Original article
S W I S S M E D W K LY 2 0 0 6 ; 1 3 6 : 8 0 5 – 8 1 0 · w w w . s m w . c h
805
Peer reviewed article
Recurrent hypoglycaemia
in HIV-positive narcotic addicts
Peter Wieslia,f, Vojtech Pavliceka, Aurel Perrenb, Esther Baechlic, Thomas Pfammatterd, Lukas Krahenbuhle,
Georg Schulthessc, Christoph Schmida
a
b
c
d
e
f
Department of Internal Medicine, Division of Endocrinology and Diabetes,
University Hospital of Zürich, Switzerland
Department of Pathology, University Hospital of Zürich, Switzerland
Department of Internal Medicine, University Hospital of Zürich, Switzerland
Department of Radiology, University Hospital of Zürich, Switzerland
Department of Visceral and Transplantation Surgery, University Hospital of Zürich, Switzerland
Department of Internal Medicine, Division of Endocrinology and Diabetes,
Kantonsspital Frauenfeld, Switzerland
Summary
Questions under study: We describe two narcotic
addict women with recurrent hypoglycaemic
episodes. In both patients, hyperinsulinaemic hypoglycaemia occurring in the fasting state was
documented and computed tomography of the
pancreas was normal.
Methods and Results: In patient 1, selective arterial calcium stimulation with hepatic venous
sampling (ASVS) revealed pronounced insulin
hypersecretion predominantly in the tail and, to a
lesser extent, in the corpus and the head of the pancreas. On laparoscopic exploration, tumours could
not be detected be it grossly or by intraoperative
ultrasound. Distal pancreatectomy was performed
laparoscopically, and histological examination of
the resected tissue revealed nesidioblastosis. ASVS
was also performed in patient 2 revealing less
marked increases in insulin secretion, ie up to 2.3fold in response to calcium stimulation of the superior mesenteric artery, consistent with the pres-
ence of pathological β-cells located predominantly
in the head of the pancreas. Surgical exploration
was not performed in this patient.
Conclusion: HIV infection had been known in
both women for around ten years and both patients
were not on antiretroviral therapy. Because symptomatic nesidioblastosis in adult patients is a very
rare disorder, we speculate that nesidioblastosis
may develop in the context of HIV infection
and/or abuse of narcotic drugs. Our observations
illustrate that neurocognitive impairment in HIVpositive patients is not always due to toxic compounds or a cerebral disorder but may be caused
by an apparently rare pancreatic disorder, nesidioblastosis. Thus, the patients should be checked for
the presence of hyperinsulinaemic hypoglycaemia.
Key words: nesidioblastosis; hypoglycaemia; insulin;
HIV; drug addict
Introduction
No financial
support declared.
Loss of consciousness may occur due to intoxication with various drugs and often requires admittance to an intensive care unit. Detailed history
of the patient is often missing and, therefore, careful physical examinations as well as monitoring of
vital functions and crucial laboratory parameters
are indispensable. Description of the circumstances under which the patient was found may
be helpful and additional information regarding
the patient’s history can occasionally be obtained
from friends or relatives. If the patient is an addict,
administration of an overdose of narcotics is a
probable cause of unconsciousness. Nevertheless,
it is crucial to look for hints, signs, and symptoms
indicating further disorders underlying unconsciousness such as head injury, cerebral bleeding,
infectious disease, or endocrine disorders. Hypoglycaemia, for instance, may be life threatening if
not detected early and treated appropriately.
�806
Fasting hypoglycaemia in narcotic addicts
Material and methods
Laboratory investigations
For the determination of plasma glucose, venous
blood samples were drawn into sodium-fluoride containing tubes. Plasma glucose was determined by the glucose
oxidase technique (Beckman Analyzer; Beckman, Fullerton, CA). Immunoreactive insulin was measured by solidphase radioimmunoassay (intra-assay coefficient of variation (CV) 5%, inter-assay CV 4.9%, lower limit of detection, 14 pmol/l) (Coat-A-Count Insulin; DPC, Los Angeles, CA). Measurement of C-peptide was performed with
a solid-phase, chemoluminescent enzyme immunoassay
(intra-assay CV 6.3%, inter-assay CV 6.3%, lower limit
of detection, 12 pmol/l) (Immulite C-peptide; DPC, Los
Angeles, CA; [1,2]).
First and second generation sulfonylureas were measured in plasma by gas chromatographic mass spectroscopy
and liquid chromatographic mass spectroscopy, respectively. b-hydroxybutyrate, cortisol, and ACTH were determined at the Institute of Clinical Chemistry of the University Hospital of Zürich by standard methods.
Selective arterial calcium stimulation with hepatic
venous sampling (ASVS)
The procedure was performed as previously described with some modifications according to the variant
arterial pancreatic anatomy [3–5]. A sampling catheter
(Cobra, 6 French) was placed transfemorally in the right
hepatic vein close to its junction with the inferior vena
cava. Selective arterial angiography and stimulation was
performed via a percutaneous femoral access with a 5
French visceral catheter and a coaxial 3 French catheter
(for the PDA and PTA). Each artery was stimulated with
calcium gluconate (0.025 milliequivalents Ca++ per kg
body weight). Blood was collected from the left hepatic
vein before (= 0), 30, 60 and 120 seconds after the intraarterial injection of calcium. At least 5 minutes lapsed between each calcium injection. The SA supplies primarily
the body and tail of the pancreas, the GDA supplies the
head and secondarily the uncinate, the SMA supplies the
uncinate and secondarily the pancreatic head. The PDA
artery in patient 1 supplied the whole pancreas after contrast administration. A more than 2-fold increase in insulin
levels as assessed by RIA [2] within 30–120 seconds after
the injection of calcium indicates the localisation of an insulin secreting tumour in the vascular territory of the stimulated artery (in contrast to no response from normal
b-cells; [2-5]).
Pathology
The resected pancreatic tissue from patient 1 was systematically sectioned into 1 mm slices, fixed in buffered
formalin, and embedded in paraffin. 4 mm thick paraffin
sections were immunostained using the avidin-biotinperoxidase technique with diaminobenzidine as peroxidase substrate (Vectastain ABC-kit, Vector Laboratories,
Burlingame, CA, U.S.A.) with nickel cobalt amplification
as previously described [6]. The primary antibodies were
directed against chromogranin A (1:1000, Boehringer
Mannheim, Mannheim, Germany), glucagon (1:250,
DAKO, Glostrup, Denmark), insulin (Bio-Genex, San
Ramon, CA, U.S.A), alpha-HCG (1:50, Seralab, Crawley Down, Sussex, GB), somatostatin (1:300, DAKO),
pancreatic polypeptide (1:60 000, Chance, Indianapolis,
U.S.A.), gastrin (1:200, DAKO), and substance P (1:3000,
Seralab).
Results
Case 1
A 35-year old woman was admitted because
of intoxication in a suicidal attempt with 4 g
methadone, 0.5 g sertraline, and an unknown
amount of oxazepame. She was known as a narcotic
addict and had witnessed the suicide of her partner a few hours before. She had a history of drug
abuse for several years and, participating in a program, received 130 mg methadone daily. Occasionally, she consumed additional drugs such as
benzodiazepines, heroin and cocaine. She was
known to be HIV-positive (CDC A2) but had
refused to take antiretroviral medications. She
had medroxyprogesterone injections every three
months for contraception.
On admission, the patient had impaired consciousness (Glasgow Coma Scale 13) and became
unconscious a few minutes after admittance. Blood
pressure was 90/60 mm Hg, pulse rate 76 beats/
min, and respiration rate 12/min. Consciousness
of the patient could not be improved by repetitive
administration of naloxone and flumazenile. Initial
laboratory evaluations were normal except for a
venous plasma glucose concentration of 1.7 mmol/
L. Glucose was infused but had no effect on
her mental state. Drug screening was positive for
methadone, opiates, and benzodiazepines. Screening for alcohol, cocaine, and barbiturates was negative. β-hydroxybutyrate concentration was as low
as 1 µmol/L.
When glucose infusion was stopped after two
days for 4 hours plasma glucose concentration
dropped to 2.3 mmol/L. Plasma insulin concentration was 137 pmol/L and the C-peptide level
was 950 pmol/L at that time. Plasma sulfonylurea
screen was negative for first and second generation
sulfonylureas, insulin antibodies were not detectable. These results suggested endogenous hyperinsulinaemic hypoglycaemia. A plasma cortisol
level of 47 nmol/L and a repeated plasma cortisol
level of 43 nmol/L the next morning (at 8.00 a.m.,
reference 280–690 nmol/L) indicated glucocorticoid deficiency. ACTH concentration was <10 ng/L
(normal <46) and plasma cortisol increased to
615 nmol/L following injection of 250 µg corticotropin. A diagnosis of acute secondary adrenocortical insufficiency was made. Seven days after
admission, plasma cortisol level at 7.30 a.m. was
420 nmol/L and increased to 630 nmol/L following
intravenous injection of 250 µg corticotropin,
suggesting that the hypothalamic-pituitary-adrenocortical (HPA)-axis returned towards normal.
�S W I S S M E D W K LY 2 0 0 6 ; 1 3 6 : 8 0 5 – 8 1 0 · w w w . s m w . c h
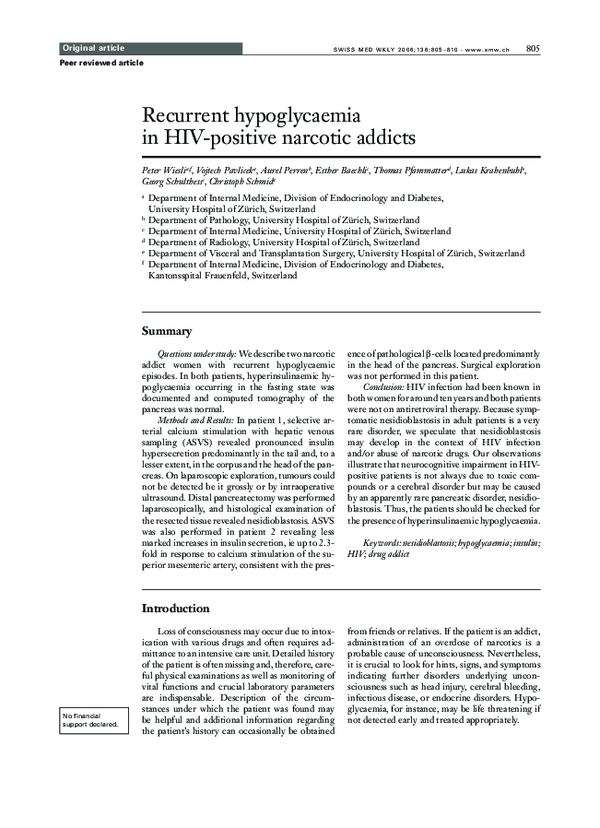
Figure 1
Insulin in the hepatic vein
(as a multiple of basal)
8
6
30 sec
4
60 sec
120 sec
2
0
PHA
SMA
A
GDA
PTA
PDA
SA
Artery stimulated
2.5
Insulin in the hepatic vein
(as a multiple of basal)
A: Selective arterial
calcium stimulation
test in patient 1.
Insulin levels in the
left hepatic vein as a
multiple of basal, 30,
60 and 120 seconds
after the intra-arterial
injection of calcium
(0.025 mEq Ca++ per
kg body weight) into
the proper hepatic
artery (PHA), superior mesenteric artery
(SMA), gastroduodenal artery (GDA),
transverse pancreatic
artery (PTA), dorsal
pancreatic artery
(PDA), and splenic
artery (SA). A 2-fold
and more increase in
the insulin level in
the hepatic vein indicates pathologic insulin-secreting cells
in the arterial distribution of SA and
PDA, less pronounced in GDA and
PTA. No significant
increase in insulin
levels is seen after
calcium injection into
the SMA and PHA.
B: Selective arterial
calcium stimulation
test in patient 2.
Insulin levels in the
left hepatic vein as a
multiple of basal, 30,
60 and 120 seconds
after the intra-arterial
injection of calcium
into the right hepatic
artery (RHA), superior mesenteric artery
(SMA), gastroduodenal artery (GDA) and
splenic artery (SA).
A 2.3-fold increase
in the insulin level in
the hepatic vein indicates pathologic insulin-secreting cells
in the arterial distribution of SMA. A
1.9-fold increase of
insulin levels is seen
after calcium injection into the SA,
RHA and a 1.6-fold
increase after injection into the GDA.
807
2
1.5
30 sec
60 sec
120 sec
1
0.5
0
RHA
B
SMA
GDA
SA
Artery stimulated
Consciousness of the patient continuously improved over the next three days corresponding to
the half-life of the enormous amount of methadone
ingested.
A more detailed history could then be obtained. The patient complained that she had experienced several episodes of unconsciousness
associated with tremor and sweating during the
preceding year. These symptoms were attributed
to the drug abuse rather than food ingestion or
deprivation. In the five years preceding this hospitalisation seizures occasionally occurred. Benzodiapezine withdrawal was assumed as the underlying
reason for the seizures. Reviewing her medical
records, a plasma glucose concentration of 2.9
mmol/L was noted ten months prior to admission.
This sample was drawn in a sodium fluoride-containing tube at a routine control. Family history
was negative for any endocrine disorder. We suspected a hypoglycaemic disorder with relative hyperinsulinaemia during hypoglycaemia and performed a 72-hour fast for further evaluation (table
1). After 48 hours the patient became disorientated
and somnolent. Plasma glucose concentration
was 1.8 mmol/L, and the neuroglycopenic symptoms resolved immediately when glucose was administrated intravenously. At termination of the
fast, plasma insulin concentration was 69 pmol/L
and C-peptide level was 230 pmol/L. Sulfonylurea screen was negative and β-hydroxybutyrate
concentration was 741 µmol/L (reference for
healthy individuals at the end of a prolonged fast:
>2500 µmol/L; [1]).
These results were indicative of an insulinoma.
However, no tumour in the pancreas could be
detected by contrast-enhanced multi-row spiral
computed tomography scanning or by contrastenhanced magnetic resonance imaging. Selective
arterial calcium stimulation with hepatic venous
sampling (ASVS) was performed. In the digital
subtraction angiography no hypervascular lesion
in the pancreas was detected. The standard stimulation scheme had to be changed according to the
variant arterial supply of the pancreas. The following arteries were stimulated: the gastro-duodenal
artery (GDA), the proper hepatic artery (PHA),
the splenic artery (SA), the superior mesenteric artery (SMA), the dorsal pancreatic artery (PDA) and
the transverse pancreatic artery (PTA). No increase of insulin concentration was measured after
stimulation of the PHA and SMA. In contrast, a
more than two-fold hepatic venous insulin increase was found after stimulation of the GDA,
PTA, PDA, and SA (figure 1A). This indicated that
abnormal β-cells were predominantly located in
the tail and, to a lesser extent, in the body and head
of the pancreas. Such a distribution of abnormal
β-cells may be encountered in patients with multiple insulinomas or nesidioblastosis.
The patient underwent laparoscopic exploration of the pancreas. The body and tail of the
pancreas were mobilised from their peritoneal end
retroperitoneal attachments. However, an insulinoma could not be detected either grossly or by intraoperative ultrasound examination. Considering
the results of ASVS, distal pancreatectomy of a
�Fasting hypoglycaemia in narcotic addicts
808
Figure 2
t
Pathology findings
A. Insulin staining,
original magnification 25҂: increased
number of islets of
Langerhans of varying size.
B. Synaptophysin,
original magnification 200҂: numerous
ductuloinsular complexes. Note intimate
apposition of ductules (ÿ) with synaptophysin-positive
neuroendocrine cells.
C. H&E staining,
original magnification 400҂: individual
neuroendocrine cells
have enlarged nuclei
( ).
D. Insulin staining,
original magnification 200҂: islets with
irregular, ragged border. Note individual
cells with enlarged
nuclei staining for
insulin ( ).
t
specimen measuring 9 ҂ 5 ҂ 3 cm was performed.
The postoperative course was uneventful and glucose levels remained within the normal range.
Histological examination of the pancreatic tissue was characteristic for nesidioblastosis. Most
strikingly, the number of islets of Langerhans was
increased. Their size and shape was very variable,
with individual hypertrophic islets measuring up
to 1.5 mm (figure 2A). The islets contained large
cells with enlarged pleomorphic nuclei. Focally,
islet cells budding from ducts (ductuloinsular complexes) were noted (figure 2B and 2C). Immunohistochemically, the islets contained all major islet
cell types staining for insulin, glucagon, somatostatin and pancreatic polypeptide. The distribution of endocrine cell types was normal with the
majority of cells staining for insulin and a peripheral ring of glucagon positive cells. Individual cells
with hyperchromatic nuclei could be identified as
β-cells.
A prolonged fast was repeated three weeks
after surgery. No neuroglycopenic symptoms
were observed during a 72-hour fast. At the end
of the fast, plasma glucose concentration was
3.4 mmol/L in association with an insulin concentration of 101 pmol/L, a C-peptide concentration
of 310 pmol/L and a β-hydroxybutyrate concentration of 689 µmol/L. During 4 years follow-up,
neither diabetes mellitus nor exocrine pancreatic
insufficiency occurred in this patient. No episodes
of unconsciousness associated with sweating or
seizures were observed any more.
Case 2
A 31-year-old woman was admitted because
of osteomyelitis of the right tibia in March 2004.
She had several blood glucose readings below
3 mmol/L and she also had a history of narcotic
drug and alcohol abuse for several years and,
participating in a program, received 400 mg
methadone daily. She consumed 1 bottle of vodka
and up to three litres of beer a day and occasion-
ally additional drugs such as benzodiazepines,
heroin and cocaine. She was known to be HIVpositive (CDC A2), and antiretroviral therapy was
not feasible due to malcompliance.
Previous history revealed no loss of consciousness, but massive alcohol consumption. The patient did not consent to a prolonged fast but only
to a continuously supervised overnight fast of 5
hours. Fasting plasma glucose concentration was
1.7 mmol/L with a corresponding plasma insulin
concentration of 85 pmol/L and C-peptide level of
580 pmol/L, but at that time she suffered from prerenal renal failure (creatinine 226 µmol/l). This
fast was suggestive but not diagnostic for hyperinsulinaemic hypoglycaemia. She refused further
evaluation of her low blood glucose readings and
left the hospital. One year and 3 month later she
was admitted again with unconsciousness. Cerebral computed tomography was normal. Initial
laboratory evaluations revealed a plasma glucose
concentration of 1.5 mol/L, plasma alcohol was
55 mmol/L, renal function was normal (creatinine
76 umol/L). An overnight fast (6 hours) was performed again and morning plasma glucose level
was 2 mmol/L, insulin 172 pmol/L and C-peptide
1040 pmol/L. After the overnight fast the patient
insisted to leave the hospital again. One month
later she was admitted to a psychiatric clinic for an
alcohol withdrawal program and was then willing
to have a further evaluation of her hypoglycaemic
disorder. A fast was started and stopped after
11 hours because plasma glucose concentration
fell to 1.9 mmol/L. At this time plasma insulin concentration was 149 pmol/L and C-peptide level
was 860 pmol/L. Sulfonylurea screen was negative
and β-hydroxybutyrate was 246 µmol/L (table 1).
Mental status could not be assessed due to benzodiazepine sedation because of craving.
These results suggested again endogenous
hyperinsulinaemic hypoglycaemia.
Medical records of the past few years revealed
that she suffered from several seizures and episodes
�S W I S S M E D W K LY 2 0 0 6 ; 1 3 6 : 8 0 5 – 8 1 0 · w w w . s m w . c h
Table 1
Laboratory values
and symptoms after
48 hours (patient 1)
and 11 hours (patient 2)
at the end of fasting Screening for sulfonylurea in plasma
was negative in both
patients.
Patient
Glucose
(mmol/l)
1
1.8
2
1.9
Insulin
(pmol/l
C-peptide
(pmol/l)
b-hydroxybutyrate
mmol/l)
(m
Mental status
69
230
741
Confusion
149
860
246
not applicable
of unconsciousness. These symptoms were attributed to drug withdrawal or intoxication. In retrospect, as in case 1, these results were indicative for
insulinoma. However, no tumour in the pancreas
could be detected by contrast-enhanced multi-row
spiral computed tomography scanning. ASVS was
performed. In the digital subtraction angiography
no hypervascular lesion was detected in the pancreas. The following arteries were stimulated: the
gastro-duodenal artery (GDA), the right hepatic
artery (RHA), the splenic artery (SA), and the superior mesenteric artery (SMA). A 2.3-fold hepatic
venous insulin increase was found after stimulation
of the SMA, and minor increases after stimulation
809
of the GDA, RHA and SA (figure 1B). This suggested that abnormal β-cells were predominantly
located in the head and, possibly to a lesser extent,
in the body and tail of the pancreas. Taken together, the negative findings by CT and angiography in a patient with hyperinsulinaemic hypoglycaemia and the current pattern in ASVS indicate a
distribution of abnormal β-cells which is consistent with nesidioblastosis.
A surgical exploration of the pancreas has not
yet been possible in this patient. After alcohol
withdrawal and regular carbohydrate supply, her
blood glucose concentrations were relatively stable in a low normal range.
Discussion
Neuroglycopenia must be considered in any
patient with impaired consciousness, even if there
seems to be an obvious explanation for loss of consciousness as it was in the presented cases. As soon
as hypoglycaemia is detected, further evaluation is
based on the clinical characteristics of the individual patient. Hypoglycaemia in the context of an intoxication of a narcotic and/or alcohol addict HIVpositive patient warrants special considerations.
First, changes in mental status [7], a cornerstone in
the diagnosis of hypoglycaemia as pointed out by
Whipple may be difficult to attribute to hypoglycaemia; second, adherence and consent to standard
medical testing and care may not be feasible. An
acute intoxication with methadone, sertraline and
oxazepame is usually not associated with hypoglycaemia. In contrast, alcohol intoxication associated
with hepatic, renal or endocrine disorders may lead
to hypoglycaemia. The co-administration of compounds such as insulin or sulfonylureas was excluded
by determining insulin, C-peptide and sulfonylurea
during hypoglycaemic episodes. Despite the patients being HIV-positive, no HIV-associated illness that could prompt hypoglycaemia was known
(including hepatic, renal or endocrine disorders).
Drugs with glucose-lowering properties including
pentamidine or trimethoprim-sulfamethoxazole
had not been prescribed.
It is important to note that marked secondary
adrenal insufficiency (as documented in patient 1 on
admission) and alcohol abuse (a problem in patient
2) may cause hypoglycaemia, however, not associated with inappropriately high insulin or C-peptide
levels; insulin secretion by healthy b-cells should be
suppressed. The occurrence of hyperinsulinaemic
hypoglycaemia during the prolonged fast is considered as a clinical hallmark of patients with insulinoma [8]. Small insulinomas may not be localised
by pancreatic imaging [9]. Therefore, ASVS is an
appropriate investigation to localise an insulinoma
[3–5, 9, 10]. A positive response to calcium stimulation in multiple vascular territories of the pancreas
is uncommon and points to the presence of multiple insulinomas or nesidioblastosis [4, 11]. Multiple
insulinomas are found almost exclusively in patients
with MEN-1 syndrome. MEN-1 was unlikely in
our patients since family history was negative and
calcium serum levels were normal. Moreover, a
germline mutation in the exons 2–10 of the meningene in patient 1 could not be found. Thus, nesidioblastosis of the pancreas was assumed, a diagnosis
which can only be confirmed histopathologically
[12].
Because of the diffuse nature of the islet-cell disease, the extent of surgical resection in patients with
nesidioblastosis is controversial. Most experts recommend distal resection of the pancreas in adult patients with nesidioblastosis [11]. ASVS allows localisation of the distribution of abnormal β-cells and
performance of a gradient-guided pancreatectomy.
In patient 1 described here, ASVS disclosed abnormal β-cells predominantly in the tail and to a lesser
extent in the body and head of the pancreas. Thus,
distal pancreatectomy to the right of the mesenteric
vein was performed laparoscopically.
In patient 2 the results of the ASVS test disclosed abnormal β-cells predominantly in the head
of the pancreas. This finding would be in agreement
with an insulinoma in the vascular territory of the
mesenteric superior artery. However, because of the
marginally pathological increases in insulin after
calcium injection into the pancreas-supplying arteries, we believe that nesidioblastosis, predominantly
in the head (2.3-fold increase) and to a lesser extent
in the tail of the pancreas (1.9-fold increase) should
be considered. The normal CT scan and the nega-
�810
Fasting hypoglycaemia in narcotic addicts
tive angiographic findings (no blush) support (but
do not prove) this hypothesis.
Symptomatic nesidioblastosis in adult patients
has been considered as a very rare disorder. Nesidioblastosis has been well described in infants with
persistent severe hypoglycaemia. In some of these
patients, mutations of the SUR1 (sulfonylurea receptor) or Kir 6.2 (inwardly rectifying potassium
channel) genes have been detected. In adult patients
with nesidioblastosis, such mutations were not detected [13]. Only in more recent years case series of
(acquired) nesidoblastosis have been reported in
adults, either idiopathic [11] or following surgery
for super obesity [14]. In these patients, hypoglycaemia occurred predominantly in the late postprandial period; and at least in the latter, b-cells hyperplasia could reflect an adaptation to an increased
demand with subsequent loss of b-cell control. Our
patients were not obese and had no history of upper
gastro-intestinal surgery. Thus, there was no specific reason to suspect that preceding severe insulin
resistance or changes in incretins could account for
β-cell pathology.
A recent pathological study suggested that islet
hyperplasia may be more frequent in adults suffering from hyperinsulinaemic hypoglycaemia than
previously thought and could account for about one
fifth of the cases. In this series, no information was
given as to whether hypoglycaemia occurred in the
postprandial or in the fasting state [15].
In our patients, the condition appears to be
rather unique in that they suffered from fasting
hypoglycaemia. Two additional patients seen at our
institution over the past 5 years with histologically
confirmed islet hyperplasia (not known for drug
abuse and HIV infection) suffered predominantly
from postprandial hypoglycaemia. Remarkably,
proinsulin levels at the end of the fast (ie in the state
of hyperinsulinaemic hypoglycaemia) were in the
low normal range of healthy fasting individuals [1],
consistent with normal insulin processing by hyperplastic islets of our two patients (as previously reported for one of them; [16]).
Earlier described cases in the U.S. by the Mayo
Clinic [12, 14] and by pathologists in Germany [15],
revealed no aetiology. It may well be that the occurrence of hyperinsulaemic hyperglycaemia in our
two patients with long-lasting narcotic drug abuse
and HIV infection occurred by chance and was a coincidence; a link between nesidioblastosis and HIV
infection and/or abuse of narcotic drugs is difficult
to test for such a rare (apparently acquired) hypoglycaemic disorder.
We suggest that HIV-positive patients with
neuroglycopenic symptoms should be checked for
the presence of hypoglycaemia.
Correspondence:
Christoph Schmid, MD
Department of Internal Medicine
Division of Endocrinology and Diabetes
University Hospital of Zürich
CH-8091 Zürich
E-Mail: christoph.schmid@usz.ch
References
1 Wiesli P, Brandle M, Zapf J, Seiler H, Zwimpfer C, Spinas GA,
et al. Assessment of hyperinsulinaemia at the termination of the
prolonged fast. Clin Chim Acta. 2004;342:227–31.
2 Wiesli P, Brandle M, Pfammatter T, Zapf J, Spinas GA, Schmid
C. Insulin determination by specific and unspecific immunoassays in patients with insulinoma evaluated by the arterial stimulation and venous sampling test. Eur J Endocrinol. 2004;151:
123–6.
3 Doppman JL, Miller DL, Chang R, Gorden P, Eastman RC,
Norton JA. Intraarterial calcium stimulation test for detection
of insulinomas. World J Surg. 1993;17:439–43.
4 Wiesli P, Brandle M, Schmid C, Krahenbuhl L, Furrer J, Keller
U, et al. Selective arterial calcium stimulation and hepatic venous sampling in the evaluation of hyperinsulinemic hypoglycemia: potential and limitations. J Vasc Interv Radiol.
2004;15:1251–6.
5 Brandle M, Pfammatter T, Spinas GA, Lehmann R, Schmid C.
Assessment of selective arterial calcium stimulation and hepatic
venous sampling to localize insulin-secreting tumours. Clin Endocrinol. 2001;55:357–62.
6 Komminoth P, Roth J, Saremaslani P, Matias-Guiu X, Wolfe
HJ, Heitz PU. Polysialic acid of the neural cell adhesion molecule in the human thyroid: a marker for medullary thyroid carcinoma and primary C-cell hyperplasia. An immunohistochemical study on 79 thyroid lesions. Am J Surg Pathol. 1994;
18:399–411.
7 Wiesli P, Schwegler B, Schmid B, Spinas GA, Schmid Ch. MiniMental State Examination is superior to plasma glucose concentrations in monitoring patients with suspected hypoglycaemic
disorders during the 72-hour fast. Eur J Endocrinol. 2005;152:
605–10.
8 Service FJ. Hypoglycemic disorders. N Engl J Med. 1995;332:
1144–52.
9 Norton JA, Shawker TH, Doppman JL, Miller DL, Fraker DL,
Cromack DT. Localization and surgical treatment of occult
insulinomas. Ann Surg. 1990;212:615–20.
10 Doppman JL, Chang R, Fraker DL, Norton JA, Alexander HR,
Miller DL, et al. Localization of insulinomas to regions of the
pancreas by intra- arterial stimulation with calcium. Ann Intern
Med. 1995;123:269–73.
11 Thompson GB, Service FJ, Andrews JC, Lloyd RV, Natt N, van
Heerden JA, et al. Noninsulinoma pancreatogenous hypoglycemia syndrome: an update in 10 surgically treated patients.
Surgery. 2000;128:937–44.
12 Harrison TS, Fajans SS, Floyd JC Jr., Thompson NW, Rasbach
DA, Santen RJ, et al. Prevalence of diffuse pancreatic beta islet
cell disease with hyperinsulinism: problems in recognition and
management. World J Surg. 1984;8:583–9.
13 Service FJ, Natt N, Thompson GB, Grant CS, van Heerden JA,
Andrews JC, et al. Noninsulinoma pancreatogenous hypoglycemia: a novel syndrome of hyperinsulinemic hypoglycemia
in adults independent of mutations in Kir6.2 and SUR1 genes.
J Clin Endocrinol Metab. 1999;84:1582–9.
14 Service GJ, Thompson GB, Service FJ, Andrews JC, CollazoClavell ML, et al. Hyperinsulinemic hypoglycemia with nesidioblastosis after gastric-bypass surgery. N Engl J Med. 2005;
353:249–54.
15 Anlauf M, Wieben D, Perren A, Sipos B, Komminoth P, Raffel
A, et al. Persistent hyperinsulinemic hypoglycemia in 15 adults
with diffuse nesidioblastosis: diagnostic criteria, incidence, and
characterization of beta-cell changes. Am J Surg Pathos. 2005;
29:524–33.
16 Wiesli P, Perren A, Saremaslani P, Pfammatter T, Spinas GA,
Schmid C. Abnormalities of proinsulin processing in functioning insulinomas: clinical implications. Clin Endocrinol. 2004;
61:424–30.
�Swiss
Medical Weekly
Swiss Medical Weekly: Call for papers
Official journal of
the Swiss Society of Infectious disease
the Swiss Society of Internal Medicine
the Swiss Respiratory Society
The many reasons why you should
choose SMW to publish your research
What Swiss Medical Weekly has to offer:
•
•
•
•
•
•
•
•
•
•
•
•
SMW’s impact factor has been steadily
rising, to the current 1.537
Open access to the publication via
the Internet, therefore wide audience
and impact
Rapid listing in Medline
LinkOut-button from PubMed
with link to the full text
website http://www.smw.ch (direct link
from each SMW record in PubMed)
No-nonsense submission – you submit
a single copy of your manuscript by
e-mail attachment
Peer review based on a broad spectrum
of international academic referees
Assistance of our professional statistician
for every article with statistical analyses
Fast peer review, by e-mail exchange with
the referees
Prompt decisions based on weekly conferences of the Editorial Board
Prompt notification on the status of your
manuscript by e-mail
Professional English copy editing
No page charges and attractive colour
offprints at no extra cost
Editorial Board
Prof. Jean-Michel Dayer, Geneva
Prof. Peter Gehr, Berne
Prof. André P. Perruchoud, Basel
Prof. Andreas Schaffner, Zurich
(Editor in chief)
Prof. Werner Straub, Berne
Prof. Ludwig von Segesser, Lausanne
International Advisory Committee
Prof. K. E. Juhani Airaksinen, Turku, Finland
Prof. Anthony Bayes de Luna, Barcelona, Spain
Prof. Hubert E. Blum, Freiburg, Germany
Prof. Walter E. Haefeli, Heidelberg, Germany
Prof. Nino Kuenzli, Los Angeles, USA
Prof. René Lutter, Amsterdam,
The Netherlands
Prof. Claude Martin, Marseille, France
Prof. Josef Patsch, Innsbruck, Austria
Prof. Luigi Tavazzi, Pavia, Italy
We evaluate manuscripts of broad clinical
interest from all specialities, including experimental medicine and clinical investigation.
We look forward to receiving your paper!
Guidelines for authors:
http://www.smw.ch/set_authors.html
Impact factor Swiss Medical Weekly
2
1.8
1.537
1.6
E ditores M edicorum H elveticorum
1.4
1.162
1.2
All manuscripts should be sent in electronic form, to:
1
0.770
0.8
0.6
0.4
Schweiz Med Wochenschr (1871–2000)
Swiss Med Wkly (continues Schweiz Med Wochenschr from 2001)
2004
2003
2002
2000
1999
1998
1997
1996
0
1995
0.2
EMH Swiss Medical Publishers Ltd.
SMW Editorial Secretariat
Farnsburgerstrasse 8
CH-4132 Muttenz
Manuscripts:
Letters to the editor:
Editorial Board:
Internet:
submission@smw.ch
letters@smw.ch
red@smw.ch
http://www.smw.ch
�
 Aurel Perren
Aurel Perren