0 ratings0% found this document useful (0 votes)
49 viewsACR Criteria PDF
ACR Criteria PDF
Uploaded by
quickdannyCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
ACR Criteria PDF
ACR Criteria PDF
Uploaded by
quickdanny0 ratings0% found this document useful (0 votes)
49 views18 pagesOriginal Title
ACR_Criteria.pdf
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
49 views18 pagesACR Criteria PDF
ACR Criteria PDF
Uploaded by
quickdannyCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 18
Revised 2019
American College of Radiology
ACR Appropriateness Criteria®
Headache
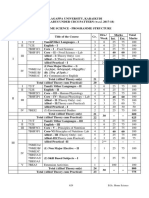
Variant 1: Sudden, severe headache or “worst headache of life.” Initial imaging.
Procedure Appropriateness Category Relative Radiation Level
CT head without IV contrast Usually Appropriate ☢☢☢
CTA head with IV contrast May Be Appropriate (Disagreement) ☢☢☢
MRA head without and with IV contrast Usually Not Appropriate O
MRA head without IV contrast Usually Not Appropriate O
MRI head without and with IV contrast Usually Not Appropriate O
MRI head without IV contrast Usually Not Appropriate O
Arteriography cervicocerebral Usually Not Appropriate ☢☢☢
CT head with IV contrast Usually Not Appropriate ☢☢☢
CT head without and with IV contrast Usually Not Appropriate ☢☢☢
Variant 2: New headache with optic disc edema. Initial imaging.
Procedure Appropriateness Category Relative Radiation Level
MRI head without and with IV contrast Usually Appropriate O
CT head without IV contrast Usually Appropriate ☢☢☢
MRI head without IV contrast Usually Appropriate O
CTV head with IV contrast May Be Appropriate ☢☢☢
MRV head without and with IV contrast May Be Appropriate O
MRV head without IV contrast May Be Appropriate O
CT head with IV contrast May Be Appropriate ☢☢☢
CT head without and with IV contrast Usually Not Appropriate ☢☢☢
Arteriography cervicocerebral Usually Not Appropriate ☢☢☢
ACR Appropriateness Criteria® 1 Headache
Variant 3: New or progressively worsening headache with one or more of the following ‘red flags’:
subacute head trauma, related activity or event (sexual activity, exertion, position),
neurological deficit, known or suspected cancer, immunosuppressed or
immunocompromised state, currently pregnant, or 50 years of age or older. Initial imaging.
Procedure Appropriateness Category Relative Radiation Level
CT head without IV contrast Usually Appropriate ☢☢☢
MRI head without and with IV contrast Usually Appropriate O
MRI head without IV contrast Usually Appropriate O
CT head with IV contrast Usually Not Appropriate ☢☢☢
CTA head with IV contrast Usually Not Appropriate ☢☢☢
MRA head without IV contrast Usually Not Appropriate O
CT head without and with IV contrast Usually Not Appropriate ☢☢☢
Arteriography cervicocerebral Usually Not Appropriate ☢☢☢
MRA head without and with IV contrast Usually Not Appropriate O
Variant 4: New headache. Classic migraine or tension-type primary headache. Normal neurologic
examination. Initial imaging.
Procedure Appropriateness Category Relative Radiation Level
Arteriography cervicocerebral Usually Not Appropriate ☢☢☢
CT head with IV contrast Usually Not Appropriate ☢☢☢
CT head without and with IV contrast Usually Not Appropriate ☢☢☢
CT head without IV contrast Usually Not Appropriate ☢☢☢
CTV head with IV contrast Usually Not Appropriate ☢☢☢
CTA head with IV contrast Usually Not Appropriate ☢☢☢
MRV head without and with IV contrast Usually Not Appropriate O
MRV head without IV contrast Usually Not Appropriate O
MRA head without and with IV contrast Usually Not Appropriate O
MRA head without IV contrast Usually Not Appropriate O
MRI head without and with IV contrast Usually Not Appropriate O
MRI head without IV contrast Usually Not Appropriate O
ACR Appropriateness Criteria® 2 Headache
Variant 5: New primary headache of suspected trigeminal autonomic origin. Initial imaging.
Procedure Appropriateness Category Relative Radiation Level
MRI head without and with IV contrast Usually Appropriate O
MRI head without IV contrast May Be Appropriate O
CT head with IV contrast Usually Not Appropriate ☢☢☢
CT head without IV contrast Usually Not Appropriate ☢☢☢
MRA head without and with IV contrast Usually Not Appropriate O
MRA head without IV contrast Usually Not Appropriate O
Arteriography cervicocerebral Usually Not Appropriate ☢☢☢
CT head without and with IV contrast Usually Not Appropriate ☢☢☢
CTA head with IV contrast Usually Not Appropriate ☢☢☢
Variant 6: Chronic headache. No new features. No neurologic deficit. Initial imaging.
Procedure Appropriateness Category Relative Radiation Level
CT head without IV contrast Usually Not Appropriate ☢☢☢
MRI head without and with IV contrast Usually Not Appropriate O
MRI head without IV contrast Usually Not Appropriate O
Arteriography cervicocerebral Usually Not Appropriate ☢☢☢
CT head with IV contrast Usually Not Appropriate ☢☢☢
CT head without and with IV contrast Usually Not Appropriate ☢☢☢
CTV head with IV contrast Usually Not Appropriate ☢☢☢
CTA head with IV contrast Usually Not Appropriate ☢☢☢
MRV head without and with IV contrast Usually Not Appropriate O
MRV head without IV contrast Usually Not Appropriate O
MRA head without and with IV contrast Usually Not Appropriate O
MRA head without IV contrast Usually Not Appropriate O
ACR Appropriateness Criteria® 3 Headache
Variant 7: Chronic headache. New features or increasing frequency. Initial Imaging.
Procedure Appropriateness Category Relative Radiation Level
MRI head without and with IV contrast Usually Appropriate O
MRI head without IV contrast Usually Appropriate O
CT head without IV contrast May Be Appropriate ☢☢☢
CT head without and with IV contrast May Be Appropriate ☢☢☢
CT head with IV contrast Usually Not Appropriate ☢☢☢
MRA head without IV contrast Usually Not Appropriate O
Arteriography cervicocerebral Usually Not Appropriate ☢☢☢
CTA head with IV contrast Usually Not Appropriate ☢☢☢
CTV head with IV contrast Usually Not Appropriate ☢☢☢
MRA head without and with IV contrast Usually Not Appropriate O
ACR Appropriateness Criteria® 4 Headache
HEADACHE
Expert Panel on Neurologic Imaging: Matthew T. Whitehead, MD a; Agustin M. Cardenas, MDb;
Amanda S. Corey, MDc; Bruno Policeni, MD, MBAd; Judah Burns, MDe; Santanu Chakraborty, MBBS, MScf;
R. Webster Crowley, MDg; Pascal Jabbour, MDh; Luke N. Ledbetter, MDi; Ryan K. Lee, MD, MBA, MRMDj;
Jeffrey S. Pannell, MDk; Jeffrey M. Pollock, MDl; William J. Powers, MDm; Gavin Setzen, MDn;
Robert Y. Shih, MDo; Rathan M. Subramaniam, MD, PhD, MPHp; Pallavi S. Utukuri, MDq;
Julie Bykowski, MD.r
Summary of Literature Review
Introduction/Background
Headache is one of the most common reasons for consulting physicians [1]. Studies have estimated overall
lifetime prevalence of 0.2% to 60% for headache of any kind [2,3], and the burden of headache has shown to be
very large. Headaches occur most commonly between the ages of 25 to 55 years.
The purpose of this document is to identify the most common clinical scenarios and the most appropriate imaging
for their assessment based on the current literature. This document does not address follow-up recommendations
for patients with a known underlying etiology for headache. Given the frequent coexistence of headache and other
neurologic, traumatic, infectious, and vascular processes, it is important to acknowledge the overlap of symptoms
with other conditions referenced in independent ACR Appropriateness Criteria documents, and others beyond the
scope of this document. To avoid delay of appropriate care, any patient with a new neurologic deficit suggesting
transient ischemic attack or stroke should have imaging guided by the ACR Appropriateness Criteria® topic on
“Cerebrovascular Disease” [4]. Headache accompanying clinical signs of meningitis should be managed by
appropriate clinical guidelines. Please also reference the ACR Appropriateness Criteria® topic on “Head Trauma”
[5], ACR Appropriateness Criteria® topic on “Cranial Neuropathy” [6], the ACR Appropriateness Criteria® topic
on “Orbits, Vision and Vision Loss” [7], the ACR Appropriateness Criteria® topic on “Sinonasal Disease” [8],
and the ACR Appropriateness Criteria® topic on “Neuroendocrine Imaging” [9], in the appropriate clinical
context.
Headaches can be broadly classified into primary and secondary forms [1]. Most common primary headaches
include migraine, tension-type, and trigeminal autonomic cephalalgias. The primary headache classification also
includes those related to cough, exercise, sexual activity, cold-stimulus, thunderclap (mimicking but not caused
by subarachnoid hemorrhage [SAH]), external pressure, stabbing, nummular, hypnic, and new daily persistent
headaches. Secondary headaches are related to trauma, cranial or cervical vascular disorders, intracranial
processes (tumor, cerebrospinal fluid pressure, seizure, etc), infection, substance use or withdrawal, referred pain,
and psychiatric disorders [10]. In most cases, the cause and type of headache can be determined by procuring a
detailed history and performing a physical examination. In the absence of worrisome features in the history or
examination, the task is then to diagnose the primary headache syndrome based on the clinical features.
In the emergency setting, the majority of patients with primary headache usually respond well medically with
nonsteroidal anti-inflammatory drugs and a minority with opioids [11]. If atypical features are present, the
neurological examination is abnormal, or the patient does not respond to conventional therapy, the possibility of a
secondary headache disorder should be investigated [12-15], and imaging might be indicated [15-17].
Neuroimaging techniques have shown to represent a valuable diagnostic bridge between neurophysiological
studies and clinical findings [18]. At the same time, it is important to consider the low yield of imaging
a
Children’s National Health System, Washington, District of Columbia. bResearch Author, Children’s of Alabama, Birmingham, Alabama. cPanel Chair,
Atlanta VA Health Care System and Emory University, Atlanta, Georgia. dPanel Vice-Chiar, University of Iowa Hospitals and Clinics, Iowa City, Iowa.
e
Montefiore Medical Center, Bronx, New York. fOttawa Hospital Research Institute and the Department of Radiology, The University of Ottawa, Ottawa,
Ontario, Canada; Canadian Association of Radiologists. gRush University Medical Center, Chicago, Illinois; Neurosurgery expert. hThomas Jefferson
University Hospital, Philadelphia, Pennsylvania; Neurosurgery expert. iUniversity of Kansas Medical Center, Kansas City, Kansas. jEinstein Healthcare
Network, Philadelphia, Pennsylvania. kUniversity of California San Diego Medical Center, San Diego, California. lOregon Health & Science University,
Portland, Oregon. mUniversity of North Carolina School of Medicine, Chapel Hill, North Carolina; American Academy of Neurology. nAlbany ENT &
Allergy Services, PC, Albany, New York; American Academy of Otolaryngology-Head and Neck Surgery. oWalter Reed National Military Medical Center,
Bethesda, Maryland. pUT Southwestern Medical Center, Dallas, Texas. qColumbia University Medical Center, New York, New York. rSpecialty Chair,
University of California San Diego Health Center, San Diego, California.
The American College of Radiology seeks and encourages collaboration with other organizations on the development of the ACR Appropriateness
Criteria through society representation on expert panels. Participation by representatives from collaborating societies on the expert panel does not necessarily
imply individual or society endorsement of the final document.
Reprint requests to: publications@acr.org
ACR Appropriateness Criteria® 5 Headache
procedures for individuals presenting with headache unaccompanied by other neurological findings [19-24].
Discussion of Procedures by Variant
Variant 1: Sudden, severe headache or “worst headache of life.” Initial imaging.
Given the morbidity and mortality of SAH from ruptured aneurysm and other causes of acute intracranial
hemorrhage, imaging is often performed in patients presenting with a sudden, severe headache or “worst headache
of life.” The “Ottawa SAH rule” [25] and subsequent validations [26,27] are clinical inclusion and exclusion
criteria that are 100% sensitive but only 15% specific. These tools were designed to not miss SAH in this patient
population; however, they were not intended to independently diagnose SAH as the headache source.
Acute presentation may overlap with thunderclap-type primary headache [27-29] and reversible cerebral
vasoconstriction syndrome, characterized by recurrent episodes of thunderclap headache with or without
neurologic symptoms [30].
If intracranial hemorrhage is identified, or if there is also a new neurologic deficit, imaging should be guided by
the ACR Appropriateness Criteria® topic on “Cerebrovascular Disease” [4].
CT Head
The most appropriate initial imaging test in this clinical setting is a noncontrast head CT [31-33]. Negative
predictive value of CT, when performed with modern scanners within the first 6 hours of symptoms and
interpreted by a staff radiologist, might be as high as 99.9% [33,34]. A recent meta-analysis including 8,907
patients recorded an incidence of missed SAH of 1.46 per 1,000 in patients with classic thunderclap headache and
absence of trauma [35]. Failure to obtain the head CT accounts for 73% of misdiagnosis [36]. There is no
evidence to support the use of CT with intravenous (IV) contrast or CT without and with IV contrast in this
setting.
CTA Head
CT angiography (CTA) is not indicated as the initial imaging technique in isolation; however, it may be useful in
conjunction with a noncontrast head CT if there are 2 or more first-degree family members with aneurysmal
SAHs. The CPT code for CTA is inclusive of both a noncontrast head CT and the arterial phase scan. This
document acknowledges that some patients may be assessed at the time of noncontrast CT as to the need to
proceed with the angiographic portion of the examination, and there may be institutional practices that have
implications for clinical decision support. However, this document is for the initial imaging test, and
appropriateness of imaging once SAH is identified is guided by the ACR Appropriateness Criteria® topic on
“Cerebrovascular Disease” [4].
MRI Head
Although SAH can be detected on MRI, particularly fluid-attenuated inversion recovery sequences [37,38], there
are other etiologies for hyperintense fluid-attenuated inversion recovery signal in the cerebrospinal fluid spaces.
There is no evidence to support the use of MRI as the initial imaging in this setting given the accuracy of CT.
MRA Head
There is no relevant literature to support the use of MR angiography (MRA) in the initial imaging evaluation of a
patient in this setting. Imaging once SAH is identified is guided by the ACR Appropriateness Criteria® topic on
“Cerebrovascular Disease” [4].
Arteriography Cervicocerebral
Conventional angiogram is the gold standard of diagnostic tests used for evaluation of an aneurysm and for
reversible cerebral vasoconstriction syndrome; however, it is not a first-line test for this presentation. Imaging of
suspected infarct, and once SAH is identified, is guided by the ACR Appropriateness Criteria® topic on
“Cerebrovascular Disease” [4].
Variant 2: New headache with optic disc edema. Initial imaging.
The presence of bilateral disc edema indicates increased intracranial pressure transmitted to the optic nerve
sheath. The differential diagnosis for headache in the setting of bilateral disc edema includes secondary causes,
such as intracranial abscess, primary or metastatic tumors, hematoma, cerebral edema, communicating or
obstructive hydrocephalus [39,40], medications or medical conditions, and pseudotumor cerebri syndrome
associated with primary idiopathic intracranial hypertension or secondary to cerebral venous thrombosis. Patients
with idiopathic intracranial hypertension are usually obese females of childbearing age. However, imaging,
ACR Appropriateness Criteria® 6 Headache
preferably with MRI/MR venography (MRV) [41,42], is included in the diagnostic criteria of this condition, given
its association with venous thrombosis or venous sinus stenosis. Cerebral venous thrombosis is a potentially lethal
disorder also associated with prothrombotic states, pregnancy, oral contraceptives, and infection [43-45]. With
early diagnosis and institution of therapy, prognosis may be improved. Indications for and timing of lumbar
puncture are beyond the scope of this document.
CT Head
Noncontrast head CT is useful to assess for space-occupying processes, such as intracranial hemorrhage, mass
effect, macroadenoma causing optic chiasm compression, and hydrocephalus. Although findings such as high-
attenuation within the venous sinuses may be evident, there is wide variability of venous anatomic differences,
and noncontrast CT is not as accurate as dedicated venographic imaging for detection of venous sinus thrombosis
[46,47]. The use of contrast should be for venographic assessment, detailed in CT venogram (CTV) below.
Postcontrast head CT may be considered for patients unwilling or unable to undergo MRI for comprehensive
parenchymal evaluation.
CTV Head
The CPT code for CTV is inclusive of both a noncontrast head CT, the venous phase scan, and 3-D
reconstructions. In the setting of optic disc edema, this is a comprehensive evaluation for cerebral venous
thrombosis. Venographic imaging techniques are complementary to anatomic imaging and comparable to
accuracy of catheter angiography [48]. There is substantial literature regarding technique and pitfalls of
interpretation, which is beyond the scope of this document. Head-to-head comparisons between CTV and MRV
for diagnosis of cerebral venous thrombosis are historic, given that changes in technology with both methods
show superb accuracy [49,50].
MRI Head
MRI provides more accurate differentiation than CT of parenchymal or meningeal processes, which may be
contributing to symptoms. Findings such as pituitary flattening and optic nerve sheath thickness may persist
without clinically evident papilledema [51]. Brain MRI and MRV have been shown to increase the diagnostic
certainty for idiopathic intracranial hypertension when one or more of the following are present: partially empty
sella, flattening of the posterior ocular globe margins, and/or transverse sinus stenosis [52].
MRV Head
Dedicated MRV is complementary to the brain MRI evaluation and may be performed without or with IV contrast
depending on institutional preference. There is substantial literature regarding technique and pitfalls of
interpretation, which is beyond the scope of this document. Although venous sinus thrombosis and stenosis can be
detected on precontrast and postcontrast brain MRI sequences, the addition of MRV has improved accuracy for
the detection of venous pathology when compared with anatomic imaging alone [53].
Arteriography Cervicocerebral
There is no relevant literature to support the use of arteriography in the initial imaging evaluation of a patient in
this setting.
Variant 3: New or progressively worsening headache with one or more of the following ‘red flags’:
subacute head trauma, related activity or event (sexual activity, exertion, position), neurological deficit,
known or suspected cancer, immunosuppressed or immunocompromised state, currently pregnant, or 50
years of age or older. Initial imaging.
“Red flag” signs, symptoms, and comorbidities have been proposed as a means to increase specificity of imaging
in new or progressively worsening headaches [20,54-57]; however, the many proposed factors have not been
independently validated. The prevailing “red flag” is a new neurologic deficit. If a patient is presenting with
symptoms of a possible transient ischemic attack or acute stroke, the use of imaging should be guided by the ACR
Appropriateness Criteria® topic on “Cerebrovascular Disease” [4], not that the patient has a headache. Similarly,
patients with suspected meningitis or encephalitis are beyond the scope of this guideline.
Imaging in the setting of acute head trauma should be guided by the ACR Appropriateness Criteria® topic on
“Head Trauma” [5], noting the discrepancy that headache is an independent high-risk factor in the New Orleans
Criteria [58], but not in the Canadian CT Head Rule [59]. Post-traumatic headache begins within 7 days of the
injury and may mimic primary headache. A single prospective study with a cohort of 543 patients with history of
traumatic brain injury reported a prevalence of headache of 49% at 1 year follow-up [60].
ACR Appropriateness Criteria® 7 Headache
Headaches associated with cough, exertion, or sexual activity are uncommon and often a primary headache
syndrome. However, imaging has shown posterior fossa processes or SAH in some cases [61] and symptoms
attributed to venous stenoses [62] and reversible cerebral vasoconstriction syndrome in others [63,64].
Manifestations of spontaneous intracranial hypotension are variable [65-67]. Comprehensive diagnostic criteria
encompassing the varied manifestations of spontaneous intracranial hypotension have been proposed [68] based
on symptoms, lumbar puncture, imaging (CT myelography, MRI, MR myelography, or radionuclide
cisternography), and response to epidural blood patch.
Patients with known cancer should have head imaging when a headache develops or if there is a change in
headache characteristics [69].
Given risk for central nervous system infections, immunosuppressed and immunocompromised patients
presenting with a new or progressive headache will often undergo cerebrospinal fluid analysis. Indications for
lumbar puncture are beyond the scope of this document.
Pregnant patients with new, progressive, or changes in chronic headache patterns have higher yields of
abnormalities on imaging [70]; although, much of the literature on headache in pregnancy is centered on
examination rather than imaging findings [71-74]. Please see the Safety Considerations in Pregnant Patients
section below for details. For imaging of suspected pituitary apoplexy, see the ACR Appropriateness Criteria®
topic on “Neuroendocrine Imaging” [9].
CT Head
In all of these circumstances, noncontrast CT can be sufficient to exclude new hemorrhage, significant mass
effect, or hydrocephalus. Please see the Safety Considerations in Pregnant Patients section below for details.
There is no evidence to support the use of CT head with contrast as the initial imaging procedure in this clinical
setting.
CTA Head
There is no relevant literature to support the use of CTA in the initial imaging evaluation of a patient in this
setting.
MRI Head
MRI is a more comprehensive alternative to CT and depending on severity of symptoms and patient stability
could be the initial imaging procedure. In the setting of known malignancy, immunosuppressed, or
immunocompromised state, the addition of postcontrast imaging further helps in evaluation of any parenchymal
or meningeal process.
Please see the Safety Considerations in Pregnant Patients section below for details. For imaging specific to
suspected pituitary apoplexy, see the ACR Appropriateness Criteria® topic on “Neuroendocrine Imaging” [9].
MRA Head
There is no relevant literature to support the use of MRA in the initial imaging evaluation of a patient in this
setting.
Arteriography Cervicocerebral
There is no relevant literature to support the use of arteriography in the initial imaging evaluation of a patient in
this setting.
Variant 4: New headache. Classic migraine or tension-type primary headache. Normal neurologic
examination. Initial imaging.
Migraine and tension-type headaches have been ranked in the top 5 most prevalent disorders in the world [75].
The International Classification of Headache Disorders-3 notes overlap in symptoms of tension-type and mild
forms of migraine [10]. Prevalence studies on migraine show that genetic factors and gender differences are
related to migraines and affect approximately 15% to 18% of women and 6% of men [76]. Studies performed
under low pretest probability conditions may be more likely to result in false-positive results [19,23,77,78], with
the consequential risk of additional and unnecessary procedures.
The ACR in the Choosing Wisely campaign (http://www.choosingwisely.org) recommends against imaging for
primary headache. For patients meeting criteria of these primary headache syndromes, having no red flags and a
normal neurological examination, neuroimaging is not necessary based upon the current available data [79].
ACR Appropriateness Criteria® 8 Headache
Clinically, a patient presenting with a new migraine with aura can mimic transient ischemic attack or acute stroke
[80]. If there is a new neurologic deficit, imaging should be guided by the ACR Appropriateness Criteria® topic
on “Cerebrovascular Disease” [4], not that the patient has a headache.
CT Head
Head CT scans have been shown to yield positive results in only 0.4% of patients that are referred with a
nontraumatic headache [81].
CTA Head
There is no relevant literature to support the use of CTA in the initial imaging evaluation of a patient in this
setting.
CTV Head
There is no relevant literature to support the use of CTV in the initial imaging evaluation of a patient in this
setting.
MRI Head
Several studies have assessed prevalence of white matter lesions in patients with migraines compared with other
headache patterns and normal populations; however, the extent and distribution have not correlated with
symptoms or affected management [82-85]. Population cohorts in Australia [86] and the United Kingdom [87]
have not shown any clinical value in imaging of patients with migraine with aura.
MRA Head
Studies evaluating MRA have shown no contribution to diagnosis or management for migraine with or without
aura [88].
MRV Head
There is no relevant literature to support the use of MRV in the initial imaging evaluation of a patient in this
setting.
Arteriography Cervicocerebral
There is no relevant literature to support the use of arteriography in the initial imaging evaluation of a patient in
this setting.
Variant 5: New primary headache of suspected trigeminal autonomic origin. Initial imaging.
Trigeminal autonomic cephalalgia is a primary headache disorder characterized by unilateral trigeminal
distribution pain with ipsilateral cranial autonomic signs and symptoms. Cluster headache is the only relatively
common member of this headache disorder family. The others are rare and are characterized by short attacks:
paroxysmal hemicrania, hemicrania continua, short unilateral neuralgiform headache attacks with unilateral
conjunctival injection and tearing, and short-lasting unilateral neuralgiform headache with cranial autonomic
symptoms. Paroxysmal hemicranias are more frequent, and individual attacks are shorter in duration when
compared with cluster headache.
There is an unexplained association with pituitary macroadenomas, which are found in 4 % of cluster headache
patients [89]. Microvascular compression has also been associated [90] and the ophthalmic form of trigeminal
neuralgia may be confused with these entities [91,92]; however, imaging in trigeminal neuralgia should be guided
by the ACR Appropriateness Criteria® topic on “Cranial Neuropathy” [6].
CT Head
CT may reveal suprasellar extent of a pituitary mass; however, it is less sensitive than MRI for evaluation of sella
processes.
CTA Head
There is no relevant literature to support the use of CTA in the initial imaging evaluation of a patient in this
setting.
MRI Head
Brain MRI without and with IV contrast is usually appropriate to perform at least once in an individual’s lifetime
when presenting with a primary headache of suspected trigeminal autonomic origin, inclusive of evaluation for a
pituitary mass [90,93]. Imaging for suspected vascular compression on the trigeminal nerve is guided by the ACR
Appropriateness Criteria® topic on “Cranial Neuropathy” [6].
ACR Appropriateness Criteria® 9 Headache
MRA Head
There is no relevant literature to support the use of MRA in the initial imaging evaluation of a patient in this
setting. Imaging in the setting of suspected trigeminal neuralgia should be guided by the ACR Appropriateness
Criteria® topic on “Cranial Neuropathy” [6].
Arteriography Cervicocerebral
There is no relevant literature to support the use of arteriography in the initial imaging evaluation of a patient in
this setting.
Variant 6: Chronic headache. No new features. No neurologic deficit. Initial imaging.
Chronic daily headache may be one of the primary headache subtypes or may be secondary to another disease
process; however, is characterized by long-duration of having headaches on 15 or more days per month.
Chronic migraine comprises 3% of all migraines, with a prevalence rate of 0.67% [94,95]. These headaches often
worsen in the setting of medication overuse whether analgesic or antimigraine medications [96]. In adult with
migraine, with no recent change in attack pattern, history of seizures, or other focal neurological symptoms or
signs, the routine use of neuroimaging is usually not warranted [57]. The yield of detecting abnormal, treatable
lesions by CT or MRI in patients with headache but normal neurological examination has been found to be low,
reported as 0.18% by Frishberg [81]. The American Headache Society guidelines advise against the use of
neuroimaging in patients with stable headaches that meet criteria for migraines [22]. The American College of
Radiology Ten Things Physicians and Patients Should Question document states: “Don’t do imaging for
uncomplicated headache. Imaging in headache patients absent specific risk factors for structural disease is not
likely to change management or improve outcome [97].”
Sempere et al [23] reported a 0.9% probability for a significant intracranial finding in chronic headache (as
defined as lasting at least 4 weeks) with a normal neurologic examination. The incidence of pathology identified
by imaging in the chronic headache group is similar to that encountered in the general population, reported as
0.7% to 6.5% [98,99].
In the face of increased imaging utilization, Gilbert et al [19] published an overall decrease in diagnostic yield for
intracranial pathology in atraumatic headache patients. They reviewed the trends in CT and MRI use in the United
States for emergency department patients with atraumatic headache from 1998 to 2008 and reported that the
percentage of this patient group who underwent imaging increased from 12.5% to 31%, whereas the prevalence of
intracranial pathology detected decreased from 10.1% to 3.5%. They noticed an important demographic difference
in the yield of the examination with conditions associated with intracranial pathology detected in 10.4% in
patient’s ≥50 years of age, but only a 2.3% yield in the patient group <50 years of age. Patients presenting with a
nonmigraine type headache had a 5.2% yield of conditions associated with intracranial pathology on imaging,
whereas imaging in the migraine patient group had a yield of 1.0%. They also reported an increased length of stay
in the emergency department for patients who received imaging.
CT Head
In the evaluation of patients with chronic headache with no new features and no concerning findings on clinical or
physical examination, there is no relevant literature to support the use of CT head in the initial evaluation.
The American Headache Society guidelines and the Choosing Wisely Campaign advise against the use of
neuroimaging in patients with stable headaches that meet criteria for migraines [22]. This document went on to
state that many headache patients have previously undergone imaging and that “in many situations, it is very
unlikely that a repeat imaging study of the head will identify any abnormality that will alter management.”
The American College of Radiology Ten Things Physicians and Patients Should Question document states “Don’t
do imaging for uncomplicated headache. Imaging in headache patients absent specific risk factors for structural
disease is not likely to change management or improve outcome [97].”
The yield of detecting abnormal, treatable lesions by CT or MRI in patients with headache and a normal
neurological examination was found to be very low as reported by Frishberg [81] and Sempere [23]. Additionally,
the incidence of pathology identified by imaging in the chronic headache group is similar to that encountered in
the general population [98,99]. Further, a study by Miller et al [100] found no increase in missed diagnosis
proportions in association with an overall 9.6% decrease in head CT utilization in patients presenting to the
emergency department with headache.
ACR Appropriateness Criteria® 10 Headache
CTA Head
There is no role for CTA in patients with chronic headache with no new features and no concerning findings on
clinical or physical examination.
CTV Head
There is no role for CTV in patients with chronic headache with no new features and no concerning findings on
clinical or physical examination.
MRI Head
In the evaluation of patients with chronic headache with no new features and no concerning findings on clinical or
physical examination, there is no relevant literature to support the use of MRI head in the initial evaluation.
The American Headache Society guidelines and the Choosing Wisely Campaign advise against the use of
neuroimaging in patients with stable headaches that meet criteria for migraines [22]. This document went on to
state that many headache patients have previously undergone imaging and that “in many situations, it is very
unlikely that a repeat imaging study of the head will identify any abnormality that will alter management.”
The American College of Radiology Ten Things Physicians and Patients Should Question document states “Don’t
do imaging for uncomplicated headache. Imaging in headache patients absent specific risk factors for structural
disease is not likely to change management or improve outcome [97].”
The yield of detecting abnormal, treatable lesions by CT or MRI in patients with headache and a normal
neurological examination was found to be very low as reported by Frishberg [81] and Sempere [23]. Additionally,
the incidence of pathology identified by imaging in the chronic headache group is similar to that encountered in
the general population [98,99].
MRA Head
There is no role for MRA in patients with chronic headache with no new features and no concerning findings on
clinical or physical examination.
MRV Head
There is no role for MRV in patients with chronic headache with no new features and no concerning findings on
clinical or physical examination.
Arteriography Cervicocerebral
There is no role for arteriography in patients with chronic headache with no new features and no concerning
findings on clinical or physical examination.
Variant 7: Chronic headache. New features or increasing frequency. Initial Imaging.
In cases with underlying pathology, patients typically present with new headache features or focal neurological
symptoms. In a retrospective review of the presentation of 111 patients with brain tumors, headache was a
symptom in 48% equally for primary and metastatic tumors [101]. Headaches were similar to tension-type in
77%, migraine type in 9%, and other types in 14%. The typical headache was bifrontal but worse ipsilaterally and
headache was the worst symptom in 45% of patients [101]. Further workup is indicated including neurologic
imaging in patients for whom the frequency, severity, or character of headache changes in the setting of a prior
history of benign headaches [17,102]. Headache increasing in frequency or severity is considered a “red flag”
[55].
CT Head
Noncontrast CT can be sufficient to exclude new hemorrhage, significant mass effect, or hydrocephalus. The
American Headache Society recommends “against CT when MRI is available, except in emergency situations”
[22,103]. CT with IV contrast should not be performed as the sole imaging test in the acute setting; contrast
material may obscure hemorrhage(s). CT without and with IV contrast may be helpful to exclude acute
intracranial hemorrhage and evaluate for potential leptomeningeal or dural enhancing lesion(s).
CTA Head
There is no relevant literature to support the use of CTA in the initial imaging evaluation of a patient in this
setting.
CTV Head
There is no relevant literature to support the use of CTV in the initial imaging evaluation of a patient in this
ACR Appropriateness Criteria® 11 Headache
setting.
MRI Head
MRI is a more comprehensive alternative to CT and in the setting of a stable patient should be the initial imaging
procedure. American Headache Society recommends “against CT when MRI is available, except in emergency
situations” [22,103]. Contrast administration will aid in detection and assessment of intracranial pathology and
brain MRI without and with IV contrast should be obtained in the setting of suspected intracranial mass or
infection.
MRA Head
There is no relevant literature to support the use of MRA in the initial imaging evaluation of a patient in this
setting.
Arteriography Cervicocerebral
There is no relevant literature to support the use of arteriography in the initial imaging evaluation of a patient in
this setting.
Summary of Recommendations
• Variant 1: In patients with sudden, severe headache or worst headache of their life, CT head without IV
contrast is usually appropriate for initial imaging. The panel did not agree on recommending CTA head with
IV contrast for patients in this clinical setting. There is insufficient medical literature to conclude whether or
not these patients would benefit from this procedure. The use of CTA head with IV contrast as an initial
imaging approach in this patient population is controversial but may be appropriate.
• Variant 2: In patients with new headache and optic disc edema, MRI head without and with IV contrast, MRI
head without IV contrast, or CT head without IV contrast are usually appropriate for the initial imaging.
These procedures are equivalent alternatives (ie, only one procedure will be ordered to provide the clinical
information to effectively manage the patient’s care).
• Variant 3: In patients with new or progressively worsening headache with one or more of the following “red
flags” of subacute head trauma, related activity or event (sexual activity, exertion, position), neurological
deficit, known or suspected cancer, immunosuppressed or immunocompromised state, age 50 years or older,
CT head without IV contrast, MRI head without and with IV contrast, or MRI head without IV contrast is
usually appropriate for the initial imaging. Pregnancy is also considered a “red flag” condition, with separate
considerations for radiation and contrast exposure. These procedures are equivalent alternatives (ie, only one
procedure will be ordered to provide the clinical information to effectively manage the patient’s care).
• Variant 4: Imaging is usually not appropriate for the initial imaging of patients with new primary migraine or
tension-type headache, with normal neurologic examination.
• Variant 5: In patients with new primary headache of suspected trigeminal autonomic origin, MRI head
without and with IV contrast is usually appropriate for the initial imaging.
• Variant 6: Imaging is usually not appropriate for the initial imaging of patients with chronic headache, no
new features and with no neurologic deficit.
• Variant 7: In patients with chronic headache presenting with new features or increasing frequency, MRI head
without and with IV contrast or MRI head without IV contrast is usually appropriate for the initial imaging.
These procedures are equivalent alternatives.
Supporting Documents
The evidence table, literature search, and appendix for this topic are available at https://acsearch.acr.org/list. The
appendix includes the strength of evidence assessment and the final rating round tabulations for each
recommendation.
For additional information on the Appropriateness Criteria methodology and other supporting documents go to
www.acr.org/ac.
Safety Considerations in Pregnant Patients
Imaging of the pregnant patient can be challenging, particularly with respect to minimizing radiation exposure
and risk. For further information and guidance, see the following ACR documents:
ACR Appropriateness Criteria® 12 Headache
• ACR–SPR Practice Parameter for the Safe and Optimal Performance of Fetal Magnetic Resonance Imaging
(MRI) [104]
• ACR-SPR Practice Parameter for Imaging Pregnant or Potentially Pregnant Adolescents and Women with
Ionizing Radiation [105]
• ACR-ACOG-AIUM-SMFM-SRU Practice Parameter for the Performance of Standard Diagnostic Obstetrical
Ultrasound [106]
• ACR Manual on Contrast Media [107]
• ACR Guidance Document on MR Safe Practices; 2013 [108]
Appropriateness Category Names and Definitions
Appropriateness
Appropriateness Category Name Appropriateness Category Definition
Rating
The imaging procedure or treatment is indicated in
Usually Appropriate 7, 8, or 9 the specified clinical scenarios at a favorable risk-
benefit ratio for patients.
The imaging procedure or treatment may be
indicated in the specified clinical scenarios as an
May Be Appropriate 4, 5, or 6 alternative to imaging procedures or treatments with
a more favorable risk-benefit ratio, or the risk-benefit
ratio for patients is equivocal.
The individual ratings are too dispersed from the
panel median. The different label provides
May Be Appropriate transparency regarding the panel’s recommendation.
5
(Disagreement) “May be appropriate” is the rating category and a
rating of 5 is assigned.
The imaging procedure or treatment is unlikely to be
indicated in the specified clinical scenarios, or the
Usually Not Appropriate 1, 2, or 3 risk-benefit ratio for patients is likely to be
unfavorable.
Relative Radiation Level Information
Potential adverse health effects associated with radiation exposure are an important factor to consider when
selecting the appropriate imaging procedure. Because there is a wide range of radiation exposures associated with
different diagnostic procedures, a relative radiation level (RRL) indication has been included for each imaging
examination. The RRLs are based on effective dose, which is a radiation dose quantity that is used to estimate
population total radiation risk associated with an imaging procedure. Patients in the pediatric age group are at
inherently higher risk from exposure, because of both organ sensitivity and longer life expectancy (relevant to the
long latency that appears to accompany radiation exposure). For these reasons, the RRL dose estimate ranges for
pediatric examinations are lower as compared with those specified for adults (see Table below). Additional
information regarding radiation dose assessment for imaging examinations can be found in the ACR
Appropriateness Criteria® Radiation Dose Assessment Introduction document [109].
ACR Appropriateness Criteria® 13 Headache
Relative Radiation Level Designations
Adult Effective Dose Estimate Pediatric Effective Dose Estimate
Relative Radiation Level*
Range Range
O 0 mSv 0 mSv
☢ <0.1 mSv <0.03 mSv
☢☢ 0.1-1 mSv 0.03-0.3 mSv
☢☢☢ 1-10 mSv 0.3-3 mSv
☢☢☢☢ 10-30 mSv 3-10 mSv
☢☢☢☢☢ 30-100 mSv 10-30 mSv
*RRL assignments for some of the examinations cannot be made, because the actual patient doses in these procedures vary
as a function of a number of factors (eg, region of the body exposed to ionizing radiation, the imaging guidance that is
used). The RRLs for these examinations are designated as “Varies.”
References
1. Mafi JN, Edwards ST, Pedersen NP, Davis RB, McCarthy EP, Landon BE. Trends in the ambulatory
management of headache: analysis of NAMCS and NHAMCS data 1999-2010. J Gen Intern Med
2015;30:548-55.
2. Stovner L, Hagen K, Jensen R, et al. The global burden of headache: a documentation of headache
prevalence and disability worldwide. Cephalalgia 2007;27:193-210.
3. Stovner LJ, Andree C. Prevalence of headache in Europe: a review for the Eurolight project. J Headache
Pain 2010;11:289-99.
4. Salmela MB, Mortazavi S, Jagadeesan BD, et al. ACR Appropriateness Criteria(R) Cerebrovascular
Disease. J Am Coll Radiol 2017;14:S34-S61.
5. Shetty VS, Reis MN, Aulino JM, et al. ACR Appropriateness Criteria Head Trauma. J Am Coll Radiol
2016;13:668-79.
6. Policeni B, Corey AS, Burns J, et al. ACR Appropriateness Criteria(R) Cranial Neuropathy. J Am Coll
Radiol 2017;14:S406-S20.
7. Kennedy TA, Corey AS, Policeni B, et al. ACR Appropriateness Criteria® Orbits Vision and Visual
Loss. J Am Coll Radiol 2018;15:S116-S31.
8. Kirsch CFE, Bykowski J, Aulino JM, et al. ACR Appropriateness Criteria(R) Sinonasal Disease. J Am
Coll Radiol 2017;14:S550-S59.
9. American College of Radiology. ACR Appropriateness Criteria®: Neuroendocrine Imaging. Available at:
https://acsearch.acr.org/docs/69485/Narrative/. Accessed March 30, 2019.
10. Olesen J. International Classification of Headache Disorders. Lancet Neurol 2018;17:396-97.
11. Cvetkovic VV, Strineka M, Knezevic-Pavlic M, Tumpic-Jakovic J, Lovrencic-Huzjan A. Analysis of
headache management in emergency room. Acta Clin Croat 2013;52:281-8.
12. Eller M, Goadsby PJ. MRI in headache. Expert Rev Neurother 2013;13:263-73.
13. Nallasamy K, Singhi SC, Singhi P. Approach to headache in emergency department. Indian J Pediatr
2012;79:376-80.
14. Silberstein SD, Lipton R, Goadsby PJ. Headache in Clinical Practice. In: Olesen J, Tfelt-Hansen P,
Welsch KMA, eds. The Headaches. 2nd ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2000.
15. Mitsikostas DD. Nocebo in headache. Curr Opin Neurol 2016;29:331-6.
16. Douglas AC, Wippold FJ, 2nd, Broderick DF, et al. ACR Appropriateness Criteria Headache. J Am Coll
Radiol 2014;11:657-67.
17. Lester MS, Liu BP. Imaging in the evaluation of headache. Med Clin North Am 2013;97:243-65.
18. May A. Pearls and pitfalls: neuroimaging in headache. Cephalalgia 2013;33:554-65.
19. Gilbert JW, Johnson KM, Larkin GL, Moore CL. Atraumatic headache in US emergency departments:
recent trends in CT/MRI utilisation and factors associated with severe intracranial pathology. Emerg Med
J 2012;29:576-81.
20. Kernick DP, Ahmed F, Bahra A, et al. Imaging patients with suspected brain tumour: guidance for
primary care. Br J Gen Pract 2008;58:880-5.
ACR Appropriateness Criteria® 14 Headache
21. Kuruvilla DE, Lipton RB. Appropriate use of neuroimaging in headache. Curr Pain Headache Rep
2015;19:17.
22. Loder E, Weizenbaum E, Frishberg B, Silberstein S. Choosing wisely in headache medicine: the
American Headache Society's list of five things physicians and patients should question. Headache
2013;53:1651-9.
23. Sempere AP, Porta-Etessam J, Medrano V, et al. Neuroimaging in the evaluation of patients with non-
acute headache. Cephalalgia 2005;25:30-5.
24. Tsushima Y, Endo K. MR imaging in the evaluation of chronic or recurrent headache. Radiology
2005;235:575-9.
25. Perry JJ, Stiell IG, Sivilotti ML, et al. High risk clinical characteristics for subarachnoid haemorrhage in
patients with acute headache: prospective cohort study. BMJ 2010;341:c5204.
26. Bellolio MF, Hess EP, Gilani WI, et al. External validation of the Ottawa subarachnoid hemorrhage
clinical decision rule in patients with acute headache. Am J Emerg Med 2015;33:244-9.
27. Perry JJ, Stiell IG, Sivilotti ML, et al. Clinical decision rules to rule out subarachnoid hemorrhage for
acute headache. JAMA 2013;310:1248-55.
28. Mortimer AM, Bradley MD, Stoodley NG, Renowden SA. Thunderclap headache: diagnostic
considerations and neuroimaging features. Clin Radiol 2013;68:e101-13.
29. Schwedt TJ. Thunderclap headaches: a focus on etiology and diagnostic evaluation. Headache
2013;53:563-9.
30. Mehdi A, Hajj-Ali RA. Reversible cerebral vasoconstriction syndrome: a comprehensive update. Curr
Pain Headache Rep 2014;18:443.
31. Quon JS, Glikstein R, Lim CS, Schwarz BA. Computed tomography for non-traumatic headache in the
emergency department and the impact of follow-up testing on altering the initial diagnosis. Emerg Radiol
2015;22:521-5.
32. Carpenter CR, Hussain AM, Ward MJ, et al. Spontaneous Subarachnoid Hemorrhage: A Systematic
Review and Meta-analysis Describing the Diagnostic Accuracy of History, Physical Examination,
Imaging, and Lumbar Puncture With an Exploration of Test Thresholds. Acad Emerg Med 2016;23:963-
1003.
33. Perry JJ, Stiell IG, Sivilotti ML, et al. Sensitivity of computed tomography performed within six hours of
onset of headache for diagnosis of subarachnoid haemorrhage: prospective cohort study. BMJ
2011;343:d4277.
34. Blok KM, Rinkel GJ, Majoie CB, et al. CT within 6 hours of headache onset to rule out subarachnoid
hemorrhage in nonacademic hospitals. Neurology 2015;84:1927-32.
35. Dubosh NM, Bellolio MF, Rabinstein AA, Edlow JA. Sensitivity of Early Brain Computed Tomography
to Exclude Aneurysmal Subarachnoid Hemorrhage: A Systematic Review and Meta-Analysis. Stroke
2016;47:750-5.
36. Suarez JI, Tarr RW, Selman WR. Aneurysmal subarachnoid hemorrhage. N Engl J Med 2006;354:387-
96.
37. da Rocha AJ, da Silva CJ, Gama HP, et al. Comparison of magnetic resonance imaging sequences with
computed tomography to detect low-grade subarachnoid hemorrhage: Role of fluid-attenuated inversion
recovery sequence. J Comput Assist Tomogr 2006;30:295-303.
38. Mohamed M, Heasly DC, Yagmurlu B, Yousem DM. Fluid-attenuated inversion recovery MR imaging
and subarachnoid hemorrhage: not a panacea. AJNR Am J Neuroradiol 2004;25:545-50.
39. Kirby S, Purdy RA. Headaches and brain tumors. Neurol Clin 2014;32:423-32.
40. Montella S, Ranieri A, Marchese M, De Simone R. Primary stabbing headache: a new dural sinus
stenosis-associated primary headache? Neurol Sci 2013;34 Suppl 1:S157-9.
41. Friedman DI, Jacobson DM. Diagnostic criteria for idiopathic intracranial hypertension. Neurology
2002;59:1492-5.
42. Friedman DI, Liu GT, Digre KB. Revised diagnostic criteria for the pseudotumor cerebri syndrome in
adults and children. Neurology 2013;81:1159-65.
43. Sidhom Y, Mansour M, Messelmani M, et al. Cerebral venous thrombosis: clinical features, risk factors,
and long-term outcome in a Tunisian cohort. J Stroke Cerebrovasc Dis 2014;23:1291-5.
44. Sparaco M, Feleppa M, Bigal ME. Cerebral Venous Thrombosis and Headache--A Case-Series. Headache
2015;55:806-14.
ACR Appropriateness Criteria® 15 Headache
45. Timoteo A, Inacio N, Machado S, Pinto AA, Parreira E. Headache as the sole presentation of cerebral
venous thrombosis: a prospective study. J Headache Pain 2012;13:487-90.
46. Avsenik J, Oblak JP, Popovic KS. Non-contrast computed tomography in the diagnosis of cerebral
venous sinus thrombosis. Radiol Oncol 2016;50:263-8.
47. Saposnik G, Barinagarrementeria F, Brown RD, Jr., et al. Diagnosis and management of cerebral venous
thrombosis: a statement for healthcare professionals from the American Heart Association/American
Stroke Association. Stroke 2011;42:1158-92.
48. Wetzel SG, Kirsch E, Stock KW, Kolbe M, Kaim A, Radue EW. Cerebral veins: comparative study of CT
venography with intraarterial digital subtraction angiography. AJNR Am J Neuroradiol 1999;20:249-55.
49. Gaikwad AB, Mudalgi BA, Patankar KB, Patil JK, Ghongade DV. Diagnostic role of 64-slice
multidetector row CT scan and CT venogram in cases of cerebral venous thrombosis. Emerg Radiol
2008;15:325-33.
50. Khandelwal N, Agarwal A, Kochhar R, et al. Comparison of CT venography with MR venography in
cerebral sinovenous thrombosis. AJR Am J Roentgenol 2006;187:1637-43.
51. Chang RO, Marshall BK, Yahyavi N, et al. Neuroimaging Features of Idiopathic Intracranial
Hypertension Persist After Resolution of Papilloedema. Neuroophthalmology 2016;40:165-70.
52. Maralani PJ, Hassanlou M, Torres C, et al. Accuracy of brain imaging in the diagnosis of idiopathic
intracranial hypertension. Clin Radiol 2012;67:656-63.
53. Morris PP, Black DF, Port J, Campeau N. Transverse Sinus Stenosis Is the Most Sensitive MR Imaging
Correlate of Idiopathic Intracranial Hypertension. AJNR Am J Neuroradiol 2017;38:471-77.
54. Detsky ME, McDonald DR, Baerlocher MO, Tomlinson GA, McCrory DC, Booth CM. Does this patient
with headache have a migraine or need neuroimaging? JAMA 2006;296:1274-83.
55. Holle D, Obermann M. The role of neuroimaging in the diagnosis of headache disorders. Ther Adv
Neurol Disord 2013;6:369-74.
56. M S, Lamont AC, Alias NA, Win MN. Red flags in patients presenting with headache: clinical
indications for neuroimaging. Br J Radiol 2003;76:532-5.
57. Sandrini G, Friberg L, Coppola G, et al. Neurophysiological tests and neuroimaging procedures in non-
acute headache (2nd edition). Eur J Neurol 2011;18:373-81.
58. Haydel MJ, Preston CA, Mills TJ, Luber S, Blaudeau E, DeBlieux PM. Indications for computed
tomography in patients with minor head injury. N Engl J Med 2000;343:100-5.
59. Stiell IG, Wells GA, Vandemheen K, et al. The Canadian CT Head Rule for patients with minor head
injury. Lancet 2001;357:1391-6.
60. Xu H, Pi H, Ma L, Su X, Wang J. Incidence of Headache After Traumatic Brain Injury in China: A Large
Prospective Study. World Neurosurg 2016;88:289-96.
61. Alvarez R, Ramon C, Pascual J. Clues in the differential diagnosis of primary vs secondary cough,
exercise, and sexual headaches. Headache 2014;54:1560-2.
62. Donnet A, Valade D, Houdart E, et al. Primary cough headache, primary exertional headache, and
primary headache associated with sexual activity: a clinical and radiological study. Neuroradiology
2013;55:297-305.
63. Pascual J, Gonzalez-Mandly A, Martin R, Oterino A. Headaches precipitated by cough, prolonged
exercise or sexual activity: a prospective etiological and clinical study. J Headache Pain 2008;9:259-66.
64. Yeh YC, Fuh JL, Chen SP, Wang SJ. Clinical features, imaging findings and outcomes of headache
associated with sexual activity. Cephalalgia 2010;30:1329-35.
65. Mokri B, Ahlskog JE, Luetmer PH. Chorea as a manifestation of spontaneous CSF leak. Neurology
2006;67:1490-1.
66. Schievink WI, Maya MM. Quadriplegia and cerebellar hemorrhage in spontaneous intracranial
hypotension. Neurology 2006;66:1777-8.
67. Syed NA, Mirza FA, Pabaney AH, Rameez ul H. Pathophysiology and management of spontaneous
intracranial hypotension--a review. J Pak Med Assoc 2012;62:51-5.
68. Schievink WI, Maya MM, Louy C, Moser FG, Tourje J. Diagnostic criteria for spontaneous spinal CSF
leaks and intracranial hypotension. AJNR Am J Neuroradiol 2008;29:853-6.
69. Nye BL, Ward TN. Clinic and Emergency Room Evaluation and Testing of Headache. Headache
2015;55:1301-8.
70. Ramchandren S, Cross BJ, Liebeskind DS. Emergent headaches during pregnancy: correlation between
neurologic examination and neuroimaging. AJNR Am J Neuroradiol 2007;28:1085-7.
ACR Appropriateness Criteria® 16 Headache
71. Azizyan A, Miller JM, Azzam RI, et al. Spontaneous retroclival hematoma in pituitary apoplexy: case
series. J Neurosurg 2015;123:808-12.
72. Jho DH, Biller BM, Agarwalla PK, Swearingen B. Pituitary apoplexy: large surgical series with grading
system. World Neurosurg 2014;82:781-90.
73. Kim WJ, Shin HY, Kim YC, Moon JY. Clinical Association Between Brain MRI Findings With Epidural
Blood Patch in Spontaneous Intracranial Hypotension. J Neurosurg Anesthesiol 2016;28:147-52.
74. Robbins MS, Farmakidis C, Dayal AK, Lipton RB. Acute headache diagnosis in pregnant women: a
hospital-based study. Neurology 2015;85:1024-30.
75. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and
injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet
2016;388:1545-602.
76. Stewart WF, Wood C, Reed ML, Roy J, Lipton RB. Cumulative lifetime migraine incidence in women
and men. Cephalalgia 2008;28:1170-8.
77. Becker LA, Green LA, Beaufait D, Kirk J, Froom J, Freeman WL. Use of CT scans for the investigation
of headache: a report from ASPN, Part 1. J Fam Pract 1993;37:129-34.
78. Goldstein JN, Camargo CA, Jr., Pelletier AJ, Edlow JA. Headache in United States emergency
departments: demographics, work-up and frequency of pathological diagnoses. Cephalalgia 2006;26:684-
90.
79. Katz M. The Cost-Effective Evaluation of Uncomplicated Headache. Med Clin North Am
2016;100:1009-17.
80. Lebedeva ER, Gurary NM, Gilev DV, Olesen J. Prospective testing of ICHD-3 beta diagnostic criteria for
migraine with aura and migraine with typical aura in patients with transient ischemic attacks. Cephalalgia
2018;38:561-67.
81. Frishberg BM. The utility of neuroimaging in the evaluation of headache in patients with normal
neurologic examinations. Neurology 1994;44:1191-7.
82. Dinia L, Bonzano L, Albano B, et al. White matter lesions progression in migraine with aura: a clinical
and MRI longitudinal study. J Neuroimaging 2013;23:47-52.
83. Gaist D, Garde E, Blaabjerg M, et al. Migraine with aura and risk of silent brain infarcts and white matter
hyperintensities: an MRI study. Brain 2016;139:2015-23.
84. Honningsvag LM, Hagen K, Haberg A, Stovner LJ, Linde M. Intracranial abnormalities and headache: A
population-based imaging study (HUNT MRI). Cephalalgia 2016;36:113-21.
85. Kruit MC, Launer LJ, Ferrari MD, van Buchem MA. Infarcts in the posterior circulation territory in
migraine. The population-based MRI CAMERA study. Brain 2005;128:2068-77.
86. Vijiaratnam N, Barber D, Lim KZ, et al. Migraine: Does aura require investigation? Clin Neurol
Neurosurg 2016;148:110-4.
87. Clarke CE, Edwards J, Nicholl DJ, Sivaguru A. Imaging results in a consecutive series of 530 new
patients in the Birmingham Headache Service. J Neurol 2010;257:1274-8.
88. Paemeleire K, Proot P, De Keyzer K, Achten E, Crevits L. Magnetic resonance angiography of the circle
of Willis in migraine patients. Clin Neurol Neurosurg 2005;107:301-5.
89. Levy MJ, Matharu MS, Meeran K, Powell M, Goadsby PJ. The clinical characteristics of headache in
patients with pituitary tumours. Brain 2005;128:1921-30.
90. Williams M, Bazina R, Tan L, Rice H, Broadley SA. Microvascular decompression of the trigeminal
nerve in the treatment of SUNCT and SUNA. J Neurol Neurosurg Psychiatry 2010;81:992-6.
91. Favier I, van Vliet JA, Roon KI, et al. Trigeminal autonomic cephalgias due to structural lesions: a review
of 31 cases. Arch Neurol 2007;64:25-31.
92. Head Imaging Guidelines. 2011. Available at:
http://www.tmhp.com/RadiologyClinicalDecisionSupport/2011/HEAD%20IMAGING%20GUIDELINE
S%202011.pdf. Accessed March 30, 2019.
93. de Coo IF, Wilbrink LA, Haan J. Symptomatic Trigeminal Autonomic Cephalalgias. Curr Pain Headache
Rep 2015;19:39.
94. Bigal ME, Lipton RB. The prognosis of migraine. Curr Opin Neurol 2008;21:301-8.
95. Silberstein S, Loder E, Diamond S, Reed ML, Bigal ME, Lipton RB. Probable migraine in the United
States: results of the American Migraine Prevalence and Prevention (AMPP) study. Cephalalgia
2007;27:220-9.
ACR Appropriateness Criteria® 17 Headache
96. Hale N, Paauw DS. Diagnosis and treatment of headache in the ambulatory care setting: a review of
classic presentations and new considerations in diagnosis and management. Med Clin North Am
2014;98:505-27.
97. Choosing Wisely® An initiative of the ABIM Foundation. American College of Radiology. Ten Things
Physicians and Patients Should Question. Available at:
http://www.choosingwisely.org/societies/american-college-of-radiology/. Accessed March 30, 2019.
98. Morris Z, Whiteley WN, Longstreth WT, Jr., et al. Incidental findings on brain magnetic resonance
imaging: systematic review and meta-analysis. BMJ 2009;339:b3016.
99. Weber F, Knopf H. Incidental findings in magnetic resonance imaging of the brains of healthy young
men. J Neurol Sci 2006;240:81-4.
100. Miller DG, Vakkalanka P, Moubarek ML, Lee S, Mohr NM. Reduced Computed Tomography Use in the
Emergency Department Evaluation of Headache Was Not Followed by Increased Death or Missed
Diagnosis. West J Emerg Med 2018;19:319-26.
101. Forsyth PA, Posner JB. Headaches in patients with brain tumors: a study of 111 patients. Neurology
1993;43:1678-83.
102. Forde G, Duarte RA, Rosen N. Managing Chronic Headache Disorders. Med Clin North Am
2016;100:117-41.
103. Choosing Wisely® An initiative of the ABIM Foundation. Clinician Lists. Available at:
http://www.choosingwisely.org/clinician-lists/. Accessed March 30, 2019.
104. American College of Radiology. ACR–SPR Practice Parameter for the Safe and Optimal Performance of
Fetal Magnetic Resonance Imaging (MRI). Available at: https://www.acr.org/-
/media/ACR/Files/Practice-Parameters/mr-fetal.pdf. Accessed March 30, 2019.
105. American College of Radiology. ACR-SPR Practice Parameter for Imaging Pregnant or Potentially
Pregnant Adolescents and Women with Ionizing Radiation. Available at: https://www.acr.org/-
/media/ACR/Files/Practice-Parameters/pregnant-pts.pdf. Accessed March 30, 2019.
106. American College of Radiology. ACR-ACOG-AIUM-SMFM-SRU Practice Parameter for the
Performance of Standard Diagnostic Obstetrical Ultrasound. Available at: https://www.acr.org/-
/media/ACR/Files/Practice-Parameters/us-ob.pdf. Accessed March 30, 2019.
107. American College of Radiology. Manual on Contrast Media. Available at: https://www.acr.org/Clinical-
Resources/Contrast-Manual. Accessed March 30, 2019.
108. Kanal E, Barkovich AJ, Bell C, et al. ACR guidance document on MR safe practices: 2013. J Magn
Reson Imaging 2013;37:501-30.
109. American College of Radiology. ACR Appropriateness Criteria® Radiation Dose Assessment
Introduction. Available at: https://www.acr.org/-/media/ACR/Files/Appropriateness-
Criteria/RadiationDoseAssessmentIntro.pdf. Accessed March 30, 2019.
The ACR Committee on Appropriateness Criteria and its expert panels have developed criteria for determining appropriate imaging examinations for
diagnosis and treatment of specified medical condition(s). These criteria are intended to guide radiologists, radiation oncologists and referring physicians
in making decisions regarding radiologic imaging and treatment. Generally, the complexity and severity of a patient’s clinical condition should dictate the
selection of appropriate imaging procedures or treatments. Only those examinations generally used for evaluation of the patient’s condition are ranked.
Other imaging studies necessary to evaluate other co-existent diseases or other medical consequences of this condition are not considered in this
document. The availability of equipment or personnel may influence the selection of appropriate imaging procedures or treatments. Imaging techniques
classified as investigational by the FDA have not been considered in developing these criteria; however, study of new equipment and applications should
be encouraged. The ultimate decision regarding the appropriateness of any specific radiologic examination or treatment must be made by the referring
physician and radiologist in light of all the circumstances presented in an individual examination.
ACR Appropriateness Criteria® 18 Headache
You might also like
- Nursing Care Plan (Impaired Skin Integrity)Document4 pagesNursing Care Plan (Impaired Skin Integrity)arlee marquez91% (161)
- Cureus-Authors GuideDocument20 pagesCureus-Authors GuidequickdannyNo ratings yet
- Research Plan: (3) Research Problem/questions (The Aim of The Study and Research Questions/problems, IfDocument3 pagesResearch Plan: (3) Research Problem/questions (The Aim of The Study and Research Questions/problems, Ifquickdanny100% (3)
- Cast and Immobilization Techniques in OrthopaedicsDocument7 pagesCast and Immobilization Techniques in OrthopaedicsKimberly SungaNo ratings yet
- Contraindications in Malignancy Grid 2015Document1 pageContraindications in Malignancy Grid 2015Sharada NayakNo ratings yet
- Wound Ostomy Continence Skills ChecklistDocument4 pagesWound Ostomy Continence Skills ChecklistnorthweststaffingNo ratings yet
- (New) CGX-Immune RECORDING SCRIPTDocument4 pages(New) CGX-Immune RECORDING SCRIPTMuhammad JamalNo ratings yet
- Head To Toe Assessment Adult HealthDocument7 pagesHead To Toe Assessment Adult HealthFrancesca LopesNo ratings yet
- CT Head AnatomyDocument57 pagesCT Head AnatomyMaajid Mohi Ud Din Malik100% (1)
- QuizzDocument2 pagesQuizzClaudiu MocanuNo ratings yet
- Imaging Quiz #1 Questions: Choice Correct OrderDocument2 pagesImaging Quiz #1 Questions: Choice Correct OrderquickdannyNo ratings yet
- Cureus-Authors GuideDocument20 pagesCureus-Authors GuidequickdannyNo ratings yet
- TinnitusDocument22 pagesTinnitusraveedkhan632No ratings yet
- Sinonasal DiseaseDocument22 pagesSinonasal Diseasemonkass81No ratings yet
- Staging and Post-Therapy Assessment of Head and Neck CancerDocument49 pagesStaging and Post-Therapy Assessment of Head and Neck Cancermonkass81No ratings yet
- Seizures and EpilepsyDocument14 pagesSeizures and Epilepsymonkass81No ratings yet
- Low Back PainDocument22 pagesLow Back PainSF TifarinNo ratings yet
- Dyspnea-Suspected Cardiac Origin (Ischemia Already Excluded)Document20 pagesDyspnea-Suspected Cardiac Origin (Ischemia Already Excluded)Parth PatilNo ratings yet
- Suspected Spine InfectionDocument17 pagesSuspected Spine Infectionmonkass81No ratings yet
- Acute Nonspecific Chest Pain-Low Probability of Coronary Artery DiseaseDocument10 pagesAcute Nonspecific Chest Pain-Low Probability of Coronary Artery Diseasevictor contrerasNo ratings yet
- Adrenal Mass EvaluationDocument19 pagesAdrenal Mass Evaluationpj rakNo ratings yet
- Abnormal Uterine BleedingDocument12 pagesAbnormal Uterine Bleedingvictor contrerasNo ratings yet
- Hematuria PDFDocument11 pagesHematuria PDFPipitNo ratings yet
- Breast Implant Evaluation - NarrativeDocument25 pagesBreast Implant Evaluation - Narrativeopenlab.doisNo ratings yet
- Postmenopausal Subacute or Chronic Pelvic PainDocument9 pagesPostmenopausal Subacute or Chronic Pelvic PainM SNo ratings yet
- Acute Nonlocalized Abdominal PainDocument17 pagesAcute Nonlocalized Abdominal PainghassanNo ratings yet
- Renal Cell Carcinoma Staging (ACR Appropriateness Criteria)Document10 pagesRenal Cell Carcinoma Staging (ACR Appropriateness Criteria)Andrew TaliaferroNo ratings yet
- Ctmri GuideDocument12 pagesCtmri Guidebsmit-f19-392No ratings yet
- Breast PainDocument9 pagesBreast PainmarysrbNo ratings yet
- Abdominal Aortic Aneurysm-Interventional Planning and Follow-UpDocument13 pagesAbdominal Aortic Aneurysm-Interventional Planning and Follow-Upvictor contrerasNo ratings yet
- Referring Physician Ordering Guide: What To Order WhenDocument12 pagesReferring Physician Ordering Guide: What To Order Whenthomasfx10No ratings yet
- Indeterminate Renal Mass ACR Appropriateness CriteriaDocument10 pagesIndeterminate Renal Mass ACR Appropriateness CriteriaAndrew TaliaferroNo ratings yet
- Adiuvante Dei Gratia Doctorum Factionis: RadioDocument13 pagesAdiuvante Dei Gratia Doctorum Factionis: RadioVon HippoNo ratings yet
- MRI Magnetic Resonance ImagingDocument4 pagesMRI Magnetic Resonance ImagingiqbalNo ratings yet
- American College of Radiology ACR Appropriateness CriteriaDocument14 pagesAmerican College of Radiology ACR Appropriateness CriteriaChavo Delocho100% (1)
- ACR Appropriateness Criteria For HematuriaDocument8 pagesACR Appropriateness Criteria For HematuriaAndrew TaliaferroNo ratings yet
- Headache: Red Flags For HeadacheDocument46 pagesHeadache: Red Flags For Headache11-MH-HU-CARMEN ROSA SECCE PEDRAZANo ratings yet
- Enls v4 0 Sah Slides FinalDocument40 pagesEnls v4 0 Sah Slides FinalTariku GelesheNo ratings yet
- Criterios de ACR Enfermedades Cerebrovasculares-1Document27 pagesCriterios de ACR Enfermedades Cerebrovasculares-1Gabriela NotarioNo ratings yet
- Sumamry of CPRs in Ortho PT-Admission ExamDocument6 pagesSumamry of CPRs in Ortho PT-Admission ExamAliaa NasserNo ratings yet
- Universal Colleges of Parañaque College of NursingDocument41 pagesUniversal Colleges of Parañaque College of NursingRalph RubinNo ratings yet
- CT Scans in The EDDocument4 pagesCT Scans in The EDRadiologi RSUKHNo ratings yet
- ALMO Neurologic Disorders Part 1Document9 pagesALMO Neurologic Disorders Part 1Pebbles PangilinanNo ratings yet
- PAM SummaryDocument17 pagesPAM Summaryawezemss99No ratings yet
- 7.2 - EcgDocument115 pages7.2 - EcgM Iqbal khan MuhmmandNo ratings yet
- CLINICAL PATHWAY FOR BRONCHIAL ASTHMA atDocument2 pagesCLINICAL PATHWAY FOR BRONCHIAL ASTHMA atdrgrizahNo ratings yet
- Radiology ContrastDocument4 pagesRadiology ContrastsreekaasamNo ratings yet
- 3 - MRCP - Part One - Past-Papers - Sept 2015Document303 pages3 - MRCP - Part One - Past-Papers - Sept 2015zgjybbzNo ratings yet
- HandbookDocument50 pagesHandbookIcHii AzizNo ratings yet
- Clinical Pathway For Bronchial Asthma atDocument3 pagesClinical Pathway For Bronchial Asthma atwenda sariNo ratings yet
- ACR Appropriateness Criteria® Acute Chest Pain - Suspected Pulmonary Embolism.Document16 pagesACR Appropriateness Criteria® Acute Chest Pain - Suspected Pulmonary Embolism.Madalina TalpauNo ratings yet
- HA - PA Findings Documentation (Head To Neck)Document9 pagesHA - PA Findings Documentation (Head To Neck)Bianca SandovalNo ratings yet
- Case 23: Doorway InformationDocument7 pagesCase 23: Doorway InformationshyrouzdNo ratings yet
- Es - E E Ess. - Cat - E - E Es.: 0.: 4395 Previous Next Lab Values Notes Calculator Reverse Color Text ZoomDocument6 pagesEs - E E Ess. - Cat - E - E Es.: 0.: 4395 Previous Next Lab Values Notes Calculator Reverse Color Text ZoomAlex ChenNo ratings yet
- Sinus Rhythm and Sinus and Atrial DysrhythmiasDocument41 pagesSinus Rhythm and Sinus and Atrial Dysrhythmiasclaudia brongNo ratings yet
- Truspected Stroke AlgorithmDocument4 pagesTruspected Stroke Algorithmtri wahyunoNo ratings yet
- Algoritma Neck PainDocument12 pagesAlgoritma Neck PainAri SudarsonoNo ratings yet
- L1 Report TemplateDocument2 pagesL1 Report TemplateRasangi Sumudu Clare SuraweeraNo ratings yet
- What Do We Do About X?Document11 pagesWhat Do We Do About X?Okki Masitah Syahfitri NasutionNo ratings yet
- Symptomatic Epilepsy - Rijalun ArridhoDocument56 pagesSymptomatic Epilepsy - Rijalun Arridhosri hartini putriNo ratings yet
- Case Presentation On Supraventricular TachycardiaDocument64 pagesCase Presentation On Supraventricular TachycardiaHazel AsperaNo ratings yet
- CVDDocument24 pagesCVDchris the greatNo ratings yet
- CT vs. Mri Compendium 2011 1 PDFDocument4 pagesCT vs. Mri Compendium 2011 1 PDFWaqas HaleemNo ratings yet
- Neuro Module Part 1Document194 pagesNeuro Module Part 1Gabriel GhiațăNo ratings yet
- Module 4bDocument24 pagesModule 4bSuharto SanduyoganNo ratings yet
- Neurology Shifting Exam: CnvandcnviiDocument9 pagesNeurology Shifting Exam: CnvandcnviicarlosNo ratings yet
- JurnalDocument18 pagesJurnalAurima Hanun KusumaNo ratings yet
- Module 5 Doppler Imaging BDocument31 pagesModule 5 Doppler Imaging BquickdannyNo ratings yet
- IFEST ProposalDocument1 pageIFEST ProposalquickdannyNo ratings yet
- Doppler Ultrasound - L1Document24 pagesDoppler Ultrasound - L1quickdannyNo ratings yet
- Varicocele and Male Infertility Evidence in The Era of Assisted Reproductive Technology 2161 038X 3 E114Document3 pagesVaricocele and Male Infertility Evidence in The Era of Assisted Reproductive Technology 2161 038X 3 E114quickdannyNo ratings yet
- J Urology 2007 06 842Document1 pageJ Urology 2007 06 842quickdannyNo ratings yet
- Reference Book: Stewart C.bushong: by Huzaifa Atique Sir Syed University of Engineering & TechnologyDocument20 pagesReference Book: Stewart C.bushong: by Huzaifa Atique Sir Syed University of Engineering & TechnologyquickdannyNo ratings yet
- Course Outline Psychology 2101 YA 2004-2005Document4 pagesCourse Outline Psychology 2101 YA 2004-2005quickdannyNo ratings yet
- Sample Acceptance LetterDocument1 pageSample Acceptance Letterquickdanny100% (1)
- Case Study 8: Problem-Based Learning in Radiographer Education: Testing The Water Before Taking The PlungeDocument16 pagesCase Study 8: Problem-Based Learning in Radiographer Education: Testing The Water Before Taking The PlungequickdannyNo ratings yet
- Cureus-Authors GuideDocument20 pagesCureus-Authors Guidequickdanny100% (1)
- Instruction: Answer Question One (40 Marks) and Any Other Two (60marks)Document4 pagesInstruction: Answer Question One (40 Marks) and Any Other Two (60marks)quickdannyNo ratings yet
- 25 - B - SC - , Home Sciene Syllabus (2017-18)Document28 pages25 - B - SC - , Home Sciene Syllabus (2017-18)quickdannyNo ratings yet
- 01-Syllabus 614 v1Document6 pages01-Syllabus 614 v1quickdannyNo ratings yet
- Prediction of Male Infertility by The World HealthDocument7 pagesPrediction of Male Infertility by The World HealthquickdannyNo ratings yet
- Liver Cirrhosis: Precipitating Factors: Predisposing FactorDocument22 pagesLiver Cirrhosis: Precipitating Factors: Predisposing FactorJorie RocoNo ratings yet
- Types Causes Signs and Symptomps Intellectual DisabilityDocument2 pagesTypes Causes Signs and Symptomps Intellectual DisabilityMae Ann Jean JustolNo ratings yet
- JOURNAL PSYCHIATRIC (B.ing)Document13 pagesJOURNAL PSYCHIATRIC (B.ing)Aprilia Fani PNo ratings yet
- Inductions - Pre Employment Health Declaration - v1.2Document5 pagesInductions - Pre Employment Health Declaration - v1.2SEBASTIAN PULIDO MOJICANo ratings yet
- A Client With Pneumonia: Nursing Care PlanDocument1 pageA Client With Pneumonia: Nursing Care PlanAnonymous cffwxNVzNo ratings yet
- ECG PPT CH 06 v3Document42 pagesECG PPT CH 06 v3cdiledu.itNo ratings yet
- A Finnish Language Blog - Medical Vocabulary in FinnishDocument4 pagesA Finnish Language Blog - Medical Vocabulary in FinnishMehadi BappyNo ratings yet
- GeriatricDocument3 pagesGeriatricJonas AcuarioNo ratings yet
- GRD121 The Blood S3 21-22Document71 pagesGRD121 The Blood S3 21-22ASHERNo ratings yet
- Exam Answers NCM 103 MidtermDocument2 pagesExam Answers NCM 103 Midtermۦۦ James100% (1)
- NCLEX Notes : Raynaud's Phenomenon - Cold Temperatures or Strong Emotions CauseDocument10 pagesNCLEX Notes : Raynaud's Phenomenon - Cold Temperatures or Strong Emotions CauseDesi Marian100% (12)
- Multiple MyelomaDocument20 pagesMultiple Myelomaasim badarNo ratings yet
- Anatomy and Physiology of The Endocrine SystemDocument41 pagesAnatomy and Physiology of The Endocrine SystemJessica Glitter100% (2)
- Homoeopathic Bedside Clinical Tips Farokh J Master.01192 - 2Document6 pagesHomoeopathic Bedside Clinical Tips Farokh J Master.01192 - 2rbilashchandraNo ratings yet
- Nursing Care of Patients Having SurgeryDocument16 pagesNursing Care of Patients Having Surgeryshellacayetano2No ratings yet
- Antibiotic Cross-Sensitivity ChartDocument1 pageAntibiotic Cross-Sensitivity ChartChing JuNo ratings yet
- Orthopedic NursingDocument21 pagesOrthopedic NursingCris Constantino San JuanNo ratings yet
- 1-Definition Epidemiology and Classification of Diabetes in Children and Adolescents PDFDocument14 pages1-Definition Epidemiology and Classification of Diabetes in Children and Adolescents PDFFrancys Sierra FariasNo ratings yet
- A Study To Determine The Prevalence of Different Types of Anemia and Assessing Its Prescription Patterns in A Teritary Care HospitalDocument16 pagesA Study To Determine The Prevalence of Different Types of Anemia and Assessing Its Prescription Patterns in A Teritary Care HospitalInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Hypoalbuminemia in CombustionDocument20 pagesHypoalbuminemia in CombustionuchixconsiNo ratings yet
- Approach To Diabetes Mellitus in YoungDocument41 pagesApproach To Diabetes Mellitus in YoungLalrin ChhanaNo ratings yet
- 8η έκδοση του 'Ατλαντα για το Διαβήτη του IDFDocument150 pages8η έκδοση του 'Ατλαντα για το Διαβήτη του IDFANDREASNo ratings yet
- 2.2 Anus, Rectum, and ProstateDocument7 pages2.2 Anus, Rectum, and ProstateMary Mirasol Manayon100% (1)
- ASTHMA & COPD (Emphysema, CB) (CHAP 20)Document10 pagesASTHMA & COPD (Emphysema, CB) (CHAP 20)Abegail QuintoNo ratings yet
- Morning Report June, 04 2018: Dr. Dr. Herlina Dimiati, Sp. A (K) ResidentDocument33 pagesMorning Report June, 04 2018: Dr. Dr. Herlina Dimiati, Sp. A (K) ResidentmuslimNo ratings yet
- Cutaneous Larva Migrans: BackgroundDocument11 pagesCutaneous Larva Migrans: BackgroundNur AzizaNo ratings yet