0 ratings0% found this document useful (0 votes)
7 viewsEent Assessment Checklist
Eent Assessment Checklist
Uploaded by
KeoniCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Eent Assessment Checklist
Eent Assessment Checklist
Uploaded by
Keoni0 ratings0% found this document useful (0 votes)
7 views4 pagesOriginal Title
EENT ASSESSMENT CHECKLIST
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
7 views4 pagesEent Assessment Checklist
Eent Assessment Checklist
Uploaded by
KeoniCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 4
CORDILLERA CAREER DEVELOPMENT COLLEGE
Buyagan, Poblacion, La Trinidad, Benguet
College of Health Education
CCDC VISION CCDC MISSION
The center of quality education Deliver quality education and services through holistic,
for culturally diverse and global accessible, and inclusive learning experiences
learners. sustaining culturally sensitive and responsible global
. citizens and leaders.
PERFORMANCE CHECKLIST
EYES, EARS, NOSE AND MOUTH
Examination light or a well-lit room
Snellen chart
Newspaper to read
Otoscope
Ear speculum
Tuning Fork
Nasal speculum
Gloves
Gauze
Cotton balls
Objective: To establish a baseline data of patient’s eyes, ears, nose and mouth and to determine any
deviation from normal physical status for the monitoring of improvement or deterioration in the health
condition of the patient
Special Consideration:
1. Consider age-appropriate communication and procedures
2. Always note for changes in size, color, odor, symmetry, formation of mass, and other deviation from
normal
3. Wear PPe if the patient manifest communicable diseases for your own protection such as mask,
gloves and face shield.
Performance Points 3 2 1
I. Knowledge
1. State the purpose/objective
2. Enumerate special considerations
3. Identify materials/equipment’s needed.
II. Skills
1. Prior to performing the procedure, introduce self and verify the client’s identity.
Explain the procedure to the client and how he/she can participate during the
assessment.
2. Prepare pieces of equipment’s needed for the procedure.
3. Perform hand hygiene and observes other appropriate infection prevention
procedures.
4. Provide client privacy
ASSESSING THE EYES
5. Evaluates distant visual acuity (with Snellen chart)
Visual acuity- degree of detail the eye can discern in an image.
Steps:
Ask the client to stand or sit 6 meters (20 ft) from the Snellen chart
Cover the eye not being tested.
Ask the client to read each line until he cannot decipher the letters of their
direction
6. Evaluates near visual acuity (with handheld vision chart, normal acuity is 14/14 with or
without lenses)
Steps:
Provide adequate lighting.
Ask the client to read from a magazine or newspaper held at a distance of 36 cm
(14 inches)
If the client normally wears corrective lenses, the glasses or lenses should be
worn during the test.
7. Evaluate visual fields for gross peripheral vision through Confrontation test.
Visual fields- the area an individual can see when looking straight ahead
Steps:
Have the client sit directly facing you at a distance of 60 to 90 cm (2-3 feet)
Ask the client to cover the right eye with a card and look directly at your nose.
Cover or close your eye directly opposite the client’s covered eye.
Hold an object in your fingers, extend your arm and move the object into the
visual field from various points in periphery. The object should be at an equal
distance from the client and yourself.
Ask the client to tell you when the moving object is first spotted.
Extraocular muscle function test
8. Checks corneal light reflex (using penlight to observe parallel alignment of light
reflection on cornea)
Steps:
Hold a penlight approximately 12 inches from the client’s face
Shine the light towards the bridge of the nose while the client stares ahead
Note the light that reflected on the corneas.
9. Performs Cover test using opaque card to cover an eye to observe for eye movement.
Steps:
Ask the client to stare straight ahead and focus on distant object
Cover 1 eye with a card
Observe the uncovered eye for movement
Remove card and observe the previously covered eye for movement.
10. Performs Position test ( six cardinal position of Gaze)
Steps:
Stand directly in front of the client and hold the penlight at a comfortable
distance such as 30 cm (1 feet) in front of the client’s eyes.
Ask the client to hold the head in a fixed position facing you and to follow the
movements of the penlight with the yes only.
Move the penlight in a slow, orderly manner through the six cardinal fields of
gaze that is from the center of the eye along the lines of the arrows and back to
the center.
Stop the movement of the penlight of the penlight periodically so that nystagmus
can be detected.
If there is (+) coordination; weakness or paralysis of one or two extra ocular
muscles
The nerve affected will be on the same side as the affected.
Inspect External Eye Structure
The examiner stands directly in front of the client at eye level
11. Inspects eyelids and eyelashes (width and position of palpebral fissures, ability to
close eyelids, direction of eyelids in comparison with eyeballs, color, swelling, lesions or
discharge
Palpebral fissures (longitudinal openings between the eyelids) for width and
symmetry. Palpebral fissures appear equal in size when the eyes are open.
12. Inspect positioning and alignment of eyeball in eye sockets without protruding or
sunken.
13.Inspect bulbar conjunctiva and sclera (clarity, color and texture)
Steps:
Retract the eyelids with your thumb and index finger, exerting pressure over the
upper and lower bony orbits
Have the client keep his or head straight while looking from side to side and then
up toward the ceiling. Observe clarity, color and texture.
14. Inspect the lacrimal apparatus over the lacrimal glands (lateral aspects of upper eyelid
and puncta (medial aspect of lower eyelid)
15. Palpate the lacrimal apparatus, noting drainage from the puncta when palpating the
nasolacrimal duct.
16.Inspects the iris and the pupil for shape and color. Inspect the size of the pupils.
PERRLA-pupils equal, round, reactive to light and accommodation
17. Test Pupillary reaction to light.
In a darkened room, have a client focus on a distant object, shine a line obliquely
into the pupil and observe the pupils’ reaction to light-normally pupils constrict
18. Test accommodation of pupils by shifting gaze from far to near (normally, pupils
constrict)
Hold a pencil or your finger about 12-15 inches from the client. Ask the client to
focus on your finger or pencil and to remain focused on it as you move it closer in
towards the yes.
EAR ASSESSMENT
1. Inspect the auricle, tragus and lobule for size and shape, position, lesions/ discoloration
and discharge .
2. Inspect the auricles for color, symmetry of size and position.
3. Palpates the auricle and mastoid process behind the ear for tenderness.
• Gently pull the auricle upward and backward for adults. (Downward and backward
forchildren.)• Fold the pinna forward (It should recoil.)Such techniques allow the nurse to
check forthe pliability or elasticity of the ear cartilages,texture and elicit tender ear areas
(feeling of pain upon touching) on the patient.• Push on the tragus.• Apply pressure on
the mastoid process
4. Palpate the ears, symmetrical upon inspection, no swelling, thickening lesions or pain
Otoscopic Examination
5. Inspects the external auditory canal with the otoscope for discharge, color and
consistency of cerumen, color and consistency of canal walls and nodules.
6. Inspects the tympanic membrane, using the otoscope for color and shape, consistency
and landmarks
Hearing and Equilibrium Tests
A. WHISPER TEST
7. Performs the whisper test by having the client place a finger on the tragus of one ear or
occlude one of patient’s ear using your finger. Whisper a two-syllable word 1 to 2 feet
behind the client. Repeat on the other ear.
Steps:
Ask the client to close his eyes
Occlude one ear by placing finger on the tragus
The nurse whisper softly toward the unoccluded ear reciting numbers with two
equally accented syllables e.g nine-four
The client is asked to repeat what is heard
WEBER TEST
8. Performs the Weber test by using a tuning fork placed on the center of the head or
forehead and asking whether the client hears the sound better in one ear or the same in
both ears
RHINNES TEST
9. Using a tuning fork and placing the base on the client’s mastoid process. When the
client can no longer hear the sound, note the time, interval and move it in from the
external ear. When the client no longer hears the sound, note the time of the interval
Steps:
Strike the tuning fork and place the stem at the mastoid process
Count the seconds until the patient says he/she can no longer hear the sound
This indicates bone conduction/ BC4.
Immediately place the still vibrating fork to the patient’s auricle near the ear canal
Count the seconds again until the patient says I can no longer hear the sound.
This indicates air conduction or AC
*Compare air and bone conduction
*Air conduction is twice as long as bone conduction
ROMBERG’s TEST
10. Performs the Romberg test to evaluate equilibrium. With feet together and arms at
the side, close eyes for 20 seconds.
11. Observe for swaying (or minimal swaying)
Note: put your arms around the client to prevent him from fall
ASSESSMENT OF THE NOSE, MOUTH AND THROAT
1. Prepare pieces of equipment needed for the procedure.
2. Inspect external nose very briefly to note for symmetry.
3. Lightly palpate the external nose to determine areas of tenderness, masses,
displacement of bone and cartilage.
4. Determine patency of both nasal cavities by occluding one nostril at a time and
asking client to sniff.
5. Inspect nasal cavities using penlight or nasal speculum for the presence of
redness, lesions, swelling and discharges.
6. Palpate frontal and maxillary sinuses for tenderness. Palpate the frontal sinuses
by using the thumbs to press up on the brow on each side of the nose. Palpate
the maxillary sinuses by pressing with thumbs up on the maxillary sinuses.
7. Percuss frontal and maxillary sinuses for tenderness. Lightly tap over the frontal
sinuses and over the maxillary sinuses for tenderness.
Mouth and Oropharynx Assessment
8. Do hand hygiene or change gloves.
9. Prepare the necessary equipment:
Sterile Gloves, Penlight, Sterile Gauze, Tongue Depressor
10. Inspect outer lips for symmetry, contour, color, presence of lesion and texture.
11. Inspect the teeth and gums. Ask the client to open the mouth. Note the number,
color, condition, and alignment of the teeth. Retract the client’s lips and cheeks to
check gums for color and consistency.
12. Inspect the buccal mucosa: use a penlight and tongue depressor to retract the lips
and cheeks to check color and consistency.
13. Inspect and palpate the tongue. Ask the client to stick out the tongue. Inspect for
color, moisture, size, and texture. Observe for fasciculations (fine tremors) and
check for midline protrusion. Palpate any lesions present for
induration(hardness).
14. Assess the ventral surface of the tongue. Ask the client to touch the tongue to the
roof of mouth, and use a penlight to inspect ventral surface of tongue, frenulum
and the area under the tongue. Check also for a short frenulum that limits tongue
motion.
15. Observe the sides of the tongue; use a square gauze pad to hold the clients
tongue to each side. Palpate any lesions, ulcers, or nodules for induration.
16. Check the strength of the tongue. Place your fingers on the external surface of
the client’s cheek. Ask the client to press the tongues tip against the inside of the
cheek to resist pressure from the fingers. Repeat on the opposite cheek.
17. Check the anterior tongue’s ability to taste by placing drops of sugar and salty
water on the tip and sides of tongue with a tongue depressor.
18. Inspect the hard palate ( anterior) and soft( posterior) palates and uvula. Ask the
client to open the mouth wide while you use a penlight to look at the roof.
Observe color and integrity.
19. Note odor. While the mouth is open wide, note any unusual or foul odor.
20. Assess the uvula. Apply a tongue depressor to the tongue ( halfway between the
tip and back of the tongue) and shine a penlight into the clients wide open
mouth. Note the characteristics and positioning of the uvula. Ask the client to say
ah and watch for the uvula and soft palate to move.
21. Inspect the tonsils. Using the tongue depressor to keep the mouth open wide,
inspect the tonsils for color, size, and presence of exudate or lesions.
22. Inspect the posterior pharyngeal wall. Keeping the tongue depressor in place,
shine the penlight on the back of the throat. Observe the color of the throat, and
note any exudate or lesions.
23. Elicit gag reflex.
24. Discard gloves and perform hand hygiene
25. Document all the findings. Report any concerns according to hospital/institution
policy
III. Attitude
1. Demonstrate preparedness, readiness and confidence in the performance of the
procedure
2. Accepts corrections/suggestions and shows willingness to improve performance.
3. Answers questions politely and tactfully
4. Observes proper decorum and behave as a mature student nurse.
TOTAL SCORE: 180 POINTS
Conforme: Evaluated by:
Signature of student: ____________________ Clinical Instructor: __ __________________
You might also like
- Health Assessment ChecklistDocument10 pagesHealth Assessment ChecklistRuby Ann Narvasa100% (1)
- Checklist Assessment of The Eyes and Visual Acuity2021 22Document3 pagesChecklist Assessment of The Eyes and Visual Acuity2021 22Trisha SabaNo ratings yet
- Head To Toe AssessmentDocument18 pagesHead To Toe AssessmentCin Dy100% (2)
- 8 Part Eye Exam RevisedDocument17 pages8 Part Eye Exam Revisedpasambalyrradjohndar100% (1)
- Health Assessment ChecklistDocument14 pagesHealth Assessment ChecklistLindy Jane100% (1)
- Assessing The Skull and Face Eye Structures and Visual Acuity Ears and Hearing Nose and Sinuses Mouth and Oropharynx and Neck Basic ConceptDocument23 pagesAssessing The Skull and Face Eye Structures and Visual Acuity Ears and Hearing Nose and Sinuses Mouth and Oropharynx and Neck Basic ConceptFrancar Jade De VeraNo ratings yet
- Performance Evaluation Checklist Assessment of The Eyes: Tarlac State University College of Science Nursing DepartmentDocument10 pagesPerformance Evaluation Checklist Assessment of The Eyes: Tarlac State University College of Science Nursing DepartmentArt russelNo ratings yet
- Assessing EyesDocument5 pagesAssessing EyesMercy Anne EcatNo ratings yet
- EARSEYESDocument93 pagesEARSEYESZen Gesner Kenneth G. EganaNo ratings yet
- Assessing The Eye Structures and Visual AcuityDocument4 pagesAssessing The Eye Structures and Visual AcuityJo Hn VengzNo ratings yet
- HA Neuro Final 1Document10 pagesHA Neuro Final 1korean barbequeNo ratings yet
- Assessing Ears and Hearing Nose and Sinuses Mouth and OropharynxDocument8 pagesAssessing Ears and Hearing Nose and Sinuses Mouth and OropharynxMercy Anne EcatNo ratings yet
- Vision Procedure With EquipmentDocument5 pagesVision Procedure With EquipmentfileacademicsNo ratings yet
- Module 2 Physical AssessmentDocument8 pagesModule 2 Physical AssessmentMaria EsNo ratings yet
- EyesDocument5 pagesEyesSiege DiamondsNo ratings yet
- Cranial Nerve Testing Student Guide and RubricDocument8 pagesCranial Nerve Testing Student Guide and Rubricbw653865No ratings yet
- Physical Assessment Part 1 Action & Rationale Normal Findings Abnormal FindingsDocument7 pagesPhysical Assessment Part 1 Action & Rationale Normal Findings Abnormal FindingsTrisha MarieNo ratings yet
- Skull, Scalp & Hair: Physical Assessment Is AnDocument10 pagesSkull, Scalp & Hair: Physical Assessment Is AnTrixie Al MarieNo ratings yet
- Skill: Assessing The Eye Structures and Visual Acuity: AssessmentDocument5 pagesSkill: Assessing The Eye Structures and Visual Acuity: AssessmentDr. Abiola KomolafeNo ratings yet
- Neurologic System Physical Assessment GuideDocument4 pagesNeurologic System Physical Assessment GuideJeff Shaun Claude PalaparNo ratings yet
- Head and Neck Assessment: ChecklistDocument2 pagesHead and Neck Assessment: ChecklistLucky Dela cruz100% (1)
- Eye AssessmentDocument4 pagesEye AssessmentAngeline VegaNo ratings yet
- Cranial Nerve ExamDocument20 pagesCranial Nerve ExamSIR ONENo ratings yet
- Nursing Care Management 101 Health Assessment: Procedural Checklist inDocument5 pagesNursing Care Management 101 Health Assessment: Procedural Checklist inKyle Randolf CuevasNo ratings yet
- Assessing Eye Structure and Visual AcuityDocument4 pagesAssessing Eye Structure and Visual AcuityRoldan BalangyaoNo ratings yet
- Assessing The Ears and HearingDocument2 pagesAssessing The Ears and HearingAL HAROUN ARAMAINNo ratings yet
- Performance Evaluation Checklist Neurological Assessment: 1. Beginning ExaminationDocument5 pagesPerformance Evaluation Checklist Neurological Assessment: 1. Beginning ExaminationDominicManlutacNo ratings yet
- Performance Evaluation Checklist Neurological Assessment: 1. Beginning ExaminationDocument5 pagesPerformance Evaluation Checklist Neurological Assessment: 1. Beginning ExaminationDominicManlutacNo ratings yet
- Assessment of The EyesDocument32 pagesAssessment of The EyesArlyn Mendenilla100% (1)
- Ultimate Guide To HeadDocument29 pagesUltimate Guide To HeadCjoy Alonday100% (1)
- Yuan Physical-Assessment-Checklist-RATIONALEDocument13 pagesYuan Physical-Assessment-Checklist-RATIONALEtmmrsptlnNo ratings yet
- Millimeter Ruler Penlight Eye Chart Opaque CardDocument13 pagesMillimeter Ruler Penlight Eye Chart Opaque CardemraduraiyenNo ratings yet
- Heent LabDocument11 pagesHeent Labapi-743783774No ratings yet
- Checklist For Physical AssessmentDocument13 pagesChecklist For Physical AssessmentSharene Kate EribalNo ratings yet
- 06 EENT AssessmentDocument36 pages06 EENT AssessmentHerlinaNababanNo ratings yet
- Assessment of The Eyes and The EarsDocument4 pagesAssessment of The Eyes and The EarsAllyssa Mae NacionNo ratings yet
- Eye Assessment and Visual AcuityDocument4 pagesEye Assessment and Visual AcuityKen KanekiNo ratings yet
- HEENT Exam Teaching DocketDocument10 pagesHEENT Exam Teaching DocketJonah R. MeranoNo ratings yet
- 8 Part Eye Exam REVISED PDFDocument16 pages8 Part Eye Exam REVISED PDFJerwin EstacioNo ratings yet
- Performing Physical Assessment of The EyeDocument14 pagesPerforming Physical Assessment of The Eyezyrine jhen100% (1)
- Eyes - Ears - Mouth - Nose (Lecture 5)Document50 pagesEyes - Ears - Mouth - Nose (Lecture 5)اسامة محمد السيد رمضانNo ratings yet
- Head To Toe AssessmentDocument21 pagesHead To Toe AssessmentZahra jane A.100% (1)
- BSN220 CHA Lab Neurological Assessment Checklist StudentDocument10 pagesBSN220 CHA Lab Neurological Assessment Checklist Studentamani.nasserhNo ratings yet
- Neurological AssessmentDocument7 pagesNeurological AssessmentSharon LawrenceNo ratings yet
- PERFORMANCE-EVALUATION-CHECKLIST-HEADDocument4 pagesPERFORMANCE-EVALUATION-CHECKLIST-HEADHaydi Pineda Medina100% (1)
- 4. Eye Assessment Theory._5cd360ef964d58509d0422fcc29cdf1cDocument36 pages4. Eye Assessment Theory._5cd360ef964d58509d0422fcc29cdf1cagaloudhNo ratings yet
- Eye MethodsDocument28 pagesEye MethodsWaqar Ul HaqNo ratings yet
- Session 4 Skills.......Document18 pagesSession 4 Skills.......Harry ChauhanNo ratings yet
- PRS EyesDocument4 pagesPRS EyesJica GulaNo ratings yet
- Assessing The Ears and HearingDocument2 pagesAssessing The Ears and HearingJo Hn VengzNo ratings yet
- Eye AssessmentDocument90 pagesEye AssessmentjkalimesNo ratings yet
- Eye Assessment: Physical Assessment Course/ TheoryDocument31 pagesEye Assessment: Physical Assessment Course/ Theoryroama3359No ratings yet
- Eyes (Doc Maala)Document53 pagesEyes (Doc Maala)jkalimesNo ratings yet
- Cranial Nerve AssessmentDocument8 pagesCranial Nerve AssessmentAllean Sarmiento Apolinario100% (1)
- EarsDocument3 pagesEarsUriel NateNo ratings yet
- Physical AssessmentDocument5 pagesPhysical AssessmentIsabel DizonNo ratings yet
- NeurologicalDocument11 pagesNeurologicalHiba V.ANo ratings yet
- Pemeriksaan Mata, Telinga, Hidung Dan Tenggorokan: Oleh: Ns. Gst. Kade Adi Widyas Pranata, S.Kep., M.SDocument72 pagesPemeriksaan Mata, Telinga, Hidung Dan Tenggorokan: Oleh: Ns. Gst. Kade Adi Widyas Pranata, S.Kep., M.SAyu Diah Sri Krisnayanti PutuNo ratings yet
- OHNS--Otolaryngology; Head and Neck surgery: pocket field guideFrom EverandOHNS--Otolaryngology; Head and Neck surgery: pocket field guideNo ratings yet
- FMT 0013matDocument5 pagesFMT 0013matdiraazlanNo ratings yet
- Facilities Director in Philadelphia PA Resume Patricia DonovanDocument2 pagesFacilities Director in Philadelphia PA Resume Patricia DonovanPatriciaDonovanNo ratings yet
- Panelinstrument Catalogu0Document36 pagesPanelinstrument Catalogu0Jatupol PongsirisartNo ratings yet
- Counter Rust 7010 TDSDocument2 pagesCounter Rust 7010 TDSFadhli KusumaNo ratings yet
- Guidelines - In-Hospital ResuscitationDocument18 pagesGuidelines - In-Hospital ResuscitationparuNo ratings yet
- Reflection Title: Addition: Name: Jawaher Ahmed Alkaabi Course: EPC 3903 - Practicum 3b Instructor: Robin OgdolDocument3 pagesReflection Title: Addition: Name: Jawaher Ahmed Alkaabi Course: EPC 3903 - Practicum 3b Instructor: Robin Ogdolapi-296835930No ratings yet
- OECD Budgeting in Chinese TaipeiDocument31 pagesOECD Budgeting in Chinese TaipeiCristian Pablo Yáñez NavarroNo ratings yet
- Gödels First Incompleteness Theorem in Simple Symbols and Simple TermsDocument5 pagesGödels First Incompleteness Theorem in Simple Symbols and Simple TermsbambambholeNo ratings yet
- 08 - A NOBRE What Remains On The Beach After Tourists Leave - The Case of Abaís Beach (Sergipe, Brazil)Document7 pages08 - A NOBRE What Remains On The Beach After Tourists Leave - The Case of Abaís Beach (Sergipe, Brazil)Anonymous HijNGQtNNo ratings yet
- Optical LAN Operations Provisioning & MaintenanceDocument2 pagesOptical LAN Operations Provisioning & MaintenanceFilipi TariganNo ratings yet
- Qap Hot Induction BendsDocument6 pagesQap Hot Induction BendsVidyut UjalaNo ratings yet
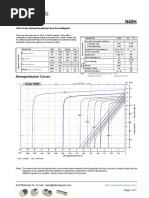
- N40H Grade Neodymium Magnets DataDocument1 pageN40H Grade Neodymium Magnets DataSteve HsuNo ratings yet
- Standard Penetration TestDocument59 pagesStandard Penetration TestcuervohijoguachoNo ratings yet
- Count in 2s and Fill in The Missing NumbersDocument3 pagesCount in 2s and Fill in The Missing Numbersjuniorcurry124No ratings yet
- First Party Short StoryDocument9 pagesFirst Party Short StoryHein Htet AungNo ratings yet
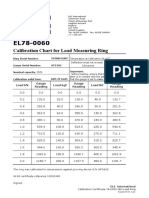
- 78-0060 - Direct Shear Load Ring Calibration CertificateDocument2 pages78-0060 - Direct Shear Load Ring Calibration CertificateBalen100% (1)
- 2Document49 pages2ZafirahAhmadFauziNo ratings yet
- User Manual EC5000 enDocument64 pagesUser Manual EC5000 enSawan Patil100% (1)
- IGNOU FST-01 Solved AssignmentsDocument11 pagesIGNOU FST-01 Solved AssignmentsSUSMITA MONDALNo ratings yet
- Eldoria The CageDocument3 pagesEldoria The CageNIA KANJIKODENo ratings yet
- Eao MCDocument100 pagesEao MCdinesh005No ratings yet
- Globalization PowerpointDocument41 pagesGlobalization PowerpointArjay Jimenez0% (1)
- Cape Unit 1 Term 2 20202021 Biology Scheme of WorkDocument4 pagesCape Unit 1 Term 2 20202021 Biology Scheme of Workalanamaharaj20No ratings yet
- EE555 Exam Jan2008 SolutionsDocument11 pagesEE555 Exam Jan2008 SolutionsYuvarajaNo ratings yet
- Criminal Complaint Against Neysa Fligor and MaryAnn Barry For PerjuryDocument33 pagesCriminal Complaint Against Neysa Fligor and MaryAnn Barry For PerjuryJames Alan BushNo ratings yet
- Medical Guide For SeafarersDocument1 pageMedical Guide For SeafarersKEITH DESOUZANo ratings yet
- Hilti. Outperform. Outlast: If You Are An Existing User - Submit Activation KeyDocument1 pageHilti. Outperform. Outlast: If You Are An Existing User - Submit Activation KeySAN HTET AUNGNo ratings yet
- Clinical Exemplar Deborah Ogunrinde University of South FloridaDocument4 pagesClinical Exemplar Deborah Ogunrinde University of South Floridaapi-402469727No ratings yet
- Module 1 Final QuizDocument5 pagesModule 1 Final QuizRota Ray100% (1)
- Clinical Teams Mental Health ManualDocument18 pagesClinical Teams Mental Health Manualapi-609422028No ratings yet