Fact Sheet PediatricAPTA Motor Development Variations Across Cultures
Fact Sheet PediatricAPTA Motor Development Variations Across Cultures
Uploaded by
Juan Ignacio Gómez IruretagoyenaCopyright:
Available Formats
Fact Sheet PediatricAPTA Motor Development Variations Across Cultures
Fact Sheet PediatricAPTA Motor Development Variations Across Cultures
Uploaded by
Juan Ignacio Gómez IruretagoyenaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Fact Sheet PediatricAPTA Motor Development Variations Across Cultures
Fact Sheet PediatricAPTA Motor Development Variations Across Cultures
Uploaded by
Juan Ignacio Gómez IruretagoyenaCopyright:
Available Formats
FACT SHEET
Motor Development Variations Across Cultures: Implications for Culturally Competent
and Family-Centered Pediatric Care
WHAT IS CULTURE?
The United States Department of Health and Human Services Office of Minority Health defines culture
as “integrated patterns of human behavior that include the language, thoughts, communications,
actions, customs, beliefs, values, and institutions of racial, ethnic, religious, or social groups.”1 Culture
has also been defined as “the learned and shared beliefs, values, and life ways of a designated or
particular group which are generally transmitted intergenerationally and influence one's thinking and
action modes.” 2
Culture is one of the many variables known to affect motor development. These variables include but
are not limited to climate,3 sex,4 early postural experience,5,6 socioeconomic status,7 nutrition,8 physical
growth,9 childrearing practices,10 and parental expectations.11
Because the concept of culture is multifaceted, this fact sheet will focus on cultural variations in motor
development as they relate to culture-based caregiving practices, routines, and parental beliefs across
different racial/ethnic groups.
WHY IS THIS IMPORTANT?
• The child population of the USA is expected to experience the majority–minority crossover in
2020.12
• By 2030, children from racial/ethnic minorities will account for more than half of the US
population under the age of 18 years.13
• By 2060, 64% of children in the USA will belong to racial and ethnic minorities compared with
56% for the total population, and nearly one in five of the nation’s total population will be foreign-
born.12
As the US child population continues to grow increasingly diverse, pediatric physical therapists must
carefully consider the child/family’s cultural background and caregiving practices when assessing
infants and children, establishing a plan of care, developing goals, and administering skilled
intervention.
CULTURE AND MOTOR DEVELOPMENT
Evidence from cross-cultural research has challenged the assumption that motor development follows a
fixed and predictable sequence.14 Culture-based variations in gross motor development have been
documented in populations around the world. The following examples in Table 1 illustrate some of
these differences and encourage a more flexible view of motor development milestones. These
examples are not all-inclusive of the current body of cross-cultural studies and should not be used to
make generalizations regarding a family’s caregiving practices or expectations regarding their child’s
development.
2018
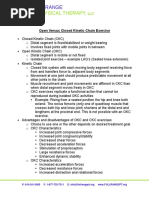
TABLE 1: Culture-Based Variations in Gross Motor Development*
What? Documented Reasons Why
Higher percentage of independent sitting in 5- Emphasis on upright positioning and opportunities
month-old infants living in Cameroon and Kenya for practicing sitting during daily activities15
compared to 5-month-old infants living in Argentina,
Italy, South Korea, and the US15
Gross motor acceleration in infants living in - Culture-based handling practices:
Jamaica,16,17 Kenya,18,19 Mali,20 Nigeria,21 and 1. Aggressive massage applied to infants with low
Uganda22,23 tone11
2. Traction applied to infants’ head and limbs for
stretching11
- Culture-based positioning practices:
1. Infants living in Africa carried in slings with little to
no head support while mothers work in the field14
2. African infants propped into sitting and walking
positions by parents19,20
- Cultural belief/value that walking promotes a child’s
integration into their society and fosters
interdependence11
Skipping of crawling by infants living in Jamaica16,17 Cultural belief/perception that crawling is primitive
and demeaning.16,17 In contrast, crawling on hands
and knees is valued in European and American
cultural groups as it promotes early independence
with mobility24
Delayed onset of gross motor milestones in infants - Predominance of supine positioning during wakeful
living in China and Japan as compared to infants moments in Eastern Asian countries25,26,27
living in Western countries25,26 - Practice of “sandbags” for infant toileting in
Northern China: infants spend more than 16 hours
per day lying supine inside a small sleeping bag
filled with fine sand26
- Infants tend to be dressed in heavy clothing, which
may limit movement exploration28
-
Infants living in Hong Kong learn to roll supine to Preference for supine positioning during the day,
prone before they roll from prone to supine, the resulting in decreased opportunities for practice of
opposite of what is observed in Western cultures27 antigravity postural control27
Slowest rate of human development in The Ache Independent mobility is perceived as dangerous
group in Paraguay, a hunter-gatherer society11,14 and is therefore discouraged by parents11,14
*not all-inclusive of cross-cultural research literature
2018 APTA Pediatrics Fact Sheets | 2
IMPLICATIONS FOR PHYSICAL THERAPISTS
• Infants from certain cultural groups may follow unique motor development trajectories due to culture-
specific caregiving practices or cultural values/beliefs.29
• Using standardized motor development screening and assessment tools to evaluate the motor
development of children in cultures other than those in which the normative samples were established
may lead to misinterpretation of results and erroneous labelling of young children a developmentally
delayed or “early achieving.” 29
o New population norms and cross-cultural adaptations for commonly used standardized motor
development screening and assessment tools are available for many cultural contexts. 29
• It is common for families to retain their culture-specific caregiving practices when they immigrate to a
different country. A child born in the US to parents raised in another country may be raised using
culture-specific handling and positioning practices of the parents’ country. 30
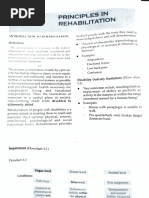
CULTURALLY COMPETENT CARE AND FAMILY-CENTERED PEDIATRIC CARE:
PUT ON YOUR THINKING CAP!
Evaluation
-Do the "delays" I identified
Examination during my examination
reflect a true developmental Diagnosis /
History delay or a culture- or family- Prognosis/ Plan of
-Do I know enough about this specific difference? Care
family's caregiving routines? -Can my client/patient's poor
-Do the family's caregiving
-Are there cultural values or performance on certain test
practices contribute to my
beliefs that may affect this items be explained by lack of
examination findings as they
family's perception of their familiarity with or exposure
relate to my client's motor
child's development? to testing objects?
development? Are these
-Do I know what is important practices strengths or potential
to this family? Do I know the barriers to my plan of care?
parents' priorities? -Have I considered using goal-
Tests and Measures setting tools to focus on what
Intervention is important to this
-Is the motor development
screening/assessment tool I Parent/caregiver child/family?
am using valid for children education: -Am I approaching goal setting
from this cultural background? -Have I explainted how as a collaborative effort
-Are there cross-cultural culture- and family-specific between myself, the
adaptations of standardized caregiving, handling and child/family and other
motor development positioning practices may disciplines involved in this
assessments appropriate for affect motor development? child's care?
this client/patient's cultural Treatment Strategies
background?
-Do my interventions
incorporate culture-specific
practices that are important
to the family and child?
DON’T ASSUME that family’s adhere to cultural norms
ASK PARENTS/CAREGIVERS: What do you consider important to your child/family?
2018 APTA Pediatrics Fact Sheets | 3
REFERENCES
1. US Department of Health and Human Services Office of Minority Health. Assuring cultural competence
in health care: recommendations for national standards and outcomes-focused research agenda.
Washington, DC: US Government Printing Office; 2000.
2. Pasick RJ, D'Onofrio CN, Otero-Sabogal R. Similarities and differences across cultures: questions to
inform a third generation for health promotion research. Health Educ Q. 1994;23(suppl):S142-61.
3. Tronick EZ, Thomas RB, Daltabuit M. The Quechua manta pouch: a caretaking practice for buffering the
Peruvian infant against the multiple stressors of high altitude. Child Dev. 1994;65:1005-13.
4. Goodway JD, Robinson LE, Crowe H. Gender differences in fundamental motor skill development in
disadvantaged preschoolers from two geographical regions. Res Q Exerc Sport. 2010;81:17-24.
5. Lobo MA, Galloway JC. Enhanced handling and positioning in early infancy advances development
throughout the first year. Child Dev. 2012;83:1290-1302.
6. Lee HM, Galloway JC. Early intensive postural and movement training advances head control in very
young infants. Phys Ther. 2012;92:935-47.
7. McPhillips M, Jordan-Black J. The effect of social disadvantage on motor development in young children:
a comparative study. J Child Psychol Psychiatr. 2007;48:1214-22.
8. Sudfeld CR, McCoy DC, Fink G, et al. Malnutrition and its determinants are associated with suboptimal
cognitive, communication, and motor development in Tanzanian children. J Nutr. 2015;145:2705-14.
9. Thelen E, Fisher DM, Ridley-Johnson R. The relationship between physical growth and a newborn
reflex. Infant Behav Dev. 2002;25:72-85
10. Kolobe TH. Childrearing practices and developmental expectations for Mexican-American mothers and
the developmental status of their infants. Phys Ther. 2004;84:439-53.
11. Cintas HL. Cross-cultural similarities and differences in development and the impact of parental
expectations on motor behavior. Pediatr Phys Ther. 1995;7:103-11.
12. Colby SL, Ortoman JM. Projection of the size and composition of the U.S. population: 2014 to 2060. US
Census Bureau 2015. Retrieved from:
https://www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf. Accessed
August 2015.
13. Perez DA, Hirschman C. The Changing racial and ethnic composition of the US population: emerging
American identities. Popul Dev Rev. 2009;35(1):1-51.
14. Adolph KE, Karasik L, Tamis-LeMonda CS. Motor skill. In Bernstein M, editor. Handbook of Cultural
Developmental Science. New York: Taylor & Francis, 2010:61-88.
15. Karasik L, Tamis-LeMonda CS, Adolph KE, Bornstein MH. Places and postures: a cross- cultural
comparison of sitting in 5-month-olds. J Cross Cult Psychol. 2015;46(8):1023-1038.
16. Hopkins B, Westra T. Motor development, maternal expectations, and the role of handling. Infant Behav
Dev. 1990;13:117-22.
17. Hopkins B, Westra T. Maternal expectations of their infants’ development: some cultural differences. Dev
Med Child Neurol. 1989;31:384-90.
18. Keefer CH, Tronick E, Dixon S, Brazelton TB. Specific differences in motor performance between Gusii
and American newborns and a modification of the Neonatal Behavioral Assessment Scale. Child Dev.
1982;53:754-9.
19. Super CM. Environmental effects on motor development: the case of African infant precocity. Dev Med
Child Neurol. 1976;18:561-7.
20. Bril B, Sabatier C. The cultural context of motor development: postural manipulations in the daily life of
Bambara babies (Mali). Int J Behav Dev. 1986;9:439-53.
21. Iloeje SO, Obiekwe VU, Kaine WN. Gross motor development of Nigerian children. Ann Trop Paediatr.
1991;11:33-9.
2018 APTA Pediatrics Fact Sheets | 4
22. Geber M. The psycho-motor development of African children in the first year, and the influence of
maternal behavior. J Soc Psychol. 1958;47:185-95.
23. Geber M, Dean RFA. Gesell Tests on African children. Pediatrics. 1957;20:1055-65.
24. Benson, JB. The significance and development of crawling in human infancy. In: Clark JE, Humphrey
JH, editors. Advances in Motor Development Research, Volume 3. New York: AMS Press; 1990:91-142.
25. Werner EE. Infants around the world: cross-cultural studies of psychomotor development from birth to
two years. J Cross-Cultural Psychol. 1972;3:111-134.
26. Mei, J. The Northern Chinese custom of rearing babies in sandbags: implications for motor and
intellectual development. In: vanRossum, J.; Laszlo, J., editors. Motor development: Aspects of Normal
and Delayed Development. Amsterdam: VU Uitgeverij; 1994.
27. Nelson ES, Yu LM, Wong D, Wong HYE, Yim L. Rolling over in infants: age, ethnicity, and cultural
differences. Dev Med Child Neurol. 2004;46:706-9.
28. Fung KP, Lau SP. Denver Developmental Screening Test: cultural variables. J Pediatr. 1985:106:343.
29. Mendonça B, Sargent B, Fetters L. The cross-cultural validity of standardized motor development
screening and assessment tools: a systematic review. Dev Med Child Neurol. 2016; 58(12):1213-1222.
30. Inman AG, Howard EE, Beaumont RL, Walker JA. Cultural transmission: Influence of contextual factors
in Asian Indian immigrant parents’ experiences. J Couns Psychol. 2007; 54: 93–100.
ADDITIONAL CULTURAL COMPETENCY RESOURCES
• APTA Cultural Competence in Physical Therapy Available at: https://www.apta.org/patient-care/public-
health-population-care/cultural-competence
• APTA Resources for Teaching Cultural Competence in Physical Therapy Education Available at: https://
www.apta.org/patient-care/public-health-population-care/cultural-competence/teaching-cultural-
competence
• Campinha-Bacote J. The process of cultural competence in the delivery of healthcare services: a model
of care. Journal of Transcultural Nursing. 2002;13(3):181-184.
• National Standards for Culturally and Linguistically Appropriate Services (CLAS) in Health and Health
Care Available at: https://thinkculturalhealth.hhs.gov/assets/pdfs/EnhancedNationalCLASStandards.pdf
• Setting the Agenda for Research in Cultural Competence in Health Care Available at:
https://archive.ahrq.gov/research/findings/factsheets/literacy/cultural/cultural.html
©2018 by the APTA Academy of Pediatric Physical Therapy,1020 N Fairfax St, Suite 400, Alexandria, VA
22314-1488, www.pediatricapta.org
Developed by expert contributor Bianca Mendonça, PT, DPT, Board-Certified Pediatric Clinical
Specialist. Supported by the Fact Sheet Committee of APTA Pediatrics.
The APTA Academy of Pediatric Physical Therapy provides access to these member-produced fact
sheets and resources for informational purposes only. They are not intended to represent the position
of APTA Pediatrics or of the American Physical Therapy Association.
2018 APTA Pediatrics Fact Sheets | 5
You might also like
- Functional Training Handbook (PDFDrive) (001-153)Document153 pagesFunctional Training Handbook (PDFDrive) (001-153)ssa.ptrainer100% (1)
- Vdoc - Pub The Muscular System Manual The Skeletal Muscles of The Human BodyDocument803 pagesVdoc - Pub The Muscular System Manual The Skeletal Muscles of The Human BodyNguyễn Thế Cường100% (14)
- Group 2 PPT RawDocument25 pagesGroup 2 PPT RawGil Sunpayco Jr.No ratings yet
- Childrearing Practices: Creating Programs Where Traditions and Modern Practices MeetDocument69 pagesChildrearing Practices: Creating Programs Where Traditions and Modern Practices MeetJayjeet BhattacharjeeNo ratings yet
- Transcultural Perspectives in The Nursing Care of ChildrenDocument23 pagesTranscultural Perspectives in The Nursing Care of Childrenceanbae.patajoNo ratings yet
- Transcultural Perspectives in The Nursing Care of Children (1) - MergedDocument81 pagesTranscultural Perspectives in The Nursing Care of Children (1) - Mergedceanbae.patajoNo ratings yet
- Children in A Culturally Diverse Society-ReportingDocument7 pagesChildren in A Culturally Diverse Society-ReportingyanduyoNo ratings yet
- Ethical Dilemmas: Feeding Children in Early Care and Learning SettingsDocument3 pagesEthical Dilemmas: Feeding Children in Early Care and Learning SettingsMishael AbogadoNo ratings yet
- Week 14 MCHNDocument5 pagesWeek 14 MCHNCyrille Kibbz DonatoNo ratings yet
- WCE - Inclusive Education RemymarDocument42 pagesWCE - Inclusive Education RemymarRemymar AnisNo ratings yet
- Pediatric ReviewerDocument3 pagesPediatric ReviewereannnicholleNo ratings yet
- CPP ManualDocument63 pagesCPP ManualLady Lyn NarsolesNo ratings yet
- Ob2 Sas 40Document7 pagesOb2 Sas 40????No ratings yet
- Final Hearth Book - PDF - CORE GroupDocument199 pagesFinal Hearth Book - PDF - CORE GroupRavishka Gunathilake100% (1)
- NAEYC Code PDFDocument4 pagesNAEYC Code PDFRoxana GhiațăuNo ratings yet
- IYCF - UNICEF Infant and Young Child Feeding Counselling Cards For Community WorkersDocument31 pagesIYCF - UNICEF Infant and Young Child Feeding Counselling Cards For Community WorkersJewelle Anne Estanilla LimenNo ratings yet
- Counselling_CardsDocument31 pagesCounselling_Cardsjulieannemanalo22No ratings yet
- Parental ChildDocument9 pagesParental ChildFadia Talia Salsabila HerviNo ratings yet
- Roles of A Child Development AssistantDocument1 pageRoles of A Child Development AssistantAngelica TronoNo ratings yet
- WK14 - Nursing Process for Promotion of Normal Growth and DevelopmentDocument4 pagesWK14 - Nursing Process for Promotion of Normal Growth and DevelopmentIanne InoueNo ratings yet
- Te Whāriki: He Whāriki Mātauranga Mō Ngā Mokopuna o Aotearoa: Early Childhood CurriculumDocument6 pagesTe Whāriki: He Whāriki Mātauranga Mō Ngā Mokopuna o Aotearoa: Early Childhood CurriculumIdol YoNo ratings yet
- YCFPDocument8 pagesYCFPMuskan ChadhaNo ratings yet
- Material Assessing children and young people health - Copy (2)Document42 pagesMaterial Assessing children and young people health - Copy (2)sesaeedhaniyah.dNo ratings yet
- Parental CareDocument2 pagesParental Care0-benk-0No ratings yet
- Developmental MilestoneDocument17 pagesDevelopmental MilestoneRafael MarvinNo ratings yet
- Project NajaDocument13 pagesProject NajaNatasha Jean CardonaNo ratings yet
- Focus On Child Health PDFDocument28 pagesFocus On Child Health PDFAbhishekNo ratings yet
- The Role of Schools in Preventing OverweightDocument11 pagesThe Role of Schools in Preventing Overweightceles83No ratings yet
- Summary OutlineDocument3 pagesSummary OutlineVy NguyễnNo ratings yet
- Savaliya Hiren - Ex.1Document7 pagesSavaliya Hiren - Ex.1Hiren SavaliyaNo ratings yet
- The Unstable Future and Health of The Youth Due To PovertyDocument3 pagesThe Unstable Future and Health of The Youth Due To PovertyOccasus DeirdreNo ratings yet
- Children and Young People's Nursing: A Philosophy of Care: Guidance For Nursing StaffDocument8 pagesChildren and Young People's Nursing: A Philosophy of Care: Guidance For Nursing Staffandreicmarin1981No ratings yet
- MATERNAL AND CHILD HEALTH NURSING SUMMARY Chapter 30-34 (Adelle Pillitteri)Document134 pagesMATERNAL AND CHILD HEALTH NURSING SUMMARY Chapter 30-34 (Adelle Pillitteri)CHRISTIE MONTANO100% (6)
- Go Baby GoDocument4 pagesGo Baby GobremuselNo ratings yet
- Pdhpe 7-10-2024 Parent and Carer GuideDocument2 pagesPdhpe 7-10-2024 Parent and Carer GuideAli MohammedNo ratings yet
- Bianka Part 2Document10 pagesBianka Part 2api-85429702No ratings yet
- H. Nursing Care Plan: Altered Parenting RoleDocument2 pagesH. Nursing Care Plan: Altered Parenting RoleClovie ArsenalNo ratings yet
- Palestine Case StudyDocument12 pagesPalestine Case StudyBashaer Abu KhadejaNo ratings yet
- Family With An Infant (Group 3)Document12 pagesFamily With An Infant (Group 3)Jessa Mae OhaoNo ratings yet
- Pediatrics 2008 High E1008 15Document10 pagesPediatrics 2008 High E1008 15Nanda Asyura RizkyaniNo ratings yet
- 120 m6Document26 pages120 m6k5gphk5pyxNo ratings yet
- Developmentally Appropriate Practice and Its Implication To K 12 (J. Ramos)Document54 pagesDevelopmentally Appropriate Practice and Its Implication To K 12 (J. Ramos)Lily Flores GauiranNo ratings yet
- Document From GreatDocument15 pagesDocument From GreatTaif SalimNo ratings yet
- Prioritizing Nutrition and Feeding in Alternative Care 1Document13 pagesPrioritizing Nutrition and Feeding in Alternative Care 1mehwishfarooq729No ratings yet
- Developmental MilestonesDocument17 pagesDevelopmental MilestonesSardono WidinugrohoNo ratings yet
- 11. Role of Nurses in Family welfare servicesDocument20 pages11. Role of Nurses in Family welfare servicesSWATHY P PNo ratings yet
- Adoption Literature ReviewDocument45 pagesAdoption Literature Reviewdanielalagrimas1No ratings yet
- The Positive Parent Raising Healthy Happy and Successful Children Birth Adolescence PDFDocument265 pagesThe Positive Parent Raising Healthy Happy and Successful Children Birth Adolescence PDFSyibly Avivy A. MulachelaNo ratings yet
- teams-IND-Nutrition-Knowledge@UNICEF (Nutrition) - UNICEF Reports-2024 Social Protection For Nutrition India A Proposed Framework-5.0Document14 pagesteams-IND-Nutrition-Knowledge@UNICEF (Nutrition) - UNICEF Reports-2024 Social Protection For Nutrition India A Proposed Framework-5.0proyecto223327No ratings yet
- 2018 Perceptions of Childcare SPMDocument9 pages2018 Perceptions of Childcare SPMDori OrtNo ratings yet
- Transes PHNDocument24 pagesTranses PHNimjuuNo ratings yet
- 06 Abr 09Document44 pages06 Abr 09plucichNo ratings yet
- ANEMIA Group LEARNING PROJECTDocument32 pagesANEMIA Group LEARNING PROJECTScribdTranslationsNo ratings yet
- Children Left BehindDocument10 pagesChildren Left BehindЛена ЩербинаNo ratings yet
- Study Guide 7 - Transcultural Perspectives in The Nursing Care of ChildrenDocument3 pagesStudy Guide 7 - Transcultural Perspectives in The Nursing Care of ChildrenTim john louie RancudoNo ratings yet
- Maece 202 Part 1Document47 pagesMaece 202 Part 1Khristine DusayenNo ratings yet
- African Socialization Goals Practices AnDocument63 pagesAfrican Socialization Goals Practices AnAngela AmoatwoNo ratings yet
- 658-Article Text-26098-2-10-20220428Document13 pages658-Article Text-26098-2-10-20220428Chloe SumalinogNo ratings yet
- Disability Awareness InfographicDocument3 pagesDisability Awareness Infographicapi-531068426No ratings yet
- Parenting Styles Decoded: Finding What Works Best for Your FamilyFrom EverandParenting Styles Decoded: Finding What Works Best for Your FamilyNo ratings yet
- Empowering Parents & Teachers: How Parents and Teachers Can Develop Collaborative PartnershipsFrom EverandEmpowering Parents & Teachers: How Parents and Teachers Can Develop Collaborative PartnershipsNo ratings yet
- OKC Vs CKC ExercisesDocument2 pagesOKC Vs CKC Exercises杨钦杰No ratings yet
- Scientific Principles of Sports RehabilitationDocument12 pagesScientific Principles of Sports RehabilitationRAJESH MALIKNo ratings yet
- Joselito Melendez CV 2 2Document2 pagesJoselito Melendez CV 2 2joselitomelendez9No ratings yet
- Resume 2023Document2 pagesResume 2023api-547385390No ratings yet
- Canada Books ReferanceDocument3 pagesCanada Books ReferanceRamkumar MurugesanNo ratings yet
- англійська 28.09.23Document1 pageанглійська 28.09.23ol.oleksandrivnaNo ratings yet
- Ankita KothariDocument5 pagesAnkita Kothariankita kothariNo ratings yet
- Sarhad University of Science & Information Technology, PeshawarDocument3 pagesSarhad University of Science & Information Technology, Peshawarkhan khanNo ratings yet
- Physical Rehabilitation Assessment MBBS5 2024Document3 pagesPhysical Rehabilitation Assessment MBBS5 2024mahfuza aliNo ratings yet
- Instant Download Canine Rehabilitation and Physical Therapy 1st Edition Darryl Millis Ms DVM PDF All ChapterDocument78 pagesInstant Download Canine Rehabilitation and Physical Therapy 1st Edition Darryl Millis Ms DVM PDF All Chapterwetalagacia100% (3)
- Sports Medicine Meets Musculoskeletal MeDocument3 pagesSports Medicine Meets Musculoskeletal MeMotea IoanaNo ratings yet
- Exploration of The History of PhysiotherapyDocument5 pagesExploration of The History of PhysiotherapyÑítíßh ÑíràlàNo ratings yet
- SIRA NumberDocument2 pagesSIRA NumberrianabeggNo ratings yet
- Assignment No. 13 - PCAMDocument1 pageAssignment No. 13 - PCAMMIPZI GAIL SILVANo ratings yet
- Defensible Documentation Quick ReferenceDocument3 pagesDefensible Documentation Quick ReferencecderdnaseNo ratings yet
- PSM RehabilitationDocument19 pagesPSM RehabilitationshivaniNo ratings yet
- Making Vision 2020 A Reality: Ben F Massey, JR, PT, MADocument4 pagesMaking Vision 2020 A Reality: Ben F Massey, JR, PT, MA杨钦杰No ratings yet
- Syllabus MPT 1 YrDocument38 pagesSyllabus MPT 1 YrShubham ChopadeNo ratings yet
- Spatial Temporal Parameters, Pelvic and Lower Limb Movements During Gait in Individuals With Reduced Passive Ankle DorsiflexionDocument7 pagesSpatial Temporal Parameters, Pelvic and Lower Limb Movements During Gait in Individuals With Reduced Passive Ankle DorsiflexionAriene RibeiroNo ratings yet
- Depression and Anxiety Symptoms Among Lebanese Lower Limb Traumatic Amputees Association With Education Employment Adjustment To Amputation and ProDocument15 pagesDepression and Anxiety Symptoms Among Lebanese Lower Limb Traumatic Amputees Association With Education Employment Adjustment To Amputation and ProResearch and Development DepartmentNo ratings yet
- Final Version of SynopsisDocument43 pagesFinal Version of Synopsisahmadalik525No ratings yet
- Evolution Healing Centre - Lived Experiences of Stroke For Bermuda 2022Document22 pagesEvolution Healing Centre - Lived Experiences of Stroke For Bermuda 2022BernewsAdminNo ratings yet
- Physical Therapy Books List (A) 01Document5 pagesPhysical Therapy Books List (A) 01Javed Noor Muhammad GabaNo ratings yet
- PPTX, 10-EffleurageDocument11 pagesPPTX, 10-EffleuragemeachieNo ratings yet
- Acceptedquals Feb 2022 UpdateDocument4 pagesAcceptedquals Feb 2022 UpdateEmma TheobaldNo ratings yet
- Biomechanical and Rehab FORDocument3 pagesBiomechanical and Rehab FORKenny ClayNo ratings yet
- Immediate download Writing Patient Client Notes Ensuring Accuracy in Documentation Fourth Edition Ginge Kettenbach ebooks 2024Document56 pagesImmediate download Writing Patient Client Notes Ensuring Accuracy in Documentation Fourth Edition Ginge Kettenbach ebooks 2024hamdanzaynah28100% (1)
- Scholarships For Physiotherapy StudentsDocument7 pagesScholarships For Physiotherapy Studentsusama jamilNo ratings yet