The Nasolabial Flap: The Most Versatile Method in Facial Reconstruction
The Nasolabial Flap: The Most Versatile Method in Facial Reconstruction
Uploaded by
shreya dasCopyright:
Available Formats
The Nasolabial Flap: The Most Versatile Method in Facial Reconstruction
The Nasolabial Flap: The Most Versatile Method in Facial Reconstruction
Uploaded by
shreya dasOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
The Nasolabial Flap: The Most Versatile Method in Facial Reconstruction
The Nasolabial Flap: The Most Versatile Method in Facial Reconstruction
Uploaded by
shreya dasCopyright:
Available Formats
THE NASOLABIAL FLAP:
THE MOST VERSATILE METHOD
IN FACIAL RECONSTRUCTION
Bayer J., Schwarzmannová K., Dušková M., Novotná K., Kníže J., Sukop A.
Department of Plastic Surgery, 3rd Faculty of Medicine, Charles University, University Hospital Královské Vinohrady, Prague,
Czech Republic
ACTA CHIRURGIAE PLASTICAE, 59, 3, 2017, pp. 00-00.
ABSTRACT workhorse and an integral instrument for KEYWORDS
every plastic surgeon. Over time multiple
The nasolabial flap was described 170 years modifications of this technique have been xxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxx
ago and still remains one of the most fre- described. In this article, authors present an xxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxx
quently used methods in facial reconstruc- overview of nasolabial flap modalities and
tion. This technically easy and maximally discuss advantages and disadvantages of
effective procedure has become a real these techniques.
INTRODUCTION mined by the amount of natural excess of tissue at the
nasolabial crease and its extensibility. The inferiorly
The nasolabial (also called melolabial) flap was one of based flap is useful for upper and lower lip defects, the
the first local flaps used for closure of defects in the mid- floor of the nose and reconstruction of the columella.4, 5
facial area. It was described in 1846 by a German surgeon, (Fig. 1, 2.)
Johann Friedrich Dieffenbach, and still remains the most
useful option for reconstruction in the area of facial tri- ANATOMY OF THE VASCULAR SUPPLY
angle due to its versatility and effectiveness.1, 2 Over 560
articles were found in PubMed search for nasolabial flap The paranasal cheek area is supplied medially by the an-
between 1960 and 2016.3 gular artery and its perforating branches. The central cheek
This flap may be either superiorly or inferiorly based. is supplied by the perforating branches from the internal
The most commonly used superiorly based flap is useful maxillary artery as well as by extensions of the transverse
for defects of the central and lateral nasal dorsum as well facial branch from the superficial temporal artery. The naso-
as the nasal tip and ala. This technique allows harvest- labial flap can be used as a random pattern type or it can be
ing a huge flap along the whole length of nasolabial fold lifted as an axial pattern flap. The vascular supply to random
down to the border of the chin and in the width deter- flaps arises from the subdermal vascular plexus and dermal
Fig. 1. Nasolabial flap with superior pedicle Fig. 2. Nasolabial flap with inferior pedicle
2017, 59, No. 3-4 ACTA CHIRURGIAE PLASTICAE 129
Fig. 3. Tumorous infiltration of the nasal ala Fig. 4. Transposition nasolabial flap
plexus, which are ultimately supplied by musculocutane- Interpolation flap
ous arteries. Thus, the appropriate plane of dissection is Interpolation flaps are similar to transposition flaps
subcutaneous fat. 6 with the difference that the interpolation flap is lifted over
an area of normal skin to reach the defect. The base of the
NASOLABIAL FLAP MODALITIES flap is not immediately adjacent to the recipient site. This
arrangement results in a bridge of tissue, or pedicle, between
Transposition flap the flap base and the surgical defect. These flaps are used
This technique, usually based on the superior pedicle, when insufficient tissue or mobility in nearby skin prevents
allows the use of the cheek tissue adjacent to the upper lip coverage of a surgical defect with primary closure or an
from which a larger flap can be harvested. The flap is raised adjacent flap. An interpolation flap is a two-stage surgery.
and transferred as a single stage procedure to an immediately The bridge must be disconnected in a second stage when the
adjacent defect. With the paramedian forehead flap, this new vascular supply is established between the wound and
technique is the most suitable method for reconstruction the flap (usually after 3 weeks).7, 10, 11 (Fig. 6 A–D.)
of the nasal lobule. This method is very suitable for nasal tip or columella
When the defect is on the lateral nasal lobule and does reconstruction. Often in combination with cartilaginous
not cross the midline, the flap may be based only on dermal grafts, mucosal flaps or skin grafts, it could be used for
blood supply. rconstruction of penetrating (complex) nasal defects.10, 11
The medial border of the flap should be drawn from the (Fig. 7A–D.)
tangent at the edge of the defect so as to leave the lateral
alar crease intact. The flap is then back-cut to approximately Advancement flap - V-Y flap
the same level and a Burrow´s triangle is removed from the A sliding flap from the nasolabial fold in a V-Y manner
upper lateral nasal skin. The cheek skin over the malar and is well suited for reconstructing the area where the lower
buccal areas is then elevated in a subcutaneous plane, so or middle third of the nose meets the cheek. Like the island
that the transposition flap becomes a secondary extension flap, the sliding flap is generally slid into the defect on
from the edge of the cheek advancement flap. The nasola- a subcutaneous pedicle.7, 12 (Fig. 8A–D.)
bial transposition flap should be defatted to the appropriate
thickness at the time of transfer so that a secondary revision Subcutaneously pedicled island flap
should be unnecessary. The flap could also be folded upon This method popularized by Bouisson (1864) is also use-
itself for nasal lining or extended past the midline. In this ful for reconstructing small defects in the nasal flank area.
case, consideration may be given either to delay the flap or The flap may be based on the facial artery or be designed
to maintain a direct communication with the subcutaneous with a subcutaneous pedicle that has an inferolateral or su-
portion of the pedicle and its branches from the angular perolateral position in relation to the flap. The skin between
artery.6, 7 (Fig. 3, 4.) the flap and the defect is undermined, and the pedicle is
Transposition nasolabial flaps are very often used pulled through. Care is taken not to place excessive torsion
for reconstruction of complex nasal defects especially in or pressure on the flap pedicle. Because the subcutaneous
the alar and tip regions. The flap could be folded upon pedicle often creates fullness at the pull-through site, this
itself to restore nasal lining usually in combination with is not one of the most favourite flaps. The cheek must be
other flaps such as forehead or contralateral nasolabial mobilized somewhat more widely than with other flaps to
flaps.8, 9, 17, 24 (Fig. 5.) avoid distorting the upper lip.4, 6, 7, 13
130 ACTA CHIRURGIAE PLASTICAE 2017, 59, No. 3-4
Fig. 5A–F. Sequence of nasal lining reconstruction with transposition nasolabial flap
2017, 59, No. 3-4 ACTA CHIRURGIAE PLASTICAE 131
Fig. 6A–D. Sequence of nasal ala defect reconstruction with interpolation nasolabial flap
Facial artery perforator based nasolabial flap DISCUSSION
The facial artery perforator-based nasolabial flap is sup-
ported by the study of angiosomes of the facial region and When choosing the method of facial reconstruction,
is usually based on the superior labial artery perforator, in- it is necessary to carefully consider surgical stress on the
cluding the facial artery perforator. These flaps are designed patient, the technical demand of the approach, and the
as rotation propeller flaps. The term “propeller flap” is an type of anaesthesia. These circumstances must meet the
island flap that reaches the recipient site by axial rotation. expected benefit of the surgery. The surgery must be un-
This technique allows greater freedom in rotation, mobility, dergone in a disease free terrain, however, it is necessary
and flap design for the reconstruction of perinasal defects. to maintain good function and an acceptable appearance.
Possible negative aspect of this method is the time required. The need of functional and aesthetic effects may be differ-
Perforator dissection is a more difficult procedure than the use ent according to each individual personality. The simplest
of other local flaps that do not require perforator dissection.14, 15 method for closure of facial defects is a skin graft. It can
be used only in superficial defects with a suitable vascular
Nasolabial free flap bed.11, 21, 22
A nasolabial free flap consisting of a part of the risorius The cosmetic outcome of skin grafts may be poor due
and buccinator muscles, buccal mucosa, and nasolabial to the colour and texture mismatch. Especially in nasal
skin is rarely used for reconstruction of full-thickness lower reconstruction, local flaps such as nasolabial or dorsal
eyelid defects. This flap, supported by the facial vessels, is nasal flap have better results. Bilobed flaps are now largely
transported via microvascular anastomosis to the superficial abandoned in nasal reconstruction because they almost
temporal vessels.16 violate the subunit principle either at the donor site or
132 ACTA CHIRURGIAE PLASTICAE 2017, 59, No. 3-4
Fig. 7A–D. Sequence of reconstruction of a penetrating defect of the nasal tip with interpolation nasolabial flap in combination with
nasal mucosal advancement
at the recipient site.19 Dorsal nasal flaps are often linked CONCLUSION
with apparent scars and are insufficient for large tip
defects.1 The nasolabial flap is an easy, quick and effective ap-
In deep and large defects of the nose and the centro- proach for treatment of smaller and middle-sized defects
facial region, only nasolabial and forehead flaps can be of the midfacial area. This technique allows harvesting
used. The forehead flap, which is more suitable for larger a wide and rich vascularized flap along the whole length
defects of the nasal dorsum and tip, represents more en- of the nasolabial fold. In combination with the wide arc
cumbering two-stage surgery, which requires general of rotation, the flap could reach almost any site of centro-
anaesthesia and results in a more visible scar at the donor facial area. The flap perfectly matches the requirements of
area18. Postoperative morbidity can be considerably higher complex reconstruction including the possibility to com-
for forehead flaps than for nasolabial flaps.1, 18, 19, 23, 25 bine it with cartilage graft. It produces a good functional
The nasolabial flap perfectly matches the requirements and aesthetic outcome with minimal donor site morbidity
of complex reconstruction of small and middle size defects and overall stress for the patient. Therefore, it is suitable
including the possibility to combine it with a cartilage for patients with higher expectations even in cases that
graft or a contralateral flap. Technically, it is an easy they are old and polymorbid. Due to its versatility and
surgery performed in local anaesthesia with minimal effectiveness, the nasolabial flap still remains the most
donor site morbidity. Disadvantages of this procedure useful option for reconstruction in the area of facial tri-
are the risk of transferring hairy skin onto the nose and angle.
two-stage procedure in the interpolation variant of this
flap.20, 21, 22, 23, 25
2017, 59, No. 3-4 ACTA CHIRURGIAE PLASTICAE 133
Fig. 8A–D. Sequence of reconstruction of defect on the nasal-cheek border with V-Y advancement nasolabial flap
REFERENCES of Cutaneous Malignancies: Single Institutional Experience of Seventy
Cases. J Cutan Aesthet Surg. 2016 Oct-Dec;9(4):220-225.
1. Thornton JF, Weathers WM. Nasolabial flap for nasal tip reconstruction. 3. Rahpeyma A, Khajehahmadi S. The place of nasolabial flap in oro-
Plast Reconstr Surg. 2008 Sep;122(3):775-81. facial reconstruction: A review. Ann Med Surg (Lond). 2016 Nov
2. Rao JK, Shende KS. Overview of Local Flaps of the Face for Reconstruction 23;12:79-87.
134 ACTA CHIRURGIAE PLASTICAE 2017, 59, No. 3-4
4. Rudkin GH, Carlsen BT, Miller TA. Nasolabial flap reconstruction of large 17. Takeda A, Akimoto M, Park K et al. Single-stage reconstruction of a full-
defects of the lower lip. Plast Reconstr Surg. 2003 Feb;111(2):810-7. thickness alar defect using a folded nasolabial flap combined with a re-
5. Yanai A, Nagata S, Tanaka H. Reconstruction of the columella with bilat- dundant skin turnover flap. J Craniofac Surg. 2014 Nov;25(6):2144-6.
eral nasolabial flaps. Plast Reconstr Surg. 1986 Jan;77(1):129-32. 18. Uchinuma E, Matsui K, Shimakura Y, Murashita K, Shioya N. Evaluation of
6. Ohtsuka H, Shioya N, Asano T. Clinical experience with nasolabial flaps. the median forehead flap and the nasolabial flap in nasal reconstruction.
Ann Plast Surg. 1981 Mar;6(3):207-12. Aesthetic Plast Surg. 1997 Mar-Apr;21(2):86-9.
7. Weerda, Hilko. Reconstructive facial plastic surgery: a problem-solving 19. Lindsay KJ, Morton JD. Flap or graft: The best of both in nasal ala recon-
manual. Univ of California Press, 2001.pPg. 36-46, 62 struction. J Plast Reconstr Aesthet Surg. 2015 Oct;68(10):1352-7.
8. Zelken JA, Reddy SK, Chang CS et al. Nasolabial and forehead flap recon- 20. Weathers WM, Wolfswinkel EM, Nguyen H, Thornton JF. Expanded uses
struction of contiguous alar-upper lip defects. J Plast Reconstr Aesthet for the nasolabial flap. Semin Plast Surg. 2013 May;27(2):104-9.
Surg. 2017 Mar;70(3):330-335. 21. Lunatschek C, Schwipper V, Scheithauer M. Soft tissue reconstruction of
9. Sukop A, Tvrdek M, Duskova M, Hýza P, Haas M, Bayer J. Nasal recon- the nose. Facial Plast Surg. 2011 Jun;27(3):249-57.
struction in children with the combination of nasolabial and island flaps. 22. Menick FJ. Practical details of nasal reconstruction. Plast Reconstr Surg.
Acta Chir Plast. 2010;52(1):3-6. 2013 Apr;131(4):613e-30e.
10. Smith JW et al. Grabb and Smith’s plastic surgery. Lippincott-Raven, 23. Konofaos P, Alvarez S, McKinnie JE, Wallace RD. Nasal Reconstruction:
1997. pg. 392. A Simplified Approach Based on 419 Operated Cases. Aesthetic Plast
11. McGregor, Ian A., and Alan D. McGregor. Fundamental techniques of Surg. 2015 Feb;39(1):91-9.
plastic surgery: and their surgical applications. Churchill Livingstone, 24. Rohrich RJ, Conrad MH. The superiorly based nasolabial flap for si-
2000. pg. 178-9. multaneous alar and cheek reconstruction. Plast Reconstr Surg. 2001
12. Rose EH. One-stage arterialized nasolabial island flap for floor of mouth Nov;108(6):1727-30.
reconstruction. Ann Plast Surg. 1981 Jan;6(1):71-5. 25. Thornton JF, Griffin JR, Constantine FC. Nasal reconstruction: an over-
13. Turan A, Kul Z, Türkaslan T, Ozyiğit T, Ozsoy Z. Reconstruction of lower view and nuances. Semin Plast Surg. 2008 Nov;22(4):257-68.
half defects of the nose with the lateral nasal artery pedicle nasolabial
island flap. Plast Reconstr Surg. 2007 May;119(6):1767-72.
14. Yoon TH, Yun IS, Rha DK, Lee WJ. Reconstruction of various perinasal
defects using facial artery perforator-based nasolabial island flaps. Arch Corresponding author:
Plast Surg. 2013 Nov;40(6):754-60.
15. Durgun M, Özakpınar HR, Selçuk CT, Sari E, Seven E, İnözü E. Repair of Jiří Bayer, M.D.
Full-Thickness Nasal Alar Defects Using Nasolabial Perforator Flaps. Ann Department of Plastic Surgery, 3rd Faculty of
Plast Surg. 2015 Oct;75(4):414-7. Medicine, Charles University
16. Sasaki K, Nozaki M, Katahira J, Kikuchi Y. A nasolabial composite free and University Hospital Královské Vinohrady
flap with buccal mucosa: reconstruction of full-thickness lower eyelid Šrobárova 50, 100 34 Prague 10, Czech Republic
defects. Plast Reconstr Surg. 1998 Aug;102(2):464-72. E-mail: bayer01@seznam.cz
2017, 59, No. 3-4 ACTA CHIRURGIAE PLASTICAE 135
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5985)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1112)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (898)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (932)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (619)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (546)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (357)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (831)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (477)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (275)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (425)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2272)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (99)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (125)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (270)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (232)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (235)
- FDA Appeal - 1.31.2024Document69 pagesFDA Appeal - 1.31.2024charlie minatoNo ratings yet
- English Short Stories For Beginners and Intermediate Learners Engaging Short Stories To Learn English and Build Your Vocabulary (2nd Edition) by Language GuruDocument79 pagesEnglish Short Stories For Beginners and Intermediate Learners Engaging Short Stories To Learn English and Build Your Vocabulary (2nd Edition) by Language GuruWilliam Farwok97% (38)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (75)
- Yoga For Sports A Journey TowaDocument538 pagesYoga For Sports A Journey TowaLorie Pg92% (12)
- Ozone Therapy in DentistryDocument16 pagesOzone Therapy in Dentistryshreya das100% (1)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- National Students Olympiad Stage IvDocument47 pagesNational Students Olympiad Stage Ivklevan11178100% (1)
- Condylar SagDocument8 pagesCondylar Sagshreya dasNo ratings yet
- 63b2c987bdb70 - Advertisement of Senior ResidentsDocument13 pages63b2c987bdb70 - Advertisement of Senior Residentsshreya dasNo ratings yet
- INI-CET January 2021advertisement NoticeDocument1 pageINI-CET January 2021advertisement Noticeshreya dasNo ratings yet
- Maxillary SinusDocument25 pagesMaxillary Sinusshreya dasNo ratings yet
- Maxillary SinusDocument6 pagesMaxillary SinusrichardNo ratings yet
- Seminar On Cementum: Shreya Das Intern Department of PeriodontiaDocument57 pagesSeminar On Cementum: Shreya Das Intern Department of Periodontiashreya dasNo ratings yet
- LCPC Indicators Guide With MOVsDocument27 pagesLCPC Indicators Guide With MOVsbarangayotolpatacNo ratings yet
- Insulin Hypoglycemic Effect in RabbitDocument3 pagesInsulin Hypoglycemic Effect in RabbitBlAcK ShArK OPNo ratings yet
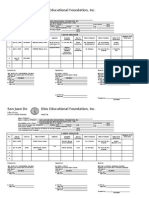
- San Juan de Dios Educational Foundation, IncDocument6 pagesSan Juan de Dios Educational Foundation, Incmae- athenaNo ratings yet
- Valena Scientific Corporation - Case StudyDocument4 pagesValena Scientific Corporation - Case Studyaaashu770% (1)
- Andhra Pradesh State Chief Minister Office - Official AP State Government Portal - AP State Portal1Document2 pagesAndhra Pradesh State Chief Minister Office - Official AP State Government Portal - AP State Portal1kishoreputhaNo ratings yet
- Supplemental Material: Lower Extremity Functional Training (LIFT) DescriptionDocument11 pagesSupplemental Material: Lower Extremity Functional Training (LIFT) DescriptionGayuh Candra BuanaNo ratings yet
- Birhane Design Report For Residence BuildingDocument10 pagesBirhane Design Report For Residence BuildingHaymanot BaynesagnNo ratings yet
- Science DirectDocument12 pagesScience DirectAthallla SyifaNo ratings yet
- Christina Branco Client Agreement Form PsychotherapyDocument3 pagesChristina Branco Client Agreement Form Psychotherapyapi-266930998No ratings yet
- Report 7Document73 pagesReport 7Kumar SagarNo ratings yet
- CE Sertificate WESTINDocument2 pagesCE Sertificate WESTINpurwoko setiawanNo ratings yet
- The Adult DCD/Dyspraxia Checklist (ADC) Instructions For Use (Kirby & Rosenblum, 2008) Revision of Scoring (2011) About DCD in AdultsDocument4 pagesThe Adult DCD/Dyspraxia Checklist (ADC) Instructions For Use (Kirby & Rosenblum, 2008) Revision of Scoring (2011) About DCD in AdultsAndreia CostaNo ratings yet
- PracticeExam 4 QsDocument17 pagesPracticeExam 4 QsBehrouz YariNo ratings yet
- PFPL Barry Brown WS18221APFDocument10 pagesPFPL Barry Brown WS18221APFMohammed Tanjil Morshed remonNo ratings yet
- Vistas 2011 Article 53Document13 pagesVistas 2011 Article 53Ateh HashimNo ratings yet
- Borderline Psychopathology and Its Treatment 1465719148Document275 pagesBorderline Psychopathology and Its Treatment 1465719148mark pavlovic100% (2)
- INGLES IV ACV-S02 Week 02Document5 pagesINGLES IV ACV-S02 Week 02Abel CuadrosNo ratings yet
- Structural Steel Design For Steel Intensive Structure by Dnyaneshwar Gawai and GroupDocument35 pagesStructural Steel Design For Steel Intensive Structure by Dnyaneshwar Gawai and GroupDnyaneshwar Gawai100% (1)
- Deep Creek InfoDocument46 pagesDeep Creek Infoapi-476696603No ratings yet
- HNSC 1100 BCA FALL 2022 Exam 1 Review SheetDocument2 pagesHNSC 1100 BCA FALL 2022 Exam 1 Review SheetKALEAH GASKINNo ratings yet
- MCQDocument3 pagesMCQFoysal SirazeeNo ratings yet
- Immediate download Hair and Scalp Disorders: Medical, Surgical, and Cosmetic Treatments 2nd Edition Amy J. Mcmichael ebooks 2024Document62 pagesImmediate download Hair and Scalp Disorders: Medical, Surgical, and Cosmetic Treatments 2nd Edition Amy J. Mcmichael ebooks 2024viccazmax100% (2)
- Piyus's Diet PlanDocument2 pagesPiyus's Diet PlanPiyushNo ratings yet
- Safety Data Sheet: Diversey Eastern and Central Africa LimitedDocument2 pagesSafety Data Sheet: Diversey Eastern and Central Africa LimitedsivabioteckNo ratings yet
- What Is Family Life CycleDocument7 pagesWhat Is Family Life Cycleapi-414688913No ratings yet
- Q1-Cookery-Module-LESSON-11 Sanitation ProceduresDocument5 pagesQ1-Cookery-Module-LESSON-11 Sanitation ProceduresMay Ann GuintoNo ratings yet