0 ratings0% found this document useful (0 votes)
14 viewsHyperthyroidism
Hyperthyroidism
Uploaded by
Navin Adhikari- Graves' disease is the most common cause of hyperthyroidism, accounting for 60-80% of cases. It most often affects women ages 20-50 and the elderly.
- Hyperthyroidism is defined as a state of thyroid hormone excess due to inappropriately high thyroid hormone synthesis and secretion by the thyroid gland. Signs and symptoms include hyperactivity, heat intolerance, palpitations, weight loss, and tremors.
- Treatment options for Graves' disease include antithyroid medications like propylthiouracil or methimazole, beta blockers, radioactive iodine therapy, or surgery. Subacute thyroiditis is treated with aspirin, NSAIDs, st
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Hyperthyroidism
Hyperthyroidism
Uploaded by
Navin Adhikari0 ratings0% found this document useful (0 votes)
14 views33 pages- Graves' disease is the most common cause of hyperthyroidism, accounting for 60-80% of cases. It most often affects women ages 20-50 and the elderly.
- Hyperthyroidism is defined as a state of thyroid hormone excess due to inappropriately high thyroid hormone synthesis and secretion by the thyroid gland. Signs and symptoms include hyperactivity, heat intolerance, palpitations, weight loss, and tremors.
- Treatment options for Graves' disease include antithyroid medications like propylthiouracil or methimazole, beta blockers, radioactive iodine therapy, or surgery. Subacute thyroiditis is treated with aspirin, NSAIDs, st
Original Title
hyperthyroidism (1)
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
- Graves' disease is the most common cause of hyperthyroidism, accounting for 60-80% of cases. It most often affects women ages 20-50 and the elderly.
- Hyperthyroidism is defined as a state of thyroid hormone excess due to inappropriately high thyroid hormone synthesis and secretion by the thyroid gland. Signs and symptoms include hyperactivity, heat intolerance, palpitations, weight loss, and tremors.
- Treatment options for Graves' disease include antithyroid medications like propylthiouracil or methimazole, beta blockers, radioactive iodine therapy, or surgery. Subacute thyroiditis is treated with aspirin, NSAIDs, st
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
0 ratings0% found this document useful (0 votes)
14 views33 pagesHyperthyroidism
Hyperthyroidism
Uploaded by
Navin Adhikari- Graves' disease is the most common cause of hyperthyroidism, accounting for 60-80% of cases. It most often affects women ages 20-50 and the elderly.
- Hyperthyroidism is defined as a state of thyroid hormone excess due to inappropriately high thyroid hormone synthesis and secretion by the thyroid gland. Signs and symptoms include hyperactivity, heat intolerance, palpitations, weight loss, and tremors.
- Treatment options for Graves' disease include antithyroid medications like propylthiouracil or methimazole, beta blockers, radioactive iodine therapy, or surgery. Subacute thyroiditis is treated with aspirin, NSAIDs, st
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
Download as pptx, pdf, or txt
You are on page 1of 33
APPROACH TO HYPERTHYROIDISM
Dr. Wishama Abdul Razzag
NAMS, Bir Hospital.
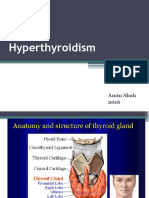
Graves disease
• Graves’ disease accounts for 60–80% of
thyrotoxicosis
• Prevalence 2 % in female and 1/1o th in male
• Age group common is 20-50 years and elderely
• The term ‘‘hyperthyroidism,’’ is a form of
thyrotoxicosis due to inappropriately high synthesis
and secretion of thyroid hormone(s) by the thyroid.
(ATA defination)
Thyrotoxicosis
• Thyrotoxicosis is a state of thyroid hormone excess
American thyroid association
defination
• Thyrotoxicosis is a condition having multiple eti-
ologies, manifestations, and potential therapies. The
term ‘‘thyrotoxicosis’’ refers to a clinical state that
results from inappropriately high thyroid hormone
action in tissues generally due to inappropriately
high tissue thyroid hormone levels.
Signs and Symptoms of
Thyrotoxicosis
• Hyperactivity, irritability, dysphoria
• Heat intolerance and sweating
• Palpitations
• Fatigue and weakness
• Weight loss with increased appetite
• Diarrhea, mild steatorrhea
• Polyuria
• Oligomenorrhea, loss of libido
• Tachycardia; atrial fibrillation in the elderly
• Tremor, muscle wasting, proximal myopathy, hyperreflexia
• Goiter ,( osteopenia in long bone) fractures
• Warm, moist skin, pruritus, urticaria, diffuse hyperpigmentation, fine hair texture, Alopecia
• Muscle weakness, proximal myopathy
• Lid retraction or lag
• Gynecomastia
Inspection
• Alopecia
• Proptosis
• Goiter
• Lean and thin body build
• Sweating hand
• Palmar erythema
• Hyperpigmentation of skin
• Gynecomastia
• Anxious and anxiety
• Swelling of leg
Graves opthalmopathy
Pathogenesis
• TSI and TBII assays. The presence of TBII in a patient with thyrotoxicosis
implies the existence of TSI, and these assays are useful in monitoring
pregnant Graves’ patients in whom high levels of TSI can cross the
placenta and cause neonatal thyrotoxicosis. Other
• TPO antibodies occur in up to 80% of cases and serve as a readily
measurable marker of autoimmunity.
• Cytokines appear to play a major role in thyroid-associated
ophthalmopathy
• TSH-R
Assessment of thyroid function
Serum TSH Serum free T4 Serum T3 Assessment
Normal hypothalamic-pituitary function
Normal Normal Normal Euthyroid
Euthyroid
Normal Normal or high Normal or high hyperthyroxinemia
Normal Normal or low Normal or low Euthyroid hypothyroxinema
Normal Low Normal or high Euthyroid: T3 therapy
Euthyroid: thyroid extract
Normal Low-normal or low Normal or high
therapy
High Low Normal or low Primary hypothyroidism
High Normal Normal Subclinical hypothyroidism
Low High or normal High Hyperthyroidism
Low Normal Normal Subclinical hyperthyroidism
Abnormal hypothalamic-pituitary function
TSH-mediated
Normal or high High High hyperthyroidism
Normal or low* Low or low-normal Low or normal Central hypothyroidism
• Subclinical hyperthyroidism is defined as a normal
serum free T4 and normal total T3 or free T3, with
subnormal serum TSH con- centration.
• overt hyperthyroidism, serum free T4, T3, or both
are elevated, and serum TSH is subnormal (usually
<0.01 mU/L in a third-generation assay).
• mild hyperthyroidism, serum T4 and free T4 can be
normal, only serum T3 may be elevated, and serum
TSH will be low or undetectable.
• Subacute thyroiditis is thought to be caused by viral
infection and is characterized by fever and thyroid
pain
• Painless thyroiditis:- due to lithium, Amiodarone,
postpartum
Note
• Serum TSH levels are considerably more sensitive
than direct thyroid hormone measurements for
assessing thyroid hormone excess
• Before doing TFT we should know error or abnormal
TFT report due to biotin, heterophilic antibody
• Stop biotin 2 days before
Investigation
• Drugs history intake history
• Thyroid function test, LFT, gamma gt, ALP, serum calcium, Blood sugar, bilirubin
• Anti TPO
• TBII assay, transthyretin, measurement of TRAb
• Ultrasound neck, thyroidal blood flow on ultrasonography
• Ultrasound pelvis
• B hcg level in urine and blood
• spot urine iodine adjusted for urine creatinine concentration or a 24-hour urine
iodine concentration)
• Radioiodine uptake scan (99mTc, 123I, or 131I)
• ECG
• Echocardiography
• Holter monitor
• Eye examination
• magnetic resonance imaging
• The ratio of total T3 to total T4 can also be useful in assessing the
etiology of thyrotoxicosis when scintigraphy is contraindicated.
Because a hyperactive gland produces more T3 than T4, T3 will be
elevated above the upper limit of normal more than T4 in
thyrotoxicosis caused by hyperthyroidism
• T4 is elevated more than T3 in thyrotoxicosis caused by thyroiditis
• A high T4 to T3 ratio may be seen in thyrotoxicosis factitia (from
exogenous levothyroxine).
• Patients with painless thyroiditis presenting within the first year
after childbirth (postpartum thyroiditis) often have a personal or
family history of auto-immune thyroid disease and typically have
measurable serum concentrations of anti–thyroid peroxidase
antibodies
How do thyroid function tests change
during pregnancy?
• Normal pregnancy is associated with an increase in
renal iodine excretion, an increase in thyroxine
binding proteins, an increase in thyroid hormone
production, and thyroid stimulatory effects of hCG.
What is the normal reference range
for serum TSH concentrations in each trimester
of pregnancy?
• A downward shift of the TSH reference range occurs during
pregnancy, with a reduction in both the lower (de-creased by
about 0.1–0.2 mU/L) and the upper limit of ma- ternal TSH
(decreased by about 0.5–1.0 mU/L), relative to the typical
nonpregnant TSH reference range.
• The largest decrease in serum TSH is observed during the first
trimester because of elevated levels of serum hCG directly
stimulating the TSH receptor and thereby increasing thyroid
hormone production
• recommendations for a TSH upper reference limit of 2.5 mU/L
in the first trimester and 3.0 mU/ L in the second and third
trimesters
Evaluation
How to establish differentials??
Treatment modality of Graves disease
• Antithyroid drugs:
• Propylthiouracil 100-200 mg every 6 to 8 hourly
• Carbimazole 10-20 mg every 8 10 12 hourly
• Methimazole 10-20 mg every 8 10 12 hourly
• Beta blokers:- Propanolol 20-40 mg every 6 hourly
• Radioiodine
• Anticoagulant therapy
• Subtotal or near total thyroidectomy
Subacute thyroiditis
• large doses of aspirin (e.g., 600 mg every 4–6 h) or
NSAIDs
• 40–60 mg of prednisone (Steroid)
• Levothyroxine replacement (50–100 μg daily)
Treatment of opthalmopathy
• Explain natural history of ophthalmopathy
• Avoid smoking.
• Discomfort can be relieved with Artificial tears (e.g., 1%
methylcellulose), eye ointment
• Dark glasses with side frames.
• Periorbital edema may respond to a more upright
sleeping position or a diuretic.
• Corneal exposure during sleep can be avoided by using
patches or taping the eyelids, Minor degrees of diplopia
improve with prisms fitted to spectacles. is preferable to
oral glucocorticoids,
Severe opthalmopathy
• Severe ophthalmopathy, with optic nerve
involvement or chemosis resulting in corneal
damage, is an emergency treatment
• Pulse therapy with IV methylprednisolone (e.g., 500
mg of methylprednisolone once weekly for 6 weeks,
then 250 mg once weekly for 6 weeks)
• Orbital decompression can be achieved by removing
bone from any wall of the orbit, thereby allowing
displacement of fat and swollen extraocular
muscles.
Thyroid dermopathy
• Thyroid dermopathy does not usually require
treatment, but it can cause cosmetic problems or
interfere with the fit of shoes.
• Surgery not required
• potency glucocorticoid ointment under an occlusive
dressing.
• Octreotide may be beneficial in some cases.
Indications for treatment of endogenous subclinical
hyperthyroidism in nonpregnant adults*
THANK YOU
You might also like
- Urinary System WorksheetDocument4 pagesUrinary System Worksheetayoonia75% (4)
- Peripheral Nervous SystemDocument1 pagePeripheral Nervous SystemChris_Barber09No ratings yet
- ThyrotoxicosisDocument105 pagesThyrotoxicosisAli Murtaza Abbas100% (1)
- Thyroid Function TestDocument28 pagesThyroid Function TestDhinesh Muthusamy100% (1)
- Thyroid Function TestDocument21 pagesThyroid Function TestPat JacintoNo ratings yet
- Thyroid Disorder: Meaza Bulbula (M. Pharm)Document61 pagesThyroid Disorder: Meaza Bulbula (M. Pharm)Ko MhdNo ratings yet
- Lec#15+16 Thyroid DisordersDocument82 pagesLec#15+16 Thyroid DisordersKhaldoun AlmomaniNo ratings yet
- PharmacotherapyDocument63 pagesPharmacotherapyNyahahahaNo ratings yet
- Hyperthyroid Is MDocument45 pagesHyperthyroid Is MThippagalla Harshitha HarshithaNo ratings yet
- Tutorial Presentation: Artika Mala (s170201) Week 2Document22 pagesTutorial Presentation: Artika Mala (s170201) Week 2Artika MalaNo ratings yet
- Hormone Assays: Immuno-Serology SectionDocument52 pagesHormone Assays: Immuno-Serology SectionjeffreyNo ratings yet
- Thyroid DiseaseDocument36 pagesThyroid Diseasejozemomo206No ratings yet
- Mbs127 Slide Hyperthyroidism 1Document46 pagesMbs127 Slide Hyperthyroidism 1revita262No ratings yet
- THYROIDDocument191 pagesTHYROIDTonie AbabonNo ratings yet
- Lecture (1) - THDocument34 pagesLecture (1) - THyoussef hossamNo ratings yet
- Lecture 17 - Thyroid Disorders (Including Struma and CA Thyroid) - Dr. M. Robikhul Ikhsan, SP - PD-KEMD (2021)Document21 pagesLecture 17 - Thyroid Disorders (Including Struma and CA Thyroid) - Dr. M. Robikhul Ikhsan, SP - PD-KEMD (2021)Ivan AditamaNo ratings yet
- Hypo Thyroid Is MDocument27 pagesHypo Thyroid Is Mdhiraj parmarNo ratings yet
- Hyperthyroid Is MDocument42 pagesHyperthyroid Is MkapilNo ratings yet
- Interpretation of Laboratory Thyroid Function Tests: The "Hidden" Health ProblemDocument38 pagesInterpretation of Laboratory Thyroid Function Tests: The "Hidden" Health Problemalanoud.877No ratings yet
- Sophie Keyte Bvms (Hons) Mvetmed (Dist) Fhea Dipacvim Mrcvs Sophie - Keyte@Bristol - Ac.UkDocument24 pagesSophie Keyte Bvms (Hons) Mvetmed (Dist) Fhea Dipacvim Mrcvs Sophie - Keyte@Bristol - Ac.UkStefana UrsuNo ratings yet
- Hyperthyroid 170715182805Document71 pagesHyperthyroid 170715182805Suryati HusinNo ratings yet
- Thyroid ReportDocument105 pagesThyroid ReportAARVNo ratings yet
- Thyroid DiseaseDocument72 pagesThyroid Diseaseluna zeidNo ratings yet
- Hyperthyroidism and HypothyroidismDocument59 pagesHyperthyroidism and HypothyroidismJun AmaroNo ratings yet
- Management of Thyroid DisordersDocument119 pagesManagement of Thyroid DisordersmatthiaspaullowNo ratings yet
- Hormones 20Document80 pagesHormones 20Stephanie Ortiz FonsecaNo ratings yet
- Lecture (2) TherapDocument25 pagesLecture (2) Therapyoussef hossamNo ratings yet
- 09 Thyroid Practice - v2Document23 pages09 Thyroid Practice - v2Shahriar honarmandNo ratings yet
- Hyper and HypothyroidismDocument63 pagesHyper and Hypothyroidismmeetgagiya2005No ratings yet
- #30 Thyroid and Thyroid TestingDocument25 pages#30 Thyroid and Thyroid TestingasclswisconsinNo ratings yet
- Thyroid Gland L-Thyroxine (T4) Vs Triiodothyronine (T3) : Follicular CellsDocument7 pagesThyroid Gland L-Thyroxine (T4) Vs Triiodothyronine (T3) : Follicular CellsPrincess Noreen SavellanoNo ratings yet
- Thyroid DiseasesDocument77 pagesThyroid DiseasesAllan MakalaNo ratings yet
- Thyroid DiseasesDocument44 pagesThyroid DiseasesPLDT HOMENo ratings yet
- Thyroid Gland DisordersDocument64 pagesThyroid Gland DisordersFaisal RavifNo ratings yet
- F1) P-Thyroid DisordersDocument9 pagesF1) P-Thyroid Disordersstella.gillesania.chenNo ratings yet
- DR Ananta Thyroid SlideDocument73 pagesDR Ananta Thyroid SlideRoshan Kumar PanditNo ratings yet
- Thyroid Function Test and Adrenal Function TestsDocument64 pagesThyroid Function Test and Adrenal Function TestsDr Abhinav Manish MDNo ratings yet
- Thyroid Gland Diseases in ChildrenDocument29 pagesThyroid Gland Diseases in ChildrenadinayNo ratings yet
- THYROTOXICOSISDocument20 pagesTHYROTOXICOSISfig8fashion1No ratings yet
- Hypothyroid in Pregnancy Andi CakraDocument32 pagesHypothyroid in Pregnancy Andi CakraCakraEkky100% (1)
- Thyroid Function Tests PPT of IMS BHUDocument74 pagesThyroid Function Tests PPT of IMS BHUPriyanshu Mandal100% (1)
- PATIENT WITH ENDOCRINE DYSFUNCTION THYROID .pptx1Document52 pagesPATIENT WITH ENDOCRINE DYSFUNCTION THYROID .pptx1sembakarani thevagumaranNo ratings yet
- HypothyroidismDocument59 pagesHypothyroidismAmir Mahmoud100% (1)
- HypertyroidismDocument46 pagesHypertyroidismenriNo ratings yet
- Thyroid Function Tests: Drneha Mahajan MD PathologyDocument71 pagesThyroid Function Tests: Drneha Mahajan MD PathologyMukesh Kumar ChaudharyNo ratings yet
- Thyroid Disease in PregnancyDocument67 pagesThyroid Disease in PregnancySiti Fatimah100% (2)
- Endocrinologic DisordersDocument80 pagesEndocrinologic Disordersfanuiel mandefroNo ratings yet
- HYPERTHYROIDISMDocument40 pagesHYPERTHYROIDISMEmmanuelNo ratings yet
- Thyroid DisordersDocument22 pagesThyroid DisordersNimer Abdelhadi AliNo ratings yet
- THyroid Function Test 123Document36 pagesTHyroid Function Test 123lenin coolNo ratings yet
- SC2 2015 HyperthyroidismDocument38 pagesSC2 2015 HyperthyroidismShafern TanNo ratings yet
- Thyroid Disorders: (Hyperthyroidism and Hypothyroidism)Document28 pagesThyroid Disorders: (Hyperthyroidism and Hypothyroidism)Mina RoxasNo ratings yet
- Hypothyroidism: Bagian Penyakit Dalam FK Uisu MedanDocument50 pagesHypothyroidism: Bagian Penyakit Dalam FK Uisu Medanindra saputraNo ratings yet
- Hyperthyroidism: A Practical Approach To Diagnosis and ManagementDocument70 pagesHyperthyroidism: A Practical Approach To Diagnosis and ManagementMutiara Manuella TambaNo ratings yet
- Thyroid Function TestsDocument29 pagesThyroid Function TestsAkwesaNo ratings yet
- Medical and Surgical Complications in Pregnancy: Ramon M. Gonzalez, MDDocument161 pagesMedical and Surgical Complications in Pregnancy: Ramon M. Gonzalez, MDaldeeray01No ratings yet
- TFT Interpretation of Difficult CasesDocument51 pagesTFT Interpretation of Difficult CasesAditya GautamNo ratings yet
- Thyroid LectureDocument65 pagesThyroid LectureAndres TabaresNo ratings yet
- Thyrotoxicosis: Presenter: Emiacu Kenneth Facilitator: Dr. Freddie KibengoDocument35 pagesThyrotoxicosis: Presenter: Emiacu Kenneth Facilitator: Dr. Freddie KibengoNinaNo ratings yet
- Disorders of The Thyroid GandDocument167 pagesDisorders of The Thyroid GandWendy Figueroa MijaresNo ratings yet
- Medical and Surgical Complications PDFDocument206 pagesMedical and Surgical Complications PDFparmcparmcNo ratings yet
- Core CH 8 Transport in HumansDocument10 pagesCore CH 8 Transport in Humansommp100% (1)
- Learning Objectives:: Pathophysiology & Therapeutics, I (MSPR 521) Lecture No. 14Document9 pagesLearning Objectives:: Pathophysiology & Therapeutics, I (MSPR 521) Lecture No. 14adzhangNo ratings yet
- DR - Datis - Kharrazian Gut Bacteria TranscriptDocument35 pagesDR - Datis - Kharrazian Gut Bacteria TranscriptGreg Wolfe100% (4)
- Integumentary SystemDocument34 pagesIntegumentary SystemJerneth Nyka FloresNo ratings yet
- Human Body - Wikipedia PDFDocument18 pagesHuman Body - Wikipedia PDFMavura ZwideNo ratings yet
- Tumors of Nervous SystemDocument50 pagesTumors of Nervous SystemNininghrNo ratings yet
- Brain Anatomy ThesisDocument4 pagesBrain Anatomy Thesisbrittanyjonescolumbia100% (2)
- Chapter 79. Adrenal GlandsDocument42 pagesChapter 79. Adrenal GlandsJeremy IrvanNo ratings yet
- The PNF (Proprioceptive Neuromuscular Facilitation) Stretching Technique - A Brief ReviewDocument6 pagesThe PNF (Proprioceptive Neuromuscular Facilitation) Stretching Technique - A Brief ReviewDiane Troncoso Alegria0% (1)
- The Human Body in Art Education Presentation in Red Brown Hand Drawn Textured StyleDocument73 pagesThe Human Body in Art Education Presentation in Red Brown Hand Drawn Textured StyleMiangela lalaNo ratings yet
- Pag-Oring Nuevo National High SchoolDocument2 pagesPag-Oring Nuevo National High SchoolAlmiraMayAlvarezMarquezNo ratings yet
- NCM 106 Drugs Acting On Immune SystemDocument24 pagesNCM 106 Drugs Acting On Immune SystemLi mNo ratings yet
- The Endocrine SystemDocument41 pagesThe Endocrine SystemОксана КрасильниковаNo ratings yet
- Lymphoma Dr. Asad 13.7.2023Document181 pagesLymphoma Dr. Asad 13.7.2023Yousuf SawdagorNo ratings yet
- Reproductive SystemDocument7 pagesReproductive SystemRiaz siddiquiNo ratings yet
- Science Unit 1 7TH JDocument2 pagesScience Unit 1 7TH JHafiz Danish Rehman RanaNo ratings yet
- Gannguan PubertasDocument56 pagesGannguan PubertasAde Yosdi PutraNo ratings yet
- Anatomy & Physiology: Mrs. Tina Joy G. Mante, RN, MANDocument30 pagesAnatomy & Physiology: Mrs. Tina Joy G. Mante, RN, MANTina G. ManteNo ratings yet
- Learn The Anatomy of The HeartDocument2 pagesLearn The Anatomy of The Heartapi-534129744No ratings yet
- Assessment of Neurologic FunctionDocument63 pagesAssessment of Neurologic FunctionChombe JcNo ratings yet
- The Respiratory SystemDocument8 pagesThe Respiratory SystemDavid DanielNo ratings yet
- Paediatric Nephrology Syllabus FinalDocument13 pagesPaediatric Nephrology Syllabus FinalClever BarbieNo ratings yet
- Lymphatic SystemDocument5 pagesLymphatic SystemEmmanuel A. GalvanNo ratings yet
- Lymphatic System MCQDocument6 pagesLymphatic System MCQtarekhk05No ratings yet
- McqsDocument10 pagesMcqsDAWOODNo ratings yet
- Data Olahan Rawat Inap2014Document58 pagesData Olahan Rawat Inap2014daffa11No ratings yet
- Histopathology: Acute T-Cell Mediated Rejection: Anne Margarette Canapi, MDDocument75 pagesHistopathology: Acute T-Cell Mediated Rejection: Anne Margarette Canapi, MDAnneCanapiNo ratings yet
- Central Nervous System: The Spinal CordDocument30 pagesCentral Nervous System: The Spinal CordRO OMNo ratings yet