Lactoferrin (LF), also known as lactotransferrin (LTF), is a multifunctional protein of the transferrin family. Lactoferrin is a globular glycoprotein with a molecular mass of about 80 kDa that is widely represented in various secretory fluids, such as milk, saliva, tears, and nasal secretions. Lactoferrin is also present in secondary granules of PMNs and is secreted by some acinar cells. Lactoferrin can be purified from milk or produced recombinantly. Human colostrum ("first milk") has the highest concentration, followed by human milk, then cow milk (150 mg/L).[5]
Lactoferrin is one of the components of the immune system of the body; it has antimicrobial activity (bacteriocide, fungicide) and is part of the innate defense, mainly at mucoses.[5] It is constantly produced and released into saliva, tears, as well as seminal and vaginal fluid.[6] Lactoferrin provides antibacterial activity to human infants.[7][8] Lactoferrin interacts with DNA and RNA, polysaccharides and heparin, and shows some of its biological functions in complexes with these ligands.
Lactoferrin supplements reduce the risk of respiratory tract infections, based on a recent meta-analysis of randomized controlled trials.[9] As with any supplements sold online, quality may be an issue because nutritional supplement production quality controls are not subject to the same strict regulatory process as medicines.[10]
History
editOccurrence of iron-containing red protein in bovine milk was reported as early as in 1939;[11] however, the protein could not be properly characterized because it could not be extracted with sufficient purity. Its first detailed studies were reported around 1960. They documented the molecular weight, isoelectric point, optical absorption spectra and presence of two iron atoms per protein molecule.[12][13] The protein was extracted from milk, contained iron and was structurally and chemically similar to serum transferrin. Therefore, it was named lactoferrin in 1961, though the name lactotransferrin was used in some earlier publications, and later studies demonstrated that the protein is not restricted to milk. The antibacterial action of lactoferrin was also documented in 1961, and was associated with its ability to bind iron.[14]
Structure
editGenes of lactoferrin
editAt least 60 gene sequences of lactoferrin have been characterized in 11 species of mammals.[15] In most species, stop codon is TAA, and TGA in Mus musculus. Deletions, insertions and mutations of stop codons affect the coding part and its length varies between 2,055 and 2,190 nucleotide pairs. Gene polymorphism between species is much more diverse than the intraspecific polymorphism of lactoferrin. There are differences in amino acid sequences: 8 in Homo sapiens, 6 in Mus musculus, 6 in Capra hircus, 10 in Bos taurus and 20 in Sus scrofa. This variation may indicate functional differences between different types of lactoferrin.[15]
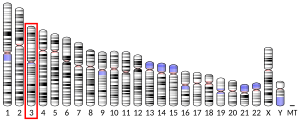
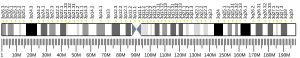
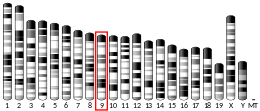
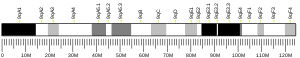
In humans, lactoferrin gene LTF is located on the third chromosome in the locus 3q21-q23. In oxen, the coding sequence consists of 17 exons and has a length of about 34,500 nucleotide pairs. Exons of the lactoferrin gene in oxen have a similar size to the exons of other genes of the transferrin family, whereas the sizes of introns differ within the family. Similarity in the size of exons and their distribution in the domains of the protein molecule indicates that the evolutionary development of lactoferrin gene occurred by duplication.[16] Study of polymorphism of genes that encode lactoferrin helps selecting livestock breeds that are resistant to mastitis.[17]
Molecular structure
editLactoferrin is one of the transferrin proteins that transfer iron to the cells and control the level of free iron in the blood and external secretions. It is present in the milk of humans and other mammals,[13] in the blood plasma and neutrophils and is one of the major proteins of virtually all exocrine secretions of mammals, such as saliva, bile, tears and pancreas.[18] Concentration of lactoferrin in the milk varies from 7 g/L in the colostrum to 1 g/L in mature milk.[citation needed][clarification needed]
X-ray diffraction reveals that lactoferrin is based on one polypeptide chain that contains about 700 amino acids and forms two homologous globular domains named N-and C-lobes. N-lobe corresponds to amino acid residues 1-333 and C-lobe to 345-692, and the ends of those domains are connected by a short α-helix.[19][20] Each lobe consists of two subdomains, N1, N2 and C1, C2, and contains one iron binding site and one glycosylation site. The degree of glycosylation of the protein may be different and therefore the molecular weight of lactoferrin varies between 76 and 80 kDa. The stability of lactoferrin has been associated with the high glycosylation degree.[21]
Lactoferrin belongs to the basic proteins, its isoelectric point is 8.7. It exists in two forms: iron-rich hololactoferrin and iron-free apolactoferrin. Their tertiary structures are different; apolactoferrin is characterized by "open" conformation of the N-lobe and the "closed" conformation of the C-lobe, and both lobes are closed in the hololactoferrin.[22]
Each lactoferrin molecule can reversibly bind two ions of iron, zinc, copper or other metals.[23] The binding sites are localized in each of the two protein globules. There, each ion is bonded with six ligands: four from the polypeptide chain (two tyrosine residues, one histidine residue and one aspartic acid residue) and two from carbonate or bicarbonate ions.
Lactoferrin forms a reddish complex with iron; its affinity for iron is 300 times higher than that of transferrin.[24] The affinity increases in weakly acidic medium. This facilitates the transfer of iron from transferrin to lactoferrin during inflammations, when the pH of tissues decreases due to accumulation of lactic and other acids.[25] The saturated iron concentration in lactoferrin in human milk is estimated as 10 to 30% (100% corresponds to all lactoferrin molecules containing 2 iron atoms). It is demonstrated that lactoferrin is involved not only in the transport of iron, zinc and copper, but also in the regulation of their intake.[26] Presence of loose ions of zinc and copper does not affect the iron binding ability of lactoferrin, and might even increase it.
Polymeric forms
editBoth in blood plasma and in secretory fluids lactoferrin can exist in different polymeric forms ranging from monomers to tetramers. Lactoferrin tends to polymerize both in vitro and in vivo, especially at high concentrations.[25] Several authors found that the dominant form of lactoferrin in physiological conditions is a tetramer, with the monomer:tetramer ratio of 1:4 at the protein concentrations of 10−5 M.[27][28][29]
It is suggested that the oligomer state of lactoferrin is determined by its concentration and that polymerization of lactoferrin is strongly affected by the presence of Ca2+ ions. In particular, monomers were dominant at concentrations below 10−10−10−11 M in the presence of Ca2+, but they converted into tetramers at lactoferrin concentrations above 10−9−10−10 M.[27][30] Titer of lactoferrin in the blood corresponds to this particular "transition concentration" and thus lactoferrin in the blood should be presented both as a monomer and tetramer. Many functional properties of lactoferrin depend on its oligomeric state. In particular, monomeric, but not tetrameric lactoferrin can strongly bind to DNA.
Function
editLactoferrin belongs to the innate immune system. Apart from its main biological function, namely binding and transport of iron ions, lactoferrin also has antibacterial, antiviral, antiparasitic, catalytic, anti-cancer, and anti-allergic functions and properties.[31]
Enzymatic activity of lactoferrin
editLactoferrin hydrolyzes RNA and exhibits the properties of pyrimidine-specific secretory ribonucleases [citation needed]. In particular, by destroying the RNA genome, milk RNase inhibits reverse transcription of retroviruses that cause breast cancer in mice.[32] Parsi women in West India have the milk RNase level markedly lower than in other groups, and their breast cancer rate is three times higher than average.[33] Thus, ribonucleases of milk, and lactoferrin in particular, might play an important role in pathogenesis.
Lactoferrin receptor
editThe lactoferrin receptor plays an important role in the internalization of lactoferrin; it also facilitates absorption of iron ions by lactoferrin. It was shown that gene expression increases with age in the duodenum and decreases in the jejunum.[34] The moonlighting glycolytic enzyme glyceraldehyde-3-phosphate dehydrogenase (GAPDH) has been demonstrated to function as a receptor for lactoferrin.[35]
Bone activity
editRibonuclease-enriched lactoferrin has been used to examine how lactoferrin affects bone. Lactoferrin has shown to have positive effects on bone turnover. It has aided in decreasing bone resorption and increasing bone formation. This was indicated by a decrease in the levels of two bone resorption markers (deoxypyridinoline and N-telopeptide) and an increase in the levels two bone formation markers (osteocalcin and alkaline phosphatase).[36] It has reduced osteoclast formation, which signifies a decrease in pro-inflammatory responses and an increase in anti-inflammatory responses [37] which indicates a reduction in bone resorption as well.
Interaction with nucleic acids
editOne of the important properties of lactoferrin is its ability to bind with nucleic acids. The fraction of protein extracted from milk, contains 3.3% RNA,[27] but, the protein preferably binds to double-stranded DNA rather than single-stranded DNA. The ability of lactoferrin to bind DNA is used for its isolation and purification using affinity chromatography with columns containing immobilized DNA-containing sorbents, such as agarose with the immobilized single-stranded DNA.[38]
Clinical significance
editAntibacterial activity
editLactoferrin's primary role is to sequester free iron, and in doing so remove essential substrate required for bacterial growth.[40] Antibacterial action of lactoferrin is also explained by the presence of specific receptors on the cell surface of microorganisms. Lactoferrin binds to lipopolysaccharide of bacterial walls, and the oxidized iron part of the lactoferrin oxidizes bacteria via formation of peroxides. This affects the membrane permeability and results in the cell breakdown (lysis).[40]
Although lactoferrin also has other antibacterial mechanisms not related to iron, such as stimulation of phagocytosis,[41] the interaction with the outer bacterial membrane described above is the most dominant and most studied.[42] Lactoferrin not only disrupts the membrane, but even penetrates into the cell. Its binding to the bacteria wall is associated with the specific peptide lactoferricin, which is located at the N-lobe of lactoferrin and is produced by in vitro cleavage of lactoferrin with another protein, trypsin.[43][44] A mechanism of the antimicrobial action of lactoferrin has been reported as lactoferrin targets H+-ATPase and interferes with proton translocation in the cell membrane, resulting in a lethal effect in vitro.[45]
Lactoferrin prevents the attachment of H. pylori in the stomach, which in turn, aids in reducing digestive system disorders. Bovine lactoferrin has more activity against H. pylori than human lactoferrin.[46]
Antiviral activity
editLactoferrin in sufficient strength acts on a wide range of human and animal viruses based on DNA and RNA genomes,[47] including the herpes simplex virus 1 and 2,[48][49][50] cytomegalovirus,[51] HIV,[49][52] hepatitis C virus,[53][54] hantaviruses, rotaviruses, poliovirus type 1,[55] human respiratory syncytial virus, murine leukemia viruses[44] and Mayaro virus.[56] Activity against COVID-19 has been speculated but not proven.[57][58][59][60]
The most studied mechanism of antiviral activity of lactoferrin is its diversion of virus particles from the target cells. Many viruses tend to bind to the lipoproteins of the cell membranes and then penetrate into the cell.[54] Lactoferrin binds to the same lipoproteins thereby repelling the virus particles. Iron-free apolactoferrin is more efficient in this function than hololactoferrin; and lactoferricin, which is responsible for antimicrobial properties of lactoferrin, shows almost no antiviral activity.[47]
Beside interacting with the cell membrane, lactoferrin also directly binds to viral particles, such as the hepatitis viruses.[54] This mechanism is also confirmed by the antiviral activity of lactoferrin against rotaviruses,[44] which act on different cell types.
Lactoferrin also suppresses virus replication after the virus penetrated into the cell.[44][52] Such an indirect antiviral effect is achieved by affecting natural killer cells, granulocytes and macrophages – cells, which play a crucial role in the early stages of viral infections, such as severe acute respiratory syndrome (SARS).[61]
Antifungal activity
editLactoferrin and lactoferricin inhibit in vitro growth of Trichophyton mentagrophytes, which are responsible for several skin diseases such as ringworm.[62] Lactoferrin also acts against the Candida albicans – a diploid fungus (a form of yeast) that causes opportunistic oral and genital infections in humans.[63][64] Fluconazole has long been used against Candida albicans, which resulted in emergence of strains resistant to this drug. However, a combination of lactoferrin with fluconazole can act against fluconazole-resistant strains of Candida albicans as well as other types of Candida: C. glabrata, C. krusei, C. parapsilosis and C. tropicalis.[63] Antifungal activity is observed for sequential incubation of Candida with lactoferrin and then with fluconazole, but not vice versa. The antifungal activity of lactoferricin exceeds that of lactoferrin. In particular, synthetic peptide 1–11 lactoferricin shows much greater activity against Candida albicans than native lactoferricin.[63]
Administration of lactoferrin through drinking water to mice with weakened immune systems and symptoms of aphthous ulcer reduced the number of Candida albicans strains in the mouth and the size of the damaged areas in the tongue.[65] Oral administration of lactoferrin to animals also reduced the number of pathogenic organisms in the tissues close to the gastrointestinal tract. Candida albicans could also be completely eradicated with a mixture containing lactoferrin, lysozyme and itraconazole in HIV-positive patients who were resistant to other antifungal drugs.[66] Such antifungal action when other drugs deem inefficient is characteristic of lactoferrin and is especially valuable for HIV-infected patients.[67] Contrary to the antiviral and antibacterial actions of lactoferrin, very little is known about the mechanism of its antifungal action. Lactoferrin seems to bind the plasma membrane of C. albicans inducing an apoptotic-like process.[64][68]
Anticarcinogenic activity
editThe anticancer activity of bovine lactoferrin (bLF) has been demonstrated in experimental lung, bladder, tongue, colon, and liver carcinogeneses on rats, possibly by suppression of phase I enzymes, such as cytochrome P450 1A2 (CYP1A2).[69] Also, in another experiment done on hamsters, bovine lactoferrin decreased the incidence of oral cancer by 50%.[70] Currently, bLF is used as an ingredient in yogurt, chewing gums, infant formulas, and cosmetics.[70]
Cystic fibrosis
editThe human lung and saliva contain a wide range of antimicrobial compound including lactoperoxidase system, producing hypothiocyanite and lactoferrin, with hypothiocyanite missing in cystic fibrosis patients.[71] Lactoferrin, a component of innate immunity, prevents bacterial biofilm development.[72][73] The loss of microbicidal activity and increased formation of biofilm due to decreased lactoferrin activity is observed in patients with cystic fibrosis.[74] In cystic fibrosis, antibiotic susceptibility may be modified by lactoferrin.[75] These findings demonstrate the important role of lactoferrin in human host defense and especially in lung.[76] Lactoferrin with hypothiocyanite has been granted orphan drug status by the EMEA[77] and the FDA.[78]
Necrotizing enterocolitis
editLow quality evidence suggests that oral lactoferrin supplementation with or without the addition of a probiotic may decrease late onset of sepsis and necrotizing enterocolitis (stage II or III) in preterm infants with no adverse effects.[79]
In diagnosis
editLactoferrin levels in tear fluid have been shown to decrease in dry eye diseases such as Sjögren's syndrome.[80] A rapid, portable test utilizing microfluidic technology has been developed to enable measurement of lactoferrin levels in human tear fluid at the point-of-care with the aim of improving diagnosis of Sjögren's syndrome and other forms of dry eye disease.[81]
Technology
editExtraction
editBovine lactoferrin can be isolated from raw milk, colostrum, or whey using methods such as salt extraction, chromatography, and membrane filtration. Lactoferrin from a variety of species, including humans, can also be produced using transgenic organisms as a recombinant protein.[82]
Nanotechnology
editLactotransferrin has been used in the synthesis of fluorescent gold quantum clusters, which has potential applications in nanotechnology.[83]
See also
editReferences
edit- ^ a b c GRCh38: Ensembl release 89: ENSG00000012223 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000032496 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ a b Sánchez L, Calvo M, Brock JH (May 1992). "Biological role of lactoferrin". Archives of Disease in Childhood. 67 (5): 657–61. doi:10.1136/adc.67.5.657. PMC 1793702. PMID 1599309.
- ^ Ashraf MF, Zubair D, Arain MA (2023). "Nutraceutical and Health-Promoting Potential of Lactoferrin, an Iron-Binding Protein in Human and Animal: Current Knowledge". Biological Trace Element Research. 202 (1): 56–72. doi:10.1007/s12011-023-03658-4. PMC 10104436. PMID 37059920.
- ^ Levin RE, Kalidas S, Gopinadhan P, Pometto A (2006). Food biotechnology. Boca Raton, FL: CRC/Taylor & Francis. p. 1028. ISBN 978-0-8247-5329-0.
- ^ Pursel VG (1998). "Modification of Production Traits". In Clark AJ (ed.). Animal Breeding: Technology for the 21st Century (Modern Genetics). Boca Raton: CRC. p. 191. ISBN 978-90-5702-292-0.
- ^ Ali AS, Hasan SS, Kow CS, Merchant HA (October 2021). "Lactoferrin reduces the risk of respiratory tract infections: A meta-analysis of randomized controlled trials" (PDF). Clinical Nutrition ESPEN. 45: 26–32. doi:10.1016/j.clnesp.2021.08.019. PMID 34620326. S2CID 238475090.
- ^ "Lactoferrin supplements could aid in the recovery of COVID19 & other Respiratory Tract Infections". EurekAlert!. Retrieved 2022-02-18.
- ^ M. Sorensen and S. P. L. Sorensen, Compf. rend. trav. lab. Carlsberg (1939) 23, 55, cited by Groves (1960)
- ^ Groves ML (1960). "The Isolation of a Red Protein from Milk". Journal of the American Chemical Society. 82 (13): 3345. doi:10.1021/ja01498a029.
- ^ a b Johansson B, Virtanen AI, Tweit RC, Dodson RM (1960). "Isolation of an iron-containing red protein from human milk" (PDF). Acta Chem. Scand. 14 (2): 510–512. doi:10.3891/acta.chem.scand.14-0510.
- ^ Naidu AS (2000). Lactoferrin: natural, multifunctional, antimicrobial. Boca Raton: CRC Press. pp. 1–2. ISBN 978-0-8493-0909-0.
- ^ a b Kang JF, Li XL, Zhou RY, Li LH, Feng FJ, Guo XL (June 2008). "Bioinformatics analysis of lactoferrin gene for several species". Biochemical Genetics. 46 (5–6): 312–22. doi:10.1007/s10528-008-9147-9. PMID 18228129. S2CID 952135.
- ^ Seyfert HM, Tuckoricz A, Interthal H, Koczan D, Hobom G (June 1994). "Structure of the bovine lactoferrin-encoding gene and its promoter". Gene. 143 (2): 265–9. doi:10.1016/0378-1119(94)90108-2. PMID 8206385.
- ^ O'Halloran F, Bahar B, Buckley F, O'Sullivan O, Sweeney T, Giblin L (January 2009). "Characterisation of single nucleotide polymorphisms identified in the bovine lactoferrin gene sequences across a range of dairy cow breeds". Biochimie. 91 (1): 68–75. doi:10.1016/j.biochi.2008.05.011. PMID 18554515.
- ^ Birgens HS (April 1985). "Lactoferrin in plasma measured by an ELISA technique: evidence that plasma lactoferrin is an indicator of neutrophil turnover and bone marrow activity in acute leukaemia". Scandinavian Journal of Haematology. 34 (4): 326–31. doi:10.1111/j.1600-0609.1985.tb00757.x. PMID 3858982.
- ^ Baker HM, Anderson BF, Kidd RD, Shewry SC, Baker EN (2000). "Lactoferrin three-dimensional structure: a framework for interpreting function". In Shimazaki K (ed.). Lactoferrin: structure, function, and applications: proceedings of the 4th International Conference on Lactoferrin: Structure, Function, and Applications, held in Sapporo, Japan, 18-22 May 1999. Amsterdam: Elsevier. ISBN 978-0-444-50317-6.
- ^ Baker EN, Baker HM (November 2005). "Molecular structure, binding properties and dynamics of lactoferrin". Cellular and Molecular Life Sciences. 62 (22): 2531–9. doi:10.1007/s00018-005-5368-9. PMC 11139133. PMID 16261257. S2CID 218464085.
- ^ Håkansson A, Zhivotovsky B, Orrenius S, Sabharwal H, Svanborg C (August 1995). "Apoptosis induced by a human milk protein". Proceedings of the National Academy of Sciences of the United States of America. 92 (17): 8064–8. Bibcode:1995PNAS...92.8064H. doi:10.1073/pnas.92.17.8064. PMC 41287. PMID 7644538.
- ^ Jameson GB, Anderson BF, Norris GE, Thomas DH, Baker EN (November 1998). "Structure of human apolactoferrin at 2.0 A resolution. Refinement and analysis of ligand-induced conformational change". Acta Crystallographica Section D. 54 (Pt 6 Pt 2): 1319–35. Bibcode:1998AcCrD..54.1319J. doi:10.1107/S0907444998004417. PMID 10089508.
- ^ Levay PF, Viljoen M (1995). "Lactoferrin: a general review". Haematologica. 80 (3): 252–67. PMID 7672721.
- ^ Mazurier J, Spik G (May 1980). "Comparative study of the iron-binding properties of human transferrins. I. Complete and sequential iron saturation and desaturation of the lactotransferrin". Biochimica et Biophysica Acta. 629 (2): 399–408. doi:10.1016/0304-4165(80)90112-9. PMID 6770907.
- ^ a b Broc JH, De Sousa M (1989). Iron in immunity, cancer, and inflammation. New York: Wiley. ISBN 978-0-471-92150-9.
- ^ Shongwe MS, Smith CA, Ainscough EW, Baker HM, Brodie AM, Baker EN (May 1992). "Anion binding by human lactoferrin: results from crystallographic and physicochemical studies". Biochemistry. 31 (18): 4451–8. doi:10.1021/bi00133a010. PMID 1581301.
- ^ a b c Bennett RM, Davis J (January 1982). "Lactoferrin interacts with deoxyribonucleic acid: a preferential reactivity with double-stranded DNA and dissociation of DNA-anti-DNA complexes". The Journal of Laboratory and Clinical Medicine. 99 (1): 127–38. PMID 6274982.
- ^ Bagby GC, Bennett RM (July 1982). "Feedback regulation of granulopoiesis: polymerization of lactoferrin abrogates its ability to inhibit CSA production". Blood. 60 (1): 108–12. doi:10.1182/blood.V60.1.108.108. PMID 6979357.
- ^ Mantel C, Miyazawa K, Broxmeyer HE (1994). "Physical Characteristics and Polymerization During Iron Saturation of Lactoferrin, A Myelopoietic Regulatory Molecule with Suppressor Activity". Lactoferrin Structure and Function. Advances in, Experimental Medicine and Biology. Vol. 357. pp. 121–32. doi:10.1007/978-1-4615-2548-6_12. ISBN 978-0-306-44734-1. PMID 7762423.
- ^ Furmanski P, Li ZP, Fortuna MB, Swamy CV, Das MR (August 1989). "Multiple molecular forms of human lactoferrin. Identification of a class of lactoferrins that possess ribonuclease activity and lack iron-binding capacity". The Journal of Experimental Medicine. 170 (2): 415–29. doi:10.1084/jem.170.2.415. PMC 2189405. PMID 2754391.
- ^ Adlerova L, Bartoskova A, Faldyna M (2008). "Lactoferrin: a review". Veterinarni Medicina. 53 (9): 457. doi:10.17221/1978-VETMED.
- ^ McCormick JJ, Larson LJ, Rich MA (October 1974). "RNase inhibition of reverse transcriptase activity in human milk". Nature. 251 (5477): 737–40. Bibcode:1974Natur.251..737M. doi:10.1038/251737a0. PMID 4139659. S2CID 4160337.
- ^ Das MR, Padhy LC, Koshy R, Sirsat SM, Rich MA (August 1976). "Human milk samples from different ethnic groups contain RNase that inhibits, and plasma membrane that stimulates, reverse transcription". Nature. 262 (5571): 802–5. Bibcode:1976Natur.262..802D. doi:10.1038/262802a0. PMID 60710. S2CID 4216981.
- ^ Liao Y, Lopez V, Shafizadeh TB, Halsted CH, Lönnerdal B (November 2007). "Cloning of a pig homologue of the human lactoferrin receptor: expression and localization during intestinal maturation in piglets". Comparative Biochemistry and Physiology. Part A, Molecular & Integrative Physiology. 148 (3): 584–90. doi:10.1016/j.cbpa.2007.08.001. PMC 2265088. PMID 17766154.
- ^ Rawat P, Kumar S, Sheokand N, Raje CI, Raje M (June 2012). "The multifunctional glycolytic protein glyceraldehyde-3-phosphate dehydrogenase (GAPDH) is a novel macrophage lactoferrin receptor". Biochemistry and Cell Biology. 90 (3): 329–38. doi:10.1139/o11-058. PMID 22292499.
- ^ Bharadwaj S, Naidu AG, Betageri GV, Prasadarao NV, Naidu AS (September 2009). "Milk ribonuclease-enriched lactoferrin induces positive effects on bone turnover markers in postmenopausal women". Osteoporosis International. 20 (9): 1603–11. doi:10.1007/s00198-009-0839-8. PMID 19172341. S2CID 10711802.
- ^ Bharadwaj S, Naidu TA, Betageri GV, Prasadarao NV, Naidu AS (November 2010). "Inflammatory responses improve with milk ribonuclease-enriched lactoferrin supplementation in postmenopausal women". Inflammation Research. 59 (11): 971–8. doi:10.1007/s00011-010-0211-7. PMID 20473630. S2CID 3180066.
- ^ Rosenmund A, Kuyas C, Haeberli A (November 1986). "Oxidative radioiodination damage to human lactoferrin". The Biochemical Journal. 240 (1): 239–45. doi:10.1042/bj2400239. PMC 1147399. PMID 3827843.
- ^ Levay PF, Viljoen M (January 1995). "Lactoferrin: a general review". Haematologica. 80 (3): 252–67. PMID 7672721.
- ^ a b Farnaud S, Evans RW (November 2003). "Lactoferrin--a multifunctional protein with antimicrobial properties". Molecular Immunology. 40 (7): 395–405. doi:10.1016/S0161-5890(03)00152-4. PMID 14568385.
- ^ Xanthou M (1998). "Immune protection of human milk". Biology of the Neonate. 74 (2): 121–33. doi:10.1159/000014018. PMID 9691154. S2CID 46828227.
- ^ Odell EW, Sarra R, Foxworthy M, Chapple DS, Evans RW (March 1996). "Antibacterial activity of peptides homologous to a loop region in human lactoferrin". FEBS Letters. 382 (1–2): 175–8. doi:10.1016/0014-5793(96)00168-8. PMID 8612745. S2CID 30937106.
- ^ Kuwata H, Yip TT, Yip CL, Tomita M, Hutchens TW (April 1998). "Bactericidal domain of lactoferrin: detection, quantitation, and characterization of lactoferricin in serum by SELDI affinity mass spectrometry". Biochemical and Biophysical Research Communications. 245 (3): 764–73. doi:10.1006/bbrc.1998.8466. PMID 9588189.
- ^ a b c d Sojar HT, Hamada N, Genco RJ (January 1998). "Structures involved in the interaction of Porphyromonas gingivalis fimbriae and human lactoferrin". FEBS Letters. 422 (2): 205–8. doi:10.1016/S0014-5793(98)00002-7. PMID 9490007. S2CID 25875928.
- ^ Andrés MT, Fierro JF (October 2010). "Antimicrobial mechanism of action of transferrins: selective inhibition of H+-ATPase". Antimicrobial Agents and Chemotherapy. 54 (10): 4335–42. doi:10.1128/AAC.01620-09. PMC 2944611. PMID 20625147.
- ^ Jellin JM, Batz F, Hitchens K (2007). Natural Medicines Comprehensive Databas (10th ed.). Therapeutic Research Faculty. p. 915. ISBN 978-0-9788205-3-4.
- ^ a b van der Strate BW, Beljaars L, Molema G, Harmsen MC, Meijer DK (December 2001). "Antiviral activities of lactoferrin". Antiviral Research. 52 (3): 225–239. CiteSeerX 10.1.1.104.745. doi:10.1016/S0166-3542(01)00195-4. PMID 11675140.
- ^ Fujihara T, Hayashi K (1995). "Lactoferrin inhibits herpes simplex virus type-1 (HSV-1) infection to mouse cornea". Archives of Virology. 140 (8): 1469–1472. doi:10.1007/BF01322673. PMID 7661698. S2CID 4396295.
- ^ a b Giansanti F, Rossi P, Massucci MT, Botti D, Antonini G, Valenti P, et al. (2002). "Antiviral activity of ovotransferrin discloses an evolutionary strategy for the defensive activities of lactoferrin". Biochemistry and Cell Biology. 80 (1): 125–130. doi:10.1139/o01-208. PMID 11908636.
- ^ Krzyzowska M, Chodkowski M, Janicka M, Dmowska D, Tomaszewska E, Ranoszek-Soliwoda K, et al. (January 2022). "Lactoferrin-Functionalized Noble Metal Nanoparticles as New Antivirals for HSV-2 Infection". Microorganisms. 10 (1): 110. doi:10.3390/microorganisms10010110. PMC 8780146. PMID 35056558.
- ^ Harmsen MC, Swart PJ, de Béthune MP, Pauwels R, De Clercq E, The TH, et al. (August 1995). "Antiviral effects of plasma and milk proteins: lactoferrin shows potent activity against both human immunodeficiency virus and human cytomegalovirus replication in vitro". The Journal of Infectious Diseases. 172 (2): 380–388. doi:10.1093/infdis/172.2.380. PMID 7622881.
- ^ a b Puddu P, Borghi P, Gessani S, Valenti P, Belardelli F, Seganti L (September 1998). "Antiviral effect of bovine lactoferrin saturated with metal ions on early steps of human immunodeficiency virus type 1 infection". The International Journal of Biochemistry & Cell Biology. 30 (9): 1055–1062. doi:10.1016/S1357-2725(98)00066-1. hdl:11573/83805. PMID 9785469.
- ^ Azzam HS, Goertz C, Fritts M, Jonas WB (February 2007). "Natural products and chronic hepatitis C virus". Liver International. 27 (1): 17–25. doi:10.1111/j.1478-3231.2006.01408.x. PMID 17241377. S2CID 7732075.
- ^ a b c Nozaki A, Ikeda M, Naganuma A, Nakamura T, Inudoh M, Tanaka K, et al. (March 2003). "Identification of a lactoferrin-derived peptide possessing binding activity to hepatitis C virus E2 envelope protein". The Journal of Biological Chemistry. 278 (12): 10162–10173. doi:10.1074/jbc.M207879200. PMID 12522210.
- ^ Arnold D, Di Biase AM, Marchetti M, Pietrantoni A, Valenti P, Seganti L, et al. (February 2002). "Antiadenovirus activity of milk proteins: lactoferrin prevents viral infection". Antiviral Research. 53 (2): 153–158. doi:10.1016/S0166-3542(01)00197-8. hdl:11573/250295. PMID 11750941.
- ^ Carvalho CA, Sousa IP, Silva JL, Oliveira AC, Gonçalves RB, Gomes AM (March 2014). "Inhibition of Mayaro virus infection by bovine lactoferrin". Virology. 452–453: 297–302. doi:10.1016/j.virol.2014.01.022. PMID 24606707.
- ^ Chang R, Ng TB, Sun WZ (September 2020). "Lactoferrin as potential preventative and adjunct treatment for COVID-19". International Journal of Antimicrobial Agents. 56 (3): 106118. doi:10.1016/j.ijantimicag.2020.106118. PMC 7390755. PMID 32738305.
- ^ Wang Y, Wang P, Wang H, Luo Y, Wan L, Jiang M, et al. (December 2020). "Lactoferrin for the treatment of COVID-19 (Review)". Experimental and Therapeutic Medicine. 20 (6): 272. doi:10.3892/etm.2020.9402. PMC 7664603. PMID 33199997.
- ^ Mirabelli C, Wotring JW, Zhang CJ, McCarty SM, Fursmidt R, Pretto CD, et al. (September 2021). "Morphological cell profiling of SARS-CoV-2 infection identifies drug repurposing candidates for COVID-19". Proceedings of the National Academy of Sciences of the United States of America. 118 (36). Bibcode:2021PNAS..11805815M. doi:10.1073/pnas.2105815118. PMC 8433531. PMID 34413211.
- ^ Rosa L, Tripepi G, Naldi E, Aimati M, Santangeli S, Venditto F, et al. (September 2021). "Ambulatory COVID-19 Patients Treated with Lactoferrin as a Supplementary Antiviral Agent: A Preliminary Study". Journal of Clinical Medicine. 10 (18): 4276. doi:10.3390/jcm10184276. PMC 8469309. PMID 34575388.
- ^ Reghunathan R, Jayapal M, Hsu LY, Chng HH, Tai D, Leung BP, et al. (January 2005). "Expression profile of immune response genes in patients with Severe Acute Respiratory Syndrome". BMC Immunology. 6: 2. doi:10.1186/1471-2172-6-2. PMC 546205. PMID 15655079.
- ^ Wakabayashi H, Uchida K, Yamauchi K, Teraguchi S, Hayasawa H, Yamaguchi H (October 2000). "Lactoferrin given in food facilitates dermatophytosis cure in guinea pig models". The Journal of Antimicrobial Chemotherapy. 46 (4): 595–602. doi:10.1093/jac/46.4.595. PMID 11020258.
- ^ a b c Lupetti A, Paulusma-Annema A, Welling MM, Dogterom-Ballering H, Brouwer CP, Senesi S, et al. (January 2003). "Synergistic activity of the N-terminal peptide of human lactoferrin and fluconazole against Candida species". Antimicrobial Agents and Chemotherapy. 47 (1): 262–7. doi:10.1128/AAC.47.1.262-267.2003. PMC 149030. PMID 12499200.
- ^ a b Viejo-Díaz M, Andrés MT, Fierro JF (April 2004). "Modulation of in vitro fungicidal activity of human lactoferrin against Candida albicans by extracellular cation concentration and target cell metabolic activity". Antimicrobial Agents and Chemotherapy. 48 (4): 1242–8. doi:10.1128/AAC.48.4.1242-1248.2004. PMC 375254. PMID 15047526.
- ^ Takakura N, Wakabayashi H, Ishibashi H, Teraguchi S, Tamura Y, Yamaguchi H, et al. (August 2003). "Oral lactoferrin treatment of experimental oral candidiasis in mice". Antimicrobial Agents and Chemotherapy. 47 (8): 2619–23. doi:10.1128/AAC.47.8.2619-2623.2003. PMC 166093. PMID 12878528.
- ^ Masci JR (October 2000). "Complete response of severe, refractory oral candidiasis to mouthwash containing lactoferrin and lysozyme". AIDS. 14 (15): 2403–4. doi:10.1097/00002030-200010200-00023. PMID 11089630.
- ^ Kuipers ME, de Vries HG, Eikelboom MC, Meijer DK, Swart PJ (November 1999). "Synergistic fungistatic effects of lactoferrin in combination with antifungal drugs against clinical Candida isolates". Antimicrobial Agents and Chemotherapy. 43 (11): 2635–41. doi:10.1128/AAC.43.11.2635. PMC 89536. PMID 10543740.
- ^ Andrés MT, Viejo-Díaz M, Fierro JF (November 2008). "Human lactoferrin induces apoptosis-like cell death in Candida albicans: critical role of K+-channel-mediated K+ efflux". Antimicrobial Agents and Chemotherapy. 52 (11): 4081–8. doi:10.1128/AAC.01597-07. PMC 2573133. PMID 18710913.
- ^ Tsuda H, Sekine K, Fujita K, Ligo M (2002). "Cancer prevention by bovine lactoferrin and underlying mechanisms--a review of experimental and clinical studies". Biochemistry and Cell Biology. 80 (1): 131–6. doi:10.1139/o01-239. PMID 11908637.
- ^ a b Chandra Mohan KV, Kumaraguruparan R, Prathiba D, Nagini S (September 2006). "Modulation of xenobiotic-metabolizing enzymes and redox status during chemoprevention of hamster buccal carcinogenesis by bovine lactoferrin". Nutrition. 22 (9): 940–6. doi:10.1016/j.nut.2006.05.017. PMID 16928475.
- ^ Moskwa P, Lorentzen D, Excoffon KJ, Zabner J, McCray PB, Nauseef WM, et al. (January 2007). "A novel host defense system of airways is defective in cystic fibrosis". American Journal of Respiratory and Critical Care Medicine. 175 (2): 174–83. doi:10.1164/rccm.200607-1029OC. PMC 2720149. PMID 17082494.
- ^ Singh PK, Schaefer AL, Parsek MR, Moninger TO, Welsh MJ, Greenberg EP (October 2000). "Quorum-sensing signals indicate that cystic fibrosis lungs are infected with bacterial biofilms". Nature. 407 (6805): 762–4. Bibcode:2000Natur.407..762S. doi:10.1038/35037627. PMID 11048725. S2CID 4372096.
- ^ Singh PK, Parsek MR, Greenberg EP, Welsh MJ (May 2002). "A component of innate immunity prevents bacterial biofilm development". Nature. 417 (6888): 552–5. Bibcode:2002Natur.417..552S. doi:10.1038/417552a. PMID 12037568. S2CID 4423528.
- ^ Rogan MP, Taggart CC, Greene CM, Murphy PG, O'Neill SJ, McElvaney NG (October 2004). "Loss of microbicidal activity and increased formation of biofilm due to decreased lactoferrin activity in patients with cystic fibrosis". The Journal of Infectious Diseases. 190 (7): 1245–53. doi:10.1086/423821. PMID 15346334.
- ^ Andrés MT, Viejo-Diaz M, Pérez F, Fierro JF (April 2005). "Antibiotic tolerance induced by lactoferrin in clinical Pseudomonas aeruginosa isolates from cystic fibrosis patients". Antimicrobial Agents and Chemotherapy. 49 (4): 1613–6. doi:10.1128/aac.49.4.1613-1616.2005. PMC 1068597. PMID 15793153.
- ^ Rogan MP, Geraghty P, Greene CM, O'Neill SJ, Taggart CC, McElvaney NG (February 2006). "Antimicrobial proteins and polypeptides in pulmonary innate defence". Respiratory Research. 7 (1): 29. doi:10.1186/1465-9921-7-29. PMC 1386663. PMID 16503962.
- ^ "Public summary of positive opinion for orphan designation of hypothiocyanite/lactoferrin for the treatment of cystic fibrosis" (PDF). Pre-authorisation Evaluation of Medicines for Human Use. European Medicines Agency. 2009-09-07. Archived from the original (PDF) on 2010-05-30. Retrieved 2010-01-23.
- ^ "Meveol: orphan drug status granted by the FDA for the treatment of cystic fibrosis". United States Food and Drug Administration. 2009-11-05. Archived from the original on 2009-12-24. Retrieved 2010-01-23.
- ^ Pammi M, Suresh G (March 2020). "Enteral lactoferrin supplementation for prevention of sepsis and necrotizing enterocolitis in preterm infants". The Cochrane Database of Systematic Reviews. 3 (3): CD007137. doi:10.1002/14651858.CD007137.pub6. PMC 7106972. PMID 32232984.
- ^ Ohashi Y, Ishida R, Kojima T, Goto E, Matsumoto Y, Watanabe K, et al. (August 2003). "Abnormal protein profiles in tears with dry eye syndrome". American Journal of Ophthalmology. 136 (2): 291–9. doi:10.1016/S0002-9394(03)00203-4. PMID 12888052.
- ^ Karns K, Herr AE (November 2011). "Human tear protein analysis enabled by an alkaline microfluidic homogeneous immunoassay". Analytical Chemistry. 83 (21): 8115–22. doi:10.1021/ac202061v. PMID 21910436.
- ^ Cui S, Lv X, Sun G, Wu W, Xu H, Li Y, et al. (2022). "Recent advances and prospects in purification and heterologous expression of lactoferrin". Food Bioengineering. 1: 58–67. doi:10.1002/fbe2.12003.
- ^ Xavier PL, Chaudhari K, Verma PK, Pal SK, Pradeep T (December 2010). "Luminescent quantum clusters of gold in transferrin family protein, lactoferrin exhibiting FRET" (PDF). Nanoscale. 2 (12): 2769–76. Bibcode:2010Nanos...2.2769X. doi:10.1039/C0NR00377H. PMID 20882247.
External links
edit- Uniprot
- LTF on the National Center for Biotechnology Information
- FDA Lactoferrin Considered Safe to Fight E. Coli.