Lecture 9
Lecture 9
Uploaded by
EsraRamosCopyright:
Available Formats
Lecture 9
Lecture 9
Uploaded by
EsraRamosOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Copyright:
Available Formats
Lecture 9
Lecture 9
Uploaded by
EsraRamosCopyright:
Available Formats
Eating and Sleep
Disorders
Chapter 8
Eating Disorders: An Overview
Two Major Types of DSM-IV Eating Disorders
Anorexia nervosa and bulimia nervosa
Both involve severe disruptions in eating behavior
Both involve extreme fear and apprehension about gaining weight
Both have strong sociocultural origins Westernized views
Bulimia Nervosa: Overview and Defining Features
Binge Eating Hallmark of Bulimia
Binge Eating excess amounts of food
Eating is perceived as uncontrollable
Compensatory Behaviors
Purging Self-induced vomiting, diuretics, laxatives
Some exercise excessively, whereas others fast
DSM-IV Subtypes of Bulimia
Purging subtype Most common subtype (e.g., vomiting, laxatives,
enemas)
Nonpurging subtype About one-third of bulimics (e.g., excess
exercise, fasting)
Bulimia Nervosa: Overview and Defining Features (cont.)
Associated Features
Most are over concerned with body shape, fear gaining weight
Most have comorbid psychological disorders
Purging methods can result in severe medical problems
Most are within 10% of target body weight
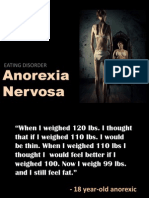
Anorexia Nervosa: Overview and Defining Features
Successful Weight Loss Hallmark of Anorexia
Intense fear of obesity and losing control over eating
Anorexics show a relentless pursuit of thinness, often beginning with
dieting
Defined as 15% below expected weight
DSM-IV Subtypes of Anorexia
Restricting subtype Limit caloric intake via diet and fasting
Binge-eating-purging subtype About 50% of anorexics
Associated Features
Most show marked disturbance in body image
Methods of weight loss can have severe life threatening medical
consequences
Most are comorbid for other psychological disorders
Binge-Eating Disorder: Overview and Defining Features
Binge-Eating Disorder Appendix of DSM-IV
Experimental diagnostic category
Engage in food binges, but do not engage in compensatory
behaviors
Associated Features
Many persons with binge-eating disorder are obese
Share similar concerns as anorexics and bulimics regarding shape
and weight
Bulimia and Anorexia: Facts and Statistics
Bulimia
Majority are female, with onset around 16 to 19 years of age
Lifetime prevalence is about 1.1% for females, 0.1% for males
6-8% of college women suffer from bulimia
Tends to be chronic if left untreated
Anorexia
Majority are female and white, from middle-to-upper middle class
families
Usually develops around age 13 or early adolescence
Tends to be more chronic and resistant to treatment than bulimia
Both Bulimia and Anorexia Are Found in Westernized Cultures
Causes of Bulimia and Anorexia: Toward an Integrative Model
Media and Cultural Considerations
Being thin = Success, happiness....really?
Cultural imperative for thinness translates into dieting
Standards of ideal body size change as much as clothes
With improved nutrition, media standards of the ideal are difficult to
achieve
Psychological and Behavioral Considerations
Low sense of personal control and self-confidence
Food restriction often leads to a preoccupation with food
An Integrative Model
Male and female ratings of body size
Figure 8.3
An integrative causal model of eating disorders
Figure 8.5
Medical and Psychological Treatment of Bulimia Nervosa
Drug Treatments
Antidepressants can help reduce binging and purging behavior
Antidepressants are not efficacious in the long-term
Psychosocial Treatments
Cognitive-behavior therapy (CBT) is the treatment of choice
Interpersonal psychotherapy results in long-term gains similar to
CBT
Medical and Psychological Treatment of Anorexia Nervosa
Medical Treatment
There are none with demonstrated efficacy
Psychological Treatment
Weight restoration First and easiest goal to achieve
Treatment involves education, behavioral, and cognitive
interventions
Treatment often involves the family
Long-term prognosis for anorexia is poorer than for bulimia
Other Eating Disorders
Rumination Disorder
Chronic regurgitation and reswallowing of partially digested food
Most prevalent among infants and persons with mental retardation
Pica
Repetitive eating of inedible substances
Seen in infants and persons with severe developmental/intellectual
disabilities
Treatment involves operant procedures
Feeding Disorder
Failure to eat adequately, resulting in insufficient weight gain
Disorder of infancy and early childhood
Treatment involves regulating eating and family therapy
Sleep Disorders: An Overview
Two Major Types of DSM-IV Sleep Disorders
Dyssomnias Difficulties in getting enough sleep, problems in the
timing of sleep, and complaints about the quality of sleep
Parasomnias Abnormal behavioral and physiological events
during sleep
Assessment of Disordered Sleep: Polysomnographic (PSG) Evaluation
Electroencephalograph (EEG) Leg movements and brain wave
activity
Electrooculograph (EOG) Eye movements
Electromyography (EMG) Muscle movements
Includes detailed history, assessment of sleep hygiene and sleep
efficiency
The Dyssomnias: Overview and Defining Features of Insomnia
Insomnia and Primary Insomnia
One of the most common sleep disorders
Difficulties initiating sleep, maintaining sleep, and/or nonrestorative
sleep
Primary insomnia Means insomnia unrelated to any other condition
(rare!)
Facts and Statistics
Insomnia is often associated with medical and/or psychological
conditions
Females reported insomnia twice as often as males
Associated Features
Many have unrealistic expectations about sleep
Many believe lack of sleep will be more disruptive than it usually is
The Dyssomnias: Overview and Defining Features of Hypersomnia
Hypersomnia and Primary Hypersomnia
Problems related to sleeping too much or excessive sleep
Person experiences excessive sleepiness as a problem
Primary hypersomnia Means hypersomnia unrelated to any other
condition (rare!)
Facts and Statistics
About 39% have a family history of hypersomnia
Hypersomnia is often associated with medical and/or psychological
conditions
Associated Features
Complain of sleepiness throughout the day, but do sleep through
the night
The Dyssomnias: Overview and Defining Features of Narcolepsy
Narcolepsy
Daytime sleepiness and cataplexy
Cataplexic attacks REM sleep, precipitated by strong emotion
Facts and Statistics
Narcolepsy is rare Affects about .03% to .16% of the population
Equally distributed between males and females
Onset during adolescence, and typically improves over time
Associated Features
Cataplexy, sleep paralysis, and hypnagogic hallucinations improve
over time
Daytime sleepiness does not remit without treatment
The Dyssomnias: Overview of Breathing-Related Sleep Disorders
Breathing-Related Sleep Disorders
Sleepiness during the day and/or disrupted sleep at night
Sleep apnea Restricted air flow and/or brief cessations of
breathing
Subtypes of Sleep Apnea
Obstructive sleep apnea (OSA) Airflow stops, but respiratory
system works
Central sleep apnea (CSA) Respiratory systems stops for brief
periods
Mixed sleep apnea Combination of OSA and CSA
The Dyssomnias: Overview of Breathing-Related Sleep Disorders (cont.)
Facts and Statistics
More common in males, occurs in 1-2% of population
Associated Features
Persons are usually minimally aware of apnea problem
Often snore, sweat during sleep, wake frequently, and have
morning headaches
May experience episodes of falling asleep during the day
Circadian Rhythm Sleep Disorders
Circadian Rhythm Disorders
Disturbed sleep (i.e., either insomnia or excessive sleepiness
during the day)
Problem is due to brains inability to synchronize day and night
Nature of Circadian Rhythms and Bodys Biological Clock
Circadian Rhythms Do not follow a 24 hour clock
Suprachiasmatic nucleus The brains biological clock, stimulates
melatonin
Types of Circadian Rhythm Disorders
Jet lag type Sleep problems related to crossing time zones
Shift work type Sleep problems related to changing work
schedules
Medical Treatments
Insomnia
Benzodiazepines and over-the-counter sleep medications
Prolonged use can cause rebound insomnia, dependence
Best as short-term solution
Hypersomnia and Narcolepsy
Stimulants (i.e., Ritalin)
Cataplexy is usually treated with antidepressants
Medical Treatments
Breathing-Related Sleep Disorders
May include medications, weight loss, or mechanical devices
Circadian Rhythm Sleep Disorders
Phase delays Moving bedtime later (best approach)
Phase advances Moving bedtime earlier (more difficult)
Use of very bright light Trick the brains biological clock
Psychological Treatments
Relaxation and Stress Reduction
Reduces stress and assists with sleep
Modify unrealistic expectations about sleep
Stimulus Control Procedures
Improved sleep hygiene Bedroom is a place for sleep and sex
only
For children Setting a regular bedtime routine
Combined Treatments
Insomnia Short-term medication plus psychotherapy is best
Lack evidence for the efficacy of combined treatments with other
dyssomnias
The Parasomnias: Nature and General Overview
Nature of Parasomnias
The problem is not with sleep itself
Problem is abnormal events during sleep, or shortly after waking
Two Classes of Parasomnias
Those that occur during REM (i.e., dream) sleep
nightmare disorder
Those that occur during non-REM (i.e., non-dream) sleep
sleep terror
sleep-walking
The Parasomnias: Overview of Nightmare Disorder
Nightmare Disorder
Occurs during REM sleep
Involves distressful and disturbing dreams
Such dreams interfere with daily life functioning and interrupt sleep
Facts and Associated Features
Dreams often awaken the sleeper
Problem is more common in children than adults
The Parasomnias: Overview of Nightmare Disorder (cont.)
Sleep Terror Disorder
Involves recurrent episodes of panic-like symptoms
Occurs during non-REM sleep
Facts and Associated Features
Problem is more common in children than adults
Often noted by a piercing scream
Child cannot be easily awakened during the episode and has little
memory of it
Treatment
Often involves a wait-and-see posture
Antidepressants (i.e., imipramine) or benzodiazepines for severe cases
Scheduled awakenings prior to the sleep terror can eliminate the problem
The Parasomnias: Overview of Sleep Walking Disorder
Sleep Walking Disorder Somnambulism
Occurs during non-REM sleep
Usually during first few hours of deep sleep
Person must leave the bed
Facts and Associated Features
Difficult, but not dangerous, to wake someone during the episode
Problem is more common in children than adults
Problem usually resolves on its own without treatment
Seems to run in families
Related Conditions
Nocturnal eating syndrome Person eats while asleep
An integrative multidimensional model of sleep disturbance
Figure 8.7
You might also like
- Psychiatric BankDocument169 pagesPsychiatric BankThatcher M Lima100% (31)
- BPS Diagnosis-Policy Guidance PDFDocument3 pagesBPS Diagnosis-Policy Guidance PDFDavidLeeNo ratings yet
- The Science and Folklore of Traumatic AmnesiaDocument5 pagesThe Science and Folklore of Traumatic AmnesiaKami75% (8)
- Bicomong Vs AlmanzaDocument2 pagesBicomong Vs AlmanzaEsraRamos100% (1)
- Annotated BibliographyDocument18 pagesAnnotated Bibliographyapi-321112294100% (1)
- Occupational Therapy Using A Sensory Integration-Based Approach With Adult PopulationsDocument2 pagesOccupational Therapy Using A Sensory Integration-Based Approach With Adult PopulationsThe American Occupational Therapy Association75% (4)
- Eating and Sleep DisordersDocument64 pagesEating and Sleep DisordersEsraRamosNo ratings yet
- Eating and Sleep DisordersDocument88 pagesEating and Sleep DisordersFrancis ZerdaNo ratings yet
- Somatoform and Sleep DisordersDocument24 pagesSomatoform and Sleep DisordersSegun Dele-davidsNo ratings yet
- Anorexia Nervosa: Dr. K.RavishankarDocument17 pagesAnorexia Nervosa: Dr. K.RavishankarChaitanya Kiran PullelaNo ratings yet
- Eating and Sleep-Wake DisordersDocument34 pagesEating and Sleep-Wake DisordersAnnie SumacotNo ratings yet
- Eating Disorders: Trisha IrelandDocument38 pagesEating Disorders: Trisha IrelandRegina PunNo ratings yet
- Anorexia Nervosa: Eating DisorderDocument21 pagesAnorexia Nervosa: Eating DisorderFrances Oscar GaviolaNo ratings yet
- Module 8 Eating and Sleep DisordersDocument36 pagesModule 8 Eating and Sleep DisordersCedric LosteNo ratings yet
- Sleeping & Eating DisordersDocument35 pagesSleeping & Eating DisordersTodd ColeNo ratings yet
- Eating Disorder Lecture 10Document39 pagesEating Disorder Lecture 10Mawadh AlsbhiNo ratings yet
- Mood Disorders - ArafatDocument40 pagesMood Disorders - Arafatمرتضى محمد منصورNo ratings yet
- ch07 BipolarDocument21 pagesch07 Bipolarpsychology.sara.cNo ratings yet
- Lecture INST-100091 2023 10 17 18 42 57Document22 pagesLecture INST-100091 2023 10 17 18 42 57Stuti PatelNo ratings yet
- Eating Disorders: Anorexia vs. BulimiaDocument17 pagesEating Disorders: Anorexia vs. BulimiabajaocNo ratings yet
- Feeding and Eating DisordersDocument19 pagesFeeding and Eating Disordersnoortaha99.57No ratings yet
- Eating disordersDocument6 pagesEating disordersUmair anwar Umair anwarNo ratings yet
- Anorexia Vs BulimiaDocument19 pagesAnorexia Vs BulimiaNylia AtibiNo ratings yet
- Weight-Related Concerns and Disorders Among Adolescents: PKK 3203 Nutrition Throughout The Life CycleDocument48 pagesWeight-Related Concerns and Disorders Among Adolescents: PKK 3203 Nutrition Throughout The Life Cyclechen chendaeNo ratings yet
- Eating Disorders: by Group A1: Marwa Alsaleh, Zahra Almousa, Maha Alshrywi, Israa AlagnamDocument28 pagesEating Disorders: by Group A1: Marwa Alsaleh, Zahra Almousa, Maha Alshrywi, Israa AlagnamYuki HimeNo ratings yet
- Sleep Disorders in The ElderlyDocument50 pagesSleep Disorders in The ElderlykikimarioNo ratings yet
- Cerebral PalsyDocument96 pagesCerebral PalsyRahini PaniNo ratings yet
- Feeding and Eating DisordersDocument41 pagesFeeding and Eating DisordersJoanNo ratings yet
- Gizi NeuroDocument26 pagesGizi NeuroAndi RiskaNo ratings yet
- Eating Disorders: Carla R MarchiraDocument37 pagesEating Disorders: Carla R MarchiraLira Riana AkbarNo ratings yet
- Eating and Feeding DisordersDocument53 pagesEating and Feeding DisorderssantospsychiatrymdNo ratings yet
- Anorexia NervosaDocument53 pagesAnorexia NervosaJayalakshmi JRNo ratings yet
- Psy240 Winter2024 Lecture6Document76 pagesPsy240 Winter2024 Lecture6aya.mazin99No ratings yet
- Eating Disorder Anorexia Nervosa Bulimia NervosaDocument50 pagesEating Disorder Anorexia Nervosa Bulimia NervosaJemi LoriNo ratings yet
- Eating DisordersDocument36 pagesEating Disordersclarence_parales100% (1)
- REREVDocument6 pagesREREVMaria Kyla VicenteNo ratings yet
- EATIING DISORDERS Fall 2023-2024Document64 pagesEATIING DISORDERS Fall 2023-2024bill haddNo ratings yet
- Health Psy Final NotlarıDocument13 pagesHealth Psy Final NotlarıSümeyye KüçükaliNo ratings yet
- Eating Disorders: by Dr. Min Min Phyo 20 August 2019Document74 pagesEating Disorders: by Dr. Min Min Phyo 20 August 2019thu thuNo ratings yet
- Approach To Floppy Infant: LT Col (DR) Bindu T Nair Professor (Pediatrics)Document56 pagesApproach To Floppy Infant: LT Col (DR) Bindu T Nair Professor (Pediatrics)Dorjee SengeNo ratings yet
- Anorexia Nervosa and Force FeedingDocument3 pagesAnorexia Nervosa and Force FeedingGalvinLeeNo ratings yet
- 10TCA in SportsDocument26 pages10TCA in SportsAlejandro EVNo ratings yet
- Eating Disorders: Dr. Shastri MotilalDocument26 pagesEating Disorders: Dr. Shastri MotilalSaraNo ratings yet
- Eating DisordersDocument15 pagesEating DisordersJana Marie CorpuzNo ratings yet
- Ma Cristy L. Exconde, MD, FPOGSDocument62 pagesMa Cristy L. Exconde, MD, FPOGSCAROL ANN PATITICO100% (1)
- CHILD & ADOLESCENT PSYCHIATRY - Eating Disorder and Others For OTDocument9 pagesCHILD & ADOLESCENT PSYCHIATRY - Eating Disorder and Others For OTEmmanuel AbiolaNo ratings yet
- Rathus PSYCH 3e PPT Chapter04Document76 pagesRathus PSYCH 3e PPT Chapter04Mark Levi CorpuzNo ratings yet
- Travelling Across Multiple Time Zones With Terror: Circadian Rhythm Disorders Brain SleepDocument4 pagesTravelling Across Multiple Time Zones With Terror: Circadian Rhythm Disorders Brain SleepQueen Anne Bobier - tomacderNo ratings yet
- Schizophrenia Fall 07Document62 pagesSchizophrenia Fall 07srinivasanaNo ratings yet
- Neurocognitive DisordersDocument56 pagesNeurocognitive Disorderskessiyathomas2No ratings yet
- Somatic Symptom Illness and NeurodevelopmentalDocument39 pagesSomatic Symptom Illness and NeurodevelopmentalMiss OpinionatedNo ratings yet
- PhysioDocument59 pagesPhysioMary LynnNo ratings yet
- Multiple SclerosisDocument3 pagesMultiple Sclerosisapi-3822433No ratings yet
- EATING DISORDERS-final Copy by ShamDocument63 pagesEATING DISORDERS-final Copy by Shamlionel andreaNo ratings yet
- Disordered Eating Vs Eating DisorderDocument34 pagesDisordered Eating Vs Eating Disordererwan berhanNo ratings yet
- Alcoholism: Alcohol Withdrawal SymptomsDocument8 pagesAlcoholism: Alcohol Withdrawal SymptomsMonnesJNo ratings yet
- Week 9 Abpsych - ZTDocument14 pagesWeek 9 Abpsych - ZTJay Rome TropiaNo ratings yet
- Als Overview enDocument71 pagesAls Overview enkharaNo ratings yet
- CPDocument86 pagesCPMahnoorNo ratings yet
- Cerebral Palsy: PediatricsDocument50 pagesCerebral Palsy: PediatricsRANJIT GOGOINo ratings yet
- Eatiing DisordersDocument69 pagesEatiing DisordersMasa MasaNo ratings yet
- MHN BipolarDocument35 pagesMHN Bipolarsinuaish syaNo ratings yet
- CP UpdatedDocument45 pagesCP UpdatedSivakumar Kathuu KarthikeyanNo ratings yet
- Pain Management 2Document48 pagesPain Management 2bensoulNo ratings yet
- W7 Lesson 9 - Diet and Eating Disorders - PresentationDocument60 pagesW7 Lesson 9 - Diet and Eating Disorders - Presentationmontanocath660No ratings yet
- Del Rosario Vs ConananDocument2 pagesDel Rosario Vs ConananEsraRamosNo ratings yet
- 1st and 2nd SetDocument8 pages1st and 2nd SetEsraRamosNo ratings yet
- Partnership 2nd Part of Consolidation (Luis)Document41 pagesPartnership 2nd Part of Consolidation (Luis)EsraRamosNo ratings yet
- Ram Part - Page 12 & 13Document52 pagesRam Part - Page 12 & 13EsraRamosNo ratings yet
- Page 12 Agency CompleteDocument109 pagesPage 12 Agency CompleteEsraRamosNo ratings yet
- PARTNERSHIP - 2nd Outline - Page 4-6Document4 pagesPARTNERSHIP - 2nd Outline - Page 4-6EsraRamosNo ratings yet
- Consolidated Page 17-18 - Trust - CompleteDocument68 pagesConsolidated Page 17-18 - Trust - CompleteEsraRamosNo ratings yet
- Agency - Page 11 - CompleteDocument47 pagesAgency - Page 11 - CompleteEsraRamosNo ratings yet
- Complete First HW PartnershipDocument202 pagesComplete First HW PartnershipEsraRamosNo ratings yet
- Agency - Page 10 - Without 4th and 6th PartDocument40 pagesAgency - Page 10 - Without 4th and 6th PartEsraRamosNo ratings yet
- BUS ORG - PAT - 5th Part of ConsolidationDocument8 pagesBUS ORG - PAT - 5th Part of ConsolidationEsraRamosNo ratings yet
- Agency Page 14-15 1st PartDocument26 pagesAgency Page 14-15 1st PartEsraRamosNo ratings yet
- BUS ORG - PAT - 5th Part of ConsolidationDocument15 pagesBUS ORG - PAT - 5th Part of ConsolidationEsraRamosNo ratings yet
- Hayashi 2004Document3 pagesHayashi 2004Ribhav GuptaNo ratings yet
- Patient Bill of Rights and Responsibilities (2)Document40 pagesPatient Bill of Rights and Responsibilities (2)anantasevtianaNo ratings yet
- PSY70203 CACP - W1 Introduction and Concept of Child PsychopathologyDocument17 pagesPSY70203 CACP - W1 Introduction and Concept of Child PsychopathologyDeepika L.No ratings yet
- Challenging Behaviors Tool KitDocument81 pagesChallenging Behaviors Tool KitDiyana HalimNo ratings yet
- COMMUNITY PSYCHOLOGY - Handout For StudentsDocument10 pagesCOMMUNITY PSYCHOLOGY - Handout For StudentsArunima RoyNo ratings yet
- Wa0007.Document15 pagesWa0007.royanraj400No ratings yet
- Children of AlcoholicsDocument36 pagesChildren of AlcoholicsAldo Realized Garcia100% (2)
- PSYCHOPATHOLOGYDocument5 pagesPSYCHOPATHOLOGYMaheshwari ANo ratings yet
- Assignment 1, Chapter 3Document4 pagesAssignment 1, Chapter 3Aishwarya MandhalkarNo ratings yet
- CEP BPSD Discussion Guide ENG RFCG Updated2019 PDFDocument8 pagesCEP BPSD Discussion Guide ENG RFCG Updated2019 PDFM.DalaniNo ratings yet
- University of The CordillerasDocument5 pagesUniversity of The CordillerasGesler Pilvan SainNo ratings yet
- Suicidal Risk Assessment - Becks Suicide Intent ScaleDocument3 pagesSuicidal Risk Assessment - Becks Suicide Intent Scalednutter012576100% (3)
- NCP FearsDocument1 pageNCP FearsFrances MercadoNo ratings yet
- CBT Depression HomeworkDocument7 pagesCBT Depression Homeworkafmtqdkpe100% (1)
- AutismDocument2 pagesAutismapi-346209737No ratings yet
- UntitledDocument20 pagesUntitledSid KolgeNo ratings yet
- Sex Lec Eleven ThreeDocument11 pagesSex Lec Eleven ThreeEmma DungogNo ratings yet
- Section 2: Antisocial Behavior: Goals of The ExerciseDocument3 pagesSection 2: Antisocial Behavior: Goals of The ExerciseSalma IbrahimNo ratings yet
- 【emotional appeal核心】Mental health messages on TikTok Analysing the use of emotional appeals in health-related #EduTok videosDocument15 pages【emotional appeal核心】Mental health messages on TikTok Analysing the use of emotional appeals in health-related #EduTok videosCHEN YIMINGNo ratings yet
- Sexual Identity and Gender IdentityDocument5 pagesSexual Identity and Gender IdentityDiego JoaquínNo ratings yet
- 30Document9 pages30Philip MercadoNo ratings yet
- Research PaperDocument49 pagesResearch Paperamna.irf08No ratings yet
- Mental Health Advocacy Presentation ExpandedDocument15 pagesMental Health Advocacy Presentation ExpandedjaredooofNo ratings yet
- 2 MMPI-2 Validity-Scales Final PDFDocument9 pages2 MMPI-2 Validity-Scales Final PDFHanifa Bi BaritoNo ratings yet
- From Dysthymia To Treatment-Resistant Depression: Evolution of A Psychopathological ConstructDocument7 pagesFrom Dysthymia To Treatment-Resistant Depression: Evolution of A Psychopathological ConstructApenasNo ratings yet