Fluid and Electrolyte Disturbances
Fluid and Electrolyte Disturbances
Uploaded by
Marie Antionette MondragonCopyright:
Available Formats
Fluid and Electrolyte Disturbances
Fluid and Electrolyte Disturbances
Uploaded by
Marie Antionette MondragonOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Fluid and Electrolyte Disturbances
Fluid and Electrolyte Disturbances
Uploaded by
Marie Antionette MondragonCopyright:
Available Formats
Fluid and Electrolyte
Disturbances Nursing Management
Monitor I&O and daily weights, as ordered
Monitor vital signs; WOF for hypotension and tachycardia
Fluid Imbalances Monitor skin and tongue turgor
Encourage small, frequent sips of oral fluids; Consider likes and
dislikes of patient
Regulate IV fluid to prescribed rate
Hypovolemia Administer medications, as prescribed
Hypovolemia occurs when loss of ECF volume exceeds the intake of
fluid.
It occurs when water and electrolytes are lost in the same proportion
as they exist in normal body fluids
Dehydration- loss of water ONLY
Cause/s:
ABNORMAL FLUID LOSS DECRESED INTAKE
THIRD SPACING
Vomiting Nausea
Edema in burns
Diarrhea Lack of access
Ascites in liver
GI suctioning to fluids
dysfunction
Profuse
diaphoresis
Poor skin turgor seen in hypovolemia
Other causes: Diabetes insipidus, adrenal insufficiency, hyperglycemia,
hemorrhage, coma
Clinical Manifestations “FEWCHART”
F - Flat neck veins
E - Eyes sunken
W- Weight loss
C - Concentrated urine (SG> 1.025, oliguria)
H - Hypotension
A - Anxiety Normal tongue appearance Dry tongue
R - Rapid, weak pulse; Respirations increased
T - Temperature elevated
Medical Management
Fluid replacement therapy
Mild- moderate
Hypervolemia
•Increase oral fluids
•Oral rehydration salts (e.g., Hydrite) Hypervolemia refers to an isotonic expansion of the ECF caused by
Severe the abnormal retention of water and sodium in approximately the
•IV Therapy same proportions in which they normally exist in the ECF.
•If with hypotension, give isotonic fluid Fluid overload
•Once normotensive, give hypotonic fluids
Antidiarrheals, if with diarrhea
•Loperamide (Diatabs)
Antiemetics, if with nausea/vomiting
•Metoclopramide (Plasil)
Hyponatremia develops when:
Causes There is too much water relative to the amount of sodium
Heart failure Too little sodium relative to the amount of water
Kidney injury
Liver cirrhosis
Excessive salt intake
Excessive administration of sodium- containing fluids in patients with
impaired regulatory mechanisms
Clinical Manifestations
Edema
Distended neck veins
Puffy eyelids
Crackles
Weight gain
Hypertension
Bounding pulse Medical Management
Tachypnea, dyspnea Sodium replacement
Increased urine output; dilute urine •Sodium-rich diet for those who can eat and drink
Medical Management •NaCl tablets
Low sodium diet (mild restriction to as low as 250 mg/day) •PLR or PNSS IV infusion, for those who cannot take sodium by
Diuretics mouth
•Thiazide diuretics- mild to moderate hypervolemia Water restriction
•Loop diuretics- severe hypervolemia •Indicated for hyponatremic patients with normal or excess fluid
Potassium supplementation, to prevent hypokalemia while on diuretics volume
Dialysis for severe renal impairment Hypertonic saline solution
•Indicated for severe hyponatremia
Nursing Management Drug Therapy: AVP receptor antagonists “vaptans”
Monitor I&O as ordered MOA: act on AVP receptors in the renal tubules to promote aquaresis
Weigh daily, WOF rapid weight gain (1kg= 1L of fluid) •Conivaptan HCl (Vaprisol) IV- hospitalized patients with moderate to
Monitor breath sounds, especially if with IV therapy severe hyponatremia
Monitor for presence of edema •C/I: seizure, delirium, coma
•Feet and ankles for ambulatory patients •Tolvaptan (Samsca)- oral medication for clinically significant
•Sacral area for bed ridden patients hypervolemic and euvolemic hyponatremia
Encourage bed rest – this favors diuresis Nursing Management
Regulate IVF as prescribed Monitor I&O and daily weights
Place on semi- Fowlers position if with dyspnea Monitor laboratory values
Reposition at regular intervals to prevent pressure ulcers Monitor the progression of manifestations
Emphasize need to read food labels For patients who are able to consume by mouth, encourage foods and
Instruct to avoid foods high in sodium fluids with high sodium content
Encourage use of seasoning substitutes such as lemon juice, onions, •Broth made with one beef cube (900mg)
and garlics •8 oz of tomato juice (700mg)
Administer IV fluids, as prescribed
Electrolyte Imbalances WOF signs of circulatory overload:
•Cough, dyspnea, puffy eyelids, dependent edema, excessive weight
gain in 24 hours, crackles)
Institute safety precautions:
•Keep side rails up
Sodium •Supervised ambulation
Most abundant electrolyte in the ECF Causes: “MODEL”
ECF concentration: 135- 145 mEq/L M - Medications, meals
Functions: O - Osmotic diuretics
•Controls body water distribution D - Diabetes insipidus
•Establishes the electrochemical state necessary for muscle E - Excessive water loss
contraction and nerve impulse transmission L - Low water intake
Hyponatremia
Serum sodium level < 135 mEq/L
Causes:
Vomiting, diarrhea, gastric suctioning
Medications: diuretics, lithium, cisplatin, heparin, and NSAIDs
Decreased aldosterone (Addison’s disease)
Water intoxication
CHF
Chronic renal failure
Clinical Manifestations
Extreme thirst- first sign Potassium
Dry, sticky mucous membranes
Oliguria Neuromuscular irritability
Firm, rubbery turgor
Red, dry, swollen tongue
Restlessness, tachycardia, fatigue In hypokalemia, “everything is low and slow”
Disorientation, hallucination
Medical Management Clinical Manifestations
Lethargy- drowsy and fatigued (early sign)
Safety Alert! Low, shallow respirations
•Serum sodium correction should be done gradually Lethal cardiac dysrhythmias (ST depression, shallow T wave,
prominent U wave)
•Too rapid reduction in sodium level renders the plasma temporarily Lots of urine (frequency and volume)
hypo-osmotic to the brain tissue Leg cramps
Limp muscles
Treat underlying cause Low blood pressure (severe)
Sodium correction Medical Management
•Hypotonic electrolyte solution- first line Potassium-rich diet:
•IV of choice: 0.3% NaCl
•Isotonic non saline solution- second line
•D5 W- indicated when water needs to be replaced without sodium
Medical Management
Provide oral fluids at regular intervals
Restrict sodium in diet, as prescribed
Monitor behavioral changes
Promote safety
Monitor intake and output
Potassium
Most abundant electrolyte in the ICF
Normal serum concentration: 3.5 to 5 mEq/L
Has an inverse relationship with sodium; direct relationship with
magnesium Potassium chloride (KCl)
Functions: Oral supplementation for mild to moderate hypokalemia
•Maintains ICF volume •S/E: small bowel lesions
•Neuromuscular excitability •Assess for abdominal distention, pain or GI bleeding
•Regulates contraction and rhythm of heart IV route for severe hypokalemia (K+ of 2 mEq/L)
•Incorporate in IV bottle, as ordered
•Never give by IV push or direct IV- this causes fatal dysrhythmias
and cardiac arrest
Hypokalemia
Serum Potassium Level <3.5 mEq/L
IV Potassium Chloride
Causes: “SAD BITCH”
S - Starvation Potassium is excreted via kidneys
A - Alkalosis (promotes the transcellular shift of K+) Should be given ONLY after adequate UO has been established
D - Drugs (Furosemide, Hydrocortisone, laxatives) A decrease in UO to less than 20 mL per hour for 2 consecutive
B - Bulimia nervosa hours is an indication to stop potassium infusion
I - inadequate intake of K+ Use an infusion pump as much as possible
T - Too much insulin Monitor patient by continuous ECG while infusion is going on
C - Cushing’s syndrome (causes kidneys to excrete K+) Apply warm compress to IV site
H - Heavy fluid loss
Nursing Management Nursing Management
Monitor for early presence in at-risk patients Monitor I&O and closely monitor signs of muscle weakness and
Encourage to consume potassium- rich foods dysrhythmias
Educate on proper use of laxative and/or diuretics Monitor vital signs, use apical pulse
Monitor I&O – 1L of urine output = 40mEq/L K+ loss Administer medications, as prescribed
Administer potassium replacement, as ordered and using the Encourage patient to strictly adhere to potassium restriction.
recommended method of administration Avoid fruits and vegetables, legumes, whole-grain breads, lean meat,
milk, eggs, coffee, tea, and cocoa
Caution patients to use salt substitutes sparingly if they are taking
Hyperkalemia other supplementary forms of potassium or potassium- sparing
diuretics
Calcium
Located primarily in the bones and teeth; the rest can be found
Serum potassium level > 5 mEq/L circulating in the serum
Less common than hypokalemia Functions:
More life-threatening because cardiac arrest is more frequently •Bone mineralization
associated with its occurrence •Stabilizes the resting membrane potential of neurons thereby
Causes: “CARED” preventing their spontaneous activation
•Regulation of muscle contraction – causes actin and myosin
C - Cellular movement of K+ from ICF to ECF filaments to slide into each other
A - Addison’s disease (hypoaldosteronism) •Cardiac contractility and conduction
R - Renal failure
E - Excessive K+ intake •Types of Calcium:
D - Drugs (Spironolactone, ACE inhibitors, NSAIDs) Ionized calcium
Protein-bound calcium
Calcium complexed to anions
Potassium Normal Values:
Neuromuscular irritability Ionized calcium: 4.5 to 5.1 mg/dL
Total calcium: 8.5 to 10.5 mg/dL
In hyperkalemia, “everything is high and fast”
Clinical Manifestations “MURDER”
M – Muscle weakness (late sign)
U – Unable to calm down (irritability, anxiety)
Hypocalcemia
R – Respiratory failure (sec. to muscle weakness)
→
D – Decreasing cardiac contractility (tachycardia bradycardia)
E – Early sign: muscle twitch/cramps
Serum calcium level < 8.5 mg/dL
Causes:
R – Rhythm abnormalities: Tall, peaked T waves and prolonged PR Primary Hypoparathyroidism
interval (most dangerous) Surgical hypoparathyroidism
Radical neck dissection
Medical Management Massive administration of citrated blood
Obtain ECG to detect changes Pancreatitis
Potassium restriction (diet and meds) Kidney injury
Calcium gluconate IV Prolonged bed rest/bed ridden patients
•Emergency management for extremely high K+ levels
•MOA: calcium antagonizes the action of hyperkalemia on the heart
but does not lower serum K+ level Extracellular Calcium
•S/E: hypotension, bradycardia
Sodium polystyrene sulfonate (Kayexalate)
•Cation exchange resin Increased cell membrane permeability
•Administer via PO or retention enema to sodium
•MOA: Increases fecal potassium excretion through binding of
potassium in the lumen of the gastrointestinal tract.
•C/I: paralytic ileus Increased neuromuscular irritability
Hyperkalemia protocol:
•Regular insulin (IV) + D50W: causes temporary shift of potassium
into the cells
•Beta-2 agonist (Salbutamol) “Everything is high and fast”
•Nebulized
•MOA: moves potassium into cells
•S/E: tachycardia, chest discomfort
Dialysis
Clinical Manifestations: Monitor and maintain airway patency
Tetany: general muscle hypertonia, with tremor and spasmodic or Institute seizure precautions
uncoordinated contractions occurring with or without efforts to make •Reduce environmental stimulation
voluntary movement •Identify and modify triggers
Latent Tetany: •Padded side rails
Numbness, tingling, and cramps in the extremities •Bed in lowest position
Stiffness of hands and feet •Oxygen and suction readily available
Overt Tetany:
•Bronchospasm
Laryngospasm
(+) Trousseau’s sign: carpopedal spasm resulting from occlusion of the
blood flow to the arm for 3 minutes
Hypocalcemia
(+) Chvostek’s sign: sharp tapping over the facial nerve causes spasm
or twitching of mouth, nose, eye Serum Calcium Level > 10.5 mg/dL
Seizures Causes:
Dysrhythmias - torsades de pointes Malignancies
Photophobia Hyperparathyroidism
Thiazide diuretics
Vitamin A and D toxicity
Chronic lithium use
Chvostek sign: a contraction of the Theophylline toxicity
facial muscles elicited in response to
light tap over the facial nerve in Extracellular Calcium
front of the ear
Decreased cell membrane permeability
to sodium
Decreased neuromuscular irritability
Trousseau sign: a carpopedal spasm
induced by inflating a blood pressure
cuff above systolic blood pressure.
“Everything is low and slow”
Clinical Manifestations:
Hypotension
ECG Changes: prolonged QT interval and lengthened ST segment Clinical Manifestations: “BACK ME UP”
Labs: hypomagnesemia B - Bone pain
Medical Management A - Arrhythmias (heart blocks, shortened QT interval and ST segment
C - Cardiac arrest (MOST DANGEROUS), constipation
Calcium salts IV K - Kidney stones
•Calcium gluconate (4.5mEq) M - Muscle weakness
•Calcium chloride (13.5mEq) E - Excessive urination
Vitamin D - increases calcium absorption from the GI tract U - Uhaw (thirst)
Calcium supplements (to be taken with meals) P - Pathologic fractures
High calcium diet
•Milk products Medical Management
•Green, leafy vegetables 0.9% NaCl solution
•Canned salmon Temporarily dilutes serum calcium and increases urinary calcium
•Canned sardines excretion
•Fresh oysters Furosemide (Lasix)
Nursing Management: Used in conjunction with PNSS
Promotes diuresis and enhances calcium excretion
Administer via slow IV/slow IV infusion Calcitonin IM
Assess IV site for evidence of infiltration Lowers calcium level by increasing calcium and phosphorous deposition
Do not use PNSS as it increases renal calcium loss; use D5W instead into bones
to dilute solution Useful for patients with heart disease or kidney injury
Do not use concurrently with solutions containing phosphates or Corticosteroids
bicarbonate Decrease bone turn over and tubular reabsorption for patients with
Encourage intake of calcium-rich foods sarcoidosis, myelomas, lymphomas, and leukemia
Advise to quit smoking and consume alcohol and caffeine in
moderation
Advise to avoid overuse of laxatives and antacids that contain
phosphorus
(oncologic origin) Clinical Manifestations:
a. Pamidronate disodium (Aredia) Cramps, spasticity
Biphosphonate (+) Trousseau and Chvostek sign
Inhibits osteoclastic activity Insomnia
S/E: fever, transient leukopenia Mood changes
b. Mithramycin Anorexia, vomiting
Cytotoxic antibiotic Increased tendon reflexes
Inhibits bone resorption and thus lowering serum calcium level Hypertension
Nursing Management Similar to hypocalcemia
Encourage early and frequent ambulation ECG changes:
Encourage oral fluids up to 3-4 L/day •Depressed ST segment
Encourage high fiber diet •Prolonged QRS
Implement safety precautions, as necessary •Dysrhythmias
Assess for signs of digitalis toxicity, especially in patients taking •PVCs
digoxin (Calcium enhances effects of digoxin) •SVT
Monitor heart rate and rhythms •Torsades de pointed
•Ventricular fibrillation
Magnesium Medical Management
High-magnesium diet for mild deficiencies
Intracellular cation
Has a direct relationship with potassium and calcium Green leafy vegetables
Normal Serum Mg++: 1.3-2.3 mg/dL Nuts
•1/3 is protein-bound Seeds
•2/3 are free cations – the active component Legumes
Absorbed in the small intestine Whole grains
Functions Seafoods
Activator of IC enzyme systems Peanut butter
Plays a role in CHO and CHON metabolism Cocoa
Affects neuromuscular irritability and contractility Magnesium supplements
Has a sedative effect- inhibits release of ACh Magnesium sulfate IV
Vasodilator and decreases peripheral resistance •For patients with overt manifestations of hypomagnesemia
•Administered using an infusion pump at a controlled rate
Nursing responsibilities:
Hypomagnesemia Magnesium sulfate IV
Monitor vital signs
Monitor urine output; (refer if U/O<100mL over 4 hours)
Calcium gluconate at bedside
Serum Mg++ level < 1.3 mg/dL Nursing Management
Frequently associated with hypokalemia and hypocalcemia Monitor at risk patients for signs and symptoms
Hypoalbuminemia= Hypomagnesemia Institute seizure precautions (severe hypomagnesemia)
Causes: “FAT GUM” Implement safety precautions if with confusion
F - Fistulas Educate on major sources of magnesium-rich foods
A - Alcohol withdrawal
T - Tube feedings/TPN (magnesium def)
G - Gastric suctioning prolonged
U - Uncontrolled BM (diarrhea)
M - Malabsorption disorders (small intestine)
Hypermagnesemia
Serum Magnesium Serum Mg++ >2.3 mg/dL
Rare electrolyte abnormality
Falsely elevated Mg++ may result from:
Hemolyzed blood specimen
Increased ACh release Blood drawn from an extremity with a torniquet that was applied too
tightly
Causes:
Kidney injury
Increased neuromuscular irritability Excessive intake of magnesium- containing antacids
DKA
“Everything is high and fast”
Serum Magnesium
Decreased ACh release
Decreased neuromuscular irritability
“Everything is low and slow”
Clinical Manifestations
Flushing
Hypotension
Muscle weakness
Drowsiness
Hypoactive reflexes
Respiratory depression
Cardiac arrest
Coma
Diaphoresis
Medical Management
Avoid giving magnesium to patients with kidney injury
Discontinue all sources of magnesium if with severe hypermagnesemia
Calcium gluconate IV - Calcium antagonizes magnesium
Ventilatory support, if with respiratory depression
Hemodialysis
If with adequate renal function:
•Furosemide (Lasix)
•PLR or PNSS
Nursing Management
Monitor vital signs, noting hypotension and shallow respirations
Assess deep tendon reflexes Increased Blood Calcium
Assess level of consciousness level
Caution on use of OTC medications
Decreased neuromuscular
excitability
Increased Calcium
excretion by kidneys
Precipitate formation
Cognitive GI Musculoskeletal Cardiac
dysfunction Disturbance symptoms symptoms
Nephrolithiasis
You might also like
- BETA HCG Test Report Format Example Sample Template Drlogy Lab ReportDocument1 pageBETA HCG Test Report Format Example Sample Template Drlogy Lab Reportseemaaingh1995No ratings yet
- NurseBossStore Nursing NotesDocument17 pagesNurseBossStore Nursing NotesMary Kimberly S. CaberteNo ratings yet
- 50 Most Commonly Prescribed Medications PDFDocument2 pages50 Most Commonly Prescribed Medications PDFChantelle Houston100% (1)
- MK Notes by YournursingspaceDocument60 pagesMK Notes by Yournursingspaceezinne obinna-uma100% (3)
- Pharm WorksheetsDocument29 pagesPharm Worksheetsj.siemens1d100% (2)
- ABGsDocument13 pagesABGsAmanda Maria100% (4)
- NCLEX Cram SheetDocument6 pagesNCLEX Cram Sheetaishwariyapokharel55No ratings yet
- Calendar of Days & Awareness DaysDocument2 pagesCalendar of Days & Awareness DaysAshfaque HossainNo ratings yet
- Medical Abbreviations: Beautiful Nursing LLCDocument2 pagesMedical Abbreviations: Beautiful Nursing LLCcarly100% (1)
- Med Surg Test 4 Study GuideDocument29 pagesMed Surg Test 4 Study GuideJess100% (2)
- Medication Work Sheet For MedSurgDocument5 pagesMedication Work Sheet For MedSurgRyanMitchell100% (3)
- Pharmacology Important Things To RememberDocument5 pagesPharmacology Important Things To RememberHydie100% (1)
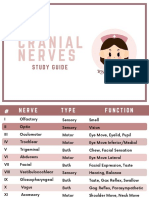
- Cranial NervesDocument6 pagesCranial Nervesvienny kayeNo ratings yet
- Analgesics: AnticonvulsantsDocument8 pagesAnalgesics: AnticonvulsantsGina Giammalvo100% (2)
- Blood Transfusions BN CopyrightDocument2 pagesBlood Transfusions BN CopyrightDENVER CARBON100% (1)
- DigitalPharmacologyBundle170Pages CompressedDocument170 pagesDigitalPharmacologyBundle170Pages Compressed98b5jc5hgtNo ratings yet
- Remembering Medication ClassificationsDocument2 pagesRemembering Medication ClassificationsGVHHNo ratings yet
- Mnemonics For NursingDocument35 pagesMnemonics For Nursingbetterdenthat100% (1)
- Pharmacology-ATI 150 Drug Cards PDFDocument4 pagesPharmacology-ATI 150 Drug Cards PDFholly100% (1)
- Lung SoundsDocument6 pagesLung SoundsAira KieNo ratings yet
- Electrolyte Imbalance Cause Signs and Symptoms Intervention ConnectionDocument6 pagesElectrolyte Imbalance Cause Signs and Symptoms Intervention ConnectionmkninnyNo ratings yet
- Med Surg BundleDocument82 pagesMed Surg BundleThe Treasure ChestNo ratings yet
- Med SurgDocument6 pagesMed SurgWANG PUPPYNo ratings yet
- Nero Drugs To KnowDocument14 pagesNero Drugs To KnowGina Giammalvo100% (2)
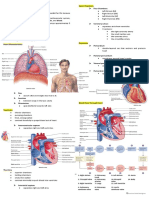
- CardionotesDocument5 pagesCardionotesNichole Coletta100% (3)
- Basic Drug Cards 3Document14 pagesBasic Drug Cards 3Karima Jones100% (1)
- Chapter 12: HEARTDocument2 pagesChapter 12: HEARTPrecious Faith RodriguezNo ratings yet
- Pharmacology FreebieDocument3 pagesPharmacology FreebieMohammad Farooq Khan50% (2)
- Lab Values - Chart by PriorityDocument2 pagesLab Values - Chart by Priorityashley100% (1)
- Clinical Med CardsDocument26 pagesClinical Med CardsLila Daniels100% (1)
- Pharm 1.11 Insulin Cheat SheetDocument1 pagePharm 1.11 Insulin Cheat SheetSanobar Charania100% (1)
- Understanding ElectrolytesDocument2 pagesUnderstanding Electrolytessurviving nursing schoolNo ratings yet
- Study BundleDocument188 pagesStudy Bundlenazbeen.ahmadi100% (1)
- Pharm SummaryDocument3 pagesPharm Summaryastorm0872No ratings yet
- MedicationsDocument27 pagesMedicationsThe Treasure ChestNo ratings yet
- Heart Blocks: "The Heart Block Poem"Document18 pagesHeart Blocks: "The Heart Block Poem"Bijay Kumar Mahato100% (1)
- Cardiac DrugsDocument4 pagesCardiac DrugsIbrahem Al100% (2)
- 17 Cardiac DrugsDocument6 pages17 Cardiac DrugshiwaralelataNo ratings yet
- IV Fluid Cheat SheetsDocument8 pagesIV Fluid Cheat SheetsNhietz SeraNo ratings yet
- Normal Lab ValuesDocument3 pagesNormal Lab ValuesHNo ratings yet
- Summary of Antidiabetic Drugs PDFDocument3 pagesSummary of Antidiabetic Drugs PDFZinc Yulo100% (1)
- Blood Transfusions : Beautiful NursingDocument1 pageBlood Transfusions : Beautiful NursingMs KillaNo ratings yet
- Endocrine NursingDocument2 pagesEndocrine Nursingsurviving nursing school100% (2)
- Arrythmia Name: Normal Sinus RhythmDocument7 pagesArrythmia Name: Normal Sinus RhythmJulx0100% (1)
- Ncle X Cheat SheetDocument24 pagesNcle X Cheat Sheet98b5jc5hgt100% (1)
- Lab Values Chart 120511 PDFDocument5 pagesLab Values Chart 120511 PDFVanessaMUeller100% (3)
- Clinical Care Plan GuideDocument13 pagesClinical Care Plan Guidej.siemens1d100% (1)
- Med Surg BundleDocument112 pagesMed Surg BundleCynthia Leyva100% (7)
- Urinary SystemDocument9 pagesUrinary SystemCailah Sofia SelausoNo ratings yet
- Pharmacology Bundle Study GuideDocument47 pagesPharmacology Bundle Study GuideAmisalu Nigusie100% (2)
- Mnemonics For NursesDocument52 pagesMnemonics For Nursessweetpearl27100% (3)
- IV Fluids Cheat Sheet Copyright BNDocument2 pagesIV Fluids Cheat Sheet Copyright BNJeshan Yanong BeltranNo ratings yet
- Electrolytes ImbalancesDocument4 pagesElectrolytes ImbalancesPeter John Ruiz100% (2)
- Nursing Pharmacology Perfusion Study GuideDocument9 pagesNursing Pharmacology Perfusion Study GuideChelsea SmithNo ratings yet
- Mnemonics PDFDocument15 pagesMnemonics PDFbeingfiredNo ratings yet
- Bundle Fundamentals of Nursing PDFDocument59 pagesBundle Fundamentals of Nursing PDFسلطان محمد فوزي سلمان100% (1)
- Cardiac Study GuideDocument11 pagesCardiac Study Guidesurviving nursing school100% (2)
- Common Drugs ChartDocument15 pagesCommon Drugs Chartforminsko100% (1)
- MedSurg and Pharm BonusDocument13 pagesMedSurg and Pharm BonusThe Treasure ChestNo ratings yet
- Electrolyte Imbalances TransDocument12 pagesElectrolyte Imbalances TransAndre AndradaNo ratings yet
- Fluid Electrolyte Imbalance n132 160210135651Document100 pagesFluid Electrolyte Imbalance n132 160210135651Shahan FarooqNo ratings yet
- Fluid Electrolyte Imbalance n132 160210135651Document99 pagesFluid Electrolyte Imbalance n132 160210135651Mala AninahNo ratings yet
- 13 Principles of Aseptic TechniqueDocument1 page13 Principles of Aseptic TechniqueMarie Antionette MondragonNo ratings yet
- Care of Clients With Gastrointestinal DisordersDocument4 pagesCare of Clients With Gastrointestinal DisordersMarie Antionette MondragonNo ratings yet
- Brown Abstract Things To Do List and PlannerDocument3 pagesBrown Abstract Things To Do List and PlannerMarie Antionette MondragonNo ratings yet
- NotesDocument4 pagesNotesMarie Antionette MondragonNo ratings yet
- Diagnostic Testing For Urinary System DisordersDocument3 pagesDiagnostic Testing For Urinary System DisordersMarie Antionette MondragonNo ratings yet
- D. NCM 234-Medical ConditionsDocument77 pagesD. NCM 234-Medical ConditionsMarie Antionette MondragonNo ratings yet
- Preop NotesDocument10 pagesPreop NotesMarie Antionette MondragonNo ratings yet
- Spot Mapping of Sitio KawayananDocument1 pageSpot Mapping of Sitio KawayananMarie Antionette MondragonNo ratings yet
- SIRITUAL NEEDS QUESTIONNAIRE (SPQN)Document3 pagesSIRITUAL NEEDS QUESTIONNAIRE (SPQN)Marie Antionette MondragonNo ratings yet
- Record of Newborn CareDocument1 pageRecord of Newborn CareMarie Antionette MondragonNo ratings yet
- B. NCM 234 - SEXUALLY TRANSMITTED DISEASES (Week 3)Document134 pagesB. NCM 234 - SEXUALLY TRANSMITTED DISEASES (Week 3)Marie Antionette MondragonNo ratings yet
- Classification of FatsDocument2 pagesClassification of FatsMarie Antionette MondragonNo ratings yet
- A. NCM 234 - REPRODUCTIVE FUNCTION DISORDERS (Week 3)Document57 pagesA. NCM 234 - REPRODUCTIVE FUNCTION DISORDERS (Week 3)Marie Antionette MondragonNo ratings yet
- Digital Scrapbook - Espina - n1Document15 pagesDigital Scrapbook - Espina - n1Marie Antionette MondragonNo ratings yet
- Fats DeficiencyDocument2 pagesFats DeficiencyMarie Antionette MondragonNo ratings yet
- Importance of LipidsDocument1 pageImportance of LipidsMarie Antionette MondragonNo ratings yet
- Functions of FatDocument2 pagesFunctions of FatMarie Antionette MondragonNo ratings yet
- 6 - The World of RegionsDocument38 pages6 - The World of RegionsMarie Antionette MondragonNo ratings yet
- Why Dragonpay?: Compared With Other Platforms, Fao Can Confirm and Verify Payments Faster Via DragonpayDocument10 pagesWhy Dragonpay?: Compared With Other Platforms, Fao Can Confirm and Verify Payments Faster Via DragonpayMarie Antionette MondragonNo ratings yet
- Line Dance ModuleDocument34 pagesLine Dance ModuleMarie Antionette MondragonNo ratings yet
- DefinitionDocument2 pagesDefinitionMarie Antionette MondragonNo ratings yet
- TimelineDocument12 pagesTimelineMarie Antionette MondragonNo ratings yet
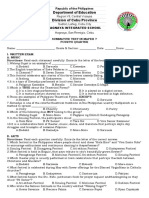
- Department of Education Division of Cebu ProvinceDocument5 pagesDepartment of Education Division of Cebu ProvinceNelsie FernanNo ratings yet
- Trauma - and Stressor-Related DisordersDocument34 pagesTrauma - and Stressor-Related DisordersjenNo ratings yet
- 704 Viet Nam Fact SheetsDocument2 pages704 Viet Nam Fact SheetsKhánh NgôNo ratings yet
- Amonoo 2019Document12 pagesAmonoo 2019zozNo ratings yet
- CD 2022 FundaICN Starters Basic - PDF - FOR REVIEWERDocument15 pagesCD 2022 FundaICN Starters Basic - PDF - FOR REVIEWERMeryville JacildoNo ratings yet
- SmokingDocument3 pagesSmokingKyle OrlanesNo ratings yet
- PEA Glaucoma TreatmentDocument9 pagesPEA Glaucoma TreatmentMenoddin shaikhNo ratings yet
- To Study 1Document69 pagesTo Study 1Alyssa RebeccaNo ratings yet
- ANTINYERIDocument12 pagesANTINYERINunuk HidayantiNo ratings yet
- Literature Review Diabetic Foot CareDocument6 pagesLiterature Review Diabetic Foot Careafdttjcns100% (1)
- Health History Form 03Document2 pagesHealth History Form 03IñakiNo ratings yet
- Colle's FractureDocument22 pagesColle's FractureAkshata HingeNo ratings yet
- Cvac 176Document18 pagesCvac 176Helder LezamaNo ratings yet
- The Blood Sugar Solution: The Ultrahealthy Program For Losing Weight, Preventing Disease, and Feeling Great Now! (The Dr. Mark Hyman Library, 1)Document23 pagesThe Blood Sugar Solution: The Ultrahealthy Program For Losing Weight, Preventing Disease, and Feeling Great Now! (The Dr. Mark Hyman Library, 1)brigitteannemarietrr100% (10)
- Inp RbeDocument13 pagesInp RbeAllaiza CristilleNo ratings yet
- Lingering InjuriesDocument12 pagesLingering Injuriessunrei musicNo ratings yet
- MainDocument7 pagesMainRosul majeedNo ratings yet
- Finbarr C. Martin and Anette Hylen RanhoffDocument13 pagesFinbarr C. Martin and Anette Hylen RanhoffMessias FilhoNo ratings yet
- Recurrent MiscarriageDocument13 pagesRecurrent MiscarriageMerahit AberaNo ratings yet
- Faisal Yunus PIPKRA How Adherence To GOLD Improve The COPD Treatment and Economic Outcomes - 3 Feb 2023-1Document37 pagesFaisal Yunus PIPKRA How Adherence To GOLD Improve The COPD Treatment and Economic Outcomes - 3 Feb 2023-1Muhammad Khairul AfifNo ratings yet
- SBAR Patient CareDocument6 pagesSBAR Patient CareFreddie254No ratings yet
- Unit 1 - Understanding PsychopathologyDocument6 pagesUnit 1 - Understanding Psychopathologybiyaspsy9No ratings yet
- Wu 2017Document12 pagesWu 2017Rashellya RasyidaNo ratings yet
- Bhert Ex - OrderDocument3 pagesBhert Ex - OrderJoy Javier Abonita RazadoNo ratings yet
- Explanation 2021 July 1Document321 pagesExplanation 2021 July 1Reshma Shaji PnsNo ratings yet
- Emergency Nursing (Medical Emergencies - ABC) - StudentsDocument19 pagesEmergency Nursing (Medical Emergencies - ABC) - StudentsAngielyn Ramos OlorazaNo ratings yet
- Laporan Pasien Konsul Divisi Endokrin FauzanDocument2 pagesLaporan Pasien Konsul Divisi Endokrin Fauzanfauzan azhariNo ratings yet
- 8 - Disorders of The GallbladderDocument33 pages8 - Disorders of The Gallbladdersohaib salamehNo ratings yet