3. Psychiatry_Child_Behavioral_Disorder
3. Psychiatry_Child_Behavioral_Disorder
Uploaded by
Tanvir DhimanCopyright:
Available Formats
3. Psychiatry_Child_Behavioral_Disorder
3. Psychiatry_Child_Behavioral_Disorder
Uploaded by
Tanvir DhimanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
3. Psychiatry_Child_Behavioral_Disorder
3. Psychiatry_Child_Behavioral_Disorder
Uploaded by
Tanvir DhimanCopyright:
Available Formats
October/ 2019
Department of Health Research
Ministry of Health and Family Welfare, Government of India
Standard Treatment Workflow (STW) for the Management of
CHILDHOOD BEHAVIORAL DISORDERS
ICD10- F90-98
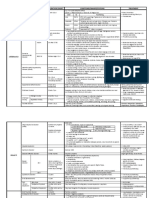
OPPOSITIONAL DEFIANT DISORDER (ODD) DIAGNOSIS
• Doesn’t obey or listen, back-answers, rude behaviors
• Demanding, stubborn, throws tantrums when
demands are not met • Symptoms are present
CONDUCT DISORDER and persistent over
• Aggressive – angry, abusive, fights, hits or hurts several months
people, bullies other children, damages articles • Attempt further
• Stealing, lying, threatening or misbehaving classification into ADHD,
with people, truant (keeps away from school ODD and CD (ADHD
without parents’ knowledge), runs away from may be present with or
home, bad company, cruelty to animals without ODD and CD
CLINICAL
ATTENTION DEFICIT HYPERACTIVITY DISORDER (ADHD)
PRESENTATION • Restless, always on the move / running, can’t sit in
CAUTION
a place,talkative
• Abrupt onset
• Can’t focus attention on a task, poor concentration,
gets easily distracted, disorganized, does not • Recent onset (few weeks
complete school work to few months)
• Too mischievous, can’t be left alone, troubles • Sudden increase in
people or damages things, or gets injured severity (consider another
• Impatient, always in a hurry, can’t wait for his turn, psychiatric disorder such
does not care for danger, acts without thinking as bipolar affective
disorder, hypomanic or
ALL 3 DISORDERS
Poor or erratic school performance and / or manic episode -> follow
complaints about behaviour from school the relevant STW)
.in
ASSESSMENT (History From Multiple Sources)
PARENT INTERVIEW FAMILY SITUATION SCHOOLING CHILD INTERVIEW
• Symptoms- onset, duration, • Health (including mental health) and • Attendance • Develop rapport( discuss neutral topics; avoid direct
type(ODD, Conduct, ADHD-as wellbeing of family members • Performance tackling of misbehaviors)
above) and severity • Cohesion, mutual understanding and • Learning • Observe:
• Developmental problems, harmony in the family
rg
problems, - Features of ADHD (restless, fidgety, easily distracted,
emotional disturbances and • Parenting and childrearing practices: • Classroom attention keeps shifting)
stress caring and disciplining, criticism, unfair behaviors - Speech and language ability, intelligence, academic
• Alcohol and substance use comparison and physical punishments, • Recent changes skills and mood
/misuse mutual blaming of parents for child’s in syllabus and/or • Enquire about any stress or difficulties child is facing at
• Impact on child and family problem school home, school, and with peers and anger control
r.o
MANAGEMENT
WORK WITH FAMILY WORK WITH THE CHILD WORK WITH THE
• PSYCHOEDUCATION
SCHOOL
- Explain the child’s behaviours are not intentional • Avoid advice
- Not child’s fault, do not blame the child • Feedback to school
• Anger management ( count
- Multifactorial causes-lack of self-regulation, and adverse environment regarding child’s
from 10 -1 backwards, move
- Can be improved with proper management condition
away from situation, deep
m
- Parents can directly contribute to the child’s improvement • Teachers to give extra
breaths, relax, self-talk to
• Help parents deal with their own worries and stress (listening, giving space to attention, help and
ventilate, validate and empathize their difficulties, reassure) cool down)
support for the child
• Recognize and manage mental health problems such as depression and alcohol • Children with ADHD:
• Extra coaching, if
problem in parents “stop-think-act” or “halt and
needed in case of
• Parent management training* proceed” technique
learning problems
.ic
*PARENT MANAGEMENT TRAINING MEDICATION (AVOID BEFORE 5 YEARS)
• Analyse the problem behaviors and understand patterns : time of occurance, triggers, • Severe and persistant aggression:
duration and consequencies - T. Risperidone under close supervision (starting
• Engage with child in mutually enjoyable, pleasurable activities (playing games, dose-0.25 mg, single daily morning dose after
discussing interesting things or doing activities together) breakfast. Based on response, increase by 0.25 mg
w
• Set clear do’s and don’ts and explain to child in clear, simple, short instructions the weekly up to 1 mg single daily dose).
consequencies (like withholding privileges following misbehavior; use star-charting Not to exceed 1 mg/day
(contingency management) and rewards based on number of stars earned - Response + : continue 3 months f/b slow taper
• In children with ADHD, develop clear daily routines, supervise activities and appreciate - Response - : 4 weeks trial, then refer
on completion of taks - Monitor adverse effects: weight gain,
st
• Limit screen time/ monitor use of electronic devices extra-pyramidal symptoms (EPS)
[if EPS : add I mg Trihexyphenidyl OD morning]
• Dos • Don’ts • Severe hyperactivity and impulsivety:
– Consistency in enforcing rules – Bribe - T. Clonidine (starting dose-25 μg single daily
– Catch the child being good and praise – False promises and threats
dose before sleep, increase by 25 μg weekly up
– Ignore negative behaviours – Harsh punishments
to100 μg per day in 2-3 divided doses
– Child can be put in a boring place till he/ – Excessive criticism and blaming
she becomes quiet for a few minutes especially in front of others - Monitor BP and drowsiness
(time-out) – Unfair comparison - Advise against sudden discontinuation
– Encourage age appropriate responsibilities – Yielding to unreasonable demands
REASONS FOR REFERRAL
Severe, complicated presentation Lack of response to treatment Severe aggression Highly dysfunctional family Alcohol and substance abuse
SECONDARY CARE (DISTRICT HOSPITAL) TERTIARY CARE (MEDICAL COLLEGE / REGIONAL REFERRAL CENTRE)
• Review and reassess diagnosis (clinical evaluation • Evaluate and manage severe behavior disorders – severe ADHD, ODD, and CD, if necessary on
using Rutter’s multi-axial system) and all the short-term inpatient basis
pointers given above • Multi-modal management with clear individualized plan
• If failed trial of Clonidine/ Moderate ADHD: • Trial of Methylphenidate in moderate / severe ADHD under expert supervision
T. Atomoxetine (starting dose-10 mg single daily • Recognize and treat comorbid disorders such as bipolar disorder, substance use disorder, and
morning dose after breakfast. Increase up to internalizing disorders and manage
1mg/ kg/day under close supervision). • Pharmacological management of older children / adolescents with severe aggression /
Monitor adverse effects and response impulsivity with Risperidone and/or Lithium
• Systematic parent management training / • Family therapy for dysfunctional / discordant families, contributing to child’s condition
behavioral management and individual therapy • Management of children in difficult circumstances with mental health issues (children in need
(as given above) of care and protection; children in conflict with law)
REFERENCES
• World Health Organization. mhGAP intervention Guide–Version 2.0 for mental, neurological and substance user disorders in non-specialized health settings. Geneva: WHO. 2016.
• Pliszka S, AACAP Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. Journal of the American
Academy of Child & Adolescent Psychiatry. 2007 Jul 1;46(7):894-921.
• Steiner H, Remsing L. Practice parameter for the assessment and treatment of children and adolescents with oppositional defiant disorder. Journal of the American Academy of Child & Adolescent
Psychiatry. 2007 Jan 1;46(1):126-41.
KEEP A HIGH THRESHOLD FOR INVASIVE PROCEDURES
This STW has been prepared by national experts of India with feasibility considerations for various levels of healthcare system in the country. These broad guidelines are advisory, and
are based on expert opinions and available scientific evidence. There may be variations in the management of an individual patient based on his/her specific condition, as decided by
the treating physician. There will be no indemnity for direct or indirect consequences. Kindly visit our web portal (stw.icmr.org.in) for more information.
© Indian Council of Medical Research and Department of Health Research, Ministry of Health & Family Welfare, Government of India.
You might also like
- Clinical Dementia Rating: ScoringDocument1 pageClinical Dementia Rating: ScoringCristi0% (1)
- Semi Structured Interview Questions For A Parent Handout For Psych Training 2-5-14Document6 pagesSemi Structured Interview Questions For A Parent Handout For Psych Training 2-5-14joan arreola100% (3)
- Breaking Free A Recovery Workbook For Facing Codependence ExportDocument6 pagesBreaking Free A Recovery Workbook For Facing Codependence ExportWayne BruceeNo ratings yet
- CDS Clinical Dementia Rating - Summary and QXQDocument5 pagesCDS Clinical Dementia Rating - Summary and QXQvickyvarelas100% (1)
- Ophthalmic LensesDocument224 pagesOphthalmic LensesPaul Rivera100% (2)
- Tricky Kids 1Document13 pagesTricky Kids 1api-355090152No ratings yet
- FINAL FlipbookDocument14 pagesFINAL FlipbookTrinity PikeNo ratings yet
- Disorders Duration/Onset Symptoms/Manifestations Treatment: Childhood DDocument7 pagesDisorders Duration/Onset Symptoms/Manifestations Treatment: Childhood DActeen Myoseen100% (2)
- Add and Adhd ResearchDocument25 pagesAdd and Adhd Researchapi-520142437100% (1)
- M A DDocument19 pagesM A DjoycesiosonNo ratings yet
- 0402 Article2Document10 pages0402 Article2Tortura ChinaNo ratings yet
- Early Indicators of Developmental Delays-2Document31 pagesEarly Indicators of Developmental Delays-2shai gestNo ratings yet
- SNED3 EBDsDocument4 pagesSNED3 EBDsejoycabaneroNo ratings yet
- Disorders Duration/On SET Symptoms/Manifestations Treatment: Level IQ FunctioningDocument1 pageDisorders Duration/On SET Symptoms/Manifestations Treatment: Level IQ Functioningoussama dieselNo ratings yet
- Behavioral and Emotional Disorders in Children and Their Anesthetic ImplicationsDocument15 pagesBehavioral and Emotional Disorders in Children and Their Anesthetic Implicationsdra.bravodanielaNo ratings yet
- Tss Infographic 7 2015Document1 pageTss Infographic 7 2015api-356243627No ratings yet
- Cy BocsDocument2 pagesCy BocsMuh Afdhol100% (1)
- SPN BrochureDocument2 pagesSPN BrochureIzzHyukNo ratings yet
- Disorders in Childhood and AdolescenceDocument6 pagesDisorders in Childhood and AdolescenceCamille Joy BaliliNo ratings yet
- What Is ADHD? Secondary CharacteristicsDocument2 pagesWhat Is ADHD? Secondary CharacteristicszzzzzzNo ratings yet
- Oppositional Defiant DisorderDocument6 pagesOppositional Defiant DisorderAsqa KhanNo ratings yet
- CARE Module 7 - Mental Health and Psychosocial Support (MHPSS)Document53 pagesCARE Module 7 - Mental Health and Psychosocial Support (MHPSS)kaseera musaNo ratings yet
- DSM-cheat SheetDocument4 pagesDSM-cheat SheetayeshafatemafahimNo ratings yet
- Parenting A Child Who Has Experienced Trauma: Factsheet For FamiliesDocument8 pagesParenting A Child Who Has Experienced Trauma: Factsheet For Familiescarla osbourneNo ratings yet
- ADHD Venn Diagrams (A4)Document12 pagesADHD Venn Diagrams (A4)flukwernsNo ratings yet
- Autism Spectrum DisorderDocument5 pagesAutism Spectrum DisorderJuliene Mari QuianNo ratings yet
- ADHDDocument7 pagesADHDEeswari Chandra SegarNo ratings yet
- Delusional Disorder 1. Definition 2. Types 3. TreatmentDocument68 pagesDelusional Disorder 1. Definition 2. Types 3. TreatmentLana LocoNo ratings yet
- Social Issues: CHILD ABUSE: Types (Define) AbusersDocument2 pagesSocial Issues: CHILD ABUSE: Types (Define) AbusersHajar KhalidNo ratings yet
- DBDs Resource...Document7 pagesDBDs Resource...Nadeem IqbalNo ratings yet
- Disorders in Childhood and AdolescenceDocument7 pagesDisorders in Childhood and AdolescenceCamille Joy BaliliNo ratings yet
- Case StudyDocument4 pagesCase StudyYdynn Parejas GavinaNo ratings yet
- Developmental DisordersDocument4 pagesDevelopmental DisordersMary Belle OrtegaNo ratings yet
- mhGAP Anne and Sass 1Document61 pagesmhGAP Anne and Sass 1erineunicerosaryNo ratings yet
- What Is ADHD?Document13 pagesWhat Is ADHD?Charmaine PenadosNo ratings yet
- DDX Behavior ProblemsDocument1 pageDDX Behavior ProblemsDivine MenchuNo ratings yet
- Child and Adolescent Disorders PDFDocument43 pagesChild and Adolescent Disorders PDFPreslee DulnuanNo ratings yet
- ADHD PamphletDocument2 pagesADHD PamphletdahocctherapyNo ratings yet
- Intoxication Assessment Tool S C A B: Sober Influenced IntoxicatedDocument1 pageIntoxication Assessment Tool S C A B: Sober Influenced IntoxicatedFawxse YTNo ratings yet
- Purboyo Solek-Autism and Attention Deficit Hyperactivity Disorder (ADHD) FiDocument38 pagesPurboyo Solek-Autism and Attention Deficit Hyperactivity Disorder (ADHD) FiSupri Adi100% (2)
- TALK On BULLYING - REVISED - FINALDocument85 pagesTALK On BULLYING - REVISED - FINALLilet PaloNo ratings yet
- SSWD AutismDocument22 pagesSSWD Autismapi-663471551No ratings yet
- Personality Disorders ChartDocument11 pagesPersonality Disorders ChartSolomon Seth Sallfors100% (1)
- Childhood Disorder-1Document32 pagesChildhood Disorder-1Hira KhanNo ratings yet
- Personality DisordersDocument4 pagesPersonality DisordersZam Pamate100% (1)
- Disinhibition BehaviorDocument3 pagesDisinhibition BehavioragingamerNo ratings yet
- CEP BPSD Discussion Guide ENG RFCG Updated2019 PDFDocument8 pagesCEP BPSD Discussion Guide ENG RFCG Updated2019 PDFM.DalaniNo ratings yet
- Emotional Distubance Fact SheetDocument2 pagesEmotional Distubance Fact Sheetapi-335203912No ratings yet
- Types of Developmental DisordersDocument60 pagesTypes of Developmental DisordersAnshika ChaudhryNo ratings yet
- Background and Treatment: Neuropsychological DeficitsDocument1 pageBackground and Treatment: Neuropsychological DeficitsStens100% (1)
- Quiz Answer Topic Table of Specifications: Item NumberDocument2 pagesQuiz Answer Topic Table of Specifications: Item NumberLmNo ratings yet
- Youth Depression: Lorna Martin Lormartin@gov - Mb.caDocument25 pagesYouth Depression: Lorna Martin Lormartin@gov - Mb.caBanasthali StudentNo ratings yet
- Childrens ADHD EBPsDocument2 pagesChildrens ADHD EBPsSherly WardoyoNo ratings yet
- Odd HandoutDocument2 pagesOdd Handoutapi-753995548No ratings yet
- Behavioral Assessment PediatricsDocument4 pagesBehavioral Assessment PediatricsByron Macalintal100% (1)
- Body Dysmorphic Disorder Body Dysmorphic Disorder: DR Shazeena QaiserDocument30 pagesBody Dysmorphic Disorder Body Dysmorphic Disorder: DR Shazeena QaiserShazeena OfficialNo ratings yet
- Behavior Management PresentationDocument72 pagesBehavior Management PresentationDasta E Lajpal E Ali DanyoreNo ratings yet
- MHN 18Document22 pagesMHN 18Vaishali SinghNo ratings yet
- Case of Leticia and Case of B (Case Study Activity)Document5 pagesCase of Leticia and Case of B (Case Study Activity)Dainah ArticuloNo ratings yet
- A4 ADHDicebergDocument6 pagesA4 ADHDicebergflukwernsNo ratings yet
- Chaos To Calm: Surviving And Thriving With An Oppositional ADHD KidFrom EverandChaos To Calm: Surviving And Thriving With An Oppositional ADHD KidNo ratings yet
- The Ultimate ADHD Diet Cookbook; A Comprehensive Guide With Easy, Delectable And Nutritious ADHD Recipes To Help Your Kids Perform Well At School, Focus, And Overcome ADHD ForeverFrom EverandThe Ultimate ADHD Diet Cookbook; A Comprehensive Guide With Easy, Delectable And Nutritious ADHD Recipes To Help Your Kids Perform Well At School, Focus, And Overcome ADHD ForeverNo ratings yet
- Dijagnostika RamenaDocument182 pagesDijagnostika Ramenamedeni22No ratings yet
- Ho Guide Peds PDFDocument44 pagesHo Guide Peds PDFCahaya Al-HazeenillahNo ratings yet
- Modul Rinologi - 7. Kelainan SeptumDocument33 pagesModul Rinologi - 7. Kelainan SeptumPutri DamayantiNo ratings yet
- Ranjeet ShahiDocument0 pagesRanjeet Shahisabhari_ram100% (1)
- Debt Securities ReviewerDocument30 pagesDebt Securities Reviewerjhie boterNo ratings yet
- An1 Active PFCDocument2 pagesAn1 Active PFCPaul PamfileNo ratings yet
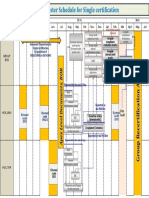
- Single Certification 29.11.2017Document1 pageSingle Certification 29.11.2017Amrendra Singh DagarNo ratings yet
- Bliss Yoga Studio Final ReportDocument36 pagesBliss Yoga Studio Final ReportlikwidsixNo ratings yet
- Alarm Security: Products and Solutions 2018 Ver. 1Document16 pagesAlarm Security: Products and Solutions 2018 Ver. 1Claudio DiazNo ratings yet
- Proper Selection of SeedsDocument1 pageProper Selection of Seedsalmors100% (1)
- Introduction To Environmental PollutionDocument12 pagesIntroduction To Environmental Pollutionsubham rajak100% (1)
- Mira Et al-2009-FEMS Yeast ResearchDocument15 pagesMira Et al-2009-FEMS Yeast ResearchRita JanelaNo ratings yet
- Research Paper in Psychology: Student: Musa, Marissa F. Bseden I-1 Professor: Mrs. Angeline PabilonaDocument16 pagesResearch Paper in Psychology: Student: Musa, Marissa F. Bseden I-1 Professor: Mrs. Angeline PabilonaGa MusaNo ratings yet
- Wide-Lite Lighting Catalog 1976Document106 pagesWide-Lite Lighting Catalog 1976Alan Masters100% (1)
- Environmental and Economic Life Cycle Assessment of PE 2016 Journal of CleanDocument9 pagesEnvironmental and Economic Life Cycle Assessment of PE 2016 Journal of CleanChris BryanNo ratings yet
- CNX PHL Anti-Corruption PolicyDocument1 pageCNX PHL Anti-Corruption PolicyMikee TanNo ratings yet
- Civil Green ConcreteDocument18 pagesCivil Green Concretesharukh88% (8)
- Best Books On PrayerDocument4 pagesBest Books On Prayerscartoneros_1No ratings yet
- The "Meselson-Stahl Experiment"Document5 pagesThe "Meselson-Stahl Experiment"Atika AnggrainiNo ratings yet
- Appendix 2. Default Occupancy CountsDocument1 pageAppendix 2. Default Occupancy CountsCarlos E MANo ratings yet
- Wheel Balancer User Manual: Pls Read This Manual Before OperationDocument27 pagesWheel Balancer User Manual: Pls Read This Manual Before OperationbabitzinNo ratings yet
- Assignment On CLMDocument5 pagesAssignment On CLMBairavarasu BhanuNo ratings yet
- MARPOL Annex 3 & 4Document7 pagesMARPOL Annex 3 & 4Gurkanwar SinghNo ratings yet
- Asme Ix QW MTDocument57 pagesAsme Ix QW MTharabiNo ratings yet
- l4 Cell Injury, Cell Death & AdaptationsDocument22 pagesl4 Cell Injury, Cell Death & AdaptationsGeethanjali SivakumarNo ratings yet
- Kits de MaintenanceDocument54 pagesKits de MaintenanceRicardo Villagomez Tamez100% (1)
- Unit 304 Prepare and Maintain Environment, Instruments and Equipment For Clinical Dental ProceduresDocument5 pagesUnit 304 Prepare and Maintain Environment, Instruments and Equipment For Clinical Dental Proceduresjolene johnstonNo ratings yet
- DuctSox DesignManualDocument20 pagesDuctSox DesignManualPanduNo ratings yet