Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser.
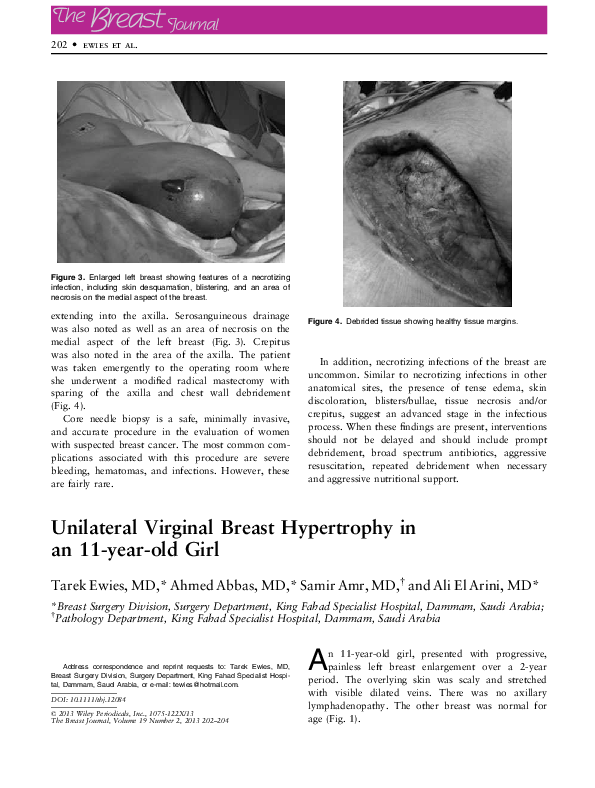
Unilateral Virginal Breast Hypertrophy in an 11-year-old Girl
Related Papers
Purpose: Cystic breast lesions are a common finding in young as well as elderly females. Although, mostly benign; they can at times be malignant too. Timely diagnosis is possible with help of Fine needle aspiration cytology (FNAC). This study was carried out with the aim of studying the panorama of various cystic breast lesions on FNAC in our setup. Materials and Methods: This was a four year prospective study carried out from May 2010 to January 2014. Cystic nature of breast mass was confirmed by palpation and by sonomammography. FNAC was then performed and the smears were stained with MGG and Papanicolaou stain. Results: Out of the 72 cases that were diagnosed to be cystic breast lesions clinically or on sonomammography, 64 were found to be benign and 08 were found to be malignant on FNAC. Retrospective imaging correlation of the 08 cystic cases revealed that they were of complex cystic nature and had either thick septae(03), solid areas (04) or dense contents (01) within. This in...
2023 •
Virginal breast hypertrophy VBH with the sobriquet "gigantomastia" is an uncommon condition with sporadic presentation usually in adolescence. Case presentation: In this retrospective study, eight patients (three case summaries presented, while the clinicopathologic features of all the patients are presented in Table 1) were managed. Discussion: The age range in this retrospective cohort study is 13-34 years and the series consists predominantly of teenagers, a third had bilateral disease, and the symptoms triad of mastalgia, cosmetic concerns, and psychosocial/esteem issues were present in all the patients. With a third consenting to surgical intervention. We present what to our knowledge must be in the global literature, one of the few largest accruals of cases of gigantomastia, the VBH, seen over time in our surgical oncology practice. Conclusion: VBH should be appraised along with other BBD to exclude malignancies and provide prompt and appropriate care whilst limiting complications. A multidisciplinary approach is particularly important and incorporating care for perceived low self-esteem cannot be overemphasized .
American Journal of Roentgenology
Pediatric and Adolescent Breast Masses: A Review of Pathophysiology, Imaging, Diagnosis, and Treatment2013 •
2019 •
Background: Benign breast ds (BBD) are common disease affecting woman mainly. These can be diagnosed by triple assessment including clinical examination, radiological imagings, and a pathological examination. Majority of the benign lesions are not associated with an increased risk for subsequent breast cancer but some may have increased risk of malignancy like atypical hyperplasia. The main problem from women’s patient of view is fear that such a lump may be a cancer. Unlike breast cancer, benign breast diseases have often been difficult to understand, in part due to variety of names that have been used to describe the various conditions. So that clinician requires in-depth knowledge to give clear explanation about breast diseases. Making an early diagnosis and planning the treatment during initial consultations, helps in alleviating unnecessary anxiety about breast cancer and unnecessary long term follow up can be avoided. So, the need for study is to analyze the spectrum of benign breast disease. Method: A total 85 patients diagnosing as benign breast diseases under the inclusion criteria were studied during the period of Oct 2014 to March 2016; in the Dept of Surgery at People’s hospital of People’s college of medical science and research center, Bhopal. Our study objectives were A. To describe the spectrum of Benign Breast Diseases with Respect to Age of incidence, Social Demography, Duration of Symptoms, Site of lumps, Clinical features specific to conditions. B. To diagnose clinically and cytologically (FNAC) Suitable patients with benign breast disease and provide either conservative or operative treatment. C. To do histopathological examination of excised specimen for the comparisons and confirmation of cytological and clinical diagnosis. Result: Fibro adenoma was the most common benign lesion encountered (65.9%) followed by Breast Abscess 18.8% disease. Fibro adenoma was presented most often in the second and third decade (75%). Lump in the breast was the commonest presentation of BBD, Lump and Mastalgia was the second commonest symptom of BBD. There was a slight preponderance of lesions in the right breast (45.9%) as compared to left breast (44.7%), shown to be significant. Most of patients belong to middle class. 100% 0f the patients were in pre menopausal group. Majority (45.9%) of lesions were of the size 2-5 cms, 31.8% were between 6-10 cms FNAC highly reliable for fibro adenoma than for other lesions. All fibro adenomas willing for surgical procedure were managed by simple excision than follow up. All 16 cases of Breast Abscess underwent incision and drainage and simple mastectomy was done in phylloide tumors. Conclusion: In the present study BBD occupy majority of total breast diseases. Fibro adenoma was the most common benign lesion (65.9%). FNAC was highly accurate and was highly reliable for fibro adenoma than for other lesions. Triple test is a prerequisite for determining management. However all fibro adenomas willing for surgical procedure were managed by simple excision than follow up. Conservative approach is acceptable in young patients, who choose conservative management, need to be informed about the limitation of the test, advised for proper follow up, and must be assessed properly if there are symptoms and clinical changes. Breast self examination should be emphasized as a part of female adult education.
Journal of Contemporary Medicine
Approach to Pediatric Breast Masses in Accompaniment with Current Literature2022 •
RELATED PAPERS
Zenodo (CERN European Organization for Nuclear Research)
2022_TRANSPORT AMPHORAS FROM GRAVISCA TO THE EASTERN AEGEAN DURING THE GREEK ARCHAIC PERIOD (7th-6th c. BC): A MULTIDISCIPLINARY APPROACH FOR CHARACTERIZATION, MANUFACTURING, PROVENANCE AND TRADE2022 •
Santangeli (a cura di), Il Codice della Crisi d'Impresa e dell'Insolvenza
Commento artt. 65-66 CCII - Procedure di composizione della crisi da sovraindebitamento. Disposizioni generali. Ambito di applicazione. Procedure familiari2023 •
Journal of basic microbiology
Antimicrobial-producing Pseudoalteromonas from the marine environment of Panama shows a high phylogenetic diversity and clonal structure2018 •
The Horizon of Medical Sciences
Effectiveness of an Educational Program Based on Health Belief Model Regarding Safe Childbirth on Selected Delivery Mode Among Pregnant Women2018 •
The Journal of Infection in Developing Countries
Asymptomatic bacteriuria persisting after catheter removal: are we missing the true catheter associated urinary tract infection burden?Journal of American Studies of Turkey
Dystopian Misogyny: Returning to 1970s Feminist Theory through Kelly Sue DeConnick’s Bitch Planet2018 •
The International Journal of Advanced Manufacturing Technology
Joint optimization of spare parts inventory and maintenance policies using genetic algorithms2006 •
2022 •
Revista Brasileira de Ortopedia
Estudo da relação anatômica do nervo sensitivo radial após fixação percutânea com fios de Kirschner2008 •
JPB Kelautan dan Perikanan Vol. 8 No. 1 Tahun 2013: 55–64
Binder Y.Nuri etal dan ifah J.perik Juni 2013 abstract2013 •
 SAMIR S AMR
SAMIR S AMR