BSN 1 H Case Application Nursing Care Plan
BSN 1 H Case Application Nursing Care Plan
Uploaded by
Antonio EscotoCopyright:
Available Formats
BSN 1 H Case Application Nursing Care Plan
BSN 1 H Case Application Nursing Care Plan
Uploaded by
Antonio EscotoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
BSN 1 H Case Application Nursing Care Plan
BSN 1 H Case Application Nursing Care Plan
Uploaded by
Antonio EscotoCopyright:
Available Formats
University of San Agustin
General Luna St., 5000 Iloilo City, Philippines
www.usa.edu.ph
COLLEGE OF HEALTH AND ALLIED MEDICAL PROFESSIONS - DEPARTMENT OF NURSING
NAME: CARLOS MIGUEL S. DE LA GENTE YEAR/SECTION:BSN 1-H
Case Application - Nursing Care Plan
Construct a Nursing Care Plan for Mr. Roman & Ms. Perez:
1. Mr. Roman, 25 years of age, presents to the triage nurse at the local emergency department,
complaining of severe generalized abdominal pain. She describes it as sharp and
intermittent. He states, “Over the last 4 days, I haven’t been able to have a bowel movement.”
He states that he is able to drink liquids and urinating without difficulty. Bowel sounds are
present in all 4 quadrants, however, they are hypoactive (decreased or quiet peristalsis).
Abdomen is distended and firm to touch. He states, “Two weeks ago I feel that my back hurts.
My doctor gave me a prescription of Tylenol #3 & I have been taking it every 6 hours for
pain.” He denies pain at the present time. Abdominal x-ray reveals a large amount of stool in his
lower colon. All other diagnostic tests are unremarkable. He was prescribed with Dulcolax 1
tablet once a day.
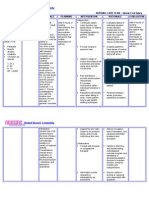
Diagnosis Goal Intervention Rationale Evaluation
Acute Abdominal Within 8 Independent: Independent: Short term:
Pain R/T pressure hours of Examine To The goal was
from distended receiving the daily promote achieved. After 4
abdomen as nursing care, routine of a patient hours of nursing
evidenced by: the patient patient. cooperatio interventions, the
will be able to n. patient reported
Subjective: express relief Obtain the Helpful in that the pain was
He states, from patient’s assessing relieved/controlle
“Two gastrointestin vital signs. the need d, that he
weeks al distress and for followed the
ago I feel maintain a Provide a interventio prescribed
that my stable stool quiet n pharmaceutical
back passage at environmen To help regimen to relieve
hurts. regular t and assess pain, that he
intervals. reduce what could verbalized non-
He also stimuli have been pharmacologic
states, (e.g., noise, the factor ways that give
"Over the lightning, affecting relief, and that he
last 4 constant the patient was able to relax
days, I interruption in his daily and sleep/rest
haven’t s) routine. correctly.
been able
to have a List all the Dependent:
bowel patient’s
movemen current Used to
t. prescription help
s. relieve
Email: cn@usa.edu.ph | Tel. No.: 0999-997-1485 | Fax No.: (033) 337-4403
University of San Agustin
General Luna St., 5000 Iloilo City, Philippines
www.usa.edu.ph
COLLEGE OF HEALTH AND ALLIED MEDICAL PROFESSIONS - DEPARTMENT OF NURSING
mild to
moderate
Objective: Dependent: pain.
Abdomen is 1. Dulcolax 1 It works
distended and tab, once a directly on
firm to touch. day the colon
2. laxative to produce
such as a bowel
Dulcolax 1- movement
tab qd .
Interdependent:
Suction to
relieve
buildup of
gas and
liquid
Surgery
2. Mrs. Perez, 48 years old, is admitted to the nursing unit 2 hours after undergoing a right
surgical removal of her breast (mastectomy). The floor nurse receives a report from the
post anesthesia care unit (PACU) nurse that includes the patient’s admitting diagnosis of
breast cancer, latest vital signs, focused assessment, medication & intravenous (IV)
orders, pain level & the time she was last medicated for pain & status of the surgical
dressing. Initially, Mrs. Perez appears to be comfortable, dozing occasionally between
short conversations with her husband, who is at her side. When she was fully awake 3
hours after, she complains of sharp, constant pain on the right side of her chest. She
rates her pain at 8 / 10 on the pain scale. She is grimacing and appears tense. The RN
took her vital signs - T = 36.5 "C; BP = 130/100 mmHg; RR = 20 bpm; PR = 80
beats/min. She inspected the surgical wound, at the right breast and reveals that the
dressing is slightly soaked with blood and intact, no pus & slightly swelling noted.
Diagnosis Goal Intervention Rationale Evaluation
Mastectomy R/T After 1 Independent: Independent: Short Term:
impaired skin hour of Establish This could Goal met. After
integrity related nurse- Rapport serve as 1hour of nurse
to surgery to patient baseline data patient
breast removal interaction Avoid sudden Sudden interactionwithi
as evidenced by: over an 8- movement movement n an 8 hour shift,
hour shift, can cause the patient was
Subjective: the patient Access mode damage to able to verbalize
She complains of will be able coping the healing and demonstrate
sharp constant to know, abilities and tissues on the theright
pain on the right pronounce, personality surgical measures
side of her chest. and show styles wound intaking of her
Email: cn@usa.edu.ph | Tel. No.: 0999-997-1485 | Fax No.: (033) 337-4403
University of San Agustin
General Luna St., 5000 Iloilo City, Philippines
www.usa.edu.ph
COLLEGE OF HEALTH AND ALLIED MEDICAL PROFESSIONS - DEPARTMENT OF NURSING
the proper To enhance post- surgical
Objective: precaution Consider the self- esteem skin.
She rates s and post- importance of and sense of
her pain surgical post-surgery self- worth.
at 8 / 10 skin care to rehabilitation The client
on the prevent . stands to
pain infection. accommodat
scale e the change
Dependent: in the center
She is Tylenol 1 tab PRN of gravity by
grimacin Advil 1 cap TID leaning to the
g and side.
appears
tense.
Email: cn@usa.edu.ph | Tel. No.: 0999-997-1485 | Fax No.: (033) 337-4403
You might also like
- Case Study 2Document7 pagesCase Study 2desdav100% (1)
- Valdez Reflective-Questions PDFDocument3 pagesValdez Reflective-Questions PDFDexel Lorren ValdezNo ratings yet
- Alc Intra1 Questionnaire HypertensiveDocument5 pagesAlc Intra1 Questionnaire HypertensiveAndrea Blanca100% (1)
- NCP Cavernous Sinus ThrombosisDocument3 pagesNCP Cavernous Sinus ThrombosisVencel Mae Famas Villahermosa50% (2)
- Nursing Care Plan: Clustered Cues Nursing Diagnosis Rationale Outcome Criteria Nursing Interventions Rationale EvaluationDocument2 pagesNursing Care Plan: Clustered Cues Nursing Diagnosis Rationale Outcome Criteria Nursing Interventions Rationale EvaluationCLEMENT, EUGENE CHADNo ratings yet
- NCP Drug StudyDocument5 pagesNCP Drug StudyAndrea JoyaNo ratings yet
- GRP 3 2 Renal Nephrectomy NCPDocument6 pagesGRP 3 2 Renal Nephrectomy NCPPam RomeroNo ratings yet
- Activity. Module 3 Lesson 1Document5 pagesActivity. Module 3 Lesson 1NightyNo ratings yet
- Nusing CareplanDocument3 pagesNusing Careplanardec_143No ratings yet
- Finals NCMB418Document24 pagesFinals NCMB418Jiro MarianoNo ratings yet
- Nursing Assessment - Pediatric Clients in The Community New 1 1Document7 pagesNursing Assessment - Pediatric Clients in The Community New 1 1Ugalde AlyssakyleNo ratings yet
- Pain Care PlanDocument18 pagesPain Care Planjordanw0613No ratings yet
- NCP Proper CholecystectomyDocument2 pagesNCP Proper CholecystectomyGail Lian SantosNo ratings yet
- Nursing Care Plan: Risk For Ineffective Airway Clearance Related To Bleeding From Tonsillectomy Short TermDocument4 pagesNursing Care Plan: Risk For Ineffective Airway Clearance Related To Bleeding From Tonsillectomy Short TermErika Danalle ArceoNo ratings yet
- Concept Map 2Document3 pagesConcept Map 2John DoeNo ratings yet
- Filipino Culture and BeliefsDocument20 pagesFilipino Culture and BeliefsYeona BaeNo ratings yet
- Sbar Template Staff To StaffDocument2 pagesSbar Template Staff To Staffrafikakurniati6100% (2)
- NU 120 Skin Integrity - Care - PlanDocument4 pagesNU 120 Skin Integrity - Care - Planmrsfelic08100% (3)
- Nursing Care Plan2Document3 pagesNursing Care Plan2gaeLtorvzNo ratings yet
- Pain Management ChecklistDocument2 pagesPain Management ChecklistLyka Dimayacyac100% (2)
- Research ProposalDocument22 pagesResearch ProposalKapil LakhwaraNo ratings yet
- NCM 112 Computation 2021Document3 pagesNCM 112 Computation 2021Marie Kelsey Acena Macaraig100% (1)
- Impaired Physical Mobility...Document3 pagesImpaired Physical Mobility...Christy BerryNo ratings yet
- N375 Critical Thinking Activity ExampleDocument6 pagesN375 Critical Thinking Activity ExamplefaizaNo ratings yet
- Diet: Bath: ActivityDocument2 pagesDiet: Bath: ActivityKristian Karl Bautista Kiw-isNo ratings yet
- NURSING CARE PLAN For TB 2003Document6 pagesNURSING CARE PLAN For TB 2003Princess Andrea Bulatao100% (1)
- Chapter 6 - MCNDocument2 pagesChapter 6 - MCNPrincess Queenie OlarteNo ratings yet
- Disharge Plan Patient'S Outcome Criteria Nursing OrderDocument2 pagesDisharge Plan Patient'S Outcome Criteria Nursing OrderDianne Loregas SanchezNo ratings yet
- NCP Charm EditedDocument6 pagesNCP Charm EditedampogeNo ratings yet
- Nursing Care Plan: Name: DRT Age: 67 Diagnosis: Cva 2° To HPNDocument3 pagesNursing Care Plan: Name: DRT Age: 67 Diagnosis: Cva 2° To HPNKristina Marie Parulan RnNo ratings yet
- NCM 116 SIDEnotes LeonorasDocument10 pagesNCM 116 SIDEnotes LeonorasChrizzha Mae Eredera EredianoNo ratings yet
- Actual SoapiesDocument8 pagesActual SoapiesBeverlyn AsparoNo ratings yet
- Course Module Course Unit Week: Bachelor of Science in Nursing NCMB 311 (Nursing Research 1)Document8 pagesCourse Module Course Unit Week: Bachelor of Science in Nursing NCMB 311 (Nursing Research 1)Jordz PlaciNo ratings yet
- Nursing Care PlanDocument7 pagesNursing Care PlanRhitzle Ann100% (1)
- NCPDocument4 pagesNCPShella CondezNo ratings yet
- Module 2 - Case 1Document9 pagesModule 2 - Case 1Joselyn M. LachicaNo ratings yet
- PNS Pain Management Guideline For Nursing CompetencyDocument10 pagesPNS Pain Management Guideline For Nursing Competencyvhon100% (1)
- Nursing Care PlanDocument6 pagesNursing Care PlanChesca MejiaNo ratings yet
- Nursing Care PlanDocument8 pagesNursing Care PlanssucbotNo ratings yet
- Nursing Health HistoryDocument25 pagesNursing Health HistoryAnthony Aquino EstacioNo ratings yet
- Imbalnce Nutrition Less Than Body RequirementsDocument3 pagesImbalnce Nutrition Less Than Body RequirementselheezaNo ratings yet
- College of Nursing Nursing Care PlanDocument3 pagesCollege of Nursing Nursing Care PlanteuuuuNo ratings yet
- Care Plan - Chronic PainDocument4 pagesCare Plan - Chronic Painapi-246639896No ratings yet
- Concept Map - Surgical GroupDocument25 pagesConcept Map - Surgical GroupIan ChristianNo ratings yet
- Pontine BleedingDocument99 pagesPontine BleedingJeffrey Dela CruzNo ratings yet
- NCPDocument6 pagesNCPNik Rose ElNo ratings yet
- Monitoring An IV Site and InfusionDocument4 pagesMonitoring An IV Site and InfusionAlex Cacayan CortinaNo ratings yet
- Patient Education: by Dr. Nadia BassuoniDocument32 pagesPatient Education: by Dr. Nadia Bassuoniاسامة محمد السيد رمضانNo ratings yet
- Nursing Care Plan: Assessment Diagnosis Inference Goal Intervention Rationale EvaluationDocument4 pagesNursing Care Plan: Assessment Diagnosis Inference Goal Intervention Rationale EvaluationSugar Capule - ManuelNo ratings yet
- NCP For Acute Pain EBPDocument3 pagesNCP For Acute Pain EBPKim LegastoNo ratings yet
- Nursing Care Plan - MergedDocument13 pagesNursing Care Plan - MergedJuls Flares SycaycoNo ratings yet
- Name: Korina A. Rabadon BSN 3-A1 Sas 10Document1 pageName: Korina A. Rabadon BSN 3-A1 Sas 10Sunny Mae Tura PuigNo ratings yet
- NCP Case Analysis GastritisDocument7 pagesNCP Case Analysis GastritisSteffi GolezNo ratings yet
- Nursingcribcom Nursing Care Plan Spinal Cord InjuryDocument2 pagesNursingcribcom Nursing Care Plan Spinal Cord InjuryJanine Erika Julom Brillantes100% (1)
- Brain Infarction NCPDocument3 pagesBrain Infarction NCPJasmn DingleNo ratings yet
- School of Health and Allied Health Sciences Nursing Department Self-Directed Learning (Nur 146 - Clinical Area)Document3 pagesSchool of Health and Allied Health Sciences Nursing Department Self-Directed Learning (Nur 146 - Clinical Area)Duchess Juliane Jose MirambelNo ratings yet
- Subjective:: Assessment Diagnosis Planning Implementation Rationale EvaluationDocument2 pagesSubjective:: Assessment Diagnosis Planning Implementation Rationale EvaluationAyra PunzalanNo ratings yet
- Ventricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandVentricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- The Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeFrom EverandThe Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeRating: 4.5 out of 5 stars4.5/5 (2)
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- Today: Hawaiian Sun Shines On AAOMS 89th Annual MeetingDocument18 pagesToday: Hawaiian Sun Shines On AAOMS 89th Annual MeetingDavid PaloNo ratings yet
- Essentials in Cardiothoracic Surgery Management of Pneumothorax and Bullous Disease For SCRIBDDocument92 pagesEssentials in Cardiothoracic Surgery Management of Pneumothorax and Bullous Disease For SCRIBDPunnarerk ThongcharoenNo ratings yet
- PBQ Scoring KeyDocument1 pagePBQ Scoring KeyWendi ChinchayanNo ratings yet
- Articaine in Oral SurgeryDocument19 pagesArticaine in Oral SurgeryAimeeNo ratings yet
- Augmented Virtual and Mixed Reality in Spinal SurgDocument12 pagesAugmented Virtual and Mixed Reality in Spinal SurgSupriya PoudelNo ratings yet
- Veterinary Surgery ThesisDocument6 pagesVeterinary Surgery Thesislbbzfoxff100% (2)
- CS Form No. 6, Revised 2020 (Application For Leave) (Fillable)Document3 pagesCS Form No. 6, Revised 2020 (Application For Leave) (Fillable)Gemma LuceroNo ratings yet
- Complications of Exodontia: A Retrospective Study: Riginal EsearchDocument6 pagesComplications of Exodontia: A Retrospective Study: Riginal EsearchrahulNo ratings yet
- 1602 Essentia Brochure WebDocument8 pages1602 Essentia Brochure WebVân UyểnhNo ratings yet
- Basic Set Mosquito Kelly Curves Allis Babcock Needle Holder Tissue Forcep Thumb Forcep Army Navy Kidney Basin Towel Clips Straight Clamp MixterDocument14 pagesBasic Set Mosquito Kelly Curves Allis Babcock Needle Holder Tissue Forcep Thumb Forcep Army Navy Kidney Basin Towel Clips Straight Clamp MixterZeng SolomonNo ratings yet
- Oral and Throat CancerDocument28 pagesOral and Throat CancerPerly PeterNo ratings yet
- Surgical Site MarkingDocument16 pagesSurgical Site Markingalejandrino_leoaugustoNo ratings yet
- Final List EMP 01.02.2022Document34 pagesFinal List EMP 01.02.2022Gulshan NaddaNo ratings yet
- MSC (N) SyllabusDocument246 pagesMSC (N) SyllabussabeethuNo ratings yet
- Multiple Colonic Injuries: For Grading and Universal Management PlanDocument3 pagesMultiple Colonic Injuries: For Grading and Universal Management PlanFelix JeoNo ratings yet
- Plastic, Reconstructive, and Cosmetic Procedures: Skin GraftsDocument7 pagesPlastic, Reconstructive, and Cosmetic Procedures: Skin GraftsRiza Angela BarazanNo ratings yet
- SENSUS Digestive 23 SeptDocument4 pagesSENSUS Digestive 23 Septryan nugrohoNo ratings yet
- Lasers in Implant Dentistry: Jon JulianDocument24 pagesLasers in Implant Dentistry: Jon JulianElena DimitriuNo ratings yet
- Intussusception in Children - UpToDateDocument45 pagesIntussusception in Children - UpToDateyalexNo ratings yet
- A Family Case Presentation, SLHDocument27 pagesA Family Case Presentation, SLHRajanNo ratings yet
- Drain's PeriAnesthesia Nursing: A Critical Care Approach., 978-1437718942Document23 pagesDrain's PeriAnesthesia Nursing: A Critical Care Approach., 978-1437718942vivienepeskoffkfz93% (14)
- The Influence of Malocclusion On Masticatory Performance A Systematic Review-Magalhaes IB Et AlDocument7 pagesThe Influence of Malocclusion On Masticatory Performance A Systematic Review-Magalhaes IB Et AlAnggiswariNo ratings yet
- Receiving and PositioningDocument45 pagesReceiving and PositioningCHALIE MEQUNo ratings yet
- UnderstandingAnesthesia1 1 2345Document144 pagesUnderstandingAnesthesia1 1 2345Manaswini SahuNo ratings yet
- Rehabilitation Following Partion Glossectomy and Neck DissectionDocument10 pagesRehabilitation Following Partion Glossectomy and Neck DissectionnotmelbrooksNo ratings yet
- FB Abb 61680000000Document6 pagesFB Abb 61680000000Iqbal HarzikyNo ratings yet
- Common Questions Asked in The MRCS Viva Examination PDFDocument4 pagesCommon Questions Asked in The MRCS Viva Examination PDFWael Shoabe100% (1)
- Psychological Issues in Paediatric SurgeryDocument8 pagesPsychological Issues in Paediatric SurgeryemagistNo ratings yet
- AHRQ Safety Program For Surgery: Antibiotic Audit ToolDocument10 pagesAHRQ Safety Program For Surgery: Antibiotic Audit ToolCarissa SulaimanNo ratings yet
- The Accuracy of Digital Templating in Uncemented Total Hip ArthroplastyDocument6 pagesThe Accuracy of Digital Templating in Uncemented Total Hip Arthroplastyson leNo ratings yet