Oral Revalida 2nd Year 2nd Sem
Oral Revalida 2nd Year 2nd Sem
Uploaded by
rodentCopyright:
Available Formats
Oral Revalida 2nd Year 2nd Sem
Oral Revalida 2nd Year 2nd Sem
Uploaded by
rodentCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Oral Revalida 2nd Year 2nd Sem
Oral Revalida 2nd Year 2nd Sem
Uploaded by
rodentCopyright:
Available Formats
PRE-ECLAMPSIA & ECLAMPSIA
PREDISPOSING FACTORS PRECIPITATING FACTORS
• Multiple gestation • Hypertension
• First pregnancy • Diabetes
• Mothers younger than 18 • Obesity
and older than 35 • Family history
• Diabetes
• PIH with previous
pregnancy
• Kidney disease
DIAGNOSTIC TESTS ETIOLOGY
• Urinalysis (kidney • Exact cause is unclear
function test) • Development of
• Blood test (liver function abnormal placenta
test)
• Ultrasound
• BP Monitoring
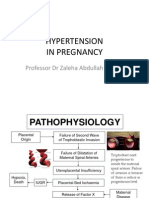
PATHOGENESIS
SIGNS & SYMPTOMS
• Gestational hypertension – BP 140/90 mmHg, systolic pressure elevated above 30 mmHg or diastolic pressure elevated 15 mmHg above pre-pregnancy
level, NO PROTEINURIA, NO EDEMA, BLOOD PRESSURE RETURNS TO NORMAL AFTER BIRTH.
• Pre-eclampsia WITHOUT severe features - BP 140/90 mmHg, systolic pressure elevated above 30 mmHg or diastolic pressure elevated 15 mmHg above
pre-pregnancy level, PROTEINURIA of +1 to +2 ON A RANDOM SAMPLE, WEIGHT GAIN OVER 2 LB/WEEK IN 2ND TRIMESTER AND 1 LB/WEEK IN 3RD
TRIMESTER, MILD EDEMA IN UPPER EXTREMITIES OR FACE
• Pre-eclampsia WITH severe features – BP 160/110 mmHg, PROTEINURIA of +3 to +4 ON A RANDOM SAMPLE AND 5g ON A 24-HOUR SAMPLE, OLIGURIA
(500 ML OR LESS IN 24 HOURS OR ALTERED RENAL FUNCTION TESTS, ELEVATED SERUM CREATININE MORE THAN 1.2 mg/dl), CEREBRAL OR VISUAL
DISTURBANCES (BLURRED VISION), PULMONARY OR CARDIAC INVOLVEMENT, EXTENSIVE PERIPHERAL EDEMA, HEPATIC DYSFUNCTION,
THROMBOCYTOPENIA, EPIGASTRIC PAIN
• Eclampsia – Either SEIZURE or COMA accompanied by signs and symptoms of pre-eclampsia are present.
IF TREATED IF TREATED
PHARMACOLOGICAL MANAGEMENT: SURGICAL MANAGEMENT:
IF TREATED • CNS depressant: Magnesium Sulfate (MgSO4) drug • Cesarian delivery
MEDICAL MANAGEMENT: of choice.
• Proteinuria monitoring • Action: CNS Depressant/ Anti Convulsive Drug
• Assess neurological Route Site: IM/IV 1st dose– IV; 2nd dose–
status, vision, changes, buttocks.
and headache • Before giving the 2nd dose: check for the IF TREATED
• Evaluate high BP (2 following: NURSING MANAGEMENT:
separate recordings; 4-6 o BP - increased or decreased Risk for injury r/t decreased
hours interval) o Urine output - 30 cc/hr; if less than 30 uteroplacental perfusion
• Assess for edema cc/hr, hold the 2nd dose, notify the • Ensure adequate
• Monitor weight changes physician at one and document the hydration.
(>2 lbs/week) findings. • Note for signs of fetal
• Left side lying, bed rest, o Check for kneejerk (+) or (-) DTR, if (-), distress.
fetal monitoring hold the 2nd dose, notify the • Fetal monitoring.
• Assess for signs of physician at once. • Encourage CBR.
seizures o Knee jerk is a sign of MgSo4 toxicity. • Administer medications
• Protein rich diet o Give antidote: Calcium Gluconate as prescribed.
(1Kg/day), watch out for • Corticosteroids – lung expansion of fetus
excessive salt intake (Betamethasone)
• Monitor intake & • Hydralazine, Labetalol, Nifedipine – anti-
output hypertensive drug
REVIEWER BY: ARIEL MAEGAN BENJAMIN
IF TREATED IF NOT TREATED
NURSING MANAGEMENT: • Organ failure
Impaired gas exchange r/t altered oxygen- • Stroke brain injury
carrying capacity of blood • Abruptio Placenta
• Monitor VS. • HELLP Syndrome
• Perform chest physiotherapy
techniques.
• Elevate head of bed and position of
patient into side-lying position to
BAD PROGNOSIS
maintain airway.
• Maternal and fetal death
• Provide oxygen as prescribed.
• Administer medication as
prescribed.
Acute pain r/t liver injury and swelling
• Position patient to take pressure
off liver.
• Provide comfort measures.
• Encourage verbalization of feelings
about pain.
• Administer medications as
prescribed.
• Teach relaxation technique such as
deep breathing exercise.
GOOD PROGNOSIS
Safe delivery and survival of the mother and
infant.
REVIEWER BY: ARIEL MAEGAN BENJAMIN
PLACENTA PREVIA
PREDISPOSING FACTORS PRECIPITATING FACTORS
• Old age • Smoking
• Multiple placenta • Intake of alcoholic
• Twins or triplets beverages
• Scarring from surgery • Recreational drugs
fibroid removal
• C-Section
• History of placenta previa
in the past pregnancy
ETIOLOGY
DIAGNOSTIC TESTS • Exact cause is unclear
• 20-week prenatal • Possibly because of upper uterus not
ultrasound well vascularized; damage from:
o Previous CS
o Abortion
o Uterine surgery
o Multiparity
PATHOGENESIS
Increase progesterone and estrogen level Pre-embryonic stage Production of fertilize ovum Implantation in the uterus
Placenta migrates to
Placenta resides in the lower where there is sufficient Insufficient blood supply Placenta arise from trophoblasts tissues
segment blood supply
IF TREATED SIGNS & SYMPTOMS IF NOT TREATED
MEDICAL MANAGEMENT: • Painless, bright red bleeding • Blood loss
• Pelvic rest • Relaxed soft uterus, non-tender • Hypoxia & premature
• UTZ • Episodes of bleeding (Minor and major bleeding) delivery of fetus
• Bed rest • Visible bleeding (not spotting)
• Bleeding; hospitalized • Intercourse post bleeding
• Monitor VS • Abnormal fetal position
• Side-lying position POOR PRONOSIS
• CBC • Placenta accreta occurs
• Clotting levels when placenta grows
deeply into uterine wall.
In placenta accreta, parts
of placenta are attached
IF TREATED which can cause severe
PHARMACOLOGICAL MANAGEMENT: blood loss after delivery.
• Corticosteroids – acts as an
anti-inflammatory and
immunosuppressive agent
(Betamethasone)
• Tocolytics
IF TREATED
SURGICAL MANAGEMENT:
• Cesarian delivery
IF TREATED
NURSING MANAGEMENT:
Decreased cardiac output r/t altered contractility
• Monitor vital signs frequently, including blood pressure, heart rate, and oxygen saturation.
• Assist with positioning the patient to optimize cardiac output, such as elevating the head of the bed or placing the patient in a semi-Fowler's position.
• Monitor fluid balance closely, including intake and output measurements.
• Administer medications as prescribed to improve cardiac contractility.
• Provide oxygen therapy as ordered to improve tissue oxygenation as prescribed.
REVIEWER BY: ARIEL MAEGAN BENJAMIN
IF TREATED
NURSING MANAGEMENT:
Impaired fetal gas exchange r/t altered blood flow
• Monitor fetal heart rate and uterine contractions regularly.
• Assist the mother in maintaining a left lateral position to optimize blood flow to the placenta.
• Encourage adequate rest and stress reduction techniques to promote optimal uterine perfusion.
• Monitor maternal blood pressure and intervene promptly if hypertension is present.
• Administer oxygen therapy to the mother as ordered to improve fetal oxygenation.
Risk for maternal and fetal injury r/t poor uteroplacental perfusion
• Monitor maternal and fetal vital signs frequently.
• Assess uterine activity and fetal well-being regularly, including fetal movement counts.
• Encourage adequate hydration and nutrition to optimize placental function.
• Assist the mother in maintaining a comfortable position to promote uteroplacental perfusion.
• Administer medications as prescribed to manage conditions such as hypertension or preterm labor.
GOOD PRONOSIS
• Safe delivery and survival
of the mother and infant.
REVIEWER BY: ARIEL MAEGAN BENJAMIN
ABRUPTIO PLACENTA
PREDISPOSING FACTORS PRECIPITATING FACTORS
• Abdominal trauma • Smoking
• Loss in uterine volume • Intake of alcoholic
• Umbilical cord prolapse beverages
(common) • Chorioamnionitis
• PIH
• Pre-eclampsia
• Multiparity
• Rupture of membrane (24hrs)
ETIOLOGY
DIAGNOSTIC TESTS • Exact cause is unclear
• Imaging/Ultrasound • Possibly causes:
o Trauma/Injury to abdomen
• Blood or blood-stained
o Rapid loss of amniotic fluid
amniotic fluid
o Previous history of
abruption
PATHOGENESIS
1. Immediate cause of placental separation: rupture of maternal vessels in the decidua basalis
2. Bleeding originates: fetal-placental vessels
3. Decidua basalis separates with its placental attachment from the uterus
4. When bleeding starts it now causes hemorrhage because of the rupture vessels
5. Detached portion of placenta: unable to exchange gasses and nutrients
6. Remaining fetoplacental unit is unable to compensate the fetus is compromised.
a. Separation of uterine wall and decidua basalis
b. Cause of degeneration of arteries
c. As bleeding starts it causes hemorrhage because of the ruptured vessels
d. Separation of placenta
SIGNS & SYMPTOMS
IF TREATED • Dark red bleeding (PAINFUL) IF NOT TREATED
MEDICAL MANAGEMENT: • Extended fundal height • Maternal: Death,
• Fluid and blood • Tender uterus hypovolemic shock, renal
replacement • Abdominal pain failure, DIC
• Oxygen inhalation • Concealed bleeding (RETROPLACENTAL) • Fetal: Death, hypoxic
• Monitor blood loss and • Hard abdomen brain injury, neonatal
fetal distress • Experience DIC (Disseminated Intravascular anemia, congenital
• CBR (lateral) Coagulation) malform
• Distressed
IF TREATED POOR PRONOSIS
PHARMACOLOGICAL • If bleeding continues,
MANAGEMENT: fetal demise may occur
• Corticosteroids – standard and 5-8% of maternal
of care for women at risk IF TREATED death.
of preterm delivery to NURSING MANAGEMENT:
decrease respiratory Acute pain r/t uterine contraction
distress syndrome and • Monitor time, frequency, intensity, and duration of
mortality. contractions
(Betamethasone and • Encourage patient to do CBR
Dexamethasone) • Provide comfort measures
• Tocolytics – May allow for • Administer medications as prescribed
the effective • Evaluate the effectiveness of pain control
administration of Impaired gas exchange r/t altered oxygen-carrying capacity of
glucocorticoids to the blood
preterm fetal to
• Monitor VS
accelerate fetal lung
• Encourage to do breathing techniques
maturation. (MgSO4,
• Elevate head of bed/position of client to maintain airway
Nifedipine)
• Provide oxygen as prescribed
• Administer medication as prescribed
Risk for infection r/t partial or total separation of placenta
• Monitor VS
IF TREATED
SURGICAL MANAGEMENT: • Note signs of infection through monitoring if the patient
has fever, positive blood cultures and altered levels of
• Cesarian delivery
consciousness GOOD PRONOSIS
• Hysterectomy: Only
• Provide comfort measures • Safe delivery and
performed if mother
developed DIC to prevent • Assess the abdominal girth survival of the
• Administer medication as prescribed mother and infant.
exsanguinations
REVIEWER BY: ARIEL MAEGAN BENJAMIN
TETRALOGY OF FALLOT
PREDISPOSING FACTORS PRECIPITATING FACTORS
• Mother old than 40yrs old • Maternal viral infection:
• Parents with TOF Rubella
• Presence of down syndrome or • Poor nutrition
DiGeorge syndrome • Alcohol use
ETIOLOGY
DIAGNOSTIC TESTS • Exact cause is unclear
• Echocardiography • Possibly causes:
• Chest X-ray o Risk factors
o May be genetic
• Electrocardiogram
PATHOGENESIS
Congenital heart defect with 4 structural defects: Ventricular septal defect, pulmonary stenosis, right ventricular hypertrophy, and overriding aorta.
1. Pulmonary stenosis – narrowing of right ventricular outflow tract into the pulmonary artery
2. Ventricular septal defect – gap between ventricles, absence or damaged septum
3. Overriding aorta – deoxygenated blood is shunted from right to left, flows over to left ventricle-immediate out
4. Right ventricular hypertrophy – occurs secondary to pulmonary stenosis, myocardium contracts harder to push blood past stenosis
TOF order: VSD, PULOMARY STENOSIS, RIGHT VENTRICULAR HYPERTROPHY, OVERRIDING AORTA
IF TREATED SIGNS & SYMPTOMS IF NOT TREATED
MEDICAL MANAGEMENT: • Tet Spell: Cyanotic, SOB, Increased RR • Congestive heart failure
• Open heart surgery • Need for chest positioning or squatting • Blood clots
• Clubbing • Bacterial endocarditis
• Fatigue • Arrhythmias
• Trouble feeding
IF TREATED • Systemic murmur
PHARMACOLOGICAL • Smaller for their age
MANAGEMENT: POOR PRONOSIS
• Phenylephrine • Death
• Propranolol
• Furosemide
• Alprostadil – a
IF TREATED
vasodilator; first-line
NURSING MANAGEMENT:
palliative therapy to
Decreased cardiac output r/t structural factors of congenital
temporarily maintain
heart defects
patency of the ductus
• Monitor VS.
arteriosus (DA) before
• Provide adequate rest periods
surgery
• Position in semi-fowler’s position
• Administer oxygen as prescribed
• Administer medications as prescribed
IF TREATED Activity intolerance r/t imbalanced oxygen supply and
SURGICAL MANAGEMENT: demand
• VSD closure • Monitor VS
• Pulmonary valve repair • Provide toys and comfort measures for quiet play
• Right ventricular outflow and to divert attention
tract anomaly correction • Provide adequate rest periods
• Blalock-Taussig (BT) Shunt • Administer oxygen as prescribed GOOD PRONOSIS
Is a placement of a • Administer medications as prescribed • Long-term survival
conduit between Risk for infection r/t chronic illness
subclavian artery and • Monitor VS
pulmonary artery for • Assess temperature, IV site if present, increased
stable pulmonary blood WBC
flow. • Perform hand hygiene and maintain sterile
technique when performing a procedure
• Provide adequate rest and nutritional needs for
age.
• Administer antibiotics as prescribed
REVIEWER BY: ARIEL MAEGAN BENJAMIN
GESTATIONAL DIABETES MELLITUS
PREDISPOSING FACTORS PRECIPITATING FACTORS
• Maternal over 35yrs old • Macrosomia
• Obesity • Multiple pregnancy
• Assessment of history
DIAGNOSTIC TESTS
ETIOLOGY
• Screening at 24-28 weeks A hormone made by the placenta prevents the
of gestation body from using insulin effectively. Glucose builds
• Fasting blood glucose up in the blood instead of being absorbed by the
• Random blood glucose cells.
PATHOGENESIS
1. Glucose intolerance
2. B-cells release insulin
3. Insulin resistance
4. Hyperglycemia
➢ Maternal circulation
➢ Increase blood glucose will have signs & symptoms of:
o Polyuria – increased amount of urine
o Polyphagia – excessive eating
o Polydipsia – excessive thirst
o Paresthesia – burning sensation on parts of the body
➢ Fetal circulation
o Increase glucose in fetus
o Increase insulin
o Increase growth of the baby
IF TREATED SIGNS & SYMPTOMS IF NOT TREATED
MEDICAL MANAGEMENT: • GDM does not show noticeable signs & symptoms, Maternal:
• Monitor urine output however, possible symptoms can be: • Risk of infection
• Monitor glucose and o Polyuria – increased amount of urine • Cesarean section
weight o Polyphagia – excessive eating • 50% risk of
• Consult dietitian o Polydipsia – excessive thirst developing DM TYPE 2
o Paresthesia – burning sensation on parts • Insulin related
of the body hypoglycemia
o Fetal:
IF TREATED • Excessive birth weight
IF TREATED • Preterm birth
PHARMACOLOGICAL NURSING MANAGEMENT:
MANAGEMENT: • Stillbirth
Deficient knowledge r/t gestational diabetes
• Insulin: Primary and • Establish rapport
initiated if the initial • Assess patient’s current knowledge regarding the disease
measure fails to achieve process, management, effects on pregnancy, and
glycemic goals POOR PRONOSIS
potential complications
• Metformin • The risk of a mother
• Explain pathophysiology aspects of diabetes, effects on
• Glyburide pregnancy, and potential complications. Explain principles
getting a gestational
diabetes again in a
of diabetic diet and have patient plan her meals
future pregnancy is
• Develop an individualized care plan based on the woman's
between 30%-84%. If
specific needs, preferences, and cultural background.
the second pregnancy
IF TREATED • Demonstrate procedure for insulin administration and
occurs within a year
SURGICAL MANAGEMENT: obtain return demonstration
after the first
• C-Section Anxiety r/t to threat to maternal and fetal well-being
pregnancy, the
• Establish rapport
recurrence is higher.
• Listen to patient’s feelings and concerns
• Provide therapeutic communication and promote open
relationship with patient
• Review potential dangers by providing factual information
• Encourage patient to share concerns with healthcare GOOD PRONOSIS
team • GDM is resolved after
Risk for fetal injury r/t elevated maternal glucose levels baby is born. However,
• Assess patient’s current diabetic control the mother can
• Provide education on proper nutrition develop the condition
• Encouraging the pregnant person to engage in regular again in any future
physical activity and maintain a healthy weight can help pregnancies.
control glucose levels.
• Monitor fundal height during each prenatal visit
• Assess fetal movement and heart rate during each
prenatal visit.
REVIEWER BY: ARIEL MAEGAN BENJAMIN
RHEUMATIC HEART DISEASE
PREDISPOSING FACTORS PRECIPITATING FACTORS
• Age (5-15) • Poor hand hygiene/hygiene
• Contracting scarlet fever • Skipping antibiotics
• Children who get repeated strep throat • Crowded places at higher-risk of
infections contracting group A strep
• Family history of RHD • Reduced access to medical care
DIAGNOSTIC TESTS ETIOLOGY
• Blood test Caused by one or several episodes of rheumatic fever, an
• Cardiac MRI autoimmune inflammatory reaction to throat infection
with group A streptococci. It most commonly occurs in
• Echocardiogram
childhood, and can lead to death or life-long disability.
• ECG
• Chest X-ray
PATHOGENESIS
IF TREATED SIGNS & SYMPTOMS IF NOT TREATED
MEDICAL MANAGEMENT: • SOB • Heart failure
• CBR • Chest Pain • Bacterial endocarditis
• Monitor VS, cardiac • Swelling (stomach, hands or feet) • Ruptured heart valve
rhythms, and • Heart murmur • Complications of
hemodynamics pregnancy and
• Avoid Valsalva delivery due to heart
• Limit activities damage
IF TREATED
NURSING MANAGEMENT:
Decreased cardiac output r/t valve dysfunction of heart failure
• Closely monitor fluid intake
IF TREATED POOR PRONOSIS
• Monitor for dysrhythmias
PHARMACOLOGICAL • The disease is
• Observe patient for understanding and compliance of
MANAGEMENT: permanent and
with medical regimen
• Anticoagulants – to requires long-term
• Administer oxygen therapy as prescribed
reduce risk of stroke or care
• Identify an emergency plan
blood clots (Warfarin) Activity intolerance r/t swelling in legs
• Antibiotics – prevent • Teach energy conservation techniques
further infection • Dangle the legs from the bedside for 10-15 mins
(Penicillin G benzathine)
• Refrain from performing non-essential activities or
procedures
• Assist with ADL
• Encourage physical activity consistent with the patient’s
IF TREATED energy levels
SURGICAL MANAGEMENT: Risk for infection r/t damaged heart vessels and potential
• Mitral valve replacement endocarditis
• Regularly monitor the patient for signs and symptoms of
infection, such as fever, chills, fatigue, and malaise
• Stress the importance of frequent handwashing with soap
and water, especially before eating, after using the GOOD PRONOSIS
restroom, and after coughing or sneezing. • Well-managed
• Encourage a balanced diet rich in fruits, vegetables, and rheumatic heart
lean proteins to support the immune system. disease can enjoy high
• Ensure that the patient receives appropriate antibiotic quality of life.
prophylaxis before dental procedures or other invasive
medical procedures as prescribed.
• Provide thorough education to the patient and their
family about the importance of good oral hygiene
practices, including regular brushing, flossing, and dental
check-ups.
REVIEWER BY: ARIEL MAEGAN BENJAMIN
You might also like
- 300+ TOP Digestive System MCQs and Answers PDF Quiz ExamDocument11 pages300+ TOP Digestive System MCQs and Answers PDF Quiz ExamMuhammad AliNo ratings yet
- Bài Trình Tiền Sản GiậtDocument21 pagesBài Trình Tiền Sản Giậttrongnguyen2232000No ratings yet
- MCN ReviewerDocument4 pagesMCN ReviewerMaria Arabella LanacaNo ratings yet
- Hypertensive Disorders of Pregnancy: Mrs - Jagadeeswari.J M.SC NursingDocument46 pagesHypertensive Disorders of Pregnancy: Mrs - Jagadeeswari.J M.SC Nursingbenikkphotos4No ratings yet
- RHU Guide for PGIs and ClerksDocument2 pagesRHU Guide for PGIs and ClerksAliya Lopez BacaramanNo ratings yet
- Module 3 - Maternal TransesDocument7 pagesModule 3 - Maternal TransesCarl UyNo ratings yet
- Plications of PregnancyDocument45 pagesPlications of PregnancyDEOGRATIAS NDAYISABANo ratings yet
- Maternal and Child Nursing (PIH, GDM, HELLP Syndrome, Eclampsia and Pre-Eclampsia)Document6 pagesMaternal and Child Nursing (PIH, GDM, HELLP Syndrome, Eclampsia and Pre-Eclampsia)PAULINE BERNICE BAGUIONo ratings yet
- Pregnancy Induced Hypertension: Definition of TermsDocument6 pagesPregnancy Induced Hypertension: Definition of TermsPAULINE BERNICE BAGUIONo ratings yet
- Hypertensive Disorders of Pregnancy: S.L.Dr. Lavinia SteleaDocument44 pagesHypertensive Disorders of Pregnancy: S.L.Dr. Lavinia Steleamajd danNo ratings yet
- 3 Hypertension in PregnancyDocument36 pages3 Hypertension in PregnancySwee WaiNo ratings yet
- Plications of PregnancyDocument16 pagesPlications of Pregnancycharleneoconnor82No ratings yet
- LR ProtocolDocument159 pagesLR ProtocolJeevan VelanNo ratings yet
- Gestational 1Document8 pagesGestational 1RoseAngelyne VicenteNo ratings yet
- SEMINAR HYPERTENSION DISORDER DURING PREGNANCY ContentDocument19 pagesSEMINAR HYPERTENSION DISORDER DURING PREGNANCY ContentMonika shankar100% (2)
- Hypertensive Disorders of Pregnancy: Priyanka GehlotDocument50 pagesHypertensive Disorders of Pregnancy: Priyanka GehlotpriyankaNo ratings yet
- Guidelines For The Management of Hypertensive Disorders of Pregnancy 2008Document5 pagesGuidelines For The Management of Hypertensive Disorders of Pregnancy 2008Firah Triple'sNo ratings yet
- Mini-OSCE Simulation: Hypertensive Disorders in PregnancyDocument16 pagesMini-OSCE Simulation: Hypertensive Disorders in PregnancyNinaNo ratings yet
- Obstetrics Study Guide 3: Mitra Ahmad Soltani 2008Document172 pagesObstetrics Study Guide 3: Mitra Ahmad Soltani 2008Anonymous N2PHMnTIYLNo ratings yet
- Abnormal OB Handout With Annotations December 12Document5 pagesAbnormal OB Handout With Annotations December 12sobrevegasam02No ratings yet
- m1 F. Kamwendo - Hypertensive Disorders in PregnancyDocument43 pagesm1 F. Kamwendo - Hypertensive Disorders in PregnancyRifqy Syaiful BahriNo ratings yet
- Ernawati - PIT Feto 2023 PreeklampsiaDocument21 pagesErnawati - PIT Feto 2023 PreeklampsiaHeldasari SianturiNo ratings yet
- Drug StudyDocument2 pagesDrug StudyJohn Ronnel De GuiaNo ratings yet
- Therapeutics Group 2 (09.07.2021 - Dr. Perez) - RDU On Hypertension in PREGNANTDocument15 pagesTherapeutics Group 2 (09.07.2021 - Dr. Perez) - RDU On Hypertension in PREGNANTEmerson QuimbaNo ratings yet
- Hypertensive Disorder in Pregnancy-2Document42 pagesHypertensive Disorder in Pregnancy-2CAC KK DABONGNo ratings yet
- Antenatal Care &assessment ofDocument39 pagesAntenatal Care &assessment ofxj74fr4ddxNo ratings yet
- Lecture 10 Pregnancy HTDocument18 pagesLecture 10 Pregnancy HTmajd danNo ratings yet
- Obstetric History Taking and ExaminationDocument51 pagesObstetric History Taking and Examinationmsashmita555No ratings yet
- 9.hypertensive Disorders of Pregnancy BSC Cinical SciencesDocument37 pages9.hypertensive Disorders of Pregnancy BSC Cinical Sciencesmctime35No ratings yet
- Hypertensive Disorder in Pregnancy Untuk KuliahDocument78 pagesHypertensive Disorder in Pregnancy Untuk Kuliah404notfoundNo ratings yet
- OB Part1 - 2022 FatimaDocument119 pagesOB Part1 - 2022 FatimaFemale calmNo ratings yet
- Preeclampsia Patient CaseDocument23 pagesPreeclampsia Patient Caseapi-714782423No ratings yet
- Management of Obstetric EmergenciesDocument66 pagesManagement of Obstetric Emergenciesputri azzahraNo ratings yet
- Pre Eclampsia: DR Kauser Mansoor Mrcog, Frcog Consultant & HODDocument46 pagesPre Eclampsia: DR Kauser Mansoor Mrcog, Frcog Consultant & HODRokr125No ratings yet
- ACOG 2020 SMI-hypertension-bundle-slidesDocument34 pagesACOG 2020 SMI-hypertension-bundle-slidesLuciana Salomé Bravo QuintanillaNo ratings yet
- Maternal Safety Bundle For: Severe Hypertension in PregnancyDocument34 pagesMaternal Safety Bundle For: Severe Hypertension in PregnancyCarlos MayaNo ratings yet
- PpqpsapdxzczxDocument24 pagesPpqpsapdxzczxAriff RosliNo ratings yet
- Diabetes in PregnancyDocument1 pageDiabetes in Pregnancycatcat669111No ratings yet
- If Aph Prov Pcos Primary Care Clinical Pathway 2Document21 pagesIf Aph Prov Pcos Primary Care Clinical Pathway 2lea20No ratings yet
- BSN 2C MCN Lec Transes 1 1Document4 pagesBSN 2C MCN Lec Transes 1 1Shahina ShayneNo ratings yet
- 3 - Bacterial Sepsis - Case 1Document36 pages3 - Bacterial Sepsis - Case 1koteshwara raoNo ratings yet
- Ob Revalida Review 2017 PDFDocument71 pagesOb Revalida Review 2017 PDFMara Medina - BorleoNo ratings yet
- Class Notes - Pre-EclampsiaDocument3 pagesClass Notes - Pre-Eclampsiasalqi2024No ratings yet
- NeonatologyDocument27 pagesNeonatologyA ANo ratings yet
- HYPERTENSIONDocument5 pagesHYPERTENSIONjmiavaldez CañasNo ratings yet
- Antenatal CareDocument43 pagesAntenatal CareAyubNo ratings yet
- Diabetes & UTI in PregnancyDocument34 pagesDiabetes & UTI in PregnancyIsraa AlaaNo ratings yet
- PancreatitisDocument45 pagesPancreatitisFernando ArancibiaNo ratings yet
- Hypertensive Diseases in PregnancyDocument38 pagesHypertensive Diseases in PregnancyIsraa AlaaNo ratings yet
- DM & Thyroid Disease During PregnancyDocument24 pagesDM & Thyroid Disease During Pregnancybodyb2714No ratings yet
- Pre EclampsiaDocument11 pagesPre EclampsiaAkinsoun MotunrayoNo ratings yet
- DR Haizun HassanDocument16 pagesDR Haizun HassanMarini MahmoodNo ratings yet
- Ob Revalida Samplex ZapDocument24 pagesOb Revalida Samplex ZapMariana B.No ratings yet
- Finals Pedia EncodedDocument62 pagesFinals Pedia EncodedCezanne Danabelle HutallaNo ratings yet
- Abnormal Uterine Bleeding Menstrual Cycle Abnormalities: Assist. Prof. George-Alexandru Roșu, MDDocument25 pagesAbnormal Uterine Bleeding Menstrual Cycle Abnormalities: Assist. Prof. George-Alexandru Roșu, MDRosu George100% (1)
- Med - Comp - Slides PDFDocument54 pagesMed - Comp - Slides PDFFiras KNo ratings yet
- Abruptio Placenta. Final OutputDocument15 pagesAbruptio Placenta. Final OutputCharles Loriaga Cruz IINo ratings yet
- HTN in PregnancyDocument36 pagesHTN in PregnancySalman RiazNo ratings yet
- I. Postpartal Infections CausesDocument6 pagesI. Postpartal Infections CausesJoanne GomezNo ratings yet
- Hypertension in Pregnancy NewDocument28 pagesHypertension in Pregnancy Newnandana vNo ratings yet
- Foley Catheter IntroductionDocument6 pagesFoley Catheter IntroductionMervin Ezekiel Amistoso FranciscoNo ratings yet
- CPG Management of Post-Operative Infectious EndophthalmitisDocument41 pagesCPG Management of Post-Operative Infectious EndophthalmitisnrajentranNo ratings yet
- The Penis: - Phimosis: Scarring of The Prepuce Which Will Not Retract Without FissuringDocument20 pagesThe Penis: - Phimosis: Scarring of The Prepuce Which Will Not Retract Without FissuringWorku KifleNo ratings yet
- The Marketing Mix of Apollo Hospitals Discusses The Service Marketing Mix or The 7PDocument12 pagesThe Marketing Mix of Apollo Hospitals Discusses The Service Marketing Mix or The 7Pwaseem100% (1)
- 3020 Unfolding Case Study Burns 1Document2 pages3020 Unfolding Case Study Burns 1api-546391110No ratings yet
- Urology TURPDocument2 pagesUrology TURPvilla88No ratings yet
- ANATOMY SHORT ANSWER QUESTIONS BANK September 2009Document4 pagesANATOMY SHORT ANSWER QUESTIONS BANK September 2009IGA ABRAHAMNo ratings yet
- Nerves of Upper LimbDocument13 pagesNerves of Upper LimbHafiz NaveedNo ratings yet
- System CardiovascularDocument22 pagesSystem Cardiovascularvk seruniNo ratings yet
- Histopath Lab (Module 2) : Receiving, Accessioning and Gross Examination of Tissue SamplesDocument5 pagesHistopath Lab (Module 2) : Receiving, Accessioning and Gross Examination of Tissue SamplesAngela ReyesNo ratings yet
- AnesDocument10 pagesAnesVenice Louisse Ranoa GuinitaNo ratings yet
- Digestive System Respiratory System Cardiovascular SystemDocument22 pagesDigestive System Respiratory System Cardiovascular SystemYuki MendezNo ratings yet
- Cerebrovascular DiseasesDocument16 pagesCerebrovascular DiseasesSopna ZenithNo ratings yet
- Chest ThesisDocument6 pagesChest Thesiskcfxiniig100% (1)
- Regenerative EndodonticsDocument7 pagesRegenerative EndodonticsEsha AroraNo ratings yet
- Brochure CPC SurgeryDocument4 pagesBrochure CPC SurgeryNoor MohammedNo ratings yet
- When Your Waters Break EarlyDocument5 pagesWhen Your Waters Break EarlyaurroritaNo ratings yet
- Management For PterygiumDocument22 pagesManagement For PterygiumAndie AlbinoNo ratings yet
- DOH 1 Ozident Einas 2020Document15 pagesDOH 1 Ozident Einas 2020Farha Navas100% (1)
- Jopr 12544Document5 pagesJopr 12544shilpapremarajan213No ratings yet
- Complete Download Topographical and Pathotopographical Medical Atlas of the Human Body 1st Edition Z. M. Seagal PDF All ChaptersDocument62 pagesComplete Download Topographical and Pathotopographical Medical Atlas of the Human Body 1st Edition Z. M. Seagal PDF All Chapterspaakowslaveq100% (1)
- Ent Surgical Consultants: What Is Reflux?Document3 pagesEnt Surgical Consultants: What Is Reflux?YofindaNo ratings yet
- STT Tecnica QuirúrgicaDocument5 pagesSTT Tecnica QuirúrgicaNathaly GuevaraNo ratings yet
- Understanding PV Loops Ebook RPV 2 WBDocument24 pagesUnderstanding PV Loops Ebook RPV 2 WBVimal NishadNo ratings yet
- Periodontal Microsurgery: Home Mcq's Discussions ContactDocument8 pagesPeriodontal Microsurgery: Home Mcq's Discussions Contactdileep9002392No ratings yet
- Don Interstitial BrachytherapyDocument53 pagesDon Interstitial BrachytherapyRajalakshmi RadhakrishnanNo ratings yet
- Lower eyelid blepharoplasty An overviewDocument9 pagesLower eyelid blepharoplasty An overviewDenisse MejiaNo ratings yet
- Peptic Ulcer DiseaseDocument45 pagesPeptic Ulcer DiseaseKulgaurav RegmiNo ratings yet
- Nueva Ecija University of Science and Technology: ActivityDocument26 pagesNueva Ecija University of Science and Technology: ActivityBeverly DatuNo ratings yet