0 ratings0% found this document useful (0 votes)
33 viewsHDP 301: Lecture #2: Immune Pathology Pain
HDP 301: Lecture #2: Immune Pathology Pain
Uploaded by
Linda NguyenThis document provides an overview of the immune system and immune pathology. It discusses the structures of the immune system, including white blood cells that mediate inflammation and immunity. It describes the innate and adaptive immune responses. It also covers dendritic cells, inflammation, the process of inflammation including increased vascular permeability and recruitment of leukocytes, and phagocytosis. Finally, it discusses alterations in immune function including excessive responses like autoimmunity and hypersensitivity reactions.
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
HDP 301: Lecture #2: Immune Pathology Pain
HDP 301: Lecture #2: Immune Pathology Pain
Uploaded by
Linda Nguyen0 ratings0% found this document useful (0 votes)
33 views51 pagesThis document provides an overview of the immune system and immune pathology. It discusses the structures of the immune system, including white blood cells that mediate inflammation and immunity. It describes the innate and adaptive immune responses. It also covers dendritic cells, inflammation, the process of inflammation including increased vascular permeability and recruitment of leukocytes, and phagocytosis. Finally, it discusses alterations in immune function including excessive responses like autoimmunity and hypersensitivity reactions.
Original Title
Untitled
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
This document provides an overview of the immune system and immune pathology. It discusses the structures of the immune system, including white blood cells that mediate inflammation and immunity. It describes the innate and adaptive immune responses. It also covers dendritic cells, inflammation, the process of inflammation including increased vascular permeability and recruitment of leukocytes, and phagocytosis. Finally, it discusses alterations in immune function including excessive responses like autoimmunity and hypersensitivity reactions.
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
0 ratings0% found this document useful (0 votes)
33 views51 pagesHDP 301: Lecture #2: Immune Pathology Pain
HDP 301: Lecture #2: Immune Pathology Pain
Uploaded by
Linda NguyenThis document provides an overview of the immune system and immune pathology. It discusses the structures of the immune system, including white blood cells that mediate inflammation and immunity. It describes the innate and adaptive immune responses. It also covers dendritic cells, inflammation, the process of inflammation including increased vascular permeability and recruitment of leukocytes, and phagocytosis. Finally, it discusses alterations in immune function including excessive responses like autoimmunity and hypersensitivity reactions.
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
Download as ppt, pdf, or txt
You are on page 1of 51
HDP 301: Lecture #2
*Immune Pathology
*Pain
Jeanine Harrison BScN MN NP
Seneca College
Pathophysiology HDP 301
Immune System
Recall the structures of the immune system:
1. Skin and mucous membranes
2. Monocytes and macrophages
3. Lymphoid system (spleen, thymus gland,
lymph nodes)
4. Bone marrow
*WBCs (leukocytes) mediate inflammation and
immunity.
WBCs are attracted to pathogens and foreign
molecules, then activated to neutralize or
destroy them
Immune System continued
The immune system is usually categorized into two
defense types:
1. Innate – no previous exposure to pathogen/antigen;
natural killer (NK) cells and phagocytic cells
(neutrophils and macrophages) are able to respond
to infection by a variety of antigens
2. Specific – more effective on 2nd exposure to an
antigen; recognize specific antigens; B cells and T
cells responsible for this type of immunity
Review these defense systems and immune system
structure using your text book
Dendritic Cells (DC)
DCs are phagocytes found all over the body
but especially in the skin and mucous
membranes. They “recognize” non-self cells
with their pattern recognition receptors
(PRRs) and become antigen-presenting cells
(APCs) when they display new markers on
their cell membranes for presentation to
Helper T cells in lymph nodes to link the
innate immune system with the adaptive
one.
Inflammation
Inflammation occurs when cells are injured
no matter the cause; protective mechanism
and begins healing process
Purpose of Inflammation:
1. To neutralize/destroy harmful invading
agents
2. To limit the spread of harmful agents to
other organs
3. To prepare damaged tissue for repair
Signs of Inflammation
1. Redness
2. Swelling
3. Heat
4. Pain
5. Loss of function
“-itis” is used to describe inflammation ex.
Tendonitis, appendicitis etc.
*Infection is usually accompanied by
inflammation; but inflammation is not always
caused by infection
Inflammation
Inflammation can be caused by exogenous
sources (surgery, trauma, burns etc) or
endogenous sources (ex. tissue ischemia
from MI)
Acute inflammation is short in duration, lasts
<2 weeks; chronic inflammation is usually
widespread, lasts longer and can result in
scar tissue and/or deformity
Process of Inflammation
Regardless of the cause, the inflammatory
response includes the same events:
1. Increased vascular permeability
2. Recruitment and emigration of leukocytes
3. Phagocytosis of antigens and debris
*Note, immediately after an injury, precapillary
arterioles around the injury vasoconstrict
briefly (possible mechanism to reduce blood
loss)
Inflammation
1. Increased Vascular Permeability
Vasodilation is caused by the release of
chemical mediators (histamine,
prostaglandins, bradykinin and leukotrienes)
from mast cells at the injured area.
These chemicals cause vasodilation more
blood flow to the area increased hydrostatic
pressure increased capillary permeability
More fluid is pushed out of blood vessels into
surrounding tissues local swelling
The increased build-up of blood and fluid in the
injured area contributes to the redness, pain,
heat and swelling
1. Increased Vascular Permeability
Histamine is a strong
vasodilator – if released in
high amounts significant
reductions in BP
Prostaglandins and
leukotrienes contribute to
vasodilation, increased
permeability and pain by
enhancing the sensitivity of
pain receptors
The fluid that accumulates
during inflammation is called
“exudate”
1. Increased Vascular Permeability
In the early phases of inflammation, platelets
move into the site and release fibronectin to
form a meshwork/net/trap, as well as
stimulating clotting to help reduce bleeding
Platelets release growth factor to stimulate
cell proliferation
Blood begins to coagulate and development
of fibrin clot occurs (usually within minutes)
Fibrin also develops in lymph vessels to “wall
off” the area of injury (reduces spread of
toxins)
2. Emigration of Leukocytes
As blood travels to the injured area, neutrophils stick
to receptors called selectins along the injured
capillary wall
Another group of receptors called integrins help
neutrophils stick and roll along the capillary
endothelial surface
Chemokines are molecules that enhance the
binding affinity of integrins so that neutrophils can
attach firmly to vessel walls
Once a neutrophil arrives at the area of injury, it can
squeeze through the spaces between endothelial
cells and “emigrate” to the inflamed tissue. This
process is called diapedesis (di- a –pe – dee –sis).
Emigration
2. Emigration
Chemotaxis – the process by which
neutrophils are attracted to inflamed tissue
Neutrophils are guided to damaged tissue by
chemicals (bacterial toxins, degenerative
products etc.)
Neutrophils immediately begin phagocytosis
and production of collagenase to break down
dead tissue
Monocytes, eosinophils and NK cells also
arrive at the area to contribute to
inflammation and to destroy infected tissues.
Diapedesis
Image from: Gordon, Joe Lecture Notes
3. Phagocytosis
Neutrophils and monocytes (macrophages) begin the
process of phagocytosis at the injured tissue
Both cells produce enzymes that digest proteins;
lysozymes, neutral proteases, collagenase, elastase,
and acid hydrolases.
Once a neutrophil leaves blood circulation to fight an
infection, it will eventually stop working and die at the
site
Pus may form at the injury site – a collection of dead
neutrophils, bacteria, and cellular debris
Macrophages last longer than neutrophils and thus
have the role of removing old neutrophils and preparing
the site for healing
Acute Inflammation
Acute inflammation can cause tissue
damage; degradative enzymes and oxidative
agents can attack local tissues
Inflammatory inactivators called “α-
antiprotease” inhibit the destructive proteases
released from activated neutrophils
They are made in the liver and circulate
continuously in the bloodstream
Individuals with antiprotease deficiencies are
at risk for inflammatory tissue destruction
Immune Response
Alterations in Immune Function
Remember: the purpose of the immune
system is to defend the body against
invasion or infection by foreign substances
called antigens
Immune disorders are divided into 2
categories:
1. Excessive Immune Response (autoimmune
and hypersensitivity)
2. Deficient Immune Response
Excessive Immune Responses
Immune system is hyperfunctioning
Autoimmunity- immune system attacks its own tissue;
recognizes a persons’ own cells as foreign and
mounts an immune response that injures self tissues
Causes are largely unknown
Hypersensitivity - normal immune response that is
inappropriately triggered/excessive/produces
undesirable effects on the body
Many autoimmune reactions toward self-tissues are
mediated through hypersensitivity mechanisms;
therefore, many autoimmune diseases are also
considered hypersensitivity reactions.
Treatments for autoimmunity
Immunosuppressive therapy is most often used
individualized depending on disease
expression
Corticosteroids and cytotoxins inhibit excessive
immune responses, but also limit the positive
and protective functions of the immune system
Corticosteroids decrease the number of
lymphocytes and alter their function; also
decrease antibody formation
Cytotoxins, such as methotrexate, kill actively
proliferating lymphocytes (reduces the number
of white blood cells)
Hypersensitivity
There are 4 types of hypersensitivity:
1. Type I – immediate allergic or anaphylactic
reaction; mediated by mast cells
vasodilation, increased vascular
permeability, hypotension,
bronchoconstriction, hives, increased
mucus secretion, itching (pruritis)
-usually occurs 15-30mins after exposure to
antigen/allergen
Type I
Examples are seasonal allergic rhinitis,
eczema, bee stings, peanut allergic
reactions, food allergies
Treatments – antihistamines, Epinephrine
(beta-adrenergic) to reduce bronchospasm
and bronchoconstriction, corticosteroids to
decrease inflammation, anticholinergics allow
bronchodilation
Hypersensitivity
2. Type II – tissue-specific, antibodies that
attack antigens on the surface of specific
cells; immediate reaction within 15-30mins
after exposure
-an example is a blood transfusion reaction
person with blood type A receives blood
type B antibodies will attack and destroy
large numbers of red blood cells
-fever, chills, flushing, tachycardia,
hypotension, nausea, anxiety, and can
progress to anaphylaxis, shock and death.
Hypersensitivity
3. Type III – immune complex reaction; failure
of the immune and phagocytic systems to
effectively remove antigen-antibody immune
complexes from tissues long-lasting and
ongoing inflammatory reaction
-caused by persistent low-grade infections or
autoimmune production of antibodies
(production of antibodies against red blood
cells for example)
Hypersensitivity
4. Type IV – delayed hypersensitivity, T-cells
react with altered or foreign cells and initiate
inflammation; no antibody involvement
Reaction is slow to develop, beginning 24
hours after exposure and lasting up to 14
days
Most common: contact hypersensitivity;
immune or inflammatory response to
chemicals, ointments, clothing, cosmetics,
dyes and adhesives
Deficient Immune Responses
Result from a functional decrease in one or more
components of the immune system
Two types:
1. Primary Immunodeficiency Disorders (PID) –
congenital (abnormal development or maturation of
immune cells) or acquired such as HIV/AIDS;
directly affect immune cell function
2. Secondary Immunodeficiency Disorders – caused
by non-immune system disorders/treatments such
as poor nutrition, stress or drugs, that secondarily
suppress immune function
UNDERSTANDING
PAIN
Pain
Pain is difficult to define and
assess because it is largely
a subjective experience
Physiological mechanisms
involved in pain are called
nociception.
(no-sis-cep- tion)
4 stages of nociception:
1. Transduction
2. Transmission
3. Perception
4. Modulation
Nociception: Transduction
Transduction is the process of converting
painful stimuli to neuronal action potentials at
the sensory receptor.
Pain receptors, nociceptors, in the periphery
are stimulated by noxious stimuli
Nociceptors are found in the skin, muscle,
connective tissue, circulatory system and in
abdominal, pelvic and thoracic organs
Nociceptors convert negative stimuli into action
potentials that progress to the spinal cord and
brain
Transduction
Nociceptors can be stimulated by damage to
nerve endings, or by the release of chemicals
at the injury site
Chemicals can be released as a result of
injury or inflammatory response; pain
chemicals include K+, H+, lactate, histamine,
serotonin, bradykinins, and prostaglandins
Chemicals depolarize the membrane
potential of the nociceptor to fire a pain signal
NSAIDs
Prostaglandin inhibitors such as aspirin and
non-steroidal anti-inflammatory drugs (NSAIDs)
are commonly used to manage pain
Prostaglandins are formed when cells are
damaged. Phospholipase A breaks down cell
membrane phospholipids into arachidonic acid
Arachidonic acid is then converted to
prostaglandins by the enzyme cyclo-oxygenase
Prostaglandins increase the sensitivity of
nociceptors pain is felt faster and easier
NSAIDs inhibit the action of cyclooxygenase =
no prostaglandin production!!
Transmission
Transmission is the movement of action
potentials along sensory neurons from
peripheral receptors to the spinal cord and
centrally to the brain (collectively the CNS)
Primary sensory fibers involved in transmission
are A-delta fibers (Aδ) and C fibers
Aδ fibers are larger, myelinated, carry pain info
faster and represent the initial response to
injury
Aδ fibers carry sharp, stinging, highly localized
and acute pain signals
Transmission
C fibers are smaller, unmyelinated and
transmit pain slowly
Pain from these fibers is poorly localized,
feels dull and achy and lasts longer
C fibers typically carry pain info to areas of
the brain that evoke emotional responses
(displeasure, anxiety)
Transmission
Sensory afferent pain fibers enter the spinal cord by
posterior nerve roots; cell bodies of pain neurons are in
the dorsal root ganglion
In the dorsal horn , collateral branches spread up and
down the spinal cord by the Tract of Lissauer result
in reflex postural adjustments when a painful body part
is suddenly withdrawn from the stimulus
Transmission Sensory afferent fibers
synapse with interneurons,
anterior motor neurons, and
sympathetic preganglionic
neurons in specific regions
of the spinal cord
Neurotransmitters and
neuropeptides are released
at this synapse; Substance
P, glutamate, GABA,
cholecystokinin
These neurotransmitters
bind to the next neuron in
the pathway new action
potential
Transmission to brain
Pain signals transmitted by spinal interneurons are then
conducted to the brain via ascending spinal pathways
Anterolateral tract – the major pathway for pain signal
transmission to brain; travels up the anterolateral
portion of the spinal cord white matter
Also called the “spinothalamic tract
Signals cross to the opposite side of the spinal cord
and carry signals up the contralateral side of the cord
Nociceptor information from the left side of the body
travels up the right anterolateral tract and vice versa.
Anterolateral tract
Two divisions:
1. Neospinothalamic division – Aδ fibers travel up this
tract to the thalamus; signals reach brain quickly,
provide brain with location of pain, no real emotional
connection
2. Paleospinothalamic division – C fibers travel up this
tract slowly and projects to widespread brain areas;
lots of emotional response; pain lasts for a long time
*C fibers are sent to the thalamus, but also the reticular
formation, mesencephalon (midbrain), cerebral cortex,
limbic system and basal ganglia.
Pain identification
The brain can localize pain
sensation because
nociceptor pathways lead
to specific anatomical
regions in the cord and
somatosensory cortex
Sensory Dermatome –
each spinal nerve contains
the nociceptor fibers for a
particular area of the body
surface
If a certain nerve is
injured/pinched, pain will
follow a typical pattern
Perception
Perception occurs when the brain receives
pain signals and interprets them as ‘painful’
Is the result of neural processing of pain
awareness and interpretation of the meaning
of the sensation
Pain is influenced by attention, distraction,
anxiety, fear, fatigue, previous experience
and expectations.
Primary somatosensory cortex and
association region, frontal lobe and limbic
structures all participate in pain processing
Perception of pain
“pain threshold” – the level of painful
stimulation required to be perceived; very
similar in everyone
“pain tolerance” – the degree of pain that one
is willing to bear before seeking relief; varies
widely among individuals
“pain expression” – the way in which the pain
experience is communicated to others; ex.
Facial grimacing, crying, moaning etc.
Modulation
Modulation is the complex mechanism whereby
synaptic transmission of pain signals is altered
Modulation occurs at multiple sites along the
pathway
Rubbing, shaking, pressing are attempts to
decrease the perception of painful stimuli
The “gate control theory” suggests that impulses
carried by large myelinated cutaneous fibers
can ‘close the gate’ on nociceptor impulse
pain signals would be blocked in the spinal cord.
Modulation Descending pathways from
the brain, more specifically
from the brainstem nucleus
called “raphe magnus”, can
project to the dorsal horn and
inhibit transmission of pain
signals
Opioids such as endorphins
and opioid drugs like
morphine produce analgesic
effects by inhibiting
Substance P release from
nociceptor neurons
Nociceptive inhibition
During periods of pain and stress, the body
can modulate pain
Serotonin, endorphins and norepinephrine all
produce analgesic effects
“stress-induced analgesia” – brain secretes
endogenous opioids
Binding of the endogenous opioids, such as
enkephalin, inhibit the release of substance P
at the synapse, and thus block the
transmission of pain
Pain Transmission
Acute vs. Chronic pain
Acute pain – resolves Chronic pain – lasts longer
when tissue injury heals, than several months beyond
usually less than 3 months, expected healing time, not
signs and symptoms typical associated with SNS activity
for stimulation of SNS body becomes
(tachycardia, increase accustomed to pain and
breathing rate etc) desensitized to noxious input
Short term therapy with Symptoms are often
nonopioid or opioid drugs is psychological (lack of sleep,
helpful disruption of routine, irritability
etc.
Most common causes of
acute pain is headache Common chronic pain
and/or migraines syndrome is fibromyalgia
collection of symptoms
without a clear physiologic
cause
Other types of pain
Cancer-related pain – subcategory of chronic pain but
may involve acute pain episodes
- Pain is a result of infiltration of organs, compression of
structures by tumor, or as a result of treatment that
damage tissues
Neuropathic pain – complex, disabling chronic pain that
results from damaged or dysfunctional nerves (not
stimulation of pain receptors)
- Can result from surgery, elevated blood glucose, viral
infection, trauma and is characterized by constant
aching sensations with bursts of burning or shock-like
pain
Other types of pain
Ischemic pain – resulting from sudden or
profound loss of blood flow to the tissues in a
particular body part (common in MI)
-lowered perfusion tissue hypoxia and injury
release of inflammatory and pain-
producing chemicals
-aching, burning or prickling pain until blood
flow is improved
Referred Pain – pain that is perceived in an area
other than the site of the injury
Common in MI pain is often felt in the jaw or left
arm
Often pain is referred to other structures in the same
sensory dermatome
Sometimes the brain cannot differentiate between
two sources of pain
Week 4
Fluid Electrolyte
Chapter 24 -25
GI Chapter
Chapter 36
You might also like
- Infectious Disorders HandoutsDocument35 pagesInfectious Disorders Handoutsfebie pachecoNo ratings yet
- لقطة شاشة ٢٠٢٣-١١-٠٩ في ٨.٥٣.٥٠ صDocument7 pagesلقطة شاشة ٢٠٢٣-١١-٠٩ في ٨.٥٣.٥٠ صmo44hh44No ratings yet
- Chetna NewDocument8 pagesChetna NewRAVINDER YADAVNo ratings yet
- Inflammation: Course Teacher: Imon RahmanDocument21 pagesInflammation: Course Teacher: Imon RahmanDaksh SabharwalNo ratings yet
- Acut INFLAMMATION - banaldrobie banaldrobieDocument11 pagesAcut INFLAMMATION - banaldrobie banaldrobieammarNo ratings yet
- Acute InflammationDocument10 pagesAcute InflammationLydia Angel HartonoNo ratings yet
- InflammationDocument40 pagesInflammationSangameswaran B.BNo ratings yet
- Inflammation and Inflammatory MediatorsDocument28 pagesInflammation and Inflammatory Mediatorsla.instagramawaNo ratings yet
- Inflammation 30.08.2022Document39 pagesInflammation 30.08.2022Abdur RaquibNo ratings yet
- Pathology (Inflammation and Wound Healing)Document14 pagesPathology (Inflammation and Wound Healing)andrew100% (1)
- Inflammation and Tissue Repair: July 2021Document54 pagesInflammation and Tissue Repair: July 2021EdenNo ratings yet
- IVMS - General Pathology, Inflammation NotesDocument19 pagesIVMS - General Pathology, Inflammation NotesMarc Imhotep Cray, M.D.100% (1)
- 6.hypersensitivity Reactions 2Document32 pages6.hypersensitivity Reactions 2عوض الكريمNo ratings yet
- Immunity PosterDocument6 pagesImmunity PosterAirJeans GamingNo ratings yet
- Inflammation CompleteDocument56 pagesInflammation CompletePunjabi Culture KhushabNo ratings yet
- 4.-acute-inflammationDocument68 pages4.-acute-inflammationjoshuafadama62No ratings yet
- Inflammatory ResponseDocument4 pagesInflammatory ResponsealoisinelsonNo ratings yet
- Protection and Hypersensitivity Mechanism Which Manifest On SkinDocument99 pagesProtection and Hypersensitivity Mechanism Which Manifest On SkinBhayuBarunaNo ratings yet
- Pathophysiology _ InflammationDocument10 pagesPathophysiology _ InflammationIngrid Caroline MunizNo ratings yet
- 2 - Hypersensitvity ReactionsDocument55 pages2 - Hypersensitvity ReactionsSafa TaweelNo ratings yet
- Week 2 - Hour 1 - Inflammation and Wound HealingDocument37 pagesWeek 2 - Hour 1 - Inflammation and Wound HealingniranjiNo ratings yet
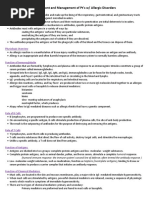
- Assessment and Management of Pt's W/ Allergic Disorders: Physiologic OverviewDocument11 pagesAssessment and Management of Pt's W/ Allergic Disorders: Physiologic OverviewChristina RichardsNo ratings yet
- Session 2Document65 pagesSession 2kasper mkNo ratings yet
- Source:Immunology Eight Edition David MaleDocument3 pagesSource:Immunology Eight Edition David MaleAzzahra FadhlilaNo ratings yet
- Hypersensitivity Reactions Type 3 and Type 4, Pathogenesis of AutoimmunityDocument20 pagesHypersensitivity Reactions Type 3 and Type 4, Pathogenesis of AutoimmunitySalomeSibashviliNo ratings yet
- INFLAMMATION للدراسة الاولية 2023 2024 exportDocument5 pagesINFLAMMATION للدراسة الاولية 2023 2024 exporthaidernajivpn2001No ratings yet
- Acute and Chronic Inflammation: Fatima Obeidat, MDDocument108 pagesAcute and Chronic Inflammation: Fatima Obeidat, MDraanja2100% (1)
- PUBHEALTHDocument18 pagesPUBHEALTHChi Keung Langit ChanNo ratings yet
- Acute Inflammation (1)Document55 pagesAcute Inflammation (1)Chilupula T PetronellaNo ratings yet
- InflammationDocument8 pagesInflammationGhazi Uddin AhmedNo ratings yet
- Workshop 1.2 Inflammation1Document30 pagesWorkshop 1.2 Inflammation1nganleo5801No ratings yet
- Inflammation and RepairDocument34 pagesInflammation and Repairanshum guptaNo ratings yet
- HypersensitivityDocument49 pagesHypersensitivityAkanksha Mahajan100% (1)
- InflammationDocument34 pagesInflammationمصطفى أحمدNo ratings yet
- Inflammation and Healing ReportDocument48 pagesInflammation and Healing Reportks75q5w94yNo ratings yet
- Mechanisms of Inflammation I, II, and III LOsDocument9 pagesMechanisms of Inflammation I, II, and III LOsAndrew SagalovNo ratings yet
- 700 - Wk. 2 - Inflammation, Infection & HIV LODocument10 pages700 - Wk. 2 - Inflammation, Infection & HIV LOAfNo ratings yet
- 3.acute InflammationDocument38 pages3.acute Inflammationyaqeenallawi23No ratings yet
- Drugs Acting On The Immune System: Retchel-Elly D. Dapli-AnDocument60 pagesDrugs Acting On The Immune System: Retchel-Elly D. Dapli-AnJoshua MendozaNo ratings yet
- GP LEC 3Document28 pagesGP LEC 3hetler343No ratings yet
- Immune FinalDocument53 pagesImmune FinalJaylord VerazonNo ratings yet
- Innate ImmunityDocument32 pagesInnate ImmunityYik sNo ratings yet
- Pathophysiology (Chapter 3 & 4)Document50 pagesPathophysiology (Chapter 3 & 4)tedasetesama8No ratings yet
- Inflammation and RepairDocument2 pagesInflammation and RepairSha BtstaNo ratings yet
- PHAR 233-InflammationDocument67 pagesPHAR 233-InflammationLina RamojNo ratings yet
- Allergy and HypersensitivityDocument49 pagesAllergy and HypersensitivityMoshe Cohen'sNo ratings yet
- 2nd Book-Physical Therapy, 2022Document88 pages2nd Book-Physical Therapy, 2022Ahmed Mahmoud MohamedNo ratings yet
- GenPath Mod3 InflammationDocument56 pagesGenPath Mod3 InflammationDanielle HayagNo ratings yet
- Disorders of Immunity Hypersensitivity Reactions: Dr. Mehzabin AhmedDocument25 pagesDisorders of Immunity Hypersensitivity Reactions: Dr. Mehzabin AhmedFrances FranciscoNo ratings yet
- Study-Notes - Inflammation-And-Repair (1) 88Document17 pagesStudy-Notes - Inflammation-And-Repair (1) 88jjjkkNo ratings yet
- Immunity 2Document4 pagesImmunity 2Mkhize KhabazelaNo ratings yet
- Inflammation and RepairDocument77 pagesInflammation and RepaironyekaNo ratings yet
- InflammationDocument8 pagesInflammationHarjot RandhawaNo ratings yet
- INFLAMMATIONDocument9 pagesINFLAMMATIONalkasimamina002No ratings yet
- Hypersensitivity ReactionsDocument25 pagesHypersensitivity Reactionsbpt2100% (4)
- HypersensitivityDocument30 pagesHypersensitivityShweta Mittal100% (1)
- Overview of InflammationDocument6 pagesOverview of InflammationArmand LiberatoNo ratings yet
- Inflammation 3Document44 pagesInflammation 3mikiyaskayleNo ratings yet
- Immunology Unveiled: A Comprehensive Journey through the Human Immune System: Guardians of the Body: The Unseen Heroes of ImmunityFrom EverandImmunology Unveiled: A Comprehensive Journey through the Human Immune System: Guardians of the Body: The Unseen Heroes of ImmunityNo ratings yet
- Hdp301vascularpathologies 2021Document2 pagesHdp301vascularpathologies 2021Linda NguyenNo ratings yet
- Wound Care and Sterile TechniqueDocument27 pagesWound Care and Sterile TechniqueLinda NguyenNo ratings yet
- Respiratory Failure, Hypoxia and HypercapneaDocument4 pagesRespiratory Failure, Hypoxia and HypercapneaLinda NguyenNo ratings yet
- UntitledDocument2 pagesUntitledLinda NguyenNo ratings yet
- UntitledDocument3 pagesUntitledLinda NguyenNo ratings yet
- Skills Checklist: Inserting A Large Bore Naso-Enteric (Referred To As Nasogastric Tube) or Orogastric Tube For Gastric SuctioningDocument2 pagesSkills Checklist: Inserting A Large Bore Naso-Enteric (Referred To As Nasogastric Tube) or Orogastric Tube For Gastric SuctioningLinda NguyenNo ratings yet
- Hdp301infectionrevisedoct2020 1Document24 pagesHdp301infectionrevisedoct2020 1Linda NguyenNo ratings yet
- Acid /base BalanceDocument10 pagesAcid /base BalanceLinda NguyenNo ratings yet
- Hdp301f&e Imbalancesf2020Document6 pagesHdp301f&e Imbalancesf2020Linda NguyenNo ratings yet
- Infection BacteriaandvirusesDocument3 pagesInfection BacteriaandvirusesLinda NguyenNo ratings yet