Nephrotic Syndrome: Practice Gap
Nephrotic Syndrome: Practice Gap
Uploaded by
Muhammad Isnaini ZuhriCopyright:
Available Formats
Nephrotic Syndrome: Practice Gap
Nephrotic Syndrome: Practice Gap
Uploaded by
Muhammad Isnaini ZuhriOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Nephrotic Syndrome: Practice Gap
Nephrotic Syndrome: Practice Gap
Uploaded by
Muhammad Isnaini ZuhriCopyright:
Available Formats
Nephrotic Syndrome
Tecile Prince Andolino, MD,*†‡ Jessica Reid-Adam, MD†
*St. Luke’s University Health Network, Bethlehem, PA.
†
Icahn School of Medicine at Mount Sinai, New York, NY.
‡
When this review was submitted, Dr. Andolino was in her third and
final year of a pediatric nephrology fellowship at Sinai.
Practice Gap
Pediatricians must be aware of the updated treatment recommendations
and the various complications associated with nephrotic syndrome,
a common childhood renal disorder.
Objectives After completing this article, readers should be able to:
1. Understand the natural history of minimal change nephrotic syndrome.
2. Recognize the clinical and laboratory findings associated with minimal
change nephrotic syndrome.
3. Plan the appropriate initial management of the first episode of minimal
change nephrotic syndrome.
4. Formulate a differential diagnosis of nephrotic syndrome with and
without hematuria.
5. Identify the cause of hyponatremia in nephrotic syndrome.
6. Recognize complications associated with nephrotic syndrome,
including those resulting from diuretic therapy.
AUTHOR DISCLOSURE Drs Andolino and
Reid-Adam have disclosed no financial 7. Understand the various factors that affect the prognosis of nephrotic
relationships relevant to this article. This syndrome.
commentary does not contain a discussion
of an unapproved/investigative use of
a commercial product/device.
ABBREVIATIONS
Nephrotic syndrome is a disorder of the kidneys that results from increased
CNF congenital nephrotic syndrome permeability of the glomerular filtration barrier. It is characterized by 4 major
Finnish type clinical characteristics that are used in establishing the diagnosis: proteinuria,
CNS congenital nephrotic syndrome hypoalbuminemia, edema, and hyperlipidemia. This article reviews nephrotic
FSGS focal segmental glomerular syndrome in the pediatric population, with special attention paid to minimal
sclerosis
change nephrotic syndrome (MCNS).
ISKDC International Study of Kidney
Disease in Children
EPIDEMIOLOGY
KDIGO Kidney Disease Improving Global
Outcomes Nephrotic syndrome can affect children of any age, from infancy to adolescence, and
MCNS minimal change nephrotic
is most commonly seen among school-aged children and adolescents. The preva-
syndrome
MN membranous nephropathy
lence worldwide is approximately 16 cases per 100,000 children with an incidence
MPGN membranoproliferative glomerular of 2 to 7 per 100,000 children. (1) Males appear to be more affected than females
nephritis at a ratio of 2:1 in children, but this predominance fails to persist in adolescence.
Vol. 36 No. 3 MARCH 2015 117
Downloaded from http://pedsinreview.aappublications.org/ by guest on March 21, 2016
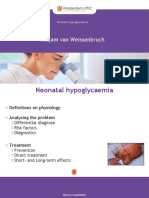
PATHOPHYSIOLOGY
The kidney uses a complex filtration system known as the
glomerular filtration barrier (GFB). It is composed of a
glomerular basement membrane sandwiched between a
fenestrated endothelium and an epithelial layer made up
of podocytes and their foot processes, with interspersed
filtration slits and slit diaphragm (Figure 1). As part of the
system’s intrinsic design, it is charge and size specific,
allowing water and small solutes to pass through its pores
into the urinary space. In nephrotic syndrome, there is an
effacement of the podocyte foot processes that can be seen
on electron microscopy. Disruption of this barrier leads to
the proteinuria seen in nephrotic syndrome.
Nephrotic syndrome can be inherited from a number of
genetic mutations that lead to defects in various regions of the
glomerular filtration barrier; presentation can vary from isolated
nephrotic syndrome seen in corticosteroid-resistant nephrotic
syndrome or focal segmental glomerular sclerosis (FSGS) to
more involved syndromes, such as nail-patella or Denys-Drash
syndromes (Table 1). Congenital nephrotic syndrome (CNS) is
usually seen within the first 3 months after birth. The classic
form of CNS is the Finnish type (CNF), which is most frequently
seen in Finland and has an incidence of 1 in 8,200 live births,
although this autosomal recessive condition has been described
in many other populations. CNF results from a mutation in the
gene encoding the protein nephrin, a key component of the slit
diaphragm. CNS is also caused by mutations of genes encoding
other proteins of the glomerular basement membrane, slit
diaphragm, and podocyte (Table 1). CNS can also be secondary
to underlying processes such as maternal lupus, neonatal
autoantibodies to neutral endopeptidase, and infections such
as syphilis, toxoplasmosis, and cytomegalovirus.
Most ongoing research into mechanisms of pathogenesis
of idiopathic nephrotic syndrome explores the roles of the
immune system and the podocyte in disease. Proposed
theories include (1) T-cell dysfunction that leads to cytokine
release that affects glomeruli and causes increased perme-
ability and (2) immune system dysfunction that leads to the
production of circulating factors (soluble urokinase plasmin- Figure 1. Glomerular filtration barrier (GFB). A. Schematic diagram;
B. normal GFB; and C. GFB in nephrotic syndrome. Note the effacement
ogen activator receptor is one example) that alter podocyte of the podocyte foot processes (P) with poor visualization of the slit
structure and/or function, resulting in proteinuria. (2)(3)(4) diaphragm (S). FE¼fenestrated endothelium. Electron microscopy images
courtesy of Fadi El Salem, MD, Icahn School of Medicine at Mount Sinai,
B-cell involvement is also suggested by reports of remission New York, NY.
after administration of rituximab, an anti-CD20 antibody. (5)
However, definitive evidence of the underlying mechanism of
syndrome refers to that which is not associated with another
action is lacking at this time.
identifiable systemic disease. Outside these 2 major group-
ings, there are 2 subsets that are based on age of presentation:
CLASSIFICATION
CNS and infantile nephrotic syndrome. Patients with the
Nephrotic syndrome can be divided into primary (idio- latter condition typically present between ages 3 months and
pathic) and secondary causes (Table 2). Idiopathic nephrotic 1 year. Some prenatal signs that are nonspecific but may
118 Pediatrics in Review
Downloaded from http://pedsinreview.aappublications.org/ by guest on March 21, 2016
TABLE 1. Genetic Forms of Nephrotic Syndrome
PROTEIN LOCATION GENE INHERITANCE PATTERN ASSOCIATED DISEASE
Nephrin Slit diaphragm NPHS1 AR CNF, FSGS
Podocin Podocyte foot process NPHS2 AR CNS, FSGS, SRNS
CD2-associated protein Slit diaphragm CD2AP AR, AD FSGS, SRNS
a-Actinin-4 Podocyte cytoskeleton ACTN2 AD FSGS, SRNS
Nonmuscle myosin heavy Podocyte cytoskeleton MYH9 Polymorphisms associated FSGS, SRNS
chain IIA with increased risk for
ESRD in blacks
LIM homeobox transcription Podocyte cytoskeleton LMX1B AD Nail-patella syndrome,
factor 1b FSGS, SRNS
Apolipoprotein L1 Podocyte cytoskeleton APOL1 Polymorphisms associated FSGS, SRNS
with increased risk for
ESRD in blacks
Inverted formin 2 Podocyte cytoskeleton INF2 AD FSGS, SRNS
Transient receptor potential Podocyte cell membrane TRPC6 AD FSGS, SRNS
cation channel 6
Laminin b2 Glomerular basement LAMB2 AR Pierson syndrome, DMS, CNS
membrane
Tetraspanin CD151 Podocyte cell membrane CD151 AR FSGS
Phospholipase C«1 Podocyte cytoplasm PLCE1/NPHS3 AR FSGS, DMS, CNS
Wilms tumor 1 Podocyte nucleus or WT1 AD Frasier syndrome, Denys-Drash
cytoplasm syndrome, FSGS, DMS, CNS
AD¼autosomal dominant; AR¼autosomal recessive; CNF¼congenital nephrotic syndrome Finnish type; CNS¼congenital nephrotic syndrome;
DMS¼diffuse mesangial sclerosis; ESRD¼end-stage renal disease; FSGS¼focal segmental glomerulosclerosis; SRNS¼(cortico)steroid-resistant nephrotic
syndrome.
suggest CNF are an enlarged placenta apparent on ultra- are other glomerulopathies that can present with nephrotic
sonogram in addition to elevated maternal serum and syndrome, including IgA nephropathy, lupus nephritis,
amniotic fluid a-fetoprotein levels. If CNF is suspected and membranoproliferative glomerulonephritis (MPGN),
in families with known risk factors, genetic testing can be and often present with a nephritic/nephrotic picture, with
performed. hematuria in addition to proteinuria. Aside from histologic
Idiopathic nephrotic syndrome can be further subdivided features, children with nephrotic syndrome can be further
based on histologic information gathered via percutaneous classified by their response to corticosteroid therapy (dis-
renal biopsy. The 3 major subgroups are MCNS (also known cussed in detail below).
as minimal change disease), FSGS, and membranous ne- Because of the patchy nature of FSGS histologically, it is
phropathy (MN). MCNS is the most common form of common to mistake FSGS for MCNS because of a sampling
nephrotic syndrome in school-aged children. On light mi- inadequacy at the time of renal biopsy; thus, an additional
croscopy, the glomeruli appear histologically normal, hence biopsy may be required at a future date to make the di-
the name minimal change disease. Although light micros- agnosis. The incidence of FSGS has increased since the
copy findings are normal, inspection by electron microscopy original studies examined nephrotic syndrome in children.
reveals fusion of the foot processes. FSGS describes what There are ongoing discoveries of genetic mutations respon-
is found histologically: some glomeruli can be normal, sible for FSGS, although these do not account for all docu-
whereas others exhibit segmental areas of sclerosis or mented cases (Table 1). Several reports suggest that MN in
scarring. Diffuse thickening of the capillary walls of the children is more commonly secondary in nature, with causes
glomeruli are histologically characteristic of MN. There such as hepatitis B and lupus inciting the pathologic changes.
Vol. 36 No. 3 MARCH 2015 119
Downloaded from http://pedsinreview.aappublications.org/ by guest on March 21, 2016
interstitial spaces (the underfill hypothesis). The hypovolemia
TABLE 2. Secondary Causes of Nephrotic that results from this fluid shift eventually leads to so-
Syndrome dium retention to compensate for the low intravascular
volume. This finding is not apparent across the board
INFECTIONS
among nephrotic patients (who may present with higher
Hepatitis B Hepatitis C plasma volumes), leading to an opposing theory of overfill
Human immunodeficiency Toxoplasmosis in which primary sodium retention leads to the edema
virus formation. One proposed mechanism is that proteinuria
Syphilis Malaria leads to increased sodium retention in the distal tubule
DISEASES OR CONDITIONS through increased activation of epithelial sodium chan-
nels. (7)
Amyloidosis Lupus
Further laboratory evaluation of patients with nephrotic
Henoch-Schönlein IgA nephropathy
purpura syndrome may reveal other abnormalities. Urinalysis can
reveal hematuria, which can be either macroscopic or mi-
Lymphoma Membranoproliferative
glomerulonephritis croscopic (>3 red blood cells per high-power field). The
percentage of patients in whom hematuria is found is lower
MEDICATIONS/DRUGS
in patients with MCNS compared with other diagnoses
Lithium Nonsteroidal anti-inflammatory
associated with nephrotic syndrome, such as FSGS and
drugs
MPGN. (8) Although microscopic hematuria is known to
Heroin Penicillamine
occur in 20% of children with MCNS, gross hematuria is
Gold Interferon g relatively uncommon and should prompt the physician to
Pamidronate consider diagnoses other than MCNS. The proteins lost in
the urine primarily consist of albumin but also include
larger proteins, such as immunoglobulins. These losses
correlate with the aforementioned hypoalbuminemia and
Idiopathic MN is more common in adults than in children, contribute to hyperlipidemia. Hyperlipidemia results from
with the exact incidence difficult to ascertain. Within the a variety of factors in nephrotic syndrome, including the
past 5 years, studies of MN revealed the presence of an decrease in oncotic pressure through loss of albumin and
autoantibody to the M-type phospholipase A2 receptor that changes in the rate of production and degradation of
is increased in adults with idiopathic MN; although anti– various products along the cholesterol pathway. More spe-
phospholipase A2 receptor has been also observed in children, cifically, there is an increase in b-hydroxy-b-methylglutaryl–
the exact prevalence among pediatric patients with MN is coenzyme A reductase activity (responsible for cholesterol
unknown at this time. (6) synthesis) with a decrease in 7a-hydroxylase activity (en-
zyme responsible for cholesterol catabolism), leading to
resultant elevated cholesterol and low-density lipoprotein
CLINICAL FEATURES
cholesterol levels. (9) Hypertriglyceridemia is a result of
Initial presentation of patients with nephrotic syndrome can decreased conversion of circulating triglycerides to free fatty
vary. The classic presentation is a child between the ages of acids due to a circulating glycoprotein, angiopoietin-like 4.
3 and 9 years with sudden-onset gravity-dependent edema. This glycoprotein is found in various tissues and is secreted
Patients tend to have periorbital edema that is often mis- in response to nephrotic range proteinuria and causes hy-
taken as sequelae from seasonal allergies. Other children pertriglyceridemia. (10)
can present without any classic signs of edema but have Serum electrolytes are generally normal in nephro-
nephrotic range proteinuria (protein level >50 mg/kg/d or tic patients. Calcium levels can be low secondary to
a spot urine protein:creatinine ratio of >2,000 mg/g) on hypoalbuminemia, but the ionized calcium will be within
urinalysis. The onset of nephrotic syndrome may some- normal limits. In addition, sodium levels can be de-
times follow a recent illness, such as a upper respiratory creased secondary to lower effective circulating volume
tract infection. There are 2 dominant theories regarding the coupled with inappropriate secretion of antidiuretic hor-
pathogenesis of edema in nephrotic syndrome. Classically, mone, causing renal retention of water. Hyponatremia
it is thought to be a result of decreased intravascular onco- can also be iatrogenic in the setting of diuretic use for
tic pressure that results in movement of fluid into the edema.
120 Pediatrics in Review
Downloaded from http://pedsinreview.aappublications.org/ by guest on March 21, 2016
COMPLICATIONS disease. Although hypothyroidism is more of a frequent
problem in patients with CNS, in whom proteinuria is
Patients with nephrotic syndrome are at risk for the devel-
heavy and long-standing, general practitioners should
opment of a variety of complications, which include throm-
recognize this as a potential issue in children who are
bosis, infections, dyslipidemia (explored in the previous
resistant to corticosteroids or who have frequent
section), and renal dysfunction. Venous thrombosis is more
relapses.
common in patients with nephrotic syndrome compared
Renal dysfunction can occur in the setting of nephrotic
with arterial thrombosis; thrombosis, when present, may
syndrome, especially with patients presenting with hypovolemia.
occur in the renal vein, sagittal sinus, or pulmonary artery.
Preceding illness, aggressive diuretic use, or sepsis with
Thrombosis in this patient population is multifactorial.
hypotension may result in decreased renal blood flow,
Patients may have a hereditary risk factor (such as Factor
causing a decrease in the glomerular filtration rate. Acute
V Leiden mutation) that predisposes them to clot forma-
kidney injury in most of these cases is reversible with
tion. They may be intravascularly depleted as a result of
remission of the nephrotic syndrome and adequate volume
nephrotic syndrome that may be exacerbated by diuretic
repletion.
use to control edema. When combined with the urinary
loss of coagulation cascade regulators (such as anti-
thrombin III) and an increase in hepatic production of MANAGEMENT AND PROGNOSIS
procoagulant factors (such as fibrinogen, factor V, and Initial workup of a child with suspected nephrotic syn-
factor VIII), conditions that favor thrombus formation drome includes urinalysis and a urine protein:creatinine
result. Thrombocytosis and platelet aggregation also ratio to establish the heavy proteinuria (usually, a urine
occur in nephrotic syndrome and may play a role in protein:creatinine ratio ‡ 2); serum chemical analyses,
thrombosis. (11) including creatinine, electrolytes, and albumin; and a cho-
In addition to urinary loss of hematologic factors, there lesterol and lipid panel. Serum complement component
is also loss of immunoglobulins. This loss of circulating C3 and antinuclear antibody titer may be indicated if there
antibodies puts nephrotic children at risk for bacterial are abnormalities within the initial aforementioned lab-
infections, particularly those with encapsulated bacteria oratory analyses or if the clinical presentation indicates
(eg, Streptococcus pneumoniae, Haemophilus influenzae, and a process other than MCNS (hematuria, elevated creat-
Group B streptococcus). Peritonitis caused by S pneumo- inine, or clinical features suggestive of autoimmune
niae is a well-described infection in children with nephrotic disease [eg, rashes, arthralgias, and unexplained fevers]).
syndrome. Patients may also experience serious infections On the basis of history, the practitioner may also consider
like cellulitis and pneumonia, and can develop sepsis. infectious causes, including hepatitis B or C or human
These children must be vaccinated against these bacteria immunodeficiency virus. A tuberculin skin test should be
because of waning immunity over time as a result of their performed at the time of diagnosis and before the start of
underlying diagnosis. Current recommendations call for therapy if results of a tuberculin skin test within the past
administration of the 23-valent pneumococcal polysac- year are not documented.
charide vaccine for all children older than 2 years with Standardization of management of patients with ne-
nephrotic syndrome. The vaccine should be administered phrotic syndrome came from prospective multicenter trials
at least 8 weeks after the last dose of the 13-valent pneu- under the International Study of Kidney Disease in Chil-
mococcal conjugate vaccine, with an additional dose of the dren (ISKDC) that began in the late 1960s. Through their
23-valent pneumococcal polysaccharide vaccine 5 years work and others, the clinical course and prognosis were
after the first dose in patients who have ongoing disease. described, and definitions of subgroups with indications
Patients undergoing treatment for nephrotic syndrome for renal biopsy were established. The cohort involved
with immunosuppressants are also at continued risk of children with nephrotic syndrome ages 3 months to 16
infections, and febrile illnesses in this population require years from North America, Europe, and Asia, and all
close follow-up. children underwent renal biopsy on entry into the study.
Beyond the urinary loss of albumin and immunoglob- Approximately 75% of patients had biopsy-proven MCNS.
ulins, nephrotic syndrome also causes the loss of other (8) Corticosteroids became the hallmark of treatment for
important proteins, including vitamin D–binding protein nephrotic syndrome and continue to be today. Patients are
and thyroid-binding globulin. This loss may cause vitamin primarily classified by their response to corticosteroid
D deficiency and increase the potential for metabolic bone therapy.
Vol. 36 No. 3 MARCH 2015 121
Downloaded from http://pedsinreview.aappublications.org/ by guest on March 21, 2016
Once the diagnosis of MCNS is suspected in a child
presenting in the classic age range for MCNS and with TABLE 3. Common Definitions of Patients With
classic features and active or latent infections are ruled out, Nephrotic Syndromea
therapy with corticosteroids should be initiated. Consultation
TERM DEFINITION
with a pediatric nephrologist and biopsy before initiation of
corticosteroid therapy should be strongly considered for Remission Urine protein:creatinine ratio <0.2 or
dipstick negative or trace reading for
patients who fall outside the typical age range (age older 3 consecutive days
than 10–12 years is often used as a cutoff) or who have
Relapse Increase in first morning urine
features atypical of MCNS (such as gross hematuria, hyper- protein:creatinine ratio to ‡2 or dipstick
tension, low complement levels, or markedly elevated creat- reading of ‡2+ for 3 of 5 consecutive days
inine level). Although most children respond to prednisone, Corticosteroid Attainment of complete remission
the importance of genetic testing is highlighted by the fact responsive with corticosteroid therapy
that certain mutations result in nephrotic syndrome that is Corticosteroid Inability to induce a remission within
resistant 4 weeks of daily corticosteroid therapy
not responsive to corticosteroid therapy. For children younger
than 1 year, there should be high suspicion for a non-MCNS Infrequent relapser 1–3 Relapses annually
diagnosis; although these patients may also require biopsy, Frequent relapser ‡2 Relapses within 6 months after
genetic testing is likely to have a higher yield in this group and initial therapy or ‡4 relapses in
any 12-month period
should be strongly considered. Prednisone and prednisolone
Corticosteroid Relapse during taper or within 2 weeks
dosing based on evidence and consensus is highlighted in
dependent of discontinuation of corticosteroid
guidelines from the Children’s Nephrotic Syndrome Con- therapy
sensus Conference (12) and, most recently, Kidney Disease: a
Adapted from Gipson et al (12) and Tarshish et al (15).
Improving Global Outcomes (KDIGO). (13) Dosing strategy
in both guidelines is similar, although recommendations
regarding length of treatment differ somewhat. KDIGO rec-
ommends an initial dose of 60 mg/m2 per day (2 mg/kg per average were able to achieve a nonrelapsing course by 3
day), with a maximum dose of 60 mg/d administered for 4 to years from initial presentation. Eighty percent of the entire
6 weeks. This is then followed by a dose of 40 mg/m2 per cohort was found retrospectively to be in remission 8 years
dose (1.5 mg/kg) every other day for 2 to 5 months, with after enrollment in the study. (15) Most of these children
tapering of the dose. This is in contrast to the consensus were noted to have MCNS as opposed to FSGS. Adjuvants to
guidelines published by the American Academy of Pedi- initial therapy in the otherwise stable outpatient population
atrics, which call for daily corticosteroids for 6 weeks may include the use of diuretics (ie, furosemide) to help
followed by alternate-day corticosteroids for another 6 with management of edema, especially if edema is severe
weeks, with no taper of dose. (12)(13) Initial studies com- enough to impair ambulation. Patients with ongoing pro-
paring a total of 8 weeks of corticosteroid therapy to teinuria should undergo serial monitoring of dyslipidemia,
a 12-week course revealed fewer relapses of nephrotic and statin drugs might be considered in children who are
syndrome in patients with the longer course. (14) Although frequent relapsers or are resistant to corticosteroids. However,
there are recommendations that corticosteroid therapy these medications are generally not needed in most patients
stop at the end of 12 weeks, there is evidence that suggests with MCNS.
that subsequent tapering of the prednisone dose for weeks The fact that most children with nephrotic syndrome are
or months results in a decrease in rate of relapse. (13) Most receiving corticosteroids for at least 3 to 5 months necessi-
children with nephrotic syndrome will respond in the first tates the discussion of prolonged corticosteroid use in this
few weeks of therapy and are labeled as corticosteroid population. The adverse effects of prednisone are well
responsive (Table 3). known and include (but are not limited to) growth impair-
The natural course of disease for most patients will be ment, weight gain with increased body mass index and
that of relapse and remission; the number of relapses is obesity, glucose intolerance, decreased bone mineralization,
variable and person dependent. In the ISKDC cohort, 75% cataracts, disturbances in behavior and/or mood, and hy-
of the initial responders who remained in remission at 6 pertension. Prednisone is an immunosuppressant and
months after initial presentation either continued to be in as such will cause increased susceptibility to infections.
remission or infrequently relapsed (one-third of the total The pediatrician should monitor for infections while the
cohort). Patients who relapsed in the first 6 months on patient is undergoing therapy and have a lower threshold
122 Pediatrics in Review
Downloaded from http://pedsinreview.aappublications.org/ by guest on March 21, 2016
TABLE 4. Alternative Therapies for Nephrotic Syndrome
DRUG CLASSIFICATION MECHANISM OF ACTION ADVERSE EFFECTS NEED TO KNOW FACTS
Cyclophosphamide Alkylating agent Depletes immune competent Alopecia, bone marrow Shown to decrease risk
cells by adding an alkyl suppression, gonadal of relapse at 6–12 months.
group to DNA toxicity with risk of Observational studies
infertility, hemorrhagic have found variation in
cystitis, secondary reported remission rates16
malignant tumor
Chlorambucil Alkylating agent Same as cyclophosphamide Bone marrow suppression, One head-to-head trial
seizures found effect to be
similar in relapse risk
when compared with
cyclophosphamide.16
Levamisole Antihelminthic and Exact mechanism not well Leukopenia, agranulocytosis, Withdrawn from the US
immunomodulator understood hepatotoxicity, vasculitis, market in 2000. Decrease
and encephalopathy in relapse rate when
compared with placebo
or prednisone but
relapses would recur
shortly after
discontinuation.16
Cyclosporine Calcineurin inhibitor Lowers the activity of T cells Nephrotoxicity, hirsutism, Effective in inducing and
and stabilizes the podocyte diabetes, hypertension, maintaining remission
actin cytoskeleton hyperkalemia, dyslipidemia, in patients. Patients often
gingival hyperplasia relapse after
discontinuation. Found
to be similar to
cyclophosphamide in
maintaining remission
at 12 months in a
meta-analysis.16–18
Tacrolimus Calcineurin inhibitor Same as cyclosporine Nephrotoxicity, diabetes, No advantage when
hypertension, hyperkalemia compared in small
head-to-head trials
with cyclosporine.16,19
Mycophenolate T- and B-cell proliferation Inhibits a vital enzyme (IMP Abdominal pain, diarrhea, Limited data when
mofetil inhibitor dehydrogenase) for leukopenia compared with
T and B cells cyclosporine and
tacrolimus. Larger
controlled trials
needed. Small trials
or studies found some
effect on patients
with CDNS.16,20
Rituximab Monoclonal antibody Antibody specific to CD20 Pulmonary toxicity, bone Case series and trials have
found on B cells marrow suppression found use in conjunction
with other medications
in CDNS allowed for
discontinuation of ‡1
immunosuppressant
medications. Patient
relapses often correlate
with recovery of B-cell
counts.5,16,21–22
Continued
Vol. 36 No. 3 MARCH 2015 123
Downloaded from http://pedsinreview.aappublications.org/ by guest on March 21, 2016
TABLE 4. (Continued )
DRUG CLASSIFICATION MECHANISM OF ACTION ADVERSE EFFECTS NEED TO KNOW FACTS
ACTH Hormone Contains peptides related to Hypertension, fluid retention, Pilot study used in
melanocortin, which binds glucose intolerance membranous nephropathy
to melanocortin receptors found decrease in
expressed in podocytes proteinuria. Small studies
found potential in
inducing remission
in FSGS.23,24
ACTH¼adrenocorticotropic hormone; CDNS¼corticosteroid-dependent nephrotic syndrome; FSGS¼focal segmental glomerular sclerosis; IMP¼inosine-5’-
monophosphate dehydrogenase.
for workup of the febrile child receiving prednisone or because they tend to have higher rates of progression to
any immunosuppressive treatment. In addition, there end-stage renal disease (estimated glomerular filtration
is likely to be some suppression of the hypothalamic- rate of <15 mL/min or dialysis dependency) and will
pituitary-adrenal axis because patients with nephrotic continue to require dialysis or renal transplantation for
syndrome are receiving daily supraphysiologic doses of management. Although transplant is curative in some
corticosteroids for at least 4 weeks and those who are forms of nephrotic syndrome (CNF, for example), certain
deemed frequent relapsers may be receiving high-dose forms of nephrotic syndrome have increased likelihood of
prednisone for longer periods. Although there has not recurrence; for example, FSGS has at least a 15% chance of
been extensive research on adrenal suppression with the recurrence in the transplanted kidney, (25) and other
recommended dosing regimen of prednisone, there is studies report rates of recurrence greater than 30%. Ther-
potential for this to occur, and pediatricians should be apies for these children often mirror those of the al-
aware of this risk. ternative therapies used for frequent relapsers who are
Patients who relapse are treated with another course of dependent on corticosteroids (Table 4). No one drug is
prednisone with the goal of decreasing the chance of cor- superior to others, and there is ongoing research to de-
ticosteroid toxicity by weaning soon after the patient is in termine disease mechanisms to better tailor therapy.
remission. The therapy includes 60 mg/m2 per day of cor- Angiotensin-converting enzyme inhibitors and angiotensin
ticosteroids as with initial presentation with weaning to II receptor blockers can also be used as a supplemental ther-
alternate-day therapy (40 mg/m2 per dose) after a urine apy to help decrease persistent proteinuria in corticosteroid-
dipstick test result is negative or trace for protein for 3 resistant nephrotic syndrome. These classes of drugs both
consecutive days. Infrequent relapsers differ from frequent reduce proteinuria and slow the progression of chronic
relapsers in recommendations concerning length of treat- kidney disease through the blockade of the renin-angiotensin
ment once the patient is receiving alternate-day therapy (4 system.
weeks vs at least 3 months in frequent relapsers). Alterna- Children who do not respond to treatment or who are
tive therapy under the guidance of a pediatric nephrologist frequent relapsers may encounter substantial strain on their
is recommended for children who are either frequent daily lives and are at risk for long-term sequelae of chronic
relapsers or steroid dependent. These alternative thera- illness. Outside the medication effects outlined in Table 4,
pies, largely immunosuppressive agents, have their own patients and families have to deal with the psychosocial
adverse effects and toxicity and have varying success rates stressors and their effect on quality of life. Beside difficul-
(Table 4). ties coping with long-term medication administration,
Children who do not respond to the initial course of pred- multiple office visits and hospitalizations inevitably lead
nisone are defined as corticosteroid resistant, which occurs to missed work and schooling. In addition, one should be
in a small percentage of the children who present with cognizant of the cosmetic adverse effects of many of the
nephrotic syndrome (approximately 10%). (15) Most of these medications used to treat nephrotic syndrome. Prednisone-
children are likely to have a diagnosis other than MCNS. As induced obesity, striae, acne, cushingoid facies, or cyclosporine-
such, referral to a pediatric nephrologist is recommended induced hirsutism may have significant social implications
for further management, which would include renal biopsy for children and adolescents and may affect medication
to aid in diagnosis. Prognosis for these children is poor adherence.
124 Pediatrics in Review
Downloaded from http://pedsinreview.aappublications.org/ by guest on March 21, 2016
CONCLUSION
Nephrotic syndrome encompasses a variety of disease pro- Summary
cesses with heavy proteinuria and hypoalbuminemia at its • On the basis of observational studies, the most common cause of
core. Despite ongoing research efforts in the mechanism nephrotic syndrome in school-aged children is minimal change
disease. (8)
of disease, first-line therapy has remained relatively un-
• On the basis of research evidence and consensus, corticosteroids
changed for decades, and corticosteroids remain the main-
are considered first-line therapy for treatment of nephrotic
stay of treatment. Guidelines published by the American syndrome. (11)(12)
Academy of Pediatrics and the KDIGO can guide the
• On the basis of consensus, prednisone therapy should be initiated
pediatrician in the treatment of MCNS. Most children at doses of 60 mg/m2 per day (2 mg/kg per day) administered for
have MCNS, which portends a good prognosis; renal 4 to 6 weeks, followed by 40 mg/m2 per dose (1.5 mg/kg) every
failure is uncommon in patients with MCNS. The course other day for at least 6 to 8 weeks. (12)(13)
of patients with nephrotic syndrome is variable, but most • On the basis of consensus and expert opinion, it is important to
patients will have periods of relapse and remission. There recognize and manage the complications that can arise in
are alternatives to corticosteroid therapy that have had patients with nephrotic syndrome, such as dyslipidemia,
infection, and thrombosis. (9)(11)(12)
success in induction and/or maintenance of remission,
• On the basis of research evidence, consensus, and expert opinion,
although findings are inconsistent, necessitating further
several alternative therapies have been observed to have variable
multicenter trials to compare these medications head efficacy in children with both corticosteroid-dependent and
to head. Genetic testing has increasingly become a valu- corticosteroid-resistant nephrotic syndrome, although caution
able tool in the identification of genetic variations as- must be exercised in the administration of these corticosteroid-
sociated with nephrotic syndrome and may obviate the sparing medications secondary to toxic adverse effects.
need for a significant number of biopsies in the future. • On the basis of observational studies, the course of nephrotic
Pediatricians must be aware of the complications second- syndrome in most patients is that of relapse and remission. (15)
ary to nephrotic syndrome and its therapies, with the
primary goal of minimizing these issues in their patients
to allow for improved growth, development, and quality of References for this article are at http://pedsinreview.aappublications.
life. org/content/36/3/117.full.
Vol. 36 No. 3 MARCH 2015 125
Downloaded from http://pedsinreview.aappublications.org/ by guest on March 21, 2016
PIR Quiz
1. Which of the following is the most common cause of nephrotic syndrome in school-aged REQUIREMENTS: Learners
children: can take Pediatrics in
A. Finnish type. Review quizzes and claim
B. Focal segmental glomerulosclerosis. credit online only at:
C. IgA nephropathy. http://pedsinreview.org.
D. Membranous nephropathy.
E. Minimal change disease. To successfully complete
2. Children with nephrotic syndrome are at particular risk for: 2015 Pediatrics in Review
A. Appendicitis. articles for AMA PRA
B. Gastritis. Category 1 CreditTM,
C. Hepatitis. learners must
D. Myositis. demonstrate a minimum
E. Peritonitis. performance level of 60%
or higher on this
3. Children with recurrent nephrotic syndrome and ongoing disease are at risk for infection
assessment, which
with encapsulated organisms. For this reason, it is important that they receive the
measures achievement of
23-valent pneumococcal polysaccharide vaccine at the time of diagnosis and:
the educational purpose
A. Annually. and/or objectives of this
B. Every other year. activity. If you score less
C. In 5 years. than 60% on the
D. In 6 months assessment, you will be
E. In 10 years. given additional
4. A 7-year-old boy presents to your office with a recent history of periorbital and pedal opportunities to answer
edema. He has been well except for a recent upper respiratory tract infection, which has questions until an overall
resolved. You suspect nephrotic syndrome. Your initial workup should include all of the 60% or greater score is
following except: achieved.
A. Albumin.
B. Cholesterol and lipid panel. This journal-based CME
C. Serum electrolytes. activity is available
D. Urine culture. through Dec. 31, 2017,
E. Urinalysis. however, credit will be
5. You have recently diagnosed a 3-year-old child as having nephrotic syndrome. The first- recorded in the year in
line treatment for this patient is: which the learner
A. Angiotensin-converting enzyme inhibitor. completes the quiz.
B. Angiotensin II receptor blocker.
C. Antibiotic.
D. Renal dialysis.
E. Corticosteroids.
126 Pediatrics in Review
Downloaded from http://pedsinreview.aappublications.org/ by guest on March 21, 2016
Nephrotic Syndrome
Tecile Prince Andolino and Jessica Reid-Adam
Pediatrics in Review 2015;36;117
DOI: 10.1542/pir.36-3-117
Updated Information & including high resolution figures, can be found at:
Services http://pedsinreview.aappublications.org/content/36/3/117
References This article cites 25 articles, 7 of which you can access for free at:
http://pedsinreview.aappublications.org/content/36/3/117#BIBL
Subspecialty Collections This article, along with others on similar topics, appears in the
following collection(s):
Journal CME
http://beta.pedsinreview.aappublications.org/cgi/collection/journal_c
me
Nephrology
http://beta.pedsinreview.aappublications.org/cgi/collection/nephrolo
gy_sub
Permissions & Licensing Information about reproducing this article in parts (figures, tables) or
in its entirety can be found online at:
http://beta.pedsinreview.aappublications.org/site/misc/Permissions.x
html
Reprints Information about ordering reprints can be found online:
http://beta.pedsinreview.aappublications.org/site/misc/reprints.xhtml
Downloaded from http://pedsinreview.aappublications.org/ by guest on March 21, 2016
Nephrotic Syndrome
Tecile Prince Andolino and Jessica Reid-Adam
Pediatrics in Review 2015;36;117
DOI: 10.1542/pir.36-3-117
The online version of this article, along with updated information and services, is
located on the World Wide Web at:
http://pedsinreview.aappublications.org/content/36/3/117
Pediatrics in Review is the official journal of the American Academy of Pediatrics. A monthly
publication, it has been published continuously since 1979. Pediatrics in Review is owned,
published, and trademarked by the American Academy of Pediatrics, 141 Northwest Point
Boulevard, Elk Grove Village, Illinois, 60007. Copyright © 2015 by the American Academy of
Pediatrics. All rights reserved. Print ISSN: 0191-9601.
Downloaded from http://pedsinreview.aappublications.org/ by guest on March 21, 2016
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good Life4/5 (6054)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You Are4/5 (1142)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On It4.5/5 (917)
- BSAVA Manual of Canine and Feline Dentistry and Oral Surgery 4th Edition100% (1)BSAVA Manual of Canine and Feline Dentistry and Oral Surgery 4th Edition394 pages
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space Race4/5 (946)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy Answers4.5/5 (361)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New America4.5/5 (273)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first Century3.5/5 (2283)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True Story3.5/5 (233)
- Benefits of Selective Vitamin D Receptor Activators in Kidney Transplanted PatientsNo ratings yetBenefits of Selective Vitamin D Receptor Activators in Kidney Transplanted Patients13 pages
- Fibroblast Growth Factor 23/klotho Axis in Chronic Kidney DiseaseNo ratings yetFibroblast Growth Factor 23/klotho Axis in Chronic Kidney Disease10 pages
- Raghuveer D V S A - MALE - 25 Yrs +917539921204 APJ1.0021927577 5857182No ratings yetRaghuveer D V S A - MALE - 25 Yrs +917539921204 APJ1.0021927577 58571822 pages
- 2021 Special Report of The Society For MaternalFetal Medicine Placenta Accreta SpectrumNo ratings yet2021 Special Report of The Society For MaternalFetal Medicine Placenta Accreta Spectrum13 pages
- Menopause & Postmenopause: Lauren Nathan, MDNo ratings yetMenopause & Postmenopause: Lauren Nathan, MD23 pages
- Karyanti - Severe Dengue - Multiorgan Involvement in Dengue - FinalNo ratings yetKaryanti - Severe Dengue - Multiorgan Involvement in Dengue - Final53 pages
- Acetylcholinesterase Inhibitors As Alzheimer Therapy From Nerve Toxins To NeuroprotectionNo ratings yetAcetylcholinesterase Inhibitors As Alzheimer Therapy From Nerve Toxins To Neuroprotection24 pages
- Amy Purdy - Living Beyond Limits - Revisión Del IntentoNo ratings yetAmy Purdy - Living Beyond Limits - Revisión Del Intento6 pages
- Efficacy and Safety of Non-Invasive Body Tightening With High-Intensity Focused Ultrasound (HIFU)No ratings yetEfficacy and Safety of Non-Invasive Body Tightening With High-Intensity Focused Ultrasound (HIFU)5 pages
- Nursing Care of A Family During Labor and BirthNo ratings yetNursing Care of A Family During Labor and Birth2 pages
- Mirjam Van Weissenbruch - Neonatal HypoglycaemiaNo ratings yetMirjam Van Weissenbruch - Neonatal Hypoglycaemia57 pages
- Hyper Male Force Reviews - Does It Really Work?No ratings yetHyper Male Force Reviews - Does It Really Work?3 pages
- (Natural Co-Q 10 For Your Heart) : Presentation by - Dr. Vikram Chauhan (MD - Ayurveda)No ratings yet(Natural Co-Q 10 For Your Heart) : Presentation by - Dr. Vikram Chauhan (MD - Ayurveda)14 pages
- 推動DA-CPR之品質管理及效能提昇暨自動心肺復甦機應用效益評估研究報告+106年11月No ratings yet推動DA-CPR之品質管理及效能提昇暨自動心肺復甦機應用效益評估研究報告+106年11月30 pages
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good Life
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You Are
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On It
- BSAVA Manual of Canine and Feline Dentistry and Oral Surgery 4th EditionBSAVA Manual of Canine and Feline Dentistry and Oral Surgery 4th Edition
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space Race
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy Answers
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic Future
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of Cancer
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy Living
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New America
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first Century
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham Lincoln
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True Story
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New Deal
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New America
- Benefits of Selective Vitamin D Receptor Activators in Kidney Transplanted PatientsBenefits of Selective Vitamin D Receptor Activators in Kidney Transplanted Patients
- Fibroblast Growth Factor 23/klotho Axis in Chronic Kidney DiseaseFibroblast Growth Factor 23/klotho Axis in Chronic Kidney Disease
- Raghuveer D V S A - MALE - 25 Yrs +917539921204 APJ1.0021927577 5857182Raghuveer D V S A - MALE - 25 Yrs +917539921204 APJ1.0021927577 5857182
- 2021 Special Report of The Society For MaternalFetal Medicine Placenta Accreta Spectrum2021 Special Report of The Society For MaternalFetal Medicine Placenta Accreta Spectrum
- Karyanti - Severe Dengue - Multiorgan Involvement in Dengue - FinalKaryanti - Severe Dengue - Multiorgan Involvement in Dengue - Final
- Acetylcholinesterase Inhibitors As Alzheimer Therapy From Nerve Toxins To NeuroprotectionAcetylcholinesterase Inhibitors As Alzheimer Therapy From Nerve Toxins To Neuroprotection
- Amy Purdy - Living Beyond Limits - Revisión Del IntentoAmy Purdy - Living Beyond Limits - Revisión Del Intento
- Efficacy and Safety of Non-Invasive Body Tightening With High-Intensity Focused Ultrasound (HIFU)Efficacy and Safety of Non-Invasive Body Tightening With High-Intensity Focused Ultrasound (HIFU)
- (Natural Co-Q 10 For Your Heart) : Presentation by - Dr. Vikram Chauhan (MD - Ayurveda)(Natural Co-Q 10 For Your Heart) : Presentation by - Dr. Vikram Chauhan (MD - Ayurveda)