0 ratings0% found this document useful (0 votes)
100 viewsCase Study NCM 118
Case Study NCM 118
Uploaded by
Romzy BasañesThis document provides information on emergency medications used to treat cardiac disorders. It discusses the actions, indications, dosages, and nursing considerations for lidocaine, magnesium sulfate, nitroglycerine, and amiodarone. Lidocaine is used to treat ventricular fibrillation and tachycardia. Magnesium sulfate corrects magnesium deficiencies and treats hypomagnesemia. Nitroglycerine provides acute relief of angina by relaxing blood vessels. Amiodarone is a class III antiarrhythmic that works by blocking potassium channels to treat arrhythmias. Close monitoring of patients is important when administering these cardiac medications.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Case Study NCM 118
Case Study NCM 118
Uploaded by
Romzy Basañes0 ratings0% found this document useful (0 votes)
100 views14 pagesThis document provides information on emergency medications used to treat cardiac disorders. It discusses the actions, indications, dosages, and nursing considerations for lidocaine, magnesium sulfate, nitroglycerine, and amiodarone. Lidocaine is used to treat ventricular fibrillation and tachycardia. Magnesium sulfate corrects magnesium deficiencies and treats hypomagnesemia. Nitroglycerine provides acute relief of angina by relaxing blood vessels. Amiodarone is a class III antiarrhythmic that works by blocking potassium channels to treat arrhythmias. Close monitoring of patients is important when administering these cardiac medications.
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
This document provides information on emergency medications used to treat cardiac disorders. It discusses the actions, indications, dosages, and nursing considerations for lidocaine, magnesium sulfate, nitroglycerine, and amiodarone. Lidocaine is used to treat ventricular fibrillation and tachycardia. Magnesium sulfate corrects magnesium deficiencies and treats hypomagnesemia. Nitroglycerine provides acute relief of angina by relaxing blood vessels. Amiodarone is a class III antiarrhythmic that works by blocking potassium channels to treat arrhythmias. Close monitoring of patients is important when administering these cardiac medications.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
100 views14 pagesCase Study NCM 118
Case Study NCM 118
Uploaded by
Romzy BasañesThis document provides information on emergency medications used to treat cardiac disorders. It discusses the actions, indications, dosages, and nursing considerations for lidocaine, magnesium sulfate, nitroglycerine, and amiodarone. Lidocaine is used to treat ventricular fibrillation and tachycardia. Magnesium sulfate corrects magnesium deficiencies and treats hypomagnesemia. Nitroglycerine provides acute relief of angina by relaxing blood vessels. Amiodarone is a class III antiarrhythmic that works by blocking potassium channels to treat arrhythmias. Close monitoring of patients is important when administering these cardiac medications.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 14
Emergency Medications for Cardiac Disorders
As presented by: Chery Lynn Arzaga & Romulo Basañes II
Client Background/History
Patient is a 30y/0 known case of epilepsy presented with
generalized tonic clonic seizures and got intubated in the emergency
department secondary to low GCS. Initially he was managed in line
with status epilepticus and kept on 4 antiepileptic drugs but EEG was
unremarkable. Later on found to have OTCs prolongation on digging
history, the patient’s family revealed use of loperamide tablets around
100-200 tablets per day. During stay he had recurrent VT and Vfib for
which a temporary pacemaker was applied and got reverted back.
Lidocaine
ACTION: Combines with fast sodium channels in myocardial cell membranes, which inhibits
sodium influx into cells and decreases ventricular depolarization, as well as automaticity and
excitability during diastole. Lidocaine also blocks nerve impulses by decreasing the
permeability of neuronal membranes to sodium, which produces local anesthesia.
INDICATION: To treat ventricular fibrillation or ventricular tachycardia
DOSAGE AND FORMS: Loading: 50 to 100 mg (or 1 to 1.5 mg/kg), given at 25 to 50 mg/min.
If desired response isn’t achieved after 5 to 10 min, second dose of 25 to 50 mg (or 0.5 to 0.75
mg/kg) given every 5 to 10 min until maximum loading dose (300 mg in 1 hr) has been given.
CONTRAINDICATIONS: Adams–Stokes syndrome; hypersensitivity to lidocaine, amide
anesthetics, or their components; severe heart block (without artificial pacemaker); Wolff–
Parkinson– White syndrome
Cont.
SPECIAL PRECAUTIONS:
Use caution when administering lidocaine to patients with compromised myocardial function
because of risk of electrolyte disturbances or fluid overload.
ADVERSE REACTIONS: CNS: Anxiety; apprehension; confusion; difficulty speaking;
dizziness; drowsiness; euphoria; hallucinations; lethargy; lightheadedness; malignant
hyperthermia; paresthesia; seizures; sensation of cold, heat, or numbness; tremors; twitching;
unconsciousness CV: Bradycardia, cardiac arrest, hypotension, new or worsening arrhythmias
EENT: Blurred vision, diplopia, tinnitus GI: Nausea, vomiting HEME: Methemoglobinemia
MS: Muscle weakness, myalgia RESP: Respiratory arrest or depression Other: Anaphylaxis,
other less severe hypersensitivity reactions; injection-site burning, irritation, petechiae, redness,
stinging, swelling, and tenderness; worsened pain
Cont.
NURSING CONSIDERATIONS:
Observe for respiratory depression after bolus injection and during I.V. infusion of lidocaine.
Keep life-support equipment and vasopressors nearby during I.V. use in case of respiratory depression or other
reactions.
Carefully check prefilled syringes before using. Use only syringes labeled “for cardiac arrhythmias” for I.V.
administration.
As ordered, titrate I.V. dose to minimum amount needed to prevent arrhythmias. If administration is controlled by a
pumping device, stop pump before container runs dry because an air embolism may result. Change intravenous
administration apparatus at least once every 24 hours.
During I.V. administration, place patient on cardiac monitor, as ordered, and closely observe her at all times. Monitor
for prolonged PR interval, widening QRS complex, or worsening arrhythmias— possible signs of drug toxicity. If
present, notify prescriber and expect to discontinue lidocaine therapy immediately. Although infrequent, also
monitor her for hypersensitivity reactions that can be as severe as anaphylaxis following lidocaine administration. If
anaphylaxis occurs, discontinue drug, notify prescriber, and provide supportive care.
If signs of toxicity, such as dizziness, occur, notify prescriber and expect to discontinue or slow infusion.
Monitor vital signs as well as BUN and serum creatinine and electrolyte levels during and after therapy.
Magnesium Sulfate
• ACTION: Assists all enzymes involved in phosphate transfer reactions that use adenosine triphosphate
(ATP). Magnesium is required for normal function of the ATP-dependent sodium–potassium pump in
muscle membranes. It may effectively treat digitalis glycoside–induced arrhythmias because correction of
hypomagnesemia improves the sodium–potassium pump’s ability to distribute potassium into intracellular
spaces and because magnesium decreases calcium uptake and potassium outflow through myocardial cell
membranes
• INDICATION: To correct magnesium deficiency and to treat severe hypomagnesemia
• DOSAGE AND FORMS: 5 g diluted in 1 L I.V. solution and infused over 3 hr.
• CONTRAINDICATIONS: Hypersensitivity to magnesium salts or any component of magnesium-
containing preparations For magnesium chloride: Coma, heart disease, renal impairment For magnesium
sulfate: Heart block, MI, preeclampsia 2 hours or less before delivery (I.V. form) For use as laxative: Acute
abdominal problem (as indicated by abdominal pain, nausea, or vomiting), diverticulitis, fecal impaction,
intestinal obstruction or perforation, colostomy or ileostomy, severe renal impairment, ulcerative colitis
Cont.
SPECIAL PRECAUTIONS:
warning Observe for and report early evidence of hypermagnesemia: bradycardia, depressed
deep tendon reflexes, diplopia, dyspnea, flushing, hypotension, nausea, slurred speech,
vomiting, and weakness.
warning Be aware that magnesium may precipitate myasthenic crisis by decreasing patient’s
sensitivity to acetylcholine.
ADVERSE REACTIONS: CNS: Confusion, decreased reflexes, dizziness, syncope CV:
Arrhythmias, hypotension GI: Flatulence, vomiting MS: Muscle cramps RESP: Dyspnea,
respiratory depression or paralysis SKIN: Diaphoresis Other: Allergic reaction,
hypermagnesemia, injection-site pain or irritation (I.M. form), laxative dependence, magnesium
toxicity.
Cont.
NURSING CONSIDERATIONS:
Always consider the 5 rights: right patient, right drugs, right dose, right time and right route
Frequently assess cardiac status of patient taking drugs that lower heart rate, such as beta
blockers, because magnesium may aggravate symptoms of heart block.
Monitor serum electrolyte levels in patients with renal insufficiency because they’re at risk for
magnesium toxicity.
Monitor v/s
Nitroglycerine
Action:Nitroglycerin is converted by mitochondrial aldehyde dehydrogenase (mtALDH) to nitric oxide
(NO), an active substance which then activates the enzyme guanylate cyclase.The activation of this
enzyme is followed by the synthesis of cyclic guanosine 3',5'-monophosphate (cGMP), activating a
cascade of protein kinase-dependent phosphorylation events in smooth muscles. This process eventually
leads to the dephosphorylation of the myosin light chain of smooth muscles, causing relaxation and
increased blood flow in veins, arteries and cardiac tissue.. The above processes lead to decreased work of
the heart decreased blood pressure, relief of anginal symptoms, and increased blood flow to the
myocardium.
Indications: indicated for the acute relief of an attack or acute prophylaxis of angina pectoris due to
coronary artery disease.
Dosage and Forms: Sublingual. Administer one tablet under the tongue or in the buccal pouch at the first
sign of an acute anginal attack. Allow tablet to dissolve without swallowing. One additional tablet may
be administered every 5 minutes until relief is obtained. No more than three tablets are recommended
within a 15-minute period.
Cont.
Contraindications: Known history of increased intracranial pressure, severe anemia, right-
sided myocardial infarction, or hypersensitivity to nitroglycerin are contraindications to
nitroglycerin therapy.
Special Precautions:
i. Excessive use may lead to the development of tolerance. Only the smallest dose required for
effective relief of the acute angina attack should be used.
ii. Severe hypotension, particularly with upright posture, may occur with small doses of
nitroglycerin particularly in patients with constrictive pericarditis, aortic or mitral stenosis,
patients who may be volume-depleted, or are already hypotensive
iii. Nitroglycerin produces dose-related headaches, especially at the start of nitroglycerin therapy,
which may be severe and persist but usually subside with continued use.
Cont.
Adverse Reactions: severe or throbbing headaches, pounding heartbeats,
fluttering in your chest, slow heart rate, lightheadedness, blurred vision, dry
mouth, chest pain or pressure, pain spreading to your jaw or shoulder, nausea,
and sweating
Nursing Considerations:
i. Check blood pressure and pulse before each administration of NTG–blood
pressure can drop precipitously after a single dose. Hold dose if systolic BP <
90 mm Hg or more than 30 mm Hg below baseline.
ii. NTG is highly unstable and should be stored in light resistant container in cool
environment
Amiodarone
Action: Amiodarone is primarily a class III antiarrhythmic. Like other antiarrhythmic drugs of this class,
amiodarone works primarily by blocking potassium rectifier currents responsible for the repolarization of
the heart during phase 3 of the cardiac action potential. This potassium channel-blocking effect results in
increased action potential duration and a prolonged effective refractory period in cardiac myocytes.
Myocyte excitability is decreased, preventing reentry mechanisms and ectopic foci from perpetuating
tachyarrhythmias.
Indications: commonly used off-label to treat supraventricular tachyarrhythmias such as atrial fibrillation
as well as for the prevention of ventricular tachyarrhythmias (VTs) in high-risk patients.
Dosage and forms: Injectable solution. 50mg/ml, 150mg/100ml, 360mg/200ml
Contraindications:
i. Hypersensitivity
ii. Severe sinus node dysfunction, 2°/3° AV block or bradycardia causing syncope (except with functioning
artificial pacemaker), cardiogenic shock
iii. Avoid during breastfeeding
Cont.
Special Precautions:
i. Indicated only for life-threatening arrhythmias because of risk for substantial toxicity; poses
major management problems that could be life-threatening in patients at risk of sudden death;
therefore, make every effort to utilize alternative agents first
ii. amiodarone may remain in your body for several months after you stop taking it. You may
continue to experience side effects of amiodarone during this time. Be sure to tell every
health care provider who treats you or prescribes any medication for you during this time that
you have recently stopped taking amiodarone.
Adverse Reactions: constipation loss of appetite headache, decreased sex drive, difficulty
falling asleep or staying asleep, flushing, changes in ability to taste and smell, changes in
amount of saliva
Cont.
Nursing Responsibilities:
i. Monitor blood pressure and apical pulse prior to administration.
ii. Cardiac monitor should be used on patients receiving amiodarone therapy.
iii. Baseline assessments should be checked of liver function and thyroid function.
iv. Monitor serum level frequently.
You might also like
- Charli NowakDocument4 pagesCharli NowakSteven Sun100% (1)
- Case Presentation Pleural EffusionDocument30 pagesCase Presentation Pleural EffusionSarita100% (5)
- RespiDocument9 pagesRespiMary Roan RonatoNo ratings yet
- Severe Anxiety As Evidenced by Repetitive ActionDocument1 pageSevere Anxiety As Evidenced by Repetitive ActionRomzy Basañes100% (3)
- Nursing Care Plan: General: Goals Met GenreralDocument3 pagesNursing Care Plan: General: Goals Met GenreralRomzy Basañes0% (1)
- Funda Saved Ms2003Document103 pagesFunda Saved Ms2003June DumdumayaNo ratings yet
- NLE Reviewers: Leadership Management Research and Ethics (LMRE)Document7 pagesNLE Reviewers: Leadership Management Research and Ethics (LMRE)Lot RositNo ratings yet
- NLE Ques and Ratio 2Document12 pagesNLE Ques and Ratio 2cesspintas CuaresmaNo ratings yet
- NVS Written ReportDocument20 pagesNVS Written ReportbabiNo ratings yet
- PALMER (NLM) Enhancement Notes Nov 2020Document21 pagesPALMER (NLM) Enhancement Notes Nov 2020Basema HashhashNo ratings yet
- Iv Fluid Sheet: Bautista A 58 2021-0000025 Milagros F Medical Ward-207Document1 pageIv Fluid Sheet: Bautista A 58 2021-0000025 Milagros F Medical Ward-207Renea Joy ArruejoNo ratings yet
- 00 PsychDocument11 pages00 PsychAngel LuayonNo ratings yet
- CHN Day 2 V GasminDocument13 pagesCHN Day 2 V Gasminadelaidah sanggacalaNo ratings yet
- College of Nursing: Xavier University Ateneo de CagayanDocument7 pagesCollege of Nursing: Xavier University Ateneo de CagayanShamsa AfdalNo ratings yet
- Gastrointestinal System Disorders NCLEX Practice - Quiz #2 - 50 Questions - NurseslabsDocument52 pagesGastrointestinal System Disorders NCLEX Practice - Quiz #2 - 50 Questions - NurseslabsGypsy Joan Trance100% (1)
- NCM 103 Fe 1ST QuizDocument4 pagesNCM 103 Fe 1ST QuizScytllaNo ratings yet
- NCM 103 MIdtermDocument3 pagesNCM 103 MIdtermmesdejen100% (1)
- Pulmonary AngiographyDocument3 pagesPulmonary AngiographyBiway RegalaNo ratings yet
- Pharmacology ReviewerDocument15 pagesPharmacology ReviewerKathrynne MendozaNo ratings yet
- P1 P2 Mastery Examination Reviewer in FNP LECTUREDocument34 pagesP1 P2 Mastery Examination Reviewer in FNP LECTUREMary Ann G. CorsanesNo ratings yet
- CIP-NCM-121-Disaster Nursing-TuesdaysDocument3 pagesCIP-NCM-121-Disaster Nursing-TuesdaysKhen QuiringNo ratings yet
- NCM 117 Passed FinalsDocument45 pagesNCM 117 Passed FinalsKrizyl Joy D. MabansagNo ratings yet
- 3 Post Test PediaDocument4 pages3 Post Test PediaJanine BaticbaticNo ratings yet
- NCMA 217 - Newborn Assessment Ma'am JhalDocument5 pagesNCMA 217 - Newborn Assessment Ma'am JhalMariah Blez BognotNo ratings yet
- Practice Questions - Digestive and Gastrointestinal Treatment ModalitiesDocument22 pagesPractice Questions - Digestive and Gastrointestinal Treatment ModalitiesIan GarifeNo ratings yet
- Chapter 44-Activity and ExerciseDocument4 pagesChapter 44-Activity and ExerciseollietonkNo ratings yet
- June 2006 Examination ControversyDocument5 pagesJune 2006 Examination ControversyJoyce AlbaladejoNo ratings yet
- Preboard Nov 2023 Np5 StudentDocument9 pagesPreboard Nov 2023 Np5 Studentyzak jouleNo ratings yet
- NCM 118 RLE Case Analysis No.2Document4 pagesNCM 118 RLE Case Analysis No.2Reyna Mee AhiyasNo ratings yet
- Checklists For Return DemonstrationDocument8 pagesChecklists For Return DemonstrationLei Anne ZapantaNo ratings yet
- Nle Review 1Document39 pagesNle Review 1Ma.Josephine AlfajoraNo ratings yet
- Module 3 Responsibilities of A Beginning Nurse ResearcherDocument9 pagesModule 3 Responsibilities of A Beginning Nurse ResearcherCaitlynNo ratings yet
- Nursing Care Plan - MergedDocument13 pagesNursing Care Plan - MergedJuls Flares SycaycoNo ratings yet
- NP 3 Bon Set ADocument38 pagesNP 3 Bon Set AGo IdeasNo ratings yet
- Neuro Hand Out Intensive Nov Pnle 2022Document12 pagesNeuro Hand Out Intensive Nov Pnle 2022Kristine BillonesNo ratings yet
- NCM117Document20 pagesNCM117Marie Isabelle HerveraNo ratings yet
- Grand Coaching: Medical Surgical NursingDocument22 pagesGrand Coaching: Medical Surgical NursingEsarpy (Nana)No ratings yet
- LM Intensive ReviewerDocument10 pagesLM Intensive ReviewerAllysa PrestonNo ratings yet
- NCM 103.1 FINAL - OkDocument99 pagesNCM 103.1 FINAL - OkElizalde HusbandNo ratings yet
- New PRC Exhibit FormDocument6 pagesNew PRC Exhibit FormPixel DinibitNo ratings yet
- Professional AdjustmentDocument3 pagesProfessional Adjustmentkamae_27No ratings yet
- Cellular Aberrations NotesDocument22 pagesCellular Aberrations NotesH50% (2)
- NCM 118 CARDIO LECTURE LIFE THREATENING EMERGENCY CONGESTIVE HEART FAILURE MVIMMACULATA 2021 For Canvas-1Document46 pagesNCM 118 CARDIO LECTURE LIFE THREATENING EMERGENCY CONGESTIVE HEART FAILURE MVIMMACULATA 2021 For Canvas-1Pollen Siega BunalNo ratings yet
- Maternity Edited2Document7 pagesMaternity Edited2male nurse0% (1)
- Prof Ad ch1-3Document3 pagesProf Ad ch1-3Daisy Ann IñigoNo ratings yet
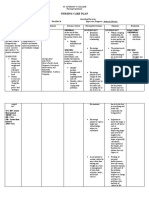
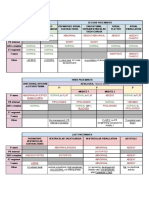
- Nursing Care Plan: NCM 109 Rle Clinical Wednesday 7:00 AM - 12:00 PMDocument10 pagesNursing Care Plan: NCM 109 Rle Clinical Wednesday 7:00 AM - 12:00 PMBiway RegalaNo ratings yet
- Medical Surgical Nursing: By: Mr. Emerson AliswagDocument137 pagesMedical Surgical Nursing: By: Mr. Emerson AliswagMarie JhoanaNo ratings yet
- Competency Appraisal QuestionaireDocument7 pagesCompetency Appraisal QuestionairePaolo AtienzaNo ratings yet
- MCN Doc PacabisDocument18 pagesMCN Doc PacabisSJane FeriaNo ratings yet
- Prof TestDocument12 pagesProf TestOlive NNo ratings yet
- ACLSDocument78 pagesACLSKajalNo ratings yet
- TP4Document14 pagesTP4Asdfghjl0% (1)
- Code of Ethics For NursesDocument2 pagesCode of Ethics For NursesAthena BendoNo ratings yet
- Psych Meds Booster Nov 2022 PnleDocument11 pagesPsych Meds Booster Nov 2022 PnleDarwin DerracoNo ratings yet
- Neuro Vital Signs Assessment Procedure and ChecklistDocument9 pagesNeuro Vital Signs Assessment Procedure and ChecklistJustine BayabosNo ratings yet
- Nursing Informatics: Bachelor of Science in NursingDocument4 pagesNursing Informatics: Bachelor of Science in NursingMichelle MallareNo ratings yet
- Funda (Course Audit)Document16 pagesFunda (Course Audit)Kath-Kath Cubillan RanayNo ratings yet
- Pharmacology Nursing 50items QuestionnaireDocument15 pagesPharmacology Nursing 50items QuestionnaireJens EspinaNo ratings yet
- NCM 118 RleDocument10 pagesNCM 118 RleJamaica Leslie NovenoNo ratings yet
- The Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeFrom EverandThe Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeRating: 4.5 out of 5 stars4.5/5 (2)
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- Ventricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandVentricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Drug Study CARDIODocument17 pagesDrug Study CARDIODiannetotz Morales100% (1)
- Drug StudyDocument6 pagesDrug StudyMaurence John Feliciano LuluquisenNo ratings yet
- Nursing Care Plan: Subjective: "I Drink Alcohol and General: Independent: Independent: Goals Met GenreralDocument3 pagesNursing Care Plan: Subjective: "I Drink Alcohol and General: Independent: Independent: Goals Met GenreralRomzy BasañesNo ratings yet
- Nursing Care Plan: General: Goals Met GenreralDocument4 pagesNursing Care Plan: General: Goals Met GenreralRomzy Basañes100% (2)
- Pathophysio - Group 3 Gender DysphoriaDocument4 pagesPathophysio - Group 3 Gender DysphoriaRomzy BasañesNo ratings yet
- Reflection Paper ADHDDocument1 pageReflection Paper ADHDRomzy BasañesNo ratings yet
- Week 1 RizalDocument2 pagesWeek 1 RizalRomzy BasañesNo ratings yet
- LeadershipDocument1 pageLeadershipRomzy BasañesNo ratings yet
- Movie Reflection Rain ManDocument1 pageMovie Reflection Rain ManRomzy Basañes100% (1)
- The Devil Wears Prada by Lauren Weisberger Is Classified As A Chick Lit Genre ofDocument3 pagesThe Devil Wears Prada by Lauren Weisberger Is Classified As A Chick Lit Genre ofRomzy BasañesNo ratings yet
- Hermeneutical PhenomenologyDocument12 pagesHermeneutical PhenomenologyRomzy Basañes50% (2)
- XXXX - Key AnswersDocument5 pagesXXXX - Key AnswersPedro GenosasNo ratings yet
- Answer All MCQ Questions From No. 1 To 50. Each Question Will Carry 2 MarksDocument4 pagesAnswer All MCQ Questions From No. 1 To 50. Each Question Will Carry 2 MarksRick Das100% (1)
- SurgeyDocument37 pagesSurgeyDr Anais AsimNo ratings yet
- Hypertension JournalDocument8 pagesHypertension JournalCarrie Joy DecalanNo ratings yet
- Lab ValuesDocument1 pageLab ValuesJohn Matthew GasmenNo ratings yet
- NCM 3114 Acid Base Imbalance-2Document13 pagesNCM 3114 Acid Base Imbalance-2Fayeh Harah PadrillanNo ratings yet
- Cardiac Drugs Questions Part IDocument110 pagesCardiac Drugs Questions Part ISanaz Niksefat100% (2)
- NCM 118 MIDTERMS PG 7Document1 pageNCM 118 MIDTERMS PG 7Kai SamaNo ratings yet
- UNIT 2 PART 2 2022-2023 - Cell Adaptation, Injury, DeathDocument108 pagesUNIT 2 PART 2 2022-2023 - Cell Adaptation, Injury, Deathdocfetus237No ratings yet
- Atrial MyxomaDocument36 pagesAtrial MyxomaPrince Jevon YapNo ratings yet
- Australian Adult Pre Exercise Screening TextbookDocument58 pagesAustralian Adult Pre Exercise Screening Textbookcarlos corteNo ratings yet
- Guidelines Aca HolterDocument39 pagesGuidelines Aca HolterMiguel PeixotoNo ratings yet
- Power of Vitamin D - A Vitamin D - Zaidi MD, SarfrazDocument179 pagesPower of Vitamin D - A Vitamin D - Zaidi MD, SarfrazElena DutuNo ratings yet
- BioDocument4 pagesBioMustofa KamalNo ratings yet
- 01 ICG Brochure ICG 20160513 SDocument2 pages01 ICG Brochure ICG 20160513 SFrancisco QuimbayoNo ratings yet
- ACLS Bradycardia AlgorithmDocument1 pageACLS Bradycardia AlgorithmLady MuffinsNo ratings yet
- Dissertation Cardiovascular DiseaseDocument6 pagesDissertation Cardiovascular DiseaseBuyCollegePaperCanada100% (1)
- CARDIOVASDocument18 pagesCARDIOVASVikash KushwahaNo ratings yet
- Pharmacology Samplex (1 Bimonthly) : 1 QuizDocument15 pagesPharmacology Samplex (1 Bimonthly) : 1 QuizCindy Mae MacamayNo ratings yet
- Captură de Ecran Din 2024-04-30 La 11.39.18Document12 pagesCaptură de Ecran Din 2024-04-30 La 11.39.18faurflaviuionutNo ratings yet
- AmlodipineDocument22 pagesAmlodipineBetaNo ratings yet
- Fetal CirculationDocument16 pagesFetal CirculationDR RESHMA AJAYNo ratings yet
- Abdalla (Letter Structure)Document3 pagesAbdalla (Letter Structure)healthpartnersmedicalserviceNo ratings yet
- Sacubitril - Valsartan - WikipediaDocument28 pagesSacubitril - Valsartan - WikipediaSUBHADIPNo ratings yet
- Medical Studies Support MDs Prescribing Hydroxychloroquine For Early Stage COVID 6th EditionDocument247 pagesMedical Studies Support MDs Prescribing Hydroxychloroquine For Early Stage COVID 6th Editionwizard1111iamNo ratings yet
- What Is A Coronary Angiogram?: HeartDocument2 pagesWhat Is A Coronary Angiogram?: HeartSebastian BujorNo ratings yet
- Physical AssessmentDocument51 pagesPhysical AssessmentJasmin Jacob100% (2)
- Topical Hemostatic Agents in Neurosurgery 2011Document35 pagesTopical Hemostatic Agents in Neurosurgery 2011Ardhynata SetiawanNo ratings yet