Diabetes Mellitus in Pregnancy: November 2015
Diabetes Mellitus in Pregnancy: November 2015
Uploaded by
eka putri nur azizahCopyright:
Available Formats
Diabetes Mellitus in Pregnancy: November 2015
Diabetes Mellitus in Pregnancy: November 2015
Uploaded by
eka putri nur azizahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Diabetes Mellitus in Pregnancy: November 2015
Diabetes Mellitus in Pregnancy: November 2015
Uploaded by
eka putri nur azizahCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/283495236
Diabetes mellitus in pregnancy
Article · November 2015
DOI: 10.4038/sljog.v37i2.7745
CITATION READS
1 3,827
2 authors:
Carmeline Motha Tiran Dias
University of Kelaniya University of Kelaniya
34 PUBLICATIONS 31 CITATIONS 70 PUBLICATIONS 125 CITATIONS
SEE PROFILE SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Fetal growth and postpartum contraception View project
Fetal CPR as a marker of failure to reach growth potential View project
All content following this page was uploaded by Carmeline Motha on 05 November 2015.
The user has requested enhancement of the downloaded file.
www.slcog.lk/sljog Leading Article
Diabetes mellitus in pregnancy
Motha MBC Dias TD
INTRODUCTION
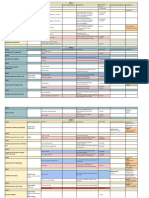
Diabetes mellitus in pregnancy Table 1 – GDM diagnostic threshold values from various organizations
could either be pregestational (pre-
existing ) or gestational. Gestational Plasma glucose concentration (mg/dl)
diabetes mellitus (GDM) is the most Organization OGTT Fasting 1 hour 2 hour 3 hour
common cause of diabetes during
glucose load
pregnancy, accounting for up to
90 % of pregnancies complicated ADA* 100g 95 180 155 140
by diabetes.1 Gestational diabetes ACOG* 100g 105 190 165 145
mellitus is defined as “any degree
NCE8 75g 100.8 140
of glucose intolerance with onset or
first recognition during pregnancy. 2 IADPSG8 75g 92 189 153
Marked variation in GDM prevalence DIPSI8
75g 140
among different racial/ethnic groups
has been documented, with higher *Diagnosis of GDM made if two or more glucose values equal to or exceeding the
prevalence among Native-American, threshold values. §Diagnosis of GDM if one or more glucose values equal to or exceeding
Asian, African-American, and the threshold values. OGTT: Oral Glucose Tolerance Test, ADA: American Diabetes
Hispanic populations than among Association, ACOG: American Council of Obstetricians and Gynecologists, NICE :
non-Hispanic whites. The prevalence National institute of clinical excellence, IADPSG: International Association of Diabetes
of gestational diabetes mellitus and Pregnancy Groups DIPSI: Diabetes in pregnancy study group India
is increasing reflecting the global
epidemic of obesity.3 In Sri Lanka, assessment for nephropathy by HAPO (The Hyperglycemia and
the prevalence of GDM was shown to estimating glomerular filtration rate Adverse Pregnancy Outcome) study
be 5.5% in a study carried out in Sri (eGFR) and urinary protein excretion which was a landmark multinational
Jayawardena general hospital while should be done prior to conception. study whose objective was to clarify
in another study done at the North The medications should be reviewed risks of adverse outcomes associated
Colombo teaching hospital, Ragama and modified to avoid teratogenic with degrees of maternal glucose
the prevalence of GDM was shown effects in the event of a pregnancy (eg: intolerance less severe than overt
to be 5.7% with the prevalence of angiotensin inhibitors/ angiotensin diabetes mellitus. 7 While the HAPO
both gestational and pregestational at receptor blockers/statins). Folic study demonstrated a positive
7.1%.4 5 acid 5 mg should be commenced linear relationship between screening
and continued throughout the first glucose values and adverse perinatal
trimester, while 75mg of aspirin outcomes it showed that blood
PRE-GESTATIONAL DIABETES should be commenced at 12 weeks of glucose values that were previously
MELLITUS gestation and continued until birth of considered ‘normal’ were associated
Preconception care forms the the baby. with adverse perinatal outcomes and
cornerstone of a successful pregnancy that the relationship of maternal
outcome in women with diabetes glucose to outcomes is a continuum.
SCREENING FOR GESTATIONAL The cut offs for gestational diabetes
preceding pregnancy. The aim of DIABETES MELLITUS
glycaemic management at this mellitus was based on the level of
stage is to attain a HbA1c <6.1%, There exists various guidelines for maternal blood glucose above which
without troublesome hypoglycaemic diagnosing GDM (Table 1). Urine key adverse outcomes (birth weight, C
symptoms. Screening for retinopathy glucose testing, fasting plasma glucose peptide levels and percent fetal body
by an ophthalmologist and and postprandial plasma glucose have fat >90th percentile) achieved an odds
been shown to have low sensitivity as ratio of 1.75 compared to mothers
screening tests for GDM and therefore with average glucose levels. The
Department of Obstetrics and Gynaecology, they are not recommended as recently published NICE guidelines
faculty of Medicine, University of Kelaniya, screening tests for gestational diabetes have lowered the cut off value for
Sri Lanka FBS to 100.8mg/dl, from the previous
mellitus6.
126mg/dl.8 (Table 1 ) The DIPSI
In March 2010, the International
Correspondence: Dr Motha MBC, recommends a glucose challenge test
Association of Diabetes and Pregnancy
with 75g of glucose taken any time
Senior Lecturer, Department of Obstetrics and Study Group (IADPSG) issued a
of the day (no need for fast) with an
Gynaecology, faculty of Medicine, University of consensus guidelines to potentially
Kelaniya, Sri Lanka. abnormal 2 hour post glucose blood
attain a single approach for GDM
sugar level considered significant.9
Email: cmotha6@gmail.com diagnosis based on the results of the
June 2015 Sri Lanka Journal of Obstetrics and Gynaecology 1
Leading Article www.slcog.lk/sljog
Universal screening for GDM is with pregestational diabetes mellitus Compared to diet alone, exercise
practiced in Sri Lanka with the 75g than in women with GDM.11 with dietary modifications has been
OGTT performed at 24-28 weeks found to lead to improved glycaemic
of pregnancy while screening for MANAGEMENT OF DIABETES control. 16 The proposed mechanism
pregestational diabetes is advocated MELLITUS IN PREGNANCY for such an improvement in glycaemic
at the booking visit in women not Benefits of treating gestational diabetes control is heightened sensitivity
known to have preexisting diabetes. mellitus has been demonstrated. The of peripheral tissues to insulin.
Australian Carbohydrate Intolerance Unfortunately, researchers have not
Study in Pregnant Women (ACHOIS), been able to suggest an evidence
PATHOPHYSIOLOGY OF GDM based intervention with guidelines
found reduced perinatal morbidity
Normal pregnancy is associated and mortality when standard for frequency, intensity, time and type
with a number of changes in glucose contemporary treatment of gestational of physical activity (FITT principle
metabolism. Data from the gold diabetes mellitus was compared for exercise prescription) that would
standard of assessment of insulin with no intervention, while more achieve good glycaemic control in
action, the euglycaemic glucose clamp recently the maternal fetal medicine women with GDM. Based on the
demonstrates that insulin action network (MFMU) study confirmed available evidence on the benefits of
reduces as pregnancy progresses due that treatment of GDM is beneficial exercise in managing GDM, ADA
to the insulin resistance created by in reducing macrosomia and large for recommends moderate exercise
certain hormones. Human placental gestational age babies. 12 13 programs for women without medical
lactogen and placental production of or obstetrical complications.17
tumour necrosis alpha (TNF-alpha) Dietary intake is fundamental to
optimal pregnancy outcomes because Pharmacological intervention in
appear to play a key role in the the management of GDM is usually
development of insulin resistance. nutritional quality and quantity
have an important impact on the employed when the woman fails
Pregnancy as an insulin resistant to meet established goals with
state may reveal even the smallest overall growth and development of
the fetus. Medical nutrition therapy conventional therapy of diet and
pre existing defects in insulin exercise. It is also indicated when
secretion or insulin sensitivity and as (MNT) is the cornerstone of managing
gestational diabetes. MNT has been elevated fasting glucose levels occur
a consequence, relative β-cell failure. while on conventional therapy,
The pathophysiological changes of defined as a ‘carbohydrate controlled
meal plan that promotes adequate because dietary modification alone
GDM are similar to those observed in has limited effect on fasting levels.
type 2 diabetes mellitus, which is also nutrition with appropriate weight
gain, normoglycemia, and the absence NICE recommends immediate
characterized by peripheral insulin treatment with insulin, with or
resistance accompanied by an insulin of ketosis.’ According to the ADA
recommendations, carbohydrate without metformin, as well as MNT, to
secretory defect. At the same time women with gestational diabetes who
there are changes in fasting glucose intake should be approximately 40 %
of total calorie intake and should be have a fasting plasma glucose level of
likely reflecting an increased uptake 126mg/dl or above at diagnosis while
of glucose by the fetoplacental unit, selected from foods with low glycaemic
index values.14 In pregnant women of in those with a FBS between 100.8-
with average fasting capillary glucose 126 mg/dl at diagnosis, addition of
readings low as 56mg/dl, found in normal body weight (BMI between
18–22.9 kg/m2), the recommendation pharmacological agents to MNT is
healthy, lean, normal glucose tolerant advocated when FBS remains above
women in the third trimester of is to consume 30–32 kcal/kg body
weight, especially during the second 126mg/dl following a two week trial
pregnancy.10 with MNT alone. 8
half of pregnancy.15 All women should
receive nutritional advice, preferably Prandial insulin and basal insulins are
ADVERSE EFFECTS OF DIABETES from an appropriately skilled the two main regimens used during
MELLITUS ON PREGNANCY dietitian. Advice on individualized pregnancy. Studies have shown that
plan for weight gain and caloric needs short acting insulin analogues (lispro
The adverse consequences of and determining protein, fat, and and aspart) are more effective than
gestational diabetes mellitus has been micronutrient needs should also be regular human insulin in achieving
known for some time but was clearly provided. target glucose values and minimizing
delineated by the HAPO study. the risk of macrosomia.18 19 Because
Macrosomia, neonatal hypoglycaemia, It is also imperative to note that only
20% of subjects in the ACHOIS trial the insulin analogues have shorter
caesarean section, shoulder dystocia, durations of action and more rapid
preeclampsia, preterm delivery, and 8% of Maternal fetal Medicine
Units Network subjects required onsets of action than regular insulin,
hyperbilirubinuria and admission to they are associated with improved
the neonatal intensive care unit was insulin, implying that lifestyle
modification and dietary intervention postprandial glycaemic control and
shown to be associated with maternal less postprandial hypoglycaemia.
hyperglycaemia. will be effective in 80–90% of women
with GDM. Due to limited data on the use of
Major maternal morbidity and basal analogues in pregnancy, NICE
mortality is more common in women recommends neutral protamine
2 Sri Lanka Journal of Obstetrics and Gynaecology June 2015
www.slcog.lk/sljog Leading Article
hagedorn (NPH) as the first choice had higher BMI in early pregnancy may be at risk of growth restriction
for long acting insulin during and higher baseline glucose levels.26 due to excessively tight maternal
pregnancy.20 The type of regimen Daily self monitoring of blood glucose control .31 A correlation has
and number of injections per day are glucose (fasting, premeal, postmeal been reported between ultrasound
determined based on the individual’s and bedtime at night), appears to be (USS) fetal abdominal circumference
needs and lifestyle. A basal bolus superior to intermittent monitoring of (AC) (AC>75th percentile) and high
insulin regimen (three bolus doses of plasma glucose as the hypoglycaemic amniotic fluid insulin levels in a
short acting insulin just prior to meals regimen could be tailored accordingly. recent study 30. There have been
with NPH insulin at night) or a split Consensus was reached at the fourth four randomized controlled studies
mixed dosage regimen (combination International workshop conference looking at the use of USS fetal AC as a
of short acting and intermediate acting on GDM on target capillary glucose guide to adjust the blood sugar levels.
insulin- Eg: Mixtard insulin twice values concentrations. Blood sugar
32 33 34 35
. Bonomo et al randomised 229
daily ) is used in pregnancy, though <95 mg/dl in the fasting state, <140 women to conventional treatment
the former regimen achieves better mg/dl at 1 hour, and <120 mg/dl 2 of GDM (glucose targets <90 mg/dl
glycaemic control.21 Pump therapy hours after starting the meal should (5.0 mmol/l) fasting and <120 mg/dl
(Continuous subcutaneous insulin be the treatment targets.27 In women (6.7 mmol/l) 2-hour post-prandial),
infusion- CSII) more closely mimics on insulin or glibenclamide, the or modified treatment targets based
physiological insulin secretion with blood sugar should not be allowed to on abdominal circumference on
evidence of less severe hypoglycaemia. drop below 72mg/dl.8 Urine glucose fetal ultrasound done two weekly as
CSII should be considered when monitoring is not useful though below. 35
adequate blood glucose control is not urine ketone monitoring can be • AC≥ 75th percentile: fasting< 80
obtained by multiple daily injections used in patients who are restricting mg/dl(4.4 mmol/l) and post-
of insulin without significant calories to detect insufficient caloric or prandial <100 mg/dl (5.5 mmol/l)
disabling hypoglycaemia. However, carbohydrate intake.28
benefits of CSII on glycaemic control • AC< 75th percentile: fasting< 100
during pregnancy have not been Although there is consensus about mg/dl(5.5 mmol/l) and post-
realized, with a Cochrane review postprandial glucose levels being prandial <140 mg/dl (7.8 mmol/l)
suggesting a potential increase in more important than preprandial They have reported a significant
infant birth weight associated with levels since the former correlates reduction in the percentage of LGA
CSII.22 The potential of a closed loop better with adverse neonatal events infants (7.9 vs. 17.9%), SGA infants
therapy, linking real time continuous such as fetal malformations, (6.0 vs. 9.0%), and macrosomia (3.3 vs.
glucose monitoring with insulin dose macrosomia, hypoglycaemia, and 11%) with this modified treatment. 35
adjustments to improve management shoulder dystocia, it has been debated USS fetal biometry may allow more
of diabetes during pregnancy is under as to whether glucose should be pragmatic treatment targets in some
investigation. measured one or two hours after a low risk patients, whilst tighter control
meal.29 Continuous blood glucose may be suggested for other patients
Metformin and glibenclanide are the monitoring using the continuous
two oral hypoglycaemics that can be at high risk of adverse perinatal
glucose monitoring system has outcomes.
used in pregnancy. Metformin can recently shown that glucose peaks
be used as an alternative or adjunct occur about 70 ± 13 minutes after a Fetal ultrasound assessment is
to insulin therapy. Metformin was meal in non diabetic pregnant women frequently used to estimate the fetal
shown to be similar to insulin with and after about 90 minutes in diabetic weight and wellbeing and to assist
regard to glycaemic control and women. safe prolongation of pregnancy and
neonatal outcome.23 Glibenclamide is time the date of delivery. However,
comparable to insulin in terms of birth Women with diabetes should have there is no uniform policy of frequency
outcome and glycaemic control and is contact with the joint diabetes and of USS examinations. Therefore, the
a suitable alternative to metformin.24 antenatal clinic for assessment of frequency of USS examinations should
NICE recommends glibenclamide for blood glucose control every 1–2 weeks be based on clinical indications. There
women with gestational diabetes in throughout pregnancy. is a paucity of high level evidence
whom blood glucose targets are not on the optimum gestational age for
achieved with metformin but who delivery in gestational diabetes.
TREATMENT ADJUSTMENT
decline insulin therapy or who cannot Different management strategies have
tolerate metformin. There is limited ACCORDING TO THE FETAL been adopted for pregestational or
evidence with regard to which oral BIOMETRIC PARAMETERS pre-existing diabetes. Rasmussen et al
hypoglycaemic should be selected. AND ANTENATAL FETAL noted that deaths in normally formed
Failure of glibenclamide was shown to infants occurred when there was
be higher in women with higher initial
SURVEILLANCE
clinical evidence of fetal macrosomia,
fasting glucose values above 115mg/ Despite optimum glycemic control polyhydramnios or poor metabolic
dl.25 Similarly for metformin, women there is a potential increase in the risk control. Consequently, uncomplicated
who required supplemental insulin of fetal macrosomia in women with GDM pregnancies could go up to 40
GDM.30 In contrast, some fetuses
June 2015 Sri Lanka Journal of Obstetrics and Gynaecology 3
Leading Article www.slcog.lk/sljog
Probability of shoulder dystocia by birth weight in diabetic and non-diabetic pregnancies37
Birth weight (g) Diabetic pregnancy Non-diabetic pregnancy
<4000 0.022 0.007
4000-4499 0.139 0.067
≥4500 0.525 0.145
completed weeks of gestation.36 active phase. Maternal hyperglycaemia hourly and an insulin infusion regimen
The potential risk of shoulder dystocia during labour increases the risk of commenced when two consecutive
is one of the major concerns in vaginal fetal hyperinsulinaemia and thus blood sugar readings are above
delivery in women with gestational hypoglycaemia and fetal acidaemia. 126 mg/dl, with insulin adjusted
diabetes. Although increasing fetal Therefore maternal blood sugar according to an insulin infusion scale.
weight is positively associated with surveillance should be continued Intravenous dextrose and insulin
the risk of shoulder dystocia, as many during labour with hourly monitoring infusion should be considered for
cases occur in instances where birth of blood sugar, in women who have women with type 1 diabetes from
weight is less than 4000 g. Rouse et al been on insulin or oral hypoglycaemics the onset of established labour. The
reported the probability of shoulder during pregnancy. infusion scale should consider both the
dystocia by birth weight in diabetic Women should have their normal diet insulin requirement in late pregnancy
and non-diabetic pregnancies37. and continue their insulin regimen and the blood glucose level. (Table 2)
Royal College of Obstetricians and until active labour begins. Women A syringe pump is set up with 50
Gynaecologists has recommended to on long acting basal insulin should U of soluble insulin in 50 ml of
offer an elective Cesarean delivery in continue this, while short acting and normal saline, while a 5% dextrose
case of estimated fetal weight >4500g intermediate acting insulin should solution containing 20 mmol/L of
in diabetic mothers. be discontinued at the time of active potassium chloride is commenced at
labour. The aim is to maintain blood 100ml per hour. If two consecutive
glucose between 70 and 126 mg/dl blood sugar readings are above 162
DIABETIC KETOACIDOSIS during labor irrespective of whether mg/dl, the infusion rate should
the women has type 1 or type 2 be shifted one column to the right
In pregnancy, diabetic ketoacidosis
diabetes or GDM.8 A maternal blood and if two consecutive readings are
(DKA) can occur at a relatively
glucose value of more than 180 mg/ below 72 mg/dl , the infusion rate
lower blood glucose level due to
dl has been conclusively proven to be should be shifted one column to the
physiological changes that accompany
associated with high risk of neonatal left. Following delivery the infusion
pregnancy. Emesis and the tendency
hypoglycemia. 38 The protocols for should be reduced to the lowest scale
for early lipolysis following relatively
use of insulin during pregnancy are and blood sugar monitored hourly
short episodes of fasting (‘accelerated
mostly based on studies in type 1 until the woman resumes her normal
starvation of pregnancy’), result in
diabetes mellitus patients. meals.
ketonuria being found in a significant
number of healthy pregnant During labour, normoglycemia is The infusion regimen can be adopted
women. Therefore, for a diagnosis mostly achieved with rapid acting for women undergoing a caesarean
of DKA in pregnancy, ketonaemia insulin when indicated, so as to section too, which should be
or academia (pH < 7.3 or serum prevent hypoglycemia in the neonate. performed in the morning hours.
bicarbonate < 15mmol/L ) should be Blood glucose should be monitored
demonstrated. DKA is associated with Table 2- Insulin infusion regimen for women during active labour 39
poor uteroplacental blood flow and
fetal acidosis, which is reflected on Current total Up to 40 41-60 61-90 > 91 units/day
cardiotocography. As fetal acidosis daliy insulin units/day units/day units/day
reverses with satisfactory treatment dose
of DKA, emergency delivery should Capillary Infusion rate Infusion rate Infusion rate Infusion rate
not be planned in the presence of an Glucose
abnormal CTG in this setting. DKA (units / hr) (units / hr) (units / hr) (units / hr)
(mg/Dl)
is a medical emergency and should
0-54 0 0 0 0
be managed in intensive care setting.
The management is similar to that of a 55-125 1.0 1.5 2.0 2.0
non-pregnant adult with DKA. 126-160 1.5 2.0 3.0 4.0
INTRAPARTUM MANAGEMENT 161-195 2.0 3.0 4.0 5.0
The insulin requirement during the 196-270 3.0 4.0 5.0 6.0
latent phase remains at a stable level >270 Exclude diabetic Exclude diabetic Exclude diabetic Exclude diabetic
though it may increase during the ketoacidosis ketoacidosis ketoacidosis ketoacidosis
4 Sri Lanka Journal of Obstetrics and Gynaecology June 2015
www.slcog.lk/sljog Leading Article
POST PARTUM MANAGEMENT above 90th centile commonly REFERANCES
complicates diabetic pregnancies. This
Immediately following delivery, 1. Report of the expert committee on the
is a result of fetal hyperinsulinaemia
insulin resistance falls dramatically. In diagnosis and classification of diabetes
and is associated with increased risk
addition to this, blood glucose falls as mellitus. Diabetes Care. 2003;26 Suppl
of shoulder dystocia, obstructed
glucose passes into breast milk. 1:S5–20.
labour, instrumental delivery, birth
Breast feeding should be commenced 2. Metzger BE. Proceedings of the third
injuries and caesarean section.
immediately following delivery in international workshop-conference on
Although less common than gestational diabetes mellitus. Diabetes.
order to reduce the risk of neonatal
macrosomia, fetal growth restriction 1991;40(Suppl 2):1–201.
hypoglycaemia. Women with type
could occur as a consequence of 3. Dabelea D, Snell-Bergeon JK, Hartsfield
1 diabetes will need a reduction
placental insufficiency especially in CL et al Increasing Prevalence of
of their insulin requirements by
women with pregestational diabetes Gestational Diabetes Mellitus (GDM)
about 30% while women with type 2
with microvascular complications. over time and by Birth Cohort Kaiser
diabetes could continue metformin
or glibenclamide with advise on Respiratory complications that are Permanente of Colorado GDM Screening
frequent snacks to reduce the risk commonly seen among neonates of Program. Diabetes Care March 2005 vol.
of hypoglycaemia. Women with diabetic women are due to inadequate 28 no. 3 579-584.
GDM should have their antenatal pulmonary fluid absorption caused 4. Siribaddana SH1, Deshabandu R,
hypoglycaemic regimen withheld by lack of labour induced stress Rajapakse D, Silva K, Fernando DJ.
while blood glucose should be hormonal surge, as elective deliveries The prevalence of gestational diabetes
monitored premeal and postmeal are performed to reduce the risk of in a Sri Lankan antenatal clinic. Ceylon
with advise on frequent snacks. late intrauterine death. Medical journal 1998;43(2): 88-91.
5. Dias, T, Palihawadana, T, Motha, C,
At six weeks postpartum the woman Other adverse fetal/neonatal Thulya SD Diabetes mellitus in pregnancy
should be reviewed with blood sugar effects include intrauterine – a Sri Lankan experience Abstract
level. The NICE recommends a FBS death, polycythaemia, jaundice, book - BJOG An International Journal of
at six weeks while some studies hypocalcaemia, hypoglycaemia and Obstetrics and Gynaecology 2015.
have shown that this would miss a hypertrophic cardiomyopathy. 6. Kousta E, Lawrence NJ, Penny A, Millauer
significant number of women with BA, Robinson S, Dornhorst A et al.
diabetes, compared to the oral glucose LONG TERM EFFECTS OF GDM Implications of new diagnostic criteria for
tolerance test.40 Advise on continuing abnormal glucose homeostasis in women
breastfeeding should be reiterated at The largest public health impact of
with previous gestational diabetes.
this point as the benefits of exclusive GDM is it’s role on future diabetes in
Diabetes Care. 1999; 22(6):933-7.
breastfeeding for at least 3 to 4 months the mother and obesity and diabetes
7. The HAPO Study Cooperative Research
has been demonstrated by a reduction in the offspring. It was found that 17–
Group. Hyperglycemia and Adverse
in childhood obesity compared to 63% of women diagnosed with GDM
Pregnancy Outcomes New England
women with GDM who did not breast will develop type 2 diabetes mellitus
journal of medicine 2008;358 (19):1991-
feed exclusively for this period.41 within 5 to16 years after delivery.42
2008.
The cumulative incidence of type 2
8. Diabetes in pregnancy: management
diabetes is highest in the first five years
of diabetes and its complications from
INFANT OF A DIABETIC MOTHER after pregnancy and then it decreases,
preconception to the postnatal period
Congenital anomalies are a reaching a plateau at ten years
NICE guideline Published: 25 February
complications of pregestational postpartum. Though there have been
studies showing a beneficial result of 2015.
diabetes mellitus as the fetuses are 9. Anjalakshi C, Balaji V, Balaji MS, et al.
exposed to hyperglycaemia during metformin and thiazolidinediones in
preventing diabetes mellitus, further A single test procedure to diagnose
the critical period of organogenesis. gestational diabetes mellitus. Acta
A linear relationship between HbA1c studies are needed to study this area
more extensively.43 44 An annual Diabetol. 2009;46(1):51-4.
and malformation rates have been 10. Parretti E, Mecacci F, Papini M et al
reported, with the optimal HbA1c HbA1c test should be performed in
women who have a negative postnatal Third trimester maternal glucose levels
set at below 6.1% with avoidance from diurnal profiles in non diabetic
of troublesome hypoglycaemic test for diabetes at 6 weeks .8
pregnancies: correlation with sonographic
symptoms. Unfortumately most Though life style modifications in parameters of fetal growth diabetes carer
anomalies occur before pregnancy the form of nutritional adjustments 2001;24:1319-23.
is recognized, highlighting the and regular exercise have shown 11. Shand A W , Bell J C, McElduff A,
need for optimal glycemic control some promising results in preventing Morris J et al Outcomes of pregnancies
at the preconception stage. The gestational diabetes mellitus, recently in women with pre-gestational diabetes
anomalies predominantly affect the published systematic reviews and mellitus and gestational diabetes mellitus;
cardiac, skeletal, central nervous and meta analyses do not show evidence a population-based study in New South
gastrointestinal systems. of a lower risk of GDM with enhanced Wales, Australia, 1998–2002. Diabetic
Macrosomia, defined as a birthweight physical activity in pregnancy.45 46 medicine 2008;25(6): 708-715.
June 2015 Sri Lanka Journal of Obstetrics and Gynaecology 5
Leading Article www.slcog.lk/sljog
12. Crowther CA, Hiller JE, Moss JR Effect of 25. Moore TR Glyburide for the treatment of 36. Rasmussen MJ. Firth R, Foley M. et
treatment of gestational diabetes mellitus gestational diabetes. A critical appraisal al. The timing of delivery in diabetic
on pregnancy outcomes New England Diabetes care 2007; 30 (supp2)-s209-13. pregnancy a 10 year review. Aust N Z J
journal of Medicine 2005; 352: 2477-86. 26. Rowan JA, Hague WM, Gao W et al Obstet Gynecol1992;32:313-7.
13. Kim C, Neston K, Knopp R. Gestational Metformin versus insulin for the treatment 37. Rouse DJ, Owen J Prophylactic
diabetes and the incidence of type 2 of gestational diabetes New England caesarean delivery for foetal macrosomia
diabetes: a systematic review. Diabetes journal of medicine 2008;358:2003-15. diagnosed by means of ultrasonography-
Care. 2002;25:1862–1868. 27. Metzger BE, Coustan DR. Summary A Faustian bargain? Am j Obstet Gynecol
14. Clapp JF. Effect of dietary carbohydrate and recommendations of the Fourth 1999;131:332-8.
on the glucose and insulin response International Workshop-Conference 38. Carron Brown S, Kyne-Grzebalski
to mixed caloric intake and exercise in on Gestational Diabetes Mellitus. The D, Mwangi B, Taylor R. Effect of
both nonpregnant and pregnant women. Organizing Committee. Diabetes Care. management policy upon 120 Type 1
Diabetes Care. 1998; 21 Suppl 2:B107- 1998; 21 Suppl 2:B161-7. diabetic pregnancies: Policy decisions in
12. 28. Gestational diabetes mellitus. practice. Diabet Med. 1999;16:573–8.
15. Jovanovic-Peterson L, Peterson CM. Diabetes Care. 2003; 26(supplement 39. Lindsay RS Diabetes in pregnancy –
Nutritional management of the obese 1):S103-S105. Diabetes management during labour
gestational diabetic pregnant woman. J 29. Jovanovic-Peterson L, Peterson CM, Oxford diabetes library 2012.
Am Coll Nutr. 1992; 11(3):246-50. Reed GF, Metzger BE, Mills JL, Knopp 40. Ferrara A, Peng T,Kim C Trends in
16. Jovanovic-Peterson L, Durak EP, RH et al. Maternal postprandial glucose postpartum diabetes screening and
Peterson CM. Randomized trial of levels and infant birth weight: the subsequent diabetes and impaired fasting
diet versus diet plus cardiovascular Diabetes in Early Pregnancy Study. The glucose among women with histories
conditioning on glucose levels in National Institute of Child Health and of gestational dibetes mellitus:A report
gestational diabetes. Am J Obstet Human Development--Diabetes in Early from the translating research into action
Gynecol. 1989; 161(2):415-9. Pregnancy Study. Am J Obstet Gynecol. for diabetes(TRIAD) study Diabetes care
17. Gestational diabetes mellitus. 1991; 164(1 Pt 1):103-11.
32:269-74.
Diabetes Care. 2003; 26(supplement 30. Kjos SL, Schaefer-Graf UM. Modified
41. Schaeffer-Graf UM, Hartmann
1):S103-S105. therapy for gestational diabetes using
R,Pawliczak J et al Association of breast
18. Lapolla A, Dalfrà MG, Fedele D. Insulin high risk and low risk fetal abdominal
feeding and early childhood overweight
therapy in pregnancy complicated by circumference growth to select strict
in children from mothers with gestational
diabetes: are insulin analogs a new versus relaxed maternal glycaemic
diabetes mellitus Diabetes care
tool? Diabetes Metab Res Rev. 2005; targets. Diabetes care 2007;30:5200-5.
2006;29:1105-7.
21(3):241-52. 31. Langer O, Levy J,Brustman L, et
42. Bellamy L , Casas JP, Hingorani AD et
19. Pettitt DJ, Ospina P, Kolaczynski JW, al. Glycaemic control in gestational
al Type 11 diabetes after gestational
Jovanovic L. Comparison of an insulin diabetes mellitus- how tight is tight
analog, insulin aspart, and regular human enough- small for gestational age versus diabetes mellitus a systematic review and
insulin with no insulin in gestational large for gestational age? Am J Obstet meta analysis Lancet 2009 373(9677)
diabetes mellitus. Diabetes Care. 2003; Gynecol1989;161:646-53. 1773-1779.
26(1):183-6. 32. Buchanan TA,Kjos SL, Montoro MN,et 43. Diabetes prevention program research
20. Metzger BE, Buchanan TA, Coustan DR, al. Use of foetal ultrasound to select group. Reduction in the incidence of
De Leiva A, Dunger DB, Hadden DR et al. metabolic therapy for pregnencies type 2 diabetes with lifestyle intervention
Summary and recommendations of the complicated by mild gestational diabetes. or metformin.New England journal of
Fifth International Workshop-Conference Diabetes care 1994;17:275-83. medicine 2002; 346:393-403.
on Gestational Diabetes Mellitus. 33. Kjos SL, Schaefar-Graf U, Sardesi 44. Xiang AH,Peter RK,Kjos SL, et al Effect
Diabetes Care. 2007; 30(2):S251-60. S, et al. A randomized controlled trial of pioglitazone on pancreatic beta cell
21. Nachum Z, et al. Twice daily versus using glycaemic pluss foetal ultrasound function and diabetes risk in Hispanic
four times daily insulin dose regimens parameters to determine insulin women with prior gestational diabetes
for diabetes in pregnancy: randomised therapy in gestational diabetes with 2006;55:517-22.
controlled trial. BMJ1999;319:1223–7. fasting hyperglycaemia. Diabetes care 45. Han S, Middleton P, Crowther CA
22. Farrar D, Tuffnell DJ,West J Continuous 2002;24:1904-10. Exercise for pregnant women in
subcutaneous insulin infusion vs multiple 34. Schaefar-Graf U, Kjos SL, Fauzan OH, preventing gestational diabetes mellitus
daily injections of insulin for pregnant et al. A randomized trial evaluating Cochrane database sys rev 2012:
women with diabetes. Cochrane a predominantly foetal growth- CD009021.
database sys rev3:CD005542. basedstrategy to guide management 46. Oostdam M, Van Poppel MN, Wouters
23. Gui J, Liu Q, Feng L. Metformin vs of gestational diabetes in Caucasian MG et al Interventions for preventing
insulin in the management of gestational women. Diabetes Care 2004;27:297-302. gestational diabetes mellitus: a
diabetes: a meta-analysis. PLoS One. 35. Bonomo M, Cetin I, Pisoni MP. et al. systematic review and meta analysis.
2013; 8(5):e64585. Flexible treatment of gestational diabetes Journal of womens health (Larchmt)
24. Langer O, Conway DL,Berkus MD et al. modulated on ultrasound evaluation 2011;20(10): 1551-1563.
A comparison of Glyburide and insulin of intrauterine growth: a controlled
in women with gestational diabetes randomized clinical trial. Diabetes Metab
mellitus New England journal of Medicine 2004;30:237-44.
2000;361: 1339-48.
6 Sri Lanka Journal of Obstetrics and Gynaecology June 2015
View publication stats
You might also like
- Stealth Health Slow Cooker CookbookDocument112 pagesStealth Health Slow Cooker Cookbookbubbalisous999100% (2)
- 190 - Gestational Diabetes Mellitus AgogDocument16 pages190 - Gestational Diabetes Mellitus Agogjorge vergara100% (2)
- Locus of ControlDocument5 pagesLocus of ControlArpit Kumar100% (1)
- Study of HypertensionDocument44 pagesStudy of HypertensionMathew PiNo ratings yet
- Slope StabilityDocument6 pagesSlope StabilityEsquerion PrietoNo ratings yet
- Cde Small Washing PlantDocument10 pagesCde Small Washing PlantRiosi G SVn100% (2)
- OBGYN0521 010-015 OB-diabetesDocument6 pagesOBGYN0521 010-015 OB-diabetesjuan carlos pradaNo ratings yet
- Local Versus International Criteria in Predicting Gestational Diabetes Mellitus Related Pregnancy OutcomesDocument10 pagesLocal Versus International Criteria in Predicting Gestational Diabetes Mellitus Related Pregnancy OutcomesCj CCNo ratings yet
- Assignment On Course During CCGDM.Document6 pagesAssignment On Course During CCGDM.Biman MondalNo ratings yet
- Who PDFDocument23 pagesWho PDFMayra PereiraNo ratings yet
- Jurnal Internasional 2 Diabetes GestasionalDocument8 pagesJurnal Internasional 2 Diabetes Gestasionalmuhammad nur husnullahNo ratings yet
- Definition, Detection, and DiagnosisDocument7 pagesDefinition, Detection, and Diagnosismeen91_daqtokpaqNo ratings yet
- STATEMENTS ADIPS GDM Management GuidelinesDocument10 pagesSTATEMENTS ADIPS GDM Management Guidelineskitten garciaNo ratings yet
- DIPSI GuidelinesDocument7 pagesDIPSI GuidelinesvinaypharmNo ratings yet
- GDMDocument3 pagesGDMErika RubionNo ratings yet
- GDM FOGSI Text Book FinalDocument29 pagesGDM FOGSI Text Book FinalKruthika Devaraja GowdaNo ratings yet
- Gestational Diabetes Mellitus: Risks and Management During and After PregnancyDocument11 pagesGestational Diabetes Mellitus: Risks and Management During and After PregnancyViki G PNo ratings yet
- Diabetes Gestacional Revision 2019Document15 pagesDiabetes Gestacional Revision 2019zaaaidaNo ratings yet
- What Are The Existing Diagnostic Criteria?Document6 pagesWhat Are The Existing Diagnostic Criteria?Utkarsh AbhilashNo ratings yet
- Gestational Diabetes Mellitus Acog CopDocument8 pagesGestational Diabetes Mellitus Acog CopAndrea Sandoval OteroNo ratings yet
- ACOG Practice Bulletin No137 PDFDocument11 pagesACOG Practice Bulletin No137 PDFRodrigo Pérez CuelloNo ratings yet
- 17 Diagnostic Strategies For Gestational Diabetes MellitusreviewDocument10 pages17 Diagnostic Strategies For Gestational Diabetes MellitusreviewdianaNo ratings yet
- The Elusive Diagnosis of Gestational Diabetes: Guest EditorialDocument4 pagesThe Elusive Diagnosis of Gestational Diabetes: Guest EditorialSarly FebrianaNo ratings yet
- Gestational Diabetes: Update in Diagnosis and ManagementDocument61 pagesGestational Diabetes: Update in Diagnosis and ManagementTriani Ismelia FirdayantiNo ratings yet
- Diabetes Acog 2017Document15 pagesDiabetes Acog 2017Holger Vicente Guerrero Guerrero100% (1)
- Jurnal ObgynDocument8 pagesJurnal ObgynayuNo ratings yet
- 2010 Update On Gestational DiabetesDocument13 pages2010 Update On Gestational DiabetesAde Gustina SiahaanNo ratings yet
- 10 1097aog 0000000000002159Document15 pages10 1097aog 0000000000002159Kathleen Cherrepano AguirreNo ratings yet
- ACOG Tech BullitinDocument20 pagesACOG Tech BullitinJosephNo ratings yet
- Recent Advances in Management of Gestational Diabetes and Pre-EclampsiaDocument36 pagesRecent Advances in Management of Gestational Diabetes and Pre-EclampsiaSyed Zahed AliNo ratings yet
- Thesis TopicDocument17 pagesThesis Topicreamer27100% (1)
- Diabetes GestacionalDocument8 pagesDiabetes GestacionalaguscollarettiNo ratings yet
- Gestational Diabetes MellitusDocument4 pagesGestational Diabetes MellitusMaykel de GuzmanNo ratings yet
- Gupta 2020Document2 pagesGupta 2020dr dakshataNo ratings yet
- Gestational Diabetes Mellitus (GDM) .TriceDocument47 pagesGestational Diabetes Mellitus (GDM) .TricejerrydanfordfxNo ratings yet
- Diagnosis and Treatment of Gestational Diabetes: Scientific Impact Paper No. 23Document6 pagesDiagnosis and Treatment of Gestational Diabetes: Scientific Impact Paper No. 23Ane DamayantiNo ratings yet
- Gestational Diabetes Mellitus, Diagnostic Approaches and Maternal Offspring ComplicationsDocument12 pagesGestational Diabetes Mellitus, Diagnostic Approaches and Maternal Offspring ComplicationsSaraid RuizNo ratings yet
- Gestational Diabetes 1Document12 pagesGestational Diabetes 1Kyla Isobel DalonosNo ratings yet
- Gestational Diabetes: Key PointsDocument5 pagesGestational Diabetes: Key PointsMayra PereiraNo ratings yet
- Management Of: Diabetes in PregnancyDocument8 pagesManagement Of: Diabetes in PregnancyNazmun NaharNo ratings yet
- DIABETES MELLITUS IN PREGNANCY - PPTX CUIXLEXDocument61 pagesDIABETES MELLITUS IN PREGNANCY - PPTX CUIXLEXh27nkhhtw4No ratings yet
- High Maternal Hba Is Associated With Overweight In Neonates: Dan Med Bul Ϧϫ/ϪDocument6 pagesHigh Maternal Hba Is Associated With Overweight In Neonates: Dan Med Bul Ϧϫ/ϪHerry SasukeNo ratings yet
- Literature Review of Gestational Diabetes MellitusDocument7 pagesLiterature Review of Gestational Diabetes Mellitusc5rc7ppr100% (1)
- Gestational Diabetes Mellitus: Welcome To The Diabetes E-Learning SuiteDocument26 pagesGestational Diabetes Mellitus: Welcome To The Diabetes E-Learning SuiteListon OtienoNo ratings yet
- Diabetes IN Pregnanc Y: Presenter: DR Leong Yuh Yang (MD Ukm) Supervisor: DR Noraza AzmeeraDocument45 pagesDiabetes IN Pregnanc Y: Presenter: DR Leong Yuh Yang (MD Ukm) Supervisor: DR Noraza AzmeeraKeserovic AdmirNo ratings yet
- Gestational Diabetes Screening in AustraliaDocument9 pagesGestational Diabetes Screening in AustraliaRaniMSinghNo ratings yet
- Diagnosis of Gestational DiabetesDocument7 pagesDiagnosis of Gestational DiabetesAl Hasyr SarminNo ratings yet
- Screening and DiagnosisDocument25 pagesScreening and DiagnosisM AbhiNo ratings yet
- Prenatal Diagnosis - 2020 - Murray - Short and Long Term Outcomes of Gestational Diabetes and Its Treatment On FetalDocument7 pagesPrenatal Diagnosis - 2020 - Murray - Short and Long Term Outcomes of Gestational Diabetes and Its Treatment On FetalVicente Fasce OlmosNo ratings yet
- Diagnosing Dysglycemia in Adolescents With Polycystic Ovary Syndrome 2014 Journal of Adolescent HealthDocument6 pagesDiagnosing Dysglycemia in Adolescents With Polycystic Ovary Syndrome 2014 Journal of Adolescent HealthfujimeisterNo ratings yet
- The Pathophysiology of Gestational Diabetes MellitusDocument35 pagesThe Pathophysiology of Gestational Diabetes MellituscalliemozartNo ratings yet
- Diabetes in Pregnancy ADA 2018Document7 pagesDiabetes in Pregnancy ADA 2018Reisa Maulidya TazamiNo ratings yet
- HHS Public Access: Gestational Diabetes MellitusDocument19 pagesHHS Public Access: Gestational Diabetes MellitusAnne MarieNo ratings yet
- Seminar 5 - DM in PregnancyDocument19 pagesSeminar 5 - DM in PregnancyHakimah K. SuhaimiNo ratings yet
- Guide Who Hyperglycaemia PregnancyDocument44 pagesGuide Who Hyperglycaemia PregnancyThinzar NweNo ratings yet
- Neoreviews 042022cmerev00036Document12 pagesNeoreviews 042022cmerev00036Agnimitra ChoudhuryNo ratings yet
- Gestational Diabetes Mellitus: Science in MedicineDocument7 pagesGestational Diabetes Mellitus: Science in MedicinerizqarrNo ratings yet
- LalalalaDocument3 pagesLalalalaEva Yuliana ChoandraNo ratings yet
- Flemish ConsensusDocument9 pagesFlemish ConsensusM AbhiNo ratings yet
- Gestational Diabetes MellitusDocument14 pagesGestational Diabetes MellitusCzarina PorciunculaNo ratings yet
- Virtual issue on diabetes in pregnancyDocument2 pagesVirtual issue on diabetes in pregnancyTudor MotasNo ratings yet
- Diabetes Mellitus & Pregnancy by D.a.mehtaDocument31 pagesDiabetes Mellitus & Pregnancy by D.a.mehtadr.d.a.mehta11No ratings yet
- Correlations Between Parameters of Glycaemic Variability and Foetal Growth Neonatal Hypoglycaemia and Hyperbilirubinemia in Women With Gestational diabetesPLoS ONEDocument14 pagesCorrelations Between Parameters of Glycaemic Variability and Foetal Growth Neonatal Hypoglycaemia and Hyperbilirubinemia in Women With Gestational diabetesPLoS ONEVicente Fasce OlmosNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 10: ObstetricsFrom EverandComplementary and Alternative Medical Lab Testing Part 10: ObstetricsNo ratings yet
- Prediabetes: A Fundamental Text: Pathophysiology, Complications, Management & ReversalFrom EverandPrediabetes: A Fundamental Text: Pathophysiology, Complications, Management & ReversalNo ratings yet
- Dandy Drinks Menu 2021Document10 pagesDandy Drinks Menu 2021MUHAMMAD DANIEL FITRI BIN CHE JARABAH MoeNo ratings yet
- Florence Gasoc - KingRichardDocument4 pagesFlorence Gasoc - KingRichardChristine HabañaNo ratings yet
- Physicians For Alberta Healthcare Mar30'2020Document11 pagesPhysicians For Alberta Healthcare Mar30'2020CityNewsTorontoNo ratings yet
- Natural Resources - Grade 5Document90 pagesNatural Resources - Grade 5rkumar_81No ratings yet
- Pearson Practice English Quick Start Guide For Students MyGrammarLabDocument11 pagesPearson Practice English Quick Start Guide For Students MyGrammarLabԱրմինե ՇեգունցNo ratings yet
- Introduction To Criminal Law (Lea1393) Tutorial Questions Instructions: Answer ALL QuestionsDocument1 pageIntroduction To Criminal Law (Lea1393) Tutorial Questions Instructions: Answer ALL QuestionsHAFIZAH SUHIDAN LEA170No ratings yet
- Periodic TableDocument1 pagePeriodic Tablekexin zhaoNo ratings yet
- Name: Gr. & Sec.: Date: Score: I. MULTIPLE CHOICE. Read and Analyze Each Statement Carefully Then Write The Letter of The Correct AnswerDocument3 pagesName: Gr. & Sec.: Date: Score: I. MULTIPLE CHOICE. Read and Analyze Each Statement Carefully Then Write The Letter of The Correct AnswerjamNo ratings yet
- Blood Sugar Desiase FixDocument10 pagesBlood Sugar Desiase FixHammNo ratings yet
- Fast Food ChainDocument12 pagesFast Food Chaingarg_09100% (1)
- Effect of Textile Industry On Health FinalDocument2 pagesEffect of Textile Industry On Health FinalSudhir Jain100% (1)
- Ruthenberg Farming Systems in The Tropics PDFDocument344 pagesRuthenberg Farming Systems in The Tropics PDFDhamma_Storehouse100% (1)
- Boiler Inspection PointsDocument33 pagesBoiler Inspection PointsHussien AlsadyNo ratings yet
- 2018 02 24berkshireletterDocument148 pages2018 02 24berkshireletterZerohedgeNo ratings yet
- Sefer ShedimDocument32 pagesSefer ShedimKNUP TFADNo ratings yet
- 2015 10 JunctionBoxes PDFDocument12 pages2015 10 JunctionBoxes PDFPradeeoNo ratings yet
- Steering Hydraulic AccumulatorDocument3 pagesSteering Hydraulic AccumulatorRafael RahealNo ratings yet
- Durinox Product CatalogDocument6 pagesDurinox Product CatalogGlen DalyNo ratings yet
- Characterization of Proteases of Bacillus Subtilis Strain 38 Isolated From Traditionally Fermented Soybean in Northern ThailandDocument5 pagesCharacterization of Proteases of Bacillus Subtilis Strain 38 Isolated From Traditionally Fermented Soybean in Northern ThailandSyed Ali Akbar BokhariNo ratings yet
- Development of Antistatic Finish in TextDocument6 pagesDevelopment of Antistatic Finish in TextANURAG JOSEPHNo ratings yet
- Algeria Flyer USA (English) New StyleDocument2 pagesAlgeria Flyer USA (English) New StylekrishimaNo ratings yet
- Q1 COT-LP - Health 7 (Health Services)Document5 pagesQ1 COT-LP - Health 7 (Health Services)violeta balinoNo ratings yet
- Walkthrough 0.65Document13 pagesWalkthrough 0.65furer4131No ratings yet
- 2019 Water Quality ReportDocument10 pages2019 Water Quality Reportjdm81No ratings yet
- Annexure Vii Cost Norms and Pattern of Assistance Udner Midh For National Horticulture Board Related Activities During Xii PlanDocument3 pagesAnnexure Vii Cost Norms and Pattern of Assistance Udner Midh For National Horticulture Board Related Activities During Xii Planumanshu3359No ratings yet