Psychoeducation
Psychoeducation
Uploaded by
Srinivas PandeshwarCopyright:
Available Formats
Psychoeducation
Psychoeducation
Uploaded by
Srinivas PandeshwarOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Psychoeducation
Psychoeducation
Uploaded by
Srinivas PandeshwarCopyright:
Available Formats
A. Atri & M.
Sharma / Californian Journal of Health Promotion 2007, Volume 5, Issue 4, 32-39
Psychoeducation: Implications for the Profession of Health Education
Ashutosh Atri1 and Manoj Sharma 2
1
University of Texas Health Sciences Center, Houston 2 University of Cincinnati Abstract
Mental illnesses contribute to substantial morbidity in the population. Education for prevention and control of mental illnesses is mandatory. Psychoeducation is the specialized education that comprises of educational endeavors directed toward the patients and their families with an aim to help prevent relapse of mental illnesses and restoration of health for mentally ill patients. Several studies have proven the value of psychoeducation in prevention and control of mental illnesses ranging from depression to schizophrenia. Psychoeducation helps the mentally ill by improving treatment adherence. Psychoeducation is a subset of health education. Psychoeducation imparted by medical professionals due to insufficient training, insufficient resources and insufficient time is at best modest. Therefore, health educators who have specialized training in health education are very well suited for psychoeducation. However, the amount of training currently being offered in many health education programs nationwide at the undergraduate and the graduate level is not sufficient to qualify the educator for dealing with mental illnesses. More course work in mental illnesses and their prevention needs to be in place. Also prospective studies need to be designed for testing the efficacy of health educators in psychoeducation. Finally incorporation of behavioral theories to psychoeducation by the profession of health education will make it more effective. 2007 Californian Journal of Health Pro motion. All rights reserved. Keywords: Psychoeducation, mental illnesses, health educators Introduction Mental illnesses affect a substantial proportion of the population. According to the Centers for Disease Control and Prevention (CDC, 1998), in the United States, an estimated 10% people had recent disability from a diagnosable mental illness and 24% had experienced a mental disorder during the preceding year. Another community-based survey found that 6.2 percent of respondents reported serious mental illness in the preceding year (Kessler et al., 2001). According to another study, approximately 4.3 million psychiatric- related emergency department visits occurred, yielding an annual rate of 21 visits per 1000 adults (Hazlett, McCarthy, Londner, & Onyike, 2004). For schizophrenia, the 12-month prevalence in the United States in 2002 was estimated at 5.1 per 1000 lives (Wu, Shi, Birnbaum, Hudson, & Kessler, 2006). Owing to a variety of reasons including stigma, many mentally ill patients do not seek treatment. Among those who seek treatment, many do not comply with the treatment. Education for prevention and control of mental illnesses is mandatory. The importance of psychoeducation in the management of the mentally ill has been reinforced in recent times by multiple prospective clinical trials which have compared a medications only approach with techniques that blended psychoeducation with medications (Colom et al., 2003; Perry, Tarrier, Morriss, McCarthy, & Limb, 1999). The outcomes from most of these studies have validated the utilization of psychoeducation as an approach that improves the efficacy of pharmacological approaches. In most instances, the blended approach remains superior to a medications only approach. Bipolar illness and schizophrenia remain just two of the many mental health conditions where the combined approach has been found better.
32
A. Atri & M. Sharma / Californian Journal of Health Promotion 2007, Volume 5, Issue 4, 32-39
As a result of these findings, the term psychoeducation is finding frequent mention in contemporary mental health literature, typically when referencing to techniques found useful in the management of the severely mentally ill. However, till date, due to a lack of unanimity on a standard definition of psychoeducation, the subject area has been riddled with a multitude of definitions. Some of the definitions are oversimplified while others over inclusive of techniques that should, strictly speaking, not fall within the purview of psychoeducation. Psychoeducation: Controversies in Definition In forming a consensus on the boundaries of psychoeducation and conceiving a working definition of the term, Goldman (1988) explores the different definitions and varying interpretations and ties them all together. Goldman (1988) defines psychoeducation as Education or training of a person with a psychiatric disorder in subject areas that serve the goals of treatment and rehabilitation, for example, enhancing the persons acceptance of his illness, promoting active cooperation with treatment and rehabilitation, and strengthening the coping skills that compensate for deficiencies caused by the disorder The two most important ways in which this definition differs from its preceding ones are as follows. First, this fairly expansive definition includes any education given to a patient with a psychiatric disorder if such education would enhance the patients ability to survive in the community. Second, this definition absolutely excludes any education given to the family as psychoeducation irrespective of what benefits or promises it may hold for the actual patient. Despite the above developments, psychoeducation, as a formal term, has continued to be used as something that depicts educational approaches for both the mentally ill and their family members. Different researchers through the late 20th and the first decade of the 21st century have continued to use differing interpretations of the term due mainly to the fact that it remains, perhaps, the most well known umbrella term that somewhat effectively convey
to the audience any measures that are nonpharmacological and that benefit the mentally ill (Colom et al., 2003; Dixon, Adams, & Lucksted, 2000; Perry et al., 1999). Some researchers have gone on record to include any and all psychosocial interventions within the purview of psychoeducation. In as much as the primary purpose of this article is not to debate the validity or redundancy of the different definitions for psychoeducation but to make a link between psychoeducation and the profession of health education, we have tried to adhere to a more inclusive approach towards psychoeducation. Such an approach treats any educational endeavor (irrespective of whether it is directed to the patient or the family) designed to help a mentally ill patient gain some semblance of recovery as psychoeducation. However, the fact that controversy has been inherent in defining psychoeducation gives us reason to believe that it may be a time to revisit some aspects of it. Psychoeducation: What Makes it so Important? An evidence-based approach dictates that for most moderately to severely debilitating mental health conditions, a combined modality approach that blends drugs with therapy and/or education remains, by far, the best in terms of outcome and eventual prognosis. Multiple studies have proven the value of psychoeducation in psychopathologies ranging from depression to schizophrenia. Pekkala & Merinder (2002), in a meta analysis of all psycho educational interventions conducted on patients with schizophrenia, found that psychoeducation was a useful part of the treatment program. Colom and colleagues (2003, 2004) assert that in the treatment of bipolar patients, psychoeducation may have a role beyond the enhancement of patient compliance to drug treatment, and holds a special role for patients with co existing personality disorders. Recent studies have proven the associations between multiple socio-environmental stressors and remission-relapse successions of mental illnesses. Levels of familial expressed emotion, parental warmth, disruptive life events that may
33
A. Atri & M. Sharma / Californian Journal of Health Promotion 2007, Volume 5, Issue 4, 32-39
accelerate goal striving have all been found to predict acute exacerbations in bipolar depression. Other psychosocial variables like marital status, social support (and more importantly the lack of it), education, socioeconomic status and lack of accurate knowledge about ones condition all influence a patients compliance to drug treatment (Miklowitz, Elizabeth, Jeffrey, Teresa, & Richard, 2003). Given that educational interventions can be designed around each of the above cited variables is in itself a prime reason that makes psychoeducation so important. Ways in which adjunctive psychoeducation may help the mentally ill are by improving treatment adherence (which remains one of the most crucial factors that governs the outcome of a disease), helping in a greater stabilization of symptoms, preventing relapses and reducing inter-episode symptoms through enhancing patients stress management abilities and finally helping in the rehabilitation of patients to the maximum level of functioning possible (Miklowitz et al., 2003). Psychoeducation helps in improving the compliance to the long term drug treatment often prescribed in mental illnesses. Psychoeducation: Contemporary Trends factors govern the trends in the field of Several psychoeducation and decide who will be authorized to practice it. It is these very factors which would deter other professions from pursuing interests in the field. If we analyze the current medical paradigm, we can find a fairly sharp split between the medical and the psychiatric domains as regards psychoeducation. Psychiatry has come closer and closer to traditional medicine in recent years, with the revelations that most psychiatric conditions are at least partially (and occasionally wholly) organic in nature. Despite these developments, psychoeducation (even basic information on psychiatric conditions that may not necessarily require an advanced degree in psychiatry) is sadly missing from most nonpsychiatric physician-patient encounters. While a number of family physicians and internists will gladly and aggressively disseminate information
about possible ways one could protect against conditions drawing from other medical specialties, most professionals shy away from flirting with any condition that is viewed as being traditionally within the domain of psychiatry. As an analogy, while a physician may be perfectly willing to discuss the prospects and prognosis of melanoma (which ideally is a dermatological condition) with a client even before he seeks a referral to a skin specialist, he may be more tempted to make an immediate referral to a psychiatrist if the same client seeks information about schizophrenia. Unlike a lot of medical specialties, the field of mental health remains plagued with unique challenges. The diagnosis of a number of mental illnesses remains, at best, a subjective attempt. While it is fairly easy to educate a diabetic about his blood sugar levels and expect him to follow those levels closely; the same may not be expected of a manic depressive (bipolar) patient who may not have an objective end point to gauge the severity of his or her disease, only subjective sensations. Further, there are schools of philosophy, aptly called the anti-psychiatry movement, which openly challenge the very existence of several mental conditions. Dain (1989), in his reflections on anti psychiatry, maintains that hostility to psychiatry actually predates the establishment of psychiatry as a profession, and organized opposition to psychiatric practices appeared in the late nineteenth century and continued well into the 20th century. These challenges make the job of designing and implementing evidence-based practices for educating patients with psychiatric conditions a very difficult, if not impossible, endeavor. Further, unlike a number of fields where the role of education is handed over the specialists employed specifically for that purpose, psychoeducation is, at best, shared between psychiatrists, therapists and other allied mental health workers. In an outpatient setting, the education role is taken over mostly by the psychiatrists and the therapists while in an inpatient setting, it is variedly divided between all mental health professionals. As long as a patient is being followed as an outpatient, he
34
A. Atri & M. Sharma / Californian Journal of Health Promotion 2007, Volume 5, Issue 4, 32-39
remains in regular contact with his psychiatrist and therapist and receives whatever psychoeducation is deemed necessary from them. Under more trying conditions when such a patient develops acute exacerbations and may have to be admitted, the Psychoeducator role is embraced by nurses and other allied workers. However, the current trend of deinstitutionalization of the mentally ill ensures that only the sickest and floridly psychotic patient would gain entrance to a psychiatric facility. It is a matter of conjecture then as to how receptive these patients can really be to the education they may be receiving inside of the facilities at a point when their powers of deductive reasoning are at a record low. In such a closed loop system it is hard for a health educator to step in even if it were proven that such a course would benefit the patients. Moreover, a 2005 study was done in Germany to assess the current status of relapse prevention in schizophrenia reveals some shocking findings (Hamann, Mischo, Langer, Leucht, & Kissling, 2005). Hamann and colleagues found that psychiatrists routinely communicated treatment plans and offered psychoeducation to only about one third of their patients, even though psychoeducation has been shown to increase medication compliance. Hogarty (2003) discusses the possible reasons why few families of the severely mentally ill have ever been offered family psychoeducation within North America, despite a quarter century of duplications. The rare families that are engaged receive mostly an occasional lecture or 'bibliotherapy', but education about evidencebased family approaches are mostly lacking. Multiple policy and organizational impediments, which may include staff burdens, cost, cynicism, philosophical differences, and lack of leadership, may be responsible (Dixon et al., 1999; Hogarty, 2003). Such findings raise serious questions about how deficient the current delivery of evidence-based mental health services (especially as regards psychoeducation) might be, and what we could do to improve them. Finally, there are vital issues about the accessibility to health education/promotion services by those with mental illnesses. The
mentally ill may find it hard to seek education about their condition outside of the medical domain due mainly to the fact that their accessibility to these efforts is further compromised as a result of their disease. Psychoeducation: A Subset of Health Education Whether psychoeducation should be included as a subset of health education or not, is a question best answered by pitting the defining elements of health education against those of psychoeducation. Green, Kreuter, Partridge, and Deeds (1980) have defined health education as, Any combination of learning experiences designed to facilitate voluntary adaptations of behavior conducive to health Reasons why psychoeducation qualifies for each element of this definition and more are not far fetched. The key elements in this standard definition are learning experiences, voluntary adaptations and behavior conducive to health. Each of these three elements can be found within psychoeducation. Irrespective of how we go about defining psychoeducation (i.e., whether or not we chose to include the education being given to the family as psychoeducation), there is a definitive learning experience involved. By educating a bipolar manic depressive patient about the warning signals for a possible manic exacerbation, we are in essence, helping him or her internalize a learning process. The education of the family members of a severely depressed individual about the importance of a 24-hour watch on that person is not hard to picture as a learning experience more or less indelibly imprinted on the minds of those people for future references. As previously mentioned, increased patient compliance to a pharmacological regimen is just one of the many benefits of psychoeducation. In that it leads to a fairly stable change in the behaviors pertaining to medication compliance, psychoeducation can be visualized as a voluntary adaptation, voluntary because no aspect of it is forced and adaptation because it
35
A. Atri & M. Sharma / Californian Journal of Health Promotion 2007, Volume 5, Issue 4, 32-39
better helps the individual in dealing with his illness. Finally, by enlightening the patients and their families about the different aspects (warning signs, symptoms, medication adherence, resources available) of the patients illness and how they interact to have a bearing on the disease itself, we can direct both the patient and the family into behaviors conducive to the mental health of that particular individual. It is fairly easy to compare and contrast the education imparted to diabetics about the premonitory signs of a low blood sugar (dizziness, rapid heart beat, etc.) with that provided to a manic depressive individual about the warning signs for a possible manic attack (speedy thoughts, disturbances in sleep rhythm and so on). Why We Need Health Educators to Psychoeducate? Despite multiple commonalities between the fields of health education and psychoeducation, there have been few attempts by practitioners in general to design studies or attempt any convergence of these two fields. Some of the reasons why this may be are fairly intuitive while others lie deeper. Perhaps one of the more important reasons is the fact that rights to any and all psychoeducation are strongly held by medical practitioners despite the fact that due either to lack of sufficient resources or sufficient time, such attempts may at best be modest (Hamann et al., 2005). The recent Deinstitutionalization movement in psychiatry has virtually ensured that a patient will only spend his most incapacitated period as a psychiatric inpatient, further reducing the time available for the educational process. Leslie and Rosenheck (1999), in their analysis of psychiatric inpatient service patterns for a group of 3.9 million privately insured individuals, found that substantial cost reductions for mental health services, over a period of two years, were primarily a result of reductions in inpatient and outpatient treatment days. Declines in inpatient service use were not accompanied by increases in outpatient service use, even for severely ill patients requiring hospitalization.
Research has repeatedly demonstrated that for a large number of mental illnesses, psychotherapy (which often includes psychoeducation) with medications produces the best outcomes (Colom et al., 2003; Dixon et al., 2000; Perry et al., 1999). However, recent evidence also maintains that severely ill patients may be unlikely to receive such evidence-based services (Lehman & Steinwachs, 1998). Even standard pharmacological conventions rooted in research are usually not followed, and as few as 10% of patients receive more complex interventions, such as supported employment or family psychoeducation. The multiple policy and organizational level factors responsible for such an abysmal state of affairs have already been mentioned above (Dixon et al., 1999; Hogarty, 2003). The problem of poor access to evidencebased practices for persons with severe mental illness has been cited by multiple reviewers of the literature (Drake et al., 2001) and was noted in the mental health report of the US Surgeon General (United States Surgeon General, 2000). Cultures which traditionally shy away from mental health, mental health practitioners and discussions about psychopathology in general may be more receptive to psychoeducation by health educators. The South Asian population in the United States offers a perfect example of one such cultural group. In their exploration of the mental health issues of the South Asian population in United States, Lin & Cheung (1999) maintain that this population has a documented historical record of low inpatient psychiatric admission, further augmented by a more recent establishment of an equally low utilization of outpatient mental health services. It has been shown that these low rates of utilization of mental health services are not correlated with low rates of psychopathologies. The earlier notion of a model minority, which maintained that a low rate of utilization of mental health services stemmed from a low rate of psychopathology, has been discarded. Instead, recent research suggests that cultural barriers may prevent help seeking by the mentally ill patients of this group early on in the disease process. Patients may wait for a substantial length of time and seek help only when all
36
A. Atri & M. Sharma / Californian Journal of Health Promotion 2007, Volume 5, Issue 4, 32-39
alternate options have been exhausted and the mental illness has deteriorated significantly (Lin, Inui, Kleinman, & Womack, 1982). For precisely this last argument, psychiatrically ill populations may be more receptive to education given in non-medical and less threatening settings. Since the simplest way of defining psychosis is to imagine it as a process whereby the individual loses touch with his reality, it is not hard to imagine why such an individual may not be receptive to any education while in the midst of an acute psychotic attack. Health educators intercept populations at a preventive level. Such an approach could better serve the mentally ill or even candidates with a subliminal mental pathology who have not been formally diagnosed. As an example, by spreading awareness about the leading signs of mania and depression, much could be done about the rising adolescent suicide rates. Also, preventive psychoeducation could possibly better serve the communities since so many of mental health needs remain unmet. A recent Centers for Disease Control and Prevention report (CDC, 2007) revealed that after falling over 28% during the period 1990 - 2003, suicide rates in America for males and females aged 1024 climbed 8%. This is the largest single oneyear rise in 15 years. Apparently, despite our best intentions, the current model, while perfect in theory, has failed to be translated into practice. Translation of theory into practice is a task well-suited for a health educator. Recommendations for the Field of Health Education Having established some cause for why psychoeducation is but a subset of health education and that consequently, health educators need to assertively treat it as one of their own areas of expertise, we need to talk about the possible steps that might help us, as a profession, achieve this goal. What is needed is an appreciation of the fact that mental health conditions are quite different from most other health education initiatives, even the ones which directly deal with diseases. The amount of tact and care needed while broaching existing or
potential issues related to mental health is essentially not required elsewhere. The amount of training currently being offered in many health education programs nationwide at the undergraduate and the graduate level is not sufficient to qualify the educator for dealing with mental illnesses. More course work in mental illnesses and their prevention needs to be in place. Emphasis needs to be given to a practical approach on ways by which psychoeducation could be blended with routine health education. On a more advanced note, it would also be in the interest of the field if well-designed prospective studies could be initiated which would help gather data about the efficacy of psychoeducation by health educators in nonmedical settings. A need also lies for studies that would compare the efficacy of psychoeducation as delivered by health educators in non-clinical settings (with or without other more traditional topics) and that delivered by conventional practitioners in clinical settings. These proposed studies would help in multiple ways. First, they will help establish the feasibility of psychoeducation by credentialed health educators. Second, by benchmarking the efforts of health educators against their counterparts in other domains, they will help create higher levels of motivation amongst the educators. Third, by incorporating behavioral theories which are very much integral to health education in psychoeducational programs, a better outcome can be assured. Finally, prospective studies would help establish evidence-based guidelines for educators in this field and help standardize any approach to the subject. Once psychoeducation by health educators becomes an accepted norm, a concerted attempt to truly blend the knowledge from the two fields could be made. Combining behavioral change theories with existing psychoeducational models to ensure enduring behavioral change in an individual would perhaps be a worthy ultimate goal.
37
A. Atri & M. Sharma / Californian Journal of Health Promotion 2007, Volume 5, Issue 4, 32-39
References Centers for Disease Control and Prevention. (1998). Self-reported frequent mental distress among adults United States, 1993-1996. Morbidity and Mortality Weekly Reports, 47(16), 326-331. Centers for Disease Control & Prevention. (2007). Suicide trends among youths and young adults aged 10-24 years United States, 1990-2004. Morbidity and Mortality Weekly Reports, 56(35), 905908. Colom, F., Vieta, E., Reinares, M., Martinez-Aran, A., Torrent, C., Goikolea, J. et al. (2003). Psychoeducation efficacy in bipolar disorders: Beyond compliance enhancement. Journal of Clinical Psychiatry, 64, 1101-1105. Colom, F., Vieta, E., Sanchez-Moreno, J., Martinez-Aran, A., Torrent, C., Reinares, M. et al. (2004). Psychoeducation in bipolar patients with comorbid personality disorders. Bipolar Disorders, 6, 294-298. Dain, N. (1989). Critics and dissenters: reflections on "anti-psychiatry" in the United States. Journal of the History of the Behavioral Sciences, 25(1), 3-25. Dixon, L., Lyles, A., Scott, J., Lehman, A., Postrado, L., Goldman, H. et al. (1999). Services to families of adults with schizophrenia: from treatment recommendations to dissemination. Psychiatric Services, 50, 233-238. Dixon, L., Adams, C., & Lucksted, A. (2000). Update on family psychoeducation for schizophrenia. Schizophrenia Bulletin, 26(1), 5-20. Drake, R. E., Goldman, H. H., Leff, H. S., Lehman, A. F., Dixon, L., Mueser, K. T. et al. (2001). Implementing evidence-based practices in routine mental health service settings. Psychiatric Services, 52, 179-182. Goldman, C. R. (1988). Toward a definition of psychoeducation. Hospital & Community Psychiatry, 39, 666-668. Green, L. W., Kreuter, M. W., Partridge, K., & Deeds, S. (1980). Health education planning: A diagnostic approach. Mountain View, CA: Mayfield Publishing. Hamann, J., Mischo, C., Langer, B., Leucht, S., & Kissling, W. (2005). Physicians' and patients' involvement in relapse prevention with antipsychotics in schizophrenia. Psychiatric Services, 56, 1448-150. Hazlett, S. B., McCarthy, M. L., Londner, M. S., & Onyike, C. U. (2004). Epidemiology of adult psychiatric visits to US emergency departments. Academic Emergency Medicine, 11, 193-195. Hogarty, G. E. (2003). Does family psychoeducation have a future? World Psychiatry, 2(1), 29-30. Kessler, R. C., Berglund, P. A., Bruce, M. L., Koch, J. R., Laska, E. M., Leaf, P. J. et al. (2001). The prevalence and correlates of untreated serious mental illness. Health Services Research, 36(6 Pt. 1), 987-1007. Lehman, A. F., & Steinwachs, D. M. (1998). Translating research into practice: The schizophrenia patient outcomes research team (PORT) treatment recommendations. Schizophrenia Bulletin, 24, 1-10. Leslie, D., & Rosenheck, R. (1999). Shifting to outpatient care? Mental health care use and cost under private insurance. American Journal of Psychiatry, 156, 1250-1257. Lin, K. M., & Cheung, F. (1999). Mental health issues for Asian Americans. Psychiatric Services, 50, 774-780. Lin, K. M., Inui, T., Kleinman, A., & Womack, W. (1982). Sociocultural determinants of the help-seeking behavior of patients with mental illness. The Journal of Nervous and Mental Disease, 170(2), 7885. Miklowitz, D. J., Elizabeth, G. L., Jeffrey, R. A., Teresa, S. L., Richard, S. L. (2003). A randomized study of family-focused psychoeducation & pharmacotherapy in the outpatient management of bipolar disorder. Archives of General Psychiatry, 60, 904-912. Pekkala, E., & Merinder, L. (2002). Psychoeducation for schizophrenia. Cochrane Database System Review, no. 2, CD002831.
38
A. Atri & M. Sharma / Californian Journal of Health Promotion 2007, Volume 5, Issue 4, 32-39
Perry, A., Tarrier, N., Morriss, R., McCarthy, E., & Limb, K. (1999). Randomized controlled trial of efficacy of teaching patients with bipolar disorder to identify early symptoms of relapse and obtain treatment. British Medical Journal, 318(7177), 149-153. United States Surgeon General. (2000). Mental health: A report of the Surgeon General. Executive summary. Rockville, MD: USDHHS, Substance Abuse and Mental Health Services administration, Center for Mental Health Services, NIH, NIMH. Wu, E. Q., Shi, L., Birnbaum, H., Hudson, T., & Kessler, R. (2006). Annual prevalence of diagnosed schizophrenia in the USA: A claims data analysis approach. Psychological Medicine, 36, 15351540.
Author Information Ashutosh Atri, MS, MD Resident, Psychiatry University of Texas Health Sciences Center, Houston 1300 Moursund Street Houston, TX 77030-3406 Ph.:740-406- 0284 E-Mail: Ashutosh_atri@hotmail.com Manoj Sharma, MBBS, Ph.D. Associate Professor, Health Promotion & Education University of Cincinnati PO Box 210068 Cincinnati, OH 45221-0068 Ph.: 513-556-3878 Fax.: 513-556-3898 E-Mail: manoj.sharma@uc.edu
39
You might also like
- YP CORE User ManualDocument36 pagesYP CORE User Manualloubwoy100% (4)
- Schneider - Search of Realistic OptimismDocument14 pagesSchneider - Search of Realistic OptimismShane Quest100% (1)
- JACOBSON & CURTIS - Recovery As Policy in Mental Health Services Strategies Emerging From The StatesDocument15 pagesJACOBSON & CURTIS - Recovery As Policy in Mental Health Services Strategies Emerging From The StatesemaildegeorgeNo ratings yet
- IPIP-NEO Narrative ReportDocument9 pagesIPIP-NEO Narrative ReportAlvin PascualNo ratings yet
- What Is Systemic About Systemic Therapy? Therapy Models Muddle Embodied Systemic PRDocument17 pagesWhat Is Systemic About Systemic Therapy? Therapy Models Muddle Embodied Systemic PRFausto Adrián Rodríguez LópezNo ratings yet
- Barbara Turner - SandplayDocument3 pagesBarbara Turner - SandplayVeraCruzNo ratings yet
- Preview of "MyDietAnalysis - Report"Document2 pagesPreview of "MyDietAnalysis - Report"LeovergeldediosNo ratings yet
- Adpcn Resource ManualDocument4 pagesAdpcn Resource ManualJayvee V. De Guzman67% (3)
- Depression Conceptualization and Treatment: Dialogues from Psychodynamic and Cognitive Behavioral PerspectivesFrom EverandDepression Conceptualization and Treatment: Dialogues from Psychodynamic and Cognitive Behavioral PerspectivesChristos CharisNo ratings yet
- 4 - PsychoeducationDocument19 pages4 - PsychoeducationMuhammad AwaisNo ratings yet
- JACOBSON & GREENLEY - What Is Recovery A Conceptual Model and ExplicationDocument4 pagesJACOBSON & GREENLEY - What Is Recovery A Conceptual Model and Explicationemaildegeorge100% (1)
- Bore, Samuel K Psycho-Educational Groups in Schools NFJCA V2 N1 2013Document9 pagesBore, Samuel K Psycho-Educational Groups in Schools NFJCA V2 N1 2013Sam LalparlienNo ratings yet
- Is The Glass Half Empty or Half FullDocument3 pagesIs The Glass Half Empty or Half FullAdonis SferaNo ratings yet
- Positive PsyDocument14 pagesPositive PsySuvrata Dahiya PilaniaNo ratings yet
- Optimism and HealthDocument5 pagesOptimism and HealthNL JsNo ratings yet
- From Client Process To Therapeutic RelatingDocument15 pagesFrom Client Process To Therapeutic Relatingjean100% (1)
- Big Five Personality Test ResultsDocument1 pageBig Five Personality Test Resultsamazing_pinoyNo ratings yet
- Assessing Coping Strategies: A Theoretically Based ApproachDocument17 pagesAssessing Coping Strategies: A Theoretically Based ApproachMelinda HavadiNo ratings yet
- Guidelines - Safeguarding Children and Young PeopleDocument108 pagesGuidelines - Safeguarding Children and Young Peopleneculai.daniela78771No ratings yet
- Courage MeasurementDocument13 pagesCourage MeasurementMaciek Brylewicz100% (1)
- Child Psychopathology SyllabusDocument43 pagesChild Psychopathology SyllabusJered AbernathyNo ratings yet
- Personal Projects Analysis: Trivial Pursuits, Magnificent Obsessions, and The Search For CoherenceDocument17 pagesPersonal Projects Analysis: Trivial Pursuits, Magnificent Obsessions, and The Search For CoherenceamdtzNo ratings yet
- Chinese Teique SFDocument8 pagesChinese Teique SFSarmad Hussain ChNo ratings yet
- Social Anxiety and Introversion in College Students PDFDocument68 pagesSocial Anxiety and Introversion in College Students PDFAdelline MariaNo ratings yet
- Book of AbstractsDocument65 pagesBook of AbstractsANDREASNo ratings yet
- Daniel Freeman, Understanding+and+TreatmentDocument24 pagesDaniel Freeman, Understanding+and+TreatmentDNNo ratings yet
- The Assessment of Children With Attachment Disorder - The Randolph PDFDocument161 pagesThe Assessment of Children With Attachment Disorder - The Randolph PDFAnonymous g3sy0uI100% (1)
- Mrcpsych SyllabusDocument24 pagesMrcpsych SyllabusimperiallightNo ratings yet
- Object Relations TheoryDocument2 pagesObject Relations TheoryMonika Joseph0% (1)
- Activity Theory As A Lens For Characterizing The Participatory UnitDocument16 pagesActivity Theory As A Lens For Characterizing The Participatory UnitShaimaa Abdel MagiedNo ratings yet
- 2two Person PsychologyDocument8 pages2two Person PsychologyHrvatski strelicarski savezNo ratings yet
- Treating Anxiety With MindfulnessDocument15 pagesTreating Anxiety With MindfulnessLeighton Frank AggNo ratings yet
- Method of PsychotherapyDocument19 pagesMethod of Psychotherapy002019ryNo ratings yet
- Family-Based Psychoeducation For Children and Adolescents With Mood Disorders - Ong & Caron (2008)Document15 pagesFamily-Based Psychoeducation For Children and Adolescents With Mood Disorders - Ong & Caron (2008)Eduardo Aguirre DávilaNo ratings yet
- 9 - The Oxford Handbook of Qualitative Research by Patricia Leavy-162-185Document24 pages9 - The Oxford Handbook of Qualitative Research by Patricia Leavy-162-185mayara.gomesNo ratings yet
- Predictors of Subjective Well-Being Across CulturesDocument13 pagesPredictors of Subjective Well-Being Across CulturesEduardo GarcìaNo ratings yet
- Life Script: Determinants and Outcomes: March 2018Document11 pagesLife Script: Determinants and Outcomes: March 2018Alexa MaciucaNo ratings yet
- Different Psychological ModelsDocument11 pagesDifferent Psychological ModelsTrina Lloren LitorjaNo ratings yet
- The Psychology of Health and Illness PDFDocument109 pagesThe Psychology of Health and Illness PDFdevNo ratings yet
- The Use of Play For Assessment and Therapy The Case of A Child With Selective MutismDocument13 pagesThe Use of Play For Assessment and Therapy The Case of A Child With Selective MutismdiniNo ratings yet
- Running Head: Neuropsychologist Career 1Document8 pagesRunning Head: Neuropsychologist Career 1selina_kollsNo ratings yet
- Russian Psychology and Neuropsychotherapy: Comparative AnalysisDocument19 pagesRussian Psychology and Neuropsychotherapy: Comparative AnalysisGustavo CabanasNo ratings yet
- Icebergs and WorldviewsDocument14 pagesIcebergs and Worldviewsstanger_eGEJNo ratings yet
- Embodied Goal PursuitDocument5 pagesEmbodied Goal PursuitRooz CaloreNo ratings yet
- Cognitive Behavioral Play TheraphyDocument14 pagesCognitive Behavioral Play TheraphygjavierperezNo ratings yet
- Principles of Transactional Analysis - by Eric BerneDocument8 pagesPrinciples of Transactional Analysis - by Eric Bernecornelpc100% (1)
- Transactional Analysis Notes AnitaDocument28 pagesTransactional Analysis Notes Anitanitinabn28No ratings yet
- SchizophreniaDocument67 pagesSchizophreniaHazirah Mokhtar100% (1)
- Nelson Jones 2e CH 01Document11 pagesNelson Jones 2e CH 01Lee Cheah EuNo ratings yet
- Running Header: ADOLESCENT DEVELOPMENT 1Document28 pagesRunning Header: ADOLESCENT DEVELOPMENT 1Coleen AndreaNo ratings yet
- (Philip J. Graham) Cognitive Behaviour Therapy ForDocument548 pages(Philip J. Graham) Cognitive Behaviour Therapy ForHenry Eduardo CervantesNo ratings yet
- Positive Behaviour Support Information Sheet For Disability Sector OrganisationsDocument9 pagesPositive Behaviour Support Information Sheet For Disability Sector Organisationsmoi5566No ratings yet
- Evidence-Based Psychotherapy For Children and AdolescentsDocument12 pagesEvidence-Based Psychotherapy For Children and Adolescentspsiho_lyNo ratings yet
- Optimism SuperstitionDocument10 pagesOptimism SuperstitionChaps Bryan CatamaNo ratings yet
- (Doi 10.12968 - Bjon.1995.4.15.876) A. Farrington - Models of Clinical Supervision PDFDocument3 pages(Doi 10.12968 - Bjon.1995.4.15.876) A. Farrington - Models of Clinical Supervision PDFHendri HariadiNo ratings yet
- Improving Mother/child Interaction To Promote Better Psychosocial Development in ChildrenDocument36 pagesImproving Mother/child Interaction To Promote Better Psychosocial Development in ChildrenDharma Reddy PashapuNo ratings yet
- Gamble Boyle Ethics in Tele Psychology 2015Document8 pagesGamble Boyle Ethics in Tele Psychology 2015DanielaLealNo ratings yet
- Strengths Based SupervisionDocument18 pagesStrengths Based SupervisionGanOn JungianNo ratings yet
- Developmental Art Therapy by MalchiodiDocument2 pagesDevelopmental Art Therapy by MalchiodiAmna iqbalNo ratings yet
- András Szántó - What Orwell Didn't Know PDFDocument6 pagesAndrás Szántó - What Orwell Didn't Know PDFMa Nu ElaNo ratings yet
- Children's Testimony: A Handbook of Psychological Research and Forensic PracticeFrom EverandChildren's Testimony: A Handbook of Psychological Research and Forensic PracticeNo ratings yet
- Working with Anger: A Constructivist ApproachFrom EverandWorking with Anger: A Constructivist ApproachPeter CumminsNo ratings yet
- Tut Lett 501 - 2014 - 3 - eDocument59 pagesTut Lett 501 - 2014 - 3 - eBeNobody20% (1)
- Ped 271 Primary School Physical and Health - 0Document67 pagesPed 271 Primary School Physical and Health - 0Muttaka Turaki GujunguNo ratings yet
- CHNDocument5 pagesCHNAnnaAlfonsoNo ratings yet
- Prevention and The Promotion of Health, Wellness, and FitnessDocument25 pagesPrevention and The Promotion of Health, Wellness, and FitnessArun TamilvananNo ratings yet
- 11 Key Areas of ResponsibilitiesDocument1 page11 Key Areas of Responsibilitiesjo_annamae4413No ratings yet
- Coordinated School Health Program ModuleDocument7 pagesCoordinated School Health Program ModuleMa. Valerie DennaNo ratings yet
- Sindh Medical MCATDocument4 pagesSindh Medical MCATTayyab ShahzadNo ratings yet
- Ew MeritDocument120 pagesEw MeritShlok RathodNo ratings yet
- MANAGMENT EXTENSION PROGRAM-Concepts and Principles of NSTP Extension Management Program and Community ImmersionDocument8 pagesMANAGMENT EXTENSION PROGRAM-Concepts and Principles of NSTP Extension Management Program and Community Immersionnina grace joy0% (1)
- CQ MQ Eligible List 2022Document81 pagesCQ MQ Eligible List 2022raju kusumaNo ratings yet
- School Nurse Job Duties, Responsibilities, and SettingsDocument3 pagesSchool Nurse Job Duties, Responsibilities, and SettingsJhey MalanyaonNo ratings yet
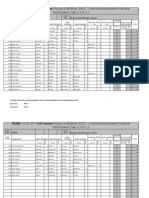
- PE2MS - GCSE 2011 Full Course Physical Education 5PE02 - Controlled Assessment PracticalDocument20 pagesPE2MS - GCSE 2011 Full Course Physical Education 5PE02 - Controlled Assessment Practicaldg_siaNo ratings yet
- Persuasive SpeechDocument2 pagesPersuasive SpeechchrisNo ratings yet
- Syllabus in Nursing Care Management 107Document11 pagesSyllabus in Nursing Care Management 107ropido100% (3)
- Help For Poor ChildrenDocument2 pagesHelp For Poor ChildrenAbdul MalickNo ratings yet
- Health Education Plan: Brokenshire College, IncDocument8 pagesHealth Education Plan: Brokenshire College, IncMaria Zarah Chrisanta AquinoNo ratings yet
- Home VisitingDocument35 pagesHome VisitingAparna KinginiNo ratings yet
- LG21 Mapeh 3 HealthDocument4 pagesLG21 Mapeh 3 HealthVanessa LimonNo ratings yet
- Sophe Esg Poster Draft 6Document1 pageSophe Esg Poster Draft 6api-248517076No ratings yet
- Georgia Health Education StandardsDocument77 pagesGeorgia Health Education StandardsWFXL_NewsNo ratings yet
- Score Sheet Poster SloganDocument8 pagesScore Sheet Poster SloganAddielou Fidelfio AbadNo ratings yet
- Hpeb 300 Exam 1 Top Tens 1Document11 pagesHpeb 300 Exam 1 Top Tens 1api-599678798No ratings yet
- OHI-S and DHE History in Patient Cardiovascular DiseasesDocument2 pagesOHI-S and DHE History in Patient Cardiovascular DiseasesmasytahdyahastiNo ratings yet
- NND 3136 Community Health Nursing I 2Document5 pagesNND 3136 Community Health Nursing I 2odhiambovictor2424No ratings yet
- Bulado, Clara - Ang Mga Dalagita Sa Sapang KawayanDocument2 pagesBulado, Clara - Ang Mga Dalagita Sa Sapang Kawayanayabulado0No ratings yet
- Vandemerwe ResumeDocument4 pagesVandemerwe Resumeapi-324739503No ratings yet
- Activity 4-PHDocument5 pagesActivity 4-PHKate MendozaNo ratings yet
- Health EducationDocument84 pagesHealth EducationJesus Mario Lopez100% (2)