Lyme Disease
Lyme Disease
Uploaded by
SanderCopyright:
Available Formats
Lyme Disease
Lyme Disease
Uploaded by
SanderOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Lyme Disease
Lyme Disease
Uploaded by
SanderCopyright:
Available Formats
LYME DISEASE FACT SHEET
BACKGROUND
Lyme Disease (LD) is a tick-borne zoonosis (a disease shared between animals and people) caused by infection with the
spirochete, Borrelia burgdorferi that is transmitted to people through the bite of an infected tick. Ixodes scapularis (the
blacklegged or deer tick) is the type of tick that carries LD in Pennsylvania. The number of annually reported cases of LD
in the United States has increased about 25-fold since reporting began in 1982. In the United States, the disease is mostly
localized to the northeastern, mid-Atlantic, and upper Midwest regions, and in northwestern California. Pennsylvania has
reported between 8,000-10,000 LD cases annually in recent years. Every county in Pennsylvania typically reports a LD
incidence higher than the national average.
WHO DOES THE ISSUE IMPACT?
a. Season: An individual’s risk of developing LD depends on each person’s likelihood of being bitten by tick vectors
infected with B. burgdorferi. This likelihood is primarily determined by the density of vector ticks in the
environment (which varies by place and season), the prevalence of B. burgdorferi infection in vector ticks, and by
the extent of person-tick contact, which is related to the type, frequency, and duration of a person’s activities in
a tick infested environment. The highest risk of LD is when nymphal deer ticks are in the environment in June and
July, however, LD can be transmitted by adult deer ticks any time of year.
b. Location: Most B. burgdorferi infections are thought to result from exposure to ticks around the home during
property maintenance, recreation, and leisure activities. Thus, individuals who live or work in residential areas
surrounded by woods or overgrown brush infested by vector ticks are at higher risk of getting LD.
c. Activities: In addition, persons who participate in recreational activities away from home such as hiking, camping,
fishing and hunting in tick habitats, and persons who engage in outdoor occupations, such as landscaping, brush
clearing, forestry, and wildlife and parks management in endemic areas may also be at risk of getting LD. When in
highly endemic areas, individuals can reduce their risk of LD by avoiding tick infested habitat. If exposure to tick
infected habitat cannot be avoided, individuals may reduce their risk of infection by applying repellents, wearing
protective clothing, and regularly checking for and removing attached ticks.
COMPLICATIONS
LD is a multi-system, multi-stage, inflammatory illness. In its early stages, the disease is readily treated with oral antibiotics;
however, untreated or inadequately treated infection may progress to late-stage arthritic, cardiac, or nervous system
complications requiring more intensive therapy.
SIGNS AND SYMPTOMS
LD most often presents with a characteristic rash, erythema migrans (EM), which can sometimes look like a bullseye. It
may also be accompanied by nonspecific symptoms such as fever, malaise, fatigue, headache, muscle aches and joint pain.
The incubation period, the time from infection to onset of EM, is typically 7 to 14 days but may be as short as 3 days and
as long as 30 days. EM is observed in 70-80% of cases with early symptomatic infection; however, some infected individuals
have no recognized illness, or have only non-specific symptoms suggesting viral illness, such as fever, headache, fatigue,
and muscle aches.
February 10, 2022
CAUSES AND TRANSMISSION
The Lyme disease bacterium, Borrelia burgdorferi, is spread through the bite of infected ticks. The blacklegged tick (or
deer tick, Ixodes scapularis) spreads the disease in the northeastern, mid-Atlantic, and north-central United States. The
western blacklegged tick (Ixodes pacificus) spreads the disease on the Pacific Coast.
TESTS AND DIAGNOSIS
LD is diagnosed based on symptoms, objective findings (such as EM, facial palsy, or arthritis), and a history of possible
exposure to infected ticks. However, since LD is endemic in Pennsylvania and infected deer ticks are found in all counties
in Pennsylvania, all Pennsylvanians are considered potentially exposed. Furthermore, many persons do not recall a tick
bite prior to their LD diagnosis, so the presence or absence of a known tick bite should never be a determining factor in
diagnosing LD. Blood tests are also performed to detect the body’s immune response to the infection. Not all patients
with LD will develop the characteristic bulls-eye rash (EM) and early blood tests may be negative in persons who are
infected with LD.
TREATMENTS
The consequences of LD can be significantly reduced by detecting and treating the infection in its early stages with
standard antibiotic regimens, since early and correct treatment usually results in a prompt and uncomplicated resolution
of symptoms. Early and uncomplicated infection, including infection presenting with isolated cranial nerve palsy, almost
always responds satisfactorily to treatment with orally administered antibiotics. Intravenous antibiotics are generally
recommended for treating meningitis, later stage neurologic LD, and complicated LD arthritis. Late, complicated LD may
respond slowly or incompletely. A minority of patients have persistent or recurrent symptoms following appropriate
antibiotic therapy. These symptoms may be due to causes other than persisting infection and may be due to tissue
damage caused during active infection.
WHAT CAN YOU DO?
To prevent LD:
• The risk of being bitten by an infected tick can be decreased by using the following precautions:
o Use insect repellent containing low concentrations (10 to 30%) of diethyltoluamide (DEET) on clothing
and exposed skin;
Apply DEET sparingly on exposed skin. Do not apply to the face. Do not use under clothing.
Do not use DEET on the hands of young children. Avoid applying to areas around the eyes and
mouth.
Do not use DEET over cuts, wounds or irritated skin. Wash treated skin with soap and water
after returning indoors, and wash treated clothing.
Avoid spraying in enclosed areas. Do not use DEET near food.
o Avoid tick-infested areas;
o Wear light colored clothing so ticks can be spotted more easily;
o Tuck pant legs into socks or boots, and shirts into pants;
o Tape the areas where pants and socks meet;
o Wear a hat, long sleeved shirt, and long pants for added protection;
o Walk in the center of trails to avoid overhanging brush; and
February 10, 2022
o Check yourself, family members and pets for ticks after leaving potentially tick infested areas and
promptly remove any ticks detected.
If you find a tick:
• If you find a tick attached to your skin, there is no need to panic. There are several tick removal devices on
the market, but a plain set of fine-tipped tweezers will remove a tick quite effectively. Prompt and proper
tick removal is very important for preventing possible disease transmission.
o Use fine-tipped tweezers and protect your fingers with a tissue, paper towel, or latex gloves. Avoid
removing ticks with your bare hands.
o Grasp the tick as close to the skin surface as possible and pull upward with steady, even pressure.
Don't twist or jerk the tick; this can cause the mouth-parts to break off and remain in the skin. If this
happens, remove the mouth-parts with tweezers. If you are unable to remove the mouth easily with
clean tweezers, leave it alone and let the skin heal.
o After removing the tick, thoroughly disinfect the bite and your hands with rubbing alcohol, an iodine
scrub, or soap and water.
o Avoid folklore remedies such as "painting" the tick with nail polish or petroleum jelly or using heat
to make the tick detach from the skin. Your goal is to remove the tick as quickly as possible; do not
wait for it to detach.
If you suspect that you or a family member might have LD:
• See your healthcare provider if you become ill after having been bitten by a tick or having spent time
outdoors participating in activities that may result in tick bites like hiking, camping, yard work, gardening,
fishing, hunting, dog walking, etc.
RESOURCES FOR MORE INFORMATION
PA DOH Vectorborne Disease webpage: Vectorborne Diseases
CDC LD website: https://www.cdc.gov/lyme/index.html
This fact sheet provides general information. Please contact your physician for specific clinical information.
If you have any questions, contact us at 1-877-PA-HEALTH.
February 10, 2022
You might also like
- St. Louise de Marillac College of BogoDocument44 pagesSt. Louise de Marillac College of BogoRenz LephoenixNo ratings yet
- Lyme Disease Brochure TemplateDocument2 pagesLyme Disease Brochure Templatetburkle50% (2)
- L1-Overview of The Infection Prevetion and ControlDocument6 pagesL1-Overview of The Infection Prevetion and Controldmutethia68No ratings yet
- Lyme DiseaseDocument5 pagesLyme DiseaseTotoJostNo ratings yet
- PediculosisDocument14 pagesPediculosisREYMARK HACOSTA100% (1)
- About Lyme DiseaseDocument4 pagesAbout Lyme DiseasekrobinetNo ratings yet
- The Outbreak of Coronavirus: The COVID-19 Pandemic in IndonesiaDocument3 pagesThe Outbreak of Coronavirus: The COVID-19 Pandemic in IndonesiaSyaira azzhavira 8ANo ratings yet
- Group#1 (Vector Born Disease & Control StratgiesDocument24 pagesGroup#1 (Vector Born Disease & Control StratgiesAli RizwanNo ratings yet
- Teaching Care Plan For DengueDocument5 pagesTeaching Care Plan For Denguemarielle_della100% (1)
- Fast Facts On Dengue FeverDocument13 pagesFast Facts On Dengue Fevermuhammad aslamNo ratings yet
- Lyme DiseaseDocument3 pagesLyme DiseaseSanderNo ratings yet
- Erbil Polythecnic University Soran Technical Insititute Midwifery Dipartment First Stage (M)Document13 pagesErbil Polythecnic University Soran Technical Insititute Midwifery Dipartment First Stage (M)Kubra ĖdrisNo ratings yet
- What Is Dengue Fever?Document2 pagesWhat Is Dengue Fever?Yan Sheng HoNo ratings yet
- A Widespread Occurrence of An Infectious Disease in A Community at A Particular TimeDocument6 pagesA Widespread Occurrence of An Infectious Disease in A Community at A Particular TimeHaris KhanNo ratings yet
- HFMDDocument2 pagesHFMDHarry FebryantoNo ratings yet
- Educators Lyme Disease and TicksDocument10 pagesEducators Lyme Disease and TicksRICHARD RODERICK OLMEDONo ratings yet
- Coronavirus Prevention: How to Keep your Immune System Strong & Reduce your Risk of DiseaseFrom EverandCoronavirus Prevention: How to Keep your Immune System Strong & Reduce your Risk of DiseaseNo ratings yet
- 3q Health l2 Common Communicable Diseases 1Document50 pages3q Health l2 Common Communicable Diseases 1roseteelaizaNo ratings yet
- Assignment IndividualDocument10 pagesAssignment Individualkartini272597No ratings yet
- Presentation on Reopening of School Post Covid19Document57 pagesPresentation on Reopening of School Post Covid19anupamaakhaitan82No ratings yet
- For Finals PEDocument6 pagesFor Finals PEAvery S. BaltazarNo ratings yet
- InfluenzaDocument2 pagesInfluenzajohnndoeeNo ratings yet
- (Impetigo) : Erbil Polythecnic University Soran Technical Insititute Nuraing Department First StageDocument14 pages(Impetigo) : Erbil Polythecnic University Soran Technical Insititute Nuraing Department First StageKubra ĖdrisNo ratings yet
- Nidovirales, and Realm Riboviria They Are Enveloped Viruses With A Positive-Sense SingleDocument4 pagesNidovirales, and Realm Riboviria They Are Enveloped Viruses With A Positive-Sense SingleAbhishekNo ratings yet
- Your Health Is: Our PriorityDocument23 pagesYour Health Is: Our PrioritynedeljkostevanovicNo ratings yet
- Dengu Awareness Month Lecture 2006Document14 pagesDengu Awareness Month Lecture 2006Jenn Botal BaguidudolNo ratings yet
- UNIT 1-Medicinal Chemistry IntroductionDocument9 pagesUNIT 1-Medicinal Chemistry Introductionshamonicah0203No ratings yet
- Dengue Fever Fact SheetDocument1 pageDengue Fever Fact Sheetiamketul6340No ratings yet
- Vorwick ScabiesDocument3 pagesVorwick ScabiesTio Norman WicaksonoNo ratings yet
- Viral MeningitisDocument20 pagesViral MeningitisFlorence ILoyd R. TorresNo ratings yet
- Hand Foot and Mouth Disease Fact SheetDocument3 pagesHand Foot and Mouth Disease Fact SheetBreixo HarguindeyNo ratings yet
- Crab EggsDocument7 pagesCrab EggsNinfa LansangNo ratings yet
- LymefsDocument2 pagesLymefsSanderNo ratings yet
- Corona VirusDocument1 pageCorona VirusLuis AriasNo ratings yet
- DengueDocument2 pagesDengueRZ Abdurrohim100% (1)
- LymeDocument7 pagesLymeSanderNo ratings yet
- Boils Skin InfectionsDocument2 pagesBoils Skin Infectionsupasana.b.1012No ratings yet
- Erbil Polythecnic University Soran Technical Insititute Midwifery Dipartment First Stage (M)Document14 pagesErbil Polythecnic University Soran Technical Insititute Midwifery Dipartment First Stage (M)Kubra ĖdrisNo ratings yet
- ImpetigoDocument1 pageImpetigoshailesh284No ratings yet
- Actividad de Nivelación Danna Diaz 10Th Grade - EnglishDocument9 pagesActividad de Nivelación Danna Diaz 10Th Grade - Englishdanna diazNo ratings yet
- Everything You Need To Know About Dengue FeverDocument10 pagesEverything You Need To Know About Dengue FeverJi AhNo ratings yet
- COVID-19 Frequently Asked Questions FINALDocument4 pagesCOVID-19 Frequently Asked Questions FINALPriskilla Grace TicoaluNo ratings yet
- Lesson: Lagonoy High School Quarter 3 Module 3Document3 pagesLesson: Lagonoy High School Quarter 3 Module 3John Mark PrestozaNo ratings yet
- Dengue Fever Advisory All IndiaDocument4 pagesDengue Fever Advisory All Indiatcforvtged.d333No ratings yet
- Common Health Problems School AgeDocument2 pagesCommon Health Problems School Age2BGrp3Plaza, Anna MaeNo ratings yet
- 336 ScabiesDocument2 pages336 ScabiesrozanfikriNo ratings yet
- What Is Coronaviruses?: FAQ: Remedial Measure To The Ongoing COVID19 OutbreakDocument4 pagesWhat Is Coronaviruses?: FAQ: Remedial Measure To The Ongoing COVID19 OutbreakNeil RiveraNo ratings yet
- What Is Dengue Fever?Document2 pagesWhat Is Dengue Fever?Sanaullah KhanNo ratings yet
- Microbiology Compilation (MRS Saliu)Document15 pagesMicrobiology Compilation (MRS Saliu)Nifemi AketanNo ratings yet
- How To ControlDocument3 pagesHow To ControlSri WahyuningsihNo ratings yet
- Covid 19 Brochure enDocument23 pagesCovid 19 Brochure enFerdinand FajardoNo ratings yet
- Lyme DiseaseDocument4 pagesLyme DiseaseSanderNo ratings yet
- Causative Agent CandidiasisDocument2 pagesCausative Agent CandidiasisDiamante MhayaleneNo ratings yet
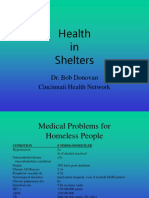
- Health in Shelters: Dr. Bob Donovan Cincinnati Health NetworkDocument47 pagesHealth in Shelters: Dr. Bob Donovan Cincinnati Health NetworkIda Bagus Udayana KramasanjayaNo ratings yet
- Scabies GuidelineJanuary 2013Document13 pagesScabies GuidelineJanuary 2013anisarahma718No ratings yet
- Oct-Nov NewsletterDocument7 pagesOct-Nov Newsletterapi-234927361No ratings yet
- ImpetigoDocument13 pagesImpetigoTasya SyafhiraNo ratings yet
- Let's Protect The EnvironmentDocument19 pagesLet's Protect The EnvironmentDevane VillanoNo ratings yet
- Signs and Symptoms of DiseaseDocument3 pagesSigns and Symptoms of DiseaseAdrian MangahasNo ratings yet
- Paper For Bio Theme Virus WD X-4Document8 pagesPaper For Bio Theme Virus WD X-4Muhammad RafiNo ratings yet
- MonkeypoxDocument4 pagesMonkeypoxTUYIZERE EmmanuelNo ratings yet
- What-Is The Novel CoronavirusDocument7 pagesWhat-Is The Novel CoronavirusmichaeelsayedNo ratings yet
- Člankonožaca Acari: KrpeljDocument4 pagesČlankonožaca Acari: KrpeljtmooyoNo ratings yet
- Ticks in Gaots in Chihota AreaDocument5 pagesTicks in Gaots in Chihota AreaChipo NyamindiNo ratings yet
- Tickborne Diseases of The United States: A Reference Manual For Healthcare ProvidersDocument52 pagesTickborne Diseases of The United States: A Reference Manual For Healthcare ProvidersJorge Navarrete LozanoNo ratings yet
- May 5, 2017Document16 pagesMay 5, 2017Anonymous KMKk9Msn5No ratings yet
- The Argasidae, Ixodidae and Nuttalliellidae (Acari: Ixodida) : A World List of Valid Tick NamesDocument28 pagesThe Argasidae, Ixodidae and Nuttalliellidae (Acari: Ixodida) : A World List of Valid Tick NamesGabriela Victoria MartinescuNo ratings yet
- Veterinary Parasitology Arthropod 2 Ticks 2015Document81 pagesVeterinary Parasitology Arthropod 2 Ticks 2015Gheorghita Ileana100% (1)
- Bravecto-Chew-BrochureDocument2 pagesBravecto-Chew-Brochureadinda larasNo ratings yet
- CHEO Algorithm Lyme Disease June2017Document4 pagesCHEO Algorithm Lyme Disease June2017itaa19No ratings yet
- Ontario Lyme Disease Risk Area Map 2021Document6 pagesOntario Lyme Disease Risk Area Map 2021Mario MenezesNo ratings yet
- Tick ID CardDocument2 pagesTick ID CardWGMENo ratings yet
- Tick Species in KentuckyDocument2 pagesTick Species in KentuckyDebbie HarbsmeierNo ratings yet
- Suffolk County Tick and Vector Borne Diseases - Final ReportDocument140 pagesSuffolk County Tick and Vector Borne Diseases - Final ReportKatie BlaslNo ratings yet
- Curs 14 Boala Lyme 2Document63 pagesCurs 14 Boala Lyme 2n1u1s1h1100% (1)
- Lecture 7 BabesiaDocument27 pagesLecture 7 BabesiaEmmanuel Thon Mading100% (1)
- Ticks in MichiganDocument1 pageTicks in MichiganJessica StrachanNo ratings yet
- Lyme Disease BorreliaDocument33 pagesLyme Disease Borreliatummalapalli venkateswara raoNo ratings yet
- Diagnosticul de Laborator Al: BorreliozelorDocument68 pagesDiagnosticul de Laborator Al: BorreliozelorVLDsNo ratings yet
- Tick - WikipediaDocument5 pagesTick - Wikipediar.taha7617No ratings yet
- Tick Paralysis in Dog-Dr - Jibachha SahDocument16 pagesTick Paralysis in Dog-Dr - Jibachha SahJibachha SahNo ratings yet
- Antiparasitic Efficacy of 10% W/V Fipronil Spot-On (Fiproline Spot-On) Against Experimental Tick (Rhipicephalus Sanguineus) Infestations On DogsDocument7 pagesAntiparasitic Efficacy of 10% W/V Fipronil Spot-On (Fiproline Spot-On) Against Experimental Tick (Rhipicephalus Sanguineus) Infestations On DogsDyahNo ratings yet
- TBRF in EuropeDocument5 pagesTBRF in EuropeCatrinel MilitaruNo ratings yet
- CVBD Easy-To-digest No 2 CoinfectionDocument8 pagesCVBD Easy-To-digest No 2 Coinfectionsnooty.eli.gamedogsNo ratings yet
- 230 Hamse Sa'ad MuseDocument30 pages230 Hamse Sa'ad MuseAbdi KhadarNo ratings yet
- Edna Adan University ThesisDocument29 pagesEdna Adan University ThesisAbdi Khadar100% (1)
- Babesia - PPT 2Document13 pagesBabesia - PPT 2jazelNo ratings yet
- Presentation-Lyme Disease - March13Document20 pagesPresentation-Lyme Disease - March13jabirNo ratings yet
- 823-Article Text-3390-2-10-20190624Document12 pages823-Article Text-3390-2-10-20190624umar yusufNo ratings yet
- Finally Complete Thssis Nuuradiin Last DraffDocument25 pagesFinally Complete Thssis Nuuradiin Last DraffAbdi KhadarNo ratings yet