Flaccid Paraplgia
Flaccid Paraplgia
Uploaded by
Kavita SharmaCopyright:
Available Formats
Flaccid Paraplgia
Flaccid Paraplgia
Uploaded by
Kavita SharmaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Flaccid Paraplgia
Flaccid Paraplgia
Uploaded by
Kavita SharmaCopyright:
Available Formats
Epidemiology and clinical management of Conus-Cauda Syndrome and flaccid paraplegia in Friuli Venezia Giulia: Data of the Spinal
Unit of Udine
Emiliana Bizzarini (1), Agostino Zampa (1), Cristina Malisan (1), Chiara Pinzini (1), Paolo Di Benedetto (1), Helmut Kern (2), Nicoletta Adami (3), Ugo Carraro (3) (1) Spinal Unit, Department of Rehabilitation Medicine, ASS N 4 Medio Friuli, Udine, Italy; (2) Laboratory of Translational Myology of the University of Padova Interdepartmental Research Center of Myology & Interuniversitary Institute of Myology & Italian C.N.R. Institute of Neuroscience, c/o Department of Biomedical Sciences, University of Padova, Italy; (3) Ludwig Boltzmann Institute of Electrostimulation and Physical Rehabilitation, Department of Physical Medicine, Wilhelminenspital. Vienna, Austria.
Abstract The Spinal Unit of the Department of Rehabilitation Medicine of Udine admits patients with Spinal Cord Injury (SCI) after discharge from Neurosurgery or Reanimation Divisions. Demographic data, etiology, duration of hospitalization, bladder managements, and mobility at admission and discharge were revisited from January 2000 to March 2008. We treated 49 complete Spinal Cord Injury patients (ASIA Impairment Scale A). The patients have an average age of 38.63 years (range 16 - 67 years). The ratio between Male and Female was 4 : 1, 40 men e 9 women. All the patients were classified complete respectively to the ASIA Impairment Scale, when no motor or sensory function was preserved in the sacral segment S4-S5. All patients were classified with the Ashworth scale from score 0 to 4. All SCI patients have been treated with conventional rehabilitation strategies for enhancing lower limbs function. At the same time these patients had active exercise for upper limbs and training for daily mobility tasks (transferring, bed mobility and sitting) and functional electrical stimulation. Really we found some difficulties to electrically stimulate denervated muscles, but we believe this approach could give more chances to patients in their recovery. The hope is to realize walking assisted by FES or a combination of this with treadmill and biofeedback training in flaccid paraplegia even in a clinical ambit. This is a good opportunity to engage a long and wide road that leaded us to be partners in the Rise2-Italy Project. A result of this collaboration is the Case Report here presented of the first enrolled person. . Key Words: SCI, Conus-Cauda Equina, Functional Electrical Stimulation. Basic Applied Myology 19 (4): 163-167, 2009
The spinal cord tapers and ends at the level between
the first and second lumbar vertebrae in an average adult. The most distal part of the spinal cord is called the conus medullaris, its tapering end continues as the filum terminale. The upper border of the conus medullaris is often not well defined. Distal to this end of the spinal cord is a collection of nerve roots, which are horsetail-like in appearance and hence called the cauda equina (Latin for horse's tail). These nerve roots constitute the anatomic connection between the central nervous system (CNS) and the peripheral nervous system (PNS). They are arranged anatomically according to the spinal segments from which they originated and are within the cerebrospinal fluid (CSF) in the subarachnoid space with the dural sac ending at the level of second sacral vertebra. The conus - 163 -
medullaris constitutes part of the spinal cord (the distal part of the cord) and is in proximity to the nerve roots. Thus, injuries to this area often yield a combination of upper motor neuron (UMN) and lower motor neuron (LMN) symptoms and signs in the dermatomes and myotomes of the affected segments. The Conus-Cauda Equina Syndrome is characterized by flaccid paraplegia, sensory impairment, pain, as well as bladder and bowel areflexia, sexual dysfunctions. It is a rare disease, which generally affects adults. We revisited 490 stories of SCI patients at their first admission to the Spinal Unit of Udine from January 2000 to May 2008. We selected the patients with spinal cord injury below D1, with a complete lesion or with a motor deficit at the lower limbs which required an intensive rehabilitation program. We selected 49
Cauda Equina Syndrome in Friuli-Venezia Giulia: Spinal Unit of Udine
Basic Applied Myology 19 (4): 163-167, 2009
complete Spinal Cord Injury patients (ASIA Impairment Scale A) and 144 incomplete SCI patients (6 AIS B, 66 AIS C, 72 AIS D) after discharge from Neurosurgery and Intensive Care Unit. All the patients were classified complete respectively to the ASIA Impairment Scale, when no motor or sensory function was preserved in the sacral segment S4-S5. At the beginning all inpatients with complete lesion had permanent bladder catheter and all of them passed through intermittent catheterism becoming outpatients. About the patients classified as A at the AIS the average age was 38.63 years (range 16 - 67 years). The ratio between Male and Female was 4 : 1, according to International Literature (40 men e 9 women). In our sample the etiology was traumatic in 46 patients, non-traumatic in 3 patients. Road accident was the main traumatic cause (30 pt).
4
100 90 80 70 60 (%) 50 40 30 20 10 0 Flaccid patients Spastic patients
2 8
2
8
24
non traumatic attem pted sui cide weapon/ violence sport bicycle m otor cycle car
3 2 2 2 1 10 30
non tra umatic attem pte d suicide weapon/v iole nce spor t bicy cle motor cyc le car
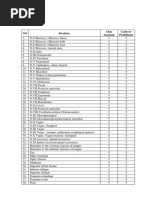
Table III: Ashworth score in SCI complete patients Clinical management of flaccid paraplegia All patients have been treated with conventional rehabilitation strategies for enhancing lower limb function after spinal cord injury focused on range of motion and stretching, upper limbs active exercise and functional training in daily mobility tasks (e.g. transferring, bed mobility, sitting) and electrical stimulation. The patients had active exercise for upper limbs and training for daily mobility tasks (transferring, bed mobility and sitting). Current studies confirm positive results for the restoring of the locomotion in SCI as an intensive taskspecific rehabilitative training, such as Body-weight Supported Treadmill Training (BWSTT), can promote supraspinal plasticity in the motor centers known to be involved in locomotion. Limited information, however, is provided describing the training progression, clinical decision making, and evaluation of progression steps. Our programs define a BWS initially set at 80% of BW. Initial training speed is chosen as the one most comfortable for the patient (0.1-0.2 m/s). Training intensity varies from 10 minutes to 45 minutes for session at a frequency of 5 days a week. The aims of the training are to decrease BWS and to increase speed in order to optimize the gait.
Table I: Etiology
L1
2 6 5 6 5 6 6 4 1 3 5
L1 D12 D10 D8 D7 D6 D5 D4 D3 D2 D1
D10
D7
D5
D3
D1
Table II: Level of Lesion All patients were classified with the Ashworth scale (Ashworth, 1964) from score 0 to 4: 0 no increase in tone; 1 spastic catch; 2 more marked increase in tone but limb easily flexed; 3 considerable increase in tone, passive movement difficult; 4 limb rigid in flexion or extension an ordinal level measure of resistance to passive movement [15]. About the patients classified with score 0, no increase in tone, at the Ashworth scale 1 had a lesion level at D2, 1 at D5, 3 at D12 and 2 at L1.
- 164 -
Cauda Equina Syndrome in Friuli-Venezia Giulia: Spinal Unit of Udine
Basic Applied Myology 19 (4): 163-167, 2009
There are several available devices used for bracing the legs in order to support standing and walking function over ground, particularly for people with complete SCI. Among the most common long-leg braces studied in the literature are the purely mechanical Parawalker [16] or the Reciprocating Gait Orthosis (RGO) [5]. These devices must be used with a walking aid (e.g. crutches or walker) for functional ambulation. The advantage of bracing is largely restricted to the general health and well being benefits related to practice of standing and the ability to ambulate shortdistance in the home or indoor settings. Energy expenditure of walking facilitated by bracing alone in spinal cord injury is extremely high and contributes to its low use. Much research is focused on the development of effective therapies directed at enhancing locomotion. Typically the majorities of these investigations focus on individuals with incomplete SCI and also predominately employ ambulation-related outcome measures. For the most part, these therapies include a form of body-weight supported treadmill training. Even if benefits can be obtained with conventional rehabilitation, locomotor training programs could be beneficial in improving lower limb muscle strength. About our casuistry of complete SCI patients (N=49), locomotion training as therapeutic exercise was realized in 15 patients, beginning with Bodyweight Supported Treadmill Training (BWSTT) and Knee Ankle Foot Orthosis (KAFO) personalized in soft-cast for the stabilization of the limbs. At discharge all patients used wheelchair for self transfer. We have experienced Patterned Electrical Stimulation assisted isometric exercise to prevent limb muscle atrophy. We know that PES-assisted isometric exercise reduces the degree of lower limb muscle atrophy in individuals with recent (~10 weeks post-injury) motor complete SCI, but not to the same extent as a comparable program of FES assisted exercise. Really a variety of electrical stimulation techniques are employed to enhance lower limb muscle structure in people with SCI. These typically involve delivering a series of electrical pulse trains to the muscle over time such that it simulates the normal exercise experience. Specific stimulation parameters (i.e., pulse width, train duration, between train intervals, method of application) and other exercise-related variables (i.e., frequency, duration, intensity, and program length) may each be varied to attain an optimal training stimulus. Really we found some difficulties to electrically stimulate denervated muscles electrical but we believe this approach could give more chance to patients in their recovery. The hope is to realize walking assisted by FES also in combination with BWSTT and biofeedback training in flaccid paraplegia even in a clinical ambit. This is a good opportunity to engage a
Fig. 1 CT scan demonstrate that the healty macroscopic apperance of the thigh of Rise2-Friuli-01LS is misleading, being due to a typical pseudo-hypertrohy related to lipodystrophy of the denervated thigh muscles. The thick layer of subcutaneous adipose tissue, toghether with those separating denervated quadriceps and hamstring muscles is at least in part responsible of the difficulties encountered in leg muscle stimulation using commercial electrical stimulators for innervated muscles. Adipose tissue also infiltrate the atrophic muscles, and thus the compact aspects of normal thigh muscles is lost. long and wide road that leaded us to be partners in the Rise2-Italy Project [1-4, 6-14]. Case Report We report a 41-year-old male patient who sustained a severe traumatic spinal cord injury in an accident at work (April 11, 2008). On clinical examination he presented with flaccid paraplegia (motor level D12). Initial magnetic resonance imaging showed a fracturedislocation D12-L1. After discharge from Neurosurgery at 15 days from trauma he was admitted in our Spinal Unit. At the clinical examination was evaluated as A at the ASIA Impairment Scale (Motor level D12, anesthesia below D12). From an electrophysiological point of view somato-sensory evoked potentials and motor evoked potentials were silent. He had begun the rehabilitation program with the purpose to reach autonomy in wheelchair locomotion and ADL. The physical rehabilitation was directed to the strengthening of upper limbs, trunk control and to preventing lower limb muscle atrophy with patterned Electrical Stimulation (quadriceps and tibialis anterior). Specific stimulation parameters (i.e., pulse width, train duration, between train intervals, method of application) were studied, but we cannot obtain an optimal training stimulus. The training was completed by passive exercise at the cycloergometer and assisted body-weight support treadmill training supported by FES. Gait over ground was not possible. At demission we verified autonomy in wheelchair locomotion and ADL, a good trunk control and an increment of aerobic performance (VO2max). Meantime - 165 -
Cauda Equina Syndrome in Friuli-Venezia Giulia: Spinal Unit of Udine
Basic Applied Myology 19 (4): 163-167, 2009
Fig 2 Human quadriceps muscle. Upper panel: normal adult. Lower panel: Muscle biopsy of Rise2Friuli_01LS at enrolment. Nine months after SCI the muscle fibers are atrophic and the interstitial tissue is increased. In the left lower corner a group of adipocytes of the infiltrating fat tissue are present. Hematoxilin-Eosin. 20x, some reinnervation of leg muscles occurred demonstrated by minimal spontaneous activity of right foot muscles, but voluntary or electrical stimulationinduced muscle contractions did not appeared. On the other hand, ES-induced dorsiflection of the ankle were achieved by transcutaneous electrical stimulation of the tibialis anterior using the Denervated Muscle Stimulation program of the STIWELL Med4 device of MED-EL (Innsbruck, Austria), that is delivering triangular or bidirectional impulses of 70 maps intensity and 150 msec duration. After this demonstration of maintained muscle contractility, the patient accepted the burden to travel to Vienna (January 21-23, 2009), to be analyzed and enrolled in the 08Rise2-Italy Program after signing the Consent and have performed a Computer Tomography analysis of his leg muscle that allowed to measure the - 166 -
thick subcutaneous fat layer and to evaluate the extent of muscle degeneration that underwent during the 9 months since Spinal Cord Injury. CT scan of left and right leg of Rise2-Friuli-01LS demonstrates that the healthy macroscopic appearance was misleading, being due to overweight and to pseudo-hypertrophic lipodystrophy of long-lasting denervated thigh muscles (Figure 1). The thick layer of subcutaneous adipose tissue, together with those separating denervated quadriceps and hamstring muscles is in part responsible of the difficulties encountered in leg muscle stimulation using commercial electrical stimulators for innervated muscles. Adipose tissue also infiltrates the atrophic muscles, and thus the compact aspect of normal thigh muscles is lost. Figure 2 shows the histological aspects of normal adult quadriceps muscle (upper panel) and the atrophic muscle of Rise2-Friuli-01LS (lower panel). After 9 months of permanent denervation muscle fibers are atrophic and the interstitial tissue is increased, but the fast and slow fiber types are still distinct by ATPase histochemistry (manuscript in preparation). In the left lower corner groups of adipocytes of the infiltrating fat tissue are present. Morphometry of muscle biopsies confirms that the muscle fibers have the characteristics of this stage of permanent denervation, while Functional Echomyography of Tibialis Anterior that the muscles are poorly perfused at rest (Manuscript in preparation). From March 2009 LS is performing Therapeutic Electrical Stimulation (TES) for denervated leg muscles, using custom-designed electrodes and stimulators developed in Vienna, Austria for the EU Project RISE (Contract n. QLG5CT-2001-02191) [3, 10]. An early result is the impressive reduction of the leg edema. This first experience strongly suggests that more subjects affected with lower motor neuron denervation of skeletal muscles than those enrolled in the EU Project RISE will benefit of the Vienna Strategy for Therapeutic Electrical Stimulation, in particular those difficult-to-stimulate due to thick subcutaneous adipose layer that hamper excitation of denervated or poorly innervated muscles. Acknowledgements The study was supported by funds of Interdepartmental Research Center of Myology of the University of Padova and Research Funds from the Ludwig Boltzmann Institute for Electrostimulation and Physical Rehabilitation at the Institute of Physical Medicine and Rehabilitation (Wilhelminenspital, Vienna, Austria). Address Correspondence to: Emiliana Bizzarini, Unit Spinale, Dipartimento di Medicina Riabilitativa, Azienda per i Servizi Sanitari N 4 Medio Friuli, Udine, Italia E-mail: biomec.imfr@ass4.sanita.fvg.it
Cauda Equina Syndrome in Friuli-Venezia Giulia: Spinal Unit of Udine
Basic Applied Myology 19 (4): 163-167, 2009
References
[9]
[1]
Bijak M, Mayr W, Rakos M, Hofer C, Lanmller H, Rafolt D, Reichel M, Sauermann S, Schmutterer C, Unger E, Russold M, Kern H. The Vienna functional electrical stimulation system for restoration of walking functions in spastic paraplegia. Artif Organs 2002; 26(3): 224-7. Bijak M, Rakos M, Hofer C, Mayr W, Strohhofer M, Raschka D, Kern H. Stimulation parameter optimization for FES supported standing up and walking in SCI patients. Artif Organs 2005; 29(3): 220-3. Boncompagni S, Kern H, Rossini K, Mayr W, Carraro U, Protasi F. Structural differentiation of skeletal muscle fibres in absence of innervation in humans. Proc Nat Acad Sci USA 2007; 104: 19339-44. Carraro U, Rossini K, Mayr W, Kern H. Muscle fiber regeneration in human permanent lower motoneuron denervation: relevance to safety and effectiveness of FES-training, which induces muscles recovery in SCI subjects. Artif Organs 2005; 29(3):187-91. Douglas R, Larson PL, D'Ambrosia R, McCall RE. The LSU reciprocating gait orthosis. Orthopaedics 1983; 6: 834-9. Gallasch E, Rafolt D, Kinz G, Fend M, Kern H, Mayr W. Evaluation of FES-induced knee joint moments in paraplegics with denervated muscles. Artif Organs 2005; 29(3): 207-11. Graupe D, Cerrel-Bazo H, Kern H, Carraro U. Walking performance, medical outcomes and patient training in FES of denervated muscles for ambulation by thoracic-level complete paraplegics. Neurol Res 2008; 30(2): 123-30. Hofer C, Mayr W, Sthr H, Unger E, Kern H. A stimulator activation of denervated muscles. Artif Organs 2002; 26(3): 276-9.
[10]
[2]
[11]
[3]
[12]
[4]
[13]
[5]
[6]
[14]
[7]
[15]
[8]
[16]
Kern H, Hofer C, Mdlin M, Forstner C, Mayr W, Richter W. Functional electrical stimulation (FES) of long-term denervated muscles in humans: Clinical observations and laboratory findings. Basic Appl Myol 2002; 12: 291-7. Kern H, Boncompagni S, Rossini K, et al. Longterm denervation in humans causes degeneration of both contractile and excitation-contraction coupling apparatus that can be reversed by functional electrical stimulation (FES). A role for myofiber regeneration? J Neuropath Exp Neurol 2004;63:919931. Kern H, Hofer C, Moedlin M, Forstner C, Raschka-Hoegler D, Mayr W, Stoehr H. Denervated muscles in humans - limitations and problems of currently used functional electrical stimulation training protocols. Artif Organs 2002; 26: 216-8. Kern H, Rossini K, Carraro U, Mayr W, Vogelauer M, Hoellwarth U, Hofer C. Muscle biopsies show that FES of denervated muscles reverses human muscle degeneration from permanent spinal motoneuron lesion. J Rehabil Res Dev 2005; 42 (3S1): 43-53 Kern H, Hofer C, Modlin M, Mayr W, Vindigni V, Zampieri S, Boncompagni S, Protasi F, Carraro U. Stable muscle atrophy in long term paraplegics with complete upper motor neuron lesion from 3- to 20-year SCI. Spinal Cord 2008; 46(4): 293-304. Mayr W, Hofer C, Bijak M, et al. Functional Electrical Stimulation (FES) of denervated muscles: existing and prospective technological solutions. Basic Appl Myol 2002; 12: 287-90. Pandyan AD, Johnson GR, Price CI, Curless RH, Barnes MP, Rodgers H. A review of the properties and limitations of the Ashworth and modified Ashworth Scales as measures of spasticity. Clin Rehabil. 1999; 13(5) :373-83. Rose GK. The principles and practice of hip guidance articulations. Prosthet Orthot Int 1979; 3: 37-43.
- 167 -
You might also like
- Mark P Jensen Hypnosis For Chronic Pain Management Workbook 2011100% (7)Mark P Jensen Hypnosis For Chronic Pain Management Workbook 2011160 pages
- Sensorimotor Control Deficiency in Recurrent Anterior Shoulder Instability Assessed With A Stabilometric Force PlatformNo ratings yetSensorimotor Control Deficiency in Recurrent Anterior Shoulder Instability Assessed With A Stabilometric Force Platform6 pages
- Pain, Trunk Muscle Strength, Spine Mobility and Disability Following Lumbar Disc SurgeryNo ratings yetPain, Trunk Muscle Strength, Spine Mobility and Disability Following Lumbar Disc Surgery5 pages
- Va Medica: Effects of Myofascial Technique in Patients With Subacute Whiplash Associated Disorders: A Pilot StudyNo ratings yetVa Medica: Effects of Myofascial Technique in Patients With Subacute Whiplash Associated Disorders: A Pilot Study0 pages
- The Effects of Scapular Stabilization Based Exercise Therapy On PDFNo ratings yetThe Effects of Scapular Stabilization Based Exercise Therapy On PDF15 pages
- Physiotherapeutic Intervention in A Patient With Spinal Cord Injury (SCI) .No ratings yetPhysiotherapeutic Intervention in A Patient With Spinal Cord Injury (SCI) .7 pages
- Aaa - THAMARA - Comparing Hot Pack, Short-Wave Diathermy, Ultrasound, and Tens On Isokinetic Strength, Pain and Functional StatusNo ratings yetAaa - THAMARA - Comparing Hot Pack, Short-Wave Diathermy, Ultrasound, and Tens On Isokinetic Strength, Pain and Functional Status9 pages
- Effects of Neural Mobilization On Pain, Straight Leg Raise Test and Disability in Patients With Radicular Low Back PainNo ratings yetEffects of Neural Mobilization On Pain, Straight Leg Raise Test and Disability in Patients With Radicular Low Back Pain4 pages
- 2020 Lamberti RCT Effectiveness of RBFT Slow Walking On Mobility in Severe Multiple SclerosisNo ratings yet2020 Lamberti RCT Effectiveness of RBFT Slow Walking On Mobility in Severe Multiple Sclerosis11 pages
- E Vects of Three Diverent Training Modalities On The Cross Sectional Area of The Lumbar Multifidus Muscle in Patients With Chronic Low Back PainNo ratings yetE Vects of Three Diverent Training Modalities On The Cross Sectional Area of The Lumbar Multifidus Muscle in Patients With Chronic Low Back Pain6 pages
- Lex D de Jong, Pieter U Dijkstra, Johan Gerritsen, Alexander CH Geurts and Klaas PostemaNo ratings yetLex D de Jong, Pieter U Dijkstra, Johan Gerritsen, Alexander CH Geurts and Klaas Postema12 pages
- Combined Arm Stretch Positioning and Neuromuscular Electrical Stimulation in Patients After Stroke A Random TrialNo ratings yetCombined Arm Stretch Positioning and Neuromuscular Electrical Stimulation in Patients After Stroke A Random Trial10 pages
- Effects of Trunk Rehabilitation With Kinesio and Placebo TapingNo ratings yetEffects of Trunk Rehabilitation With Kinesio and Placebo Taping15 pages
- Case Report Rehabilitation Program in A Patient With A Displaced Femoral Neck FractureNo ratings yetCase Report Rehabilitation Program in A Patient With A Displaced Femoral Neck Fracture26 pages
- Pelvic Muscle Rehabilitation A StandardiNo ratings yetPelvic Muscle Rehabilitation A Standardi8 pages
- Research Article: Effects of Low-Level Laser Therapy and Eccentric Exercises in The Treatment of Patellar TendinopathyNo ratings yetResearch Article: Effects of Low-Level Laser Therapy and Eccentric Exercises in The Treatment of Patellar Tendinopathy7 pages
- Case Report Rehabilitation Program in A Patient With Intertrochanteric Femoral FractureNo ratings yetCase Report Rehabilitation Program in A Patient With Intertrochanteric Femoral Fracture26 pages
- Sex-Related Differences and Effects of Short and LNo ratings yetSex-Related Differences and Effects of Short and L16 pages
- Evaluation of The Lateral Instability of The Ankle by Inversion Simulation Device and Assessment of The Rehabilitation ProgramNo ratings yetEvaluation of The Lateral Instability of The Ankle by Inversion Simulation Device and Assessment of The Rehabilitation Program13 pages
- Heavy-Load Eccentric Calf Muscle Training For The Treatment of Chronic Achilles TendinosisNo ratings yetHeavy-Load Eccentric Calf Muscle Training For The Treatment of Chronic Achilles Tendinosis8 pages
- Assessment of The Anterior Talofibular Ligament Thickness 2017 Journal of MeNo ratings yetAssessment of The Anterior Talofibular Ligament Thickness 2017 Journal of Me5 pages
- Brain: Altering Spinal Cord Excitability Enables Voluntary Movements After Chronic Complete Paralysis in HumansNo ratings yetBrain: Altering Spinal Cord Excitability Enables Voluntary Movements After Chronic Complete Paralysis in Humans16 pages
- Characteristics of Myofascial Pain Syndrome of The Infraspinatus MuscleNo ratings yetCharacteristics of Myofascial Pain Syndrome of The Infraspinatus Muscle9 pages
- Case Report Rehabilitation Program in Patient With Ankle FractureNo ratings yetCase Report Rehabilitation Program in Patient With Ankle Fracture26 pages
- Case Report Rehabilitation Program in A Patient With Tibial Condyle FractureNo ratings yetCase Report Rehabilitation Program in A Patient With Tibial Condyle Fracture26 pages
- Original Paper: Lumbar Disk Herniations - Clinical Status, Diagnosis, Imaging, Surgical Treatment and Global OutcomeNo ratings yetOriginal Paper: Lumbar Disk Herniations - Clinical Status, Diagnosis, Imaging, Surgical Treatment and Global Outcome6 pages
- Case Report Rehabilitation Program in A Patient With Fracture of The Distal FemurNo ratings yetCase Report Rehabilitation Program in A Patient With Fracture of The Distal Femur26 pages
- Research Article: Correlation Between TMD and Cervical Spine Pain and Mobility: Is The Whole Body Balance TMJ Related?No ratings yetResearch Article: Correlation Between TMD and Cervical Spine Pain and Mobility: Is The Whole Body Balance TMJ Related?8 pages
- Comparison of Effect of Hip Joint Mobilization and Hip Joint Muscle Strengthening Exercises With Knee Osteoarthritis A. Tanvi, R. Amrita, R. Deepak, P. Kopal Srji Vol 3-Issue 1 Year 2014100% (1)Comparison of Effect of Hip Joint Mobilization and Hip Joint Muscle Strengthening Exercises With Knee Osteoarthritis A. Tanvi, R. Amrita, R. Deepak, P. Kopal Srji Vol 3-Issue 1 Year 201413 pages
- Case Report: Rehabilitation Program in A Patient With Congenital Dysplasia and Subluxation of The HipNo ratings yetCase Report: Rehabilitation Program in A Patient With Congenital Dysplasia and Subluxation of The Hip26 pages
- The immediate effects of specific-myofascial release technique versus Proprioceptive neuromuscular facilitation Hold-relax technique on hamstring flexibility in sub-acute and chronic stroke patients–An experimental studyNo ratings yetThe immediate effects of specific-myofascial release technique versus Proprioceptive neuromuscular facilitation Hold-relax technique on hamstring flexibility in sub-acute and chronic stroke patients–An experimental study5 pages
- Validity of The Lateral Gliding Test As Tool ForNo ratings yetValidity of The Lateral Gliding Test As Tool For7 pages
- The Timing of Rehabilitation Commencement After Reconstruction of the Anterior Cruciate LigamentNo ratings yetThe Timing of Rehabilitation Commencement After Reconstruction of the Anterior Cruciate Ligament108 pages
- Effects of Respiratory-Muscle Exercise On Spinal Curvature100% (1)Effects of Respiratory-Muscle Exercise On Spinal Curvature6 pages
- Lap - Sementara - Nervus Cranialis & SpinalisNo ratings yetLap - Sementara - Nervus Cranialis & Spinalis11 pages
- Body Systems Webquest!: System: The Integumentary SystemNo ratings yetBody Systems Webquest!: System: The Integumentary System2 pages
- The Nervous System: MC102 Nur - Human Anatomy and Physiology March 30 - April 4, 2020No ratings yetThe Nervous System: MC102 Nur - Human Anatomy and Physiology March 30 - April 4, 2020124 pages
- Lesson Plan 4 - Peripheral Nervous SystemNo ratings yetLesson Plan 4 - Peripheral Nervous System6 pages
- Lecture Notes For Chapter 14 (Autonomic Nervous System) PDFNo ratings yetLecture Notes For Chapter 14 (Autonomic Nervous System) PDF60 pages
- Organisation of The Nervous System: Form 5 Biology Chapter 3 Body Coordination (A)No ratings yetOrganisation of The Nervous System: Form 5 Biology Chapter 3 Body Coordination (A)24 pages
- Chapter 13 - The Peripheral Nervous System and Reflex Activity100% (1)Chapter 13 - The Peripheral Nervous System and Reflex Activity53 pages
- General Anatomy-Nervous System Lec 1-Dr - GosaiNo ratings yetGeneral Anatomy-Nervous System Lec 1-Dr - Gosai18 pages
- Foundations of Behavioral Neuroscience 10th Edition Neil Carlson all chapter instant download100% (1)Foundations of Behavioral Neuroscience 10th Edition Neil Carlson all chapter instant download65 pages
- Mark P Jensen Hypnosis For Chronic Pain Management Workbook 2011Mark P Jensen Hypnosis For Chronic Pain Management Workbook 2011
- Sensorimotor Control Deficiency in Recurrent Anterior Shoulder Instability Assessed With A Stabilometric Force PlatformSensorimotor Control Deficiency in Recurrent Anterior Shoulder Instability Assessed With A Stabilometric Force Platform
- Pain, Trunk Muscle Strength, Spine Mobility and Disability Following Lumbar Disc SurgeryPain, Trunk Muscle Strength, Spine Mobility and Disability Following Lumbar Disc Surgery
- Va Medica: Effects of Myofascial Technique in Patients With Subacute Whiplash Associated Disorders: A Pilot StudyVa Medica: Effects of Myofascial Technique in Patients With Subacute Whiplash Associated Disorders: A Pilot Study
- The Effects of Scapular Stabilization Based Exercise Therapy On PDFThe Effects of Scapular Stabilization Based Exercise Therapy On PDF
- Physiotherapeutic Intervention in A Patient With Spinal Cord Injury (SCI) .Physiotherapeutic Intervention in A Patient With Spinal Cord Injury (SCI) .
- Aaa - THAMARA - Comparing Hot Pack, Short-Wave Diathermy, Ultrasound, and Tens On Isokinetic Strength, Pain and Functional StatusAaa - THAMARA - Comparing Hot Pack, Short-Wave Diathermy, Ultrasound, and Tens On Isokinetic Strength, Pain and Functional Status
- Effects of Neural Mobilization On Pain, Straight Leg Raise Test and Disability in Patients With Radicular Low Back PainEffects of Neural Mobilization On Pain, Straight Leg Raise Test and Disability in Patients With Radicular Low Back Pain
- 2020 Lamberti RCT Effectiveness of RBFT Slow Walking On Mobility in Severe Multiple Sclerosis2020 Lamberti RCT Effectiveness of RBFT Slow Walking On Mobility in Severe Multiple Sclerosis
- E Vects of Three Diverent Training Modalities On The Cross Sectional Area of The Lumbar Multifidus Muscle in Patients With Chronic Low Back PainE Vects of Three Diverent Training Modalities On The Cross Sectional Area of The Lumbar Multifidus Muscle in Patients With Chronic Low Back Pain
- Lex D de Jong, Pieter U Dijkstra, Johan Gerritsen, Alexander CH Geurts and Klaas PostemaLex D de Jong, Pieter U Dijkstra, Johan Gerritsen, Alexander CH Geurts and Klaas Postema
- Combined Arm Stretch Positioning and Neuromuscular Electrical Stimulation in Patients After Stroke A Random TrialCombined Arm Stretch Positioning and Neuromuscular Electrical Stimulation in Patients After Stroke A Random Trial
- Effects of Trunk Rehabilitation With Kinesio and Placebo TapingEffects of Trunk Rehabilitation With Kinesio and Placebo Taping
- Case Report Rehabilitation Program in A Patient With A Displaced Femoral Neck FractureCase Report Rehabilitation Program in A Patient With A Displaced Femoral Neck Fracture
- Research Article: Effects of Low-Level Laser Therapy and Eccentric Exercises in The Treatment of Patellar TendinopathyResearch Article: Effects of Low-Level Laser Therapy and Eccentric Exercises in The Treatment of Patellar Tendinopathy
- Case Report Rehabilitation Program in A Patient With Intertrochanteric Femoral FractureCase Report Rehabilitation Program in A Patient With Intertrochanteric Femoral Fracture
- Sex-Related Differences and Effects of Short and LSex-Related Differences and Effects of Short and L
- Evaluation of The Lateral Instability of The Ankle by Inversion Simulation Device and Assessment of The Rehabilitation ProgramEvaluation of The Lateral Instability of The Ankle by Inversion Simulation Device and Assessment of The Rehabilitation Program
- Heavy-Load Eccentric Calf Muscle Training For The Treatment of Chronic Achilles TendinosisHeavy-Load Eccentric Calf Muscle Training For The Treatment of Chronic Achilles Tendinosis
- Assessment of The Anterior Talofibular Ligament Thickness 2017 Journal of MeAssessment of The Anterior Talofibular Ligament Thickness 2017 Journal of Me
- Brain: Altering Spinal Cord Excitability Enables Voluntary Movements After Chronic Complete Paralysis in HumansBrain: Altering Spinal Cord Excitability Enables Voluntary Movements After Chronic Complete Paralysis in Humans
- Characteristics of Myofascial Pain Syndrome of The Infraspinatus MuscleCharacteristics of Myofascial Pain Syndrome of The Infraspinatus Muscle
- Case Report Rehabilitation Program in Patient With Ankle FractureCase Report Rehabilitation Program in Patient With Ankle Fracture
- Case Report Rehabilitation Program in A Patient With Tibial Condyle FractureCase Report Rehabilitation Program in A Patient With Tibial Condyle Fracture
- Original Paper: Lumbar Disk Herniations - Clinical Status, Diagnosis, Imaging, Surgical Treatment and Global OutcomeOriginal Paper: Lumbar Disk Herniations - Clinical Status, Diagnosis, Imaging, Surgical Treatment and Global Outcome
- Case Report Rehabilitation Program in A Patient With Fracture of The Distal FemurCase Report Rehabilitation Program in A Patient With Fracture of The Distal Femur
- Research Article: Correlation Between TMD and Cervical Spine Pain and Mobility: Is The Whole Body Balance TMJ Related?Research Article: Correlation Between TMD and Cervical Spine Pain and Mobility: Is The Whole Body Balance TMJ Related?
- Comparison of Effect of Hip Joint Mobilization and Hip Joint Muscle Strengthening Exercises With Knee Osteoarthritis A. Tanvi, R. Amrita, R. Deepak, P. Kopal Srji Vol 3-Issue 1 Year 2014Comparison of Effect of Hip Joint Mobilization and Hip Joint Muscle Strengthening Exercises With Knee Osteoarthritis A. Tanvi, R. Amrita, R. Deepak, P. Kopal Srji Vol 3-Issue 1 Year 2014
- Case Report: Rehabilitation Program in A Patient With Congenital Dysplasia and Subluxation of The HipCase Report: Rehabilitation Program in A Patient With Congenital Dysplasia and Subluxation of The Hip
- The immediate effects of specific-myofascial release technique versus Proprioceptive neuromuscular facilitation Hold-relax technique on hamstring flexibility in sub-acute and chronic stroke patients–An experimental studyThe immediate effects of specific-myofascial release technique versus Proprioceptive neuromuscular facilitation Hold-relax technique on hamstring flexibility in sub-acute and chronic stroke patients–An experimental study
- The Timing of Rehabilitation Commencement After Reconstruction of the Anterior Cruciate LigamentThe Timing of Rehabilitation Commencement After Reconstruction of the Anterior Cruciate Ligament
- Effects of Respiratory-Muscle Exercise On Spinal CurvatureEffects of Respiratory-Muscle Exercise On Spinal Curvature
- Body Systems Webquest!: System: The Integumentary SystemBody Systems Webquest!: System: The Integumentary System
- The Nervous System: MC102 Nur - Human Anatomy and Physiology March 30 - April 4, 2020The Nervous System: MC102 Nur - Human Anatomy and Physiology March 30 - April 4, 2020
- Lecture Notes For Chapter 14 (Autonomic Nervous System) PDFLecture Notes For Chapter 14 (Autonomic Nervous System) PDF
- Organisation of The Nervous System: Form 5 Biology Chapter 3 Body Coordination (A)Organisation of The Nervous System: Form 5 Biology Chapter 3 Body Coordination (A)
- Chapter 13 - The Peripheral Nervous System and Reflex ActivityChapter 13 - The Peripheral Nervous System and Reflex Activity
- Foundations of Behavioral Neuroscience 10th Edition Neil Carlson all chapter instant downloadFoundations of Behavioral Neuroscience 10th Edition Neil Carlson all chapter instant download