The Neck (Gross)Document21 pagesRoot of The Neck (Gross)Kimsha ConcepcionNo ratings yet
- The Upper ExtremityDocument9 pagesThe Upper ExtremityHiruzaminNo ratings yet
- Muscle Innervation Chart IIDocument7 pagesMuscle Innervation Chart IIkimsue9448No ratings yet
- ACL Injuries: Care of The Young Athlete Patient Education HandoutsDocument2 pagesACL Injuries: Care of The Young Athlete Patient Education Handoutsindra20dhira100% (1)
- Oral CavityDocument5 pagesOral CavitySoha Jan KhuhawarNo ratings yet
- Skull TopographyDocument43 pagesSkull TopographyGernalyn Ann MagayagaNo ratings yet
- TorticollisDocument8 pagesTorticollisNarishaAmeliaNo ratings yet
- Quarantine Hypertrophy Full BodyDocument41 pagesQuarantine Hypertrophy Full BodyΧρήστος ΓιάντσηςNo ratings yet
- 108 Vital AreasDocument16 pages108 Vital Areasnikrok1100% (19)
- Case Reflection: Left CLAVICLE Fracture - Group IDocument34 pagesCase Reflection: Left CLAVICLE Fracture - Group ILili WidiantoNo ratings yet
- Bones and Skeletal Tissues: Part A: Prepared by Janice Meeking, Mount Royal CollegeDocument41 pagesBones and Skeletal Tissues: Part A: Prepared by Janice Meeking, Mount Royal CollegeRaul ReynosoNo ratings yet
- AnotomyPhysiology PDFDocument410 pagesAnotomyPhysiology PDFindramaniNo ratings yet
- PhysioEx Activity 7Document8 pagesPhysioEx Activity 7i1011221013No ratings yet
- A Pattern Recognition Approach To Myopathy. CONTINUUMDocument24 pagesA Pattern Recognition Approach To Myopathy. CONTINUUMjorgegrodlNo ratings yet
- Orthopedic EmergenciesDocument75 pagesOrthopedic EmergenciesAlex beharuNo ratings yet
- MS Musculoskeletal ReviewDocument12 pagesMS Musculoskeletal ReviewShayesra-Radina Laja SahibadNo ratings yet
- Chapter 1-Musculoskeletal SystemDocument113 pagesChapter 1-Musculoskeletal SystemWang Ming YaNo ratings yet
- Balance, Equilibrium, & Stability: Kinesiology RHS 341 Dr. Einas Al-EisaDocument32 pagesBalance, Equilibrium, & Stability: Kinesiology RHS 341 Dr. Einas Al-Eisashabatat2002No ratings yet
- Hardness of The Upper LimbDocument9 pagesHardness of The Upper LimbSoka Bog.98No ratings yet
- Musculoskeletal SystemDocument93 pagesMusculoskeletal Systemromeo jr mostolesNo ratings yet
- Krok 1 - 2014 (Anatomy)Document20 pagesKrok 1 - 2014 (Anatomy)Shameem UabackerNo ratings yet
- Vivek Sharm Acl ReconstructionDocument7 pagesVivek Sharm Acl ReconstructionJuan Pablo FuentesNo ratings yet
- Grappler Grip Strength 21 Day Challenge Ebook With ToCDocument79 pagesGrappler Grip Strength 21 Day Challenge Ebook With ToCjose100% (1)
- Muscle - Re EducationDocument20 pagesMuscle - Re EducationRam RamNo ratings yet
- Mitland For Cevical SpineDocument52 pagesMitland For Cevical SpineMohamed RamadanNo ratings yet
- HeightDocument4 pagesHeightThiện Nhân NguyễnNo ratings yet
- Injury and Injury Prevention: by - Aryan Pathange & Otto ManskinenDocument8 pagesInjury and Injury Prevention: by - Aryan Pathange & Otto Manskinenaryan pathangeNo ratings yet
- Pelvic Neurovasculature Practice QuizDocument4 pagesPelvic Neurovasculature Practice QuizMr .Hacker xDNo ratings yet
- Muscle CrosswordDocument3 pagesMuscle CrosswordStasia CleggNo ratings yet